Identification of Depression and Screening for Work Disabilities among Long-Term Unemployed People
Abstract
1. Introduction
2. Materials and Methods
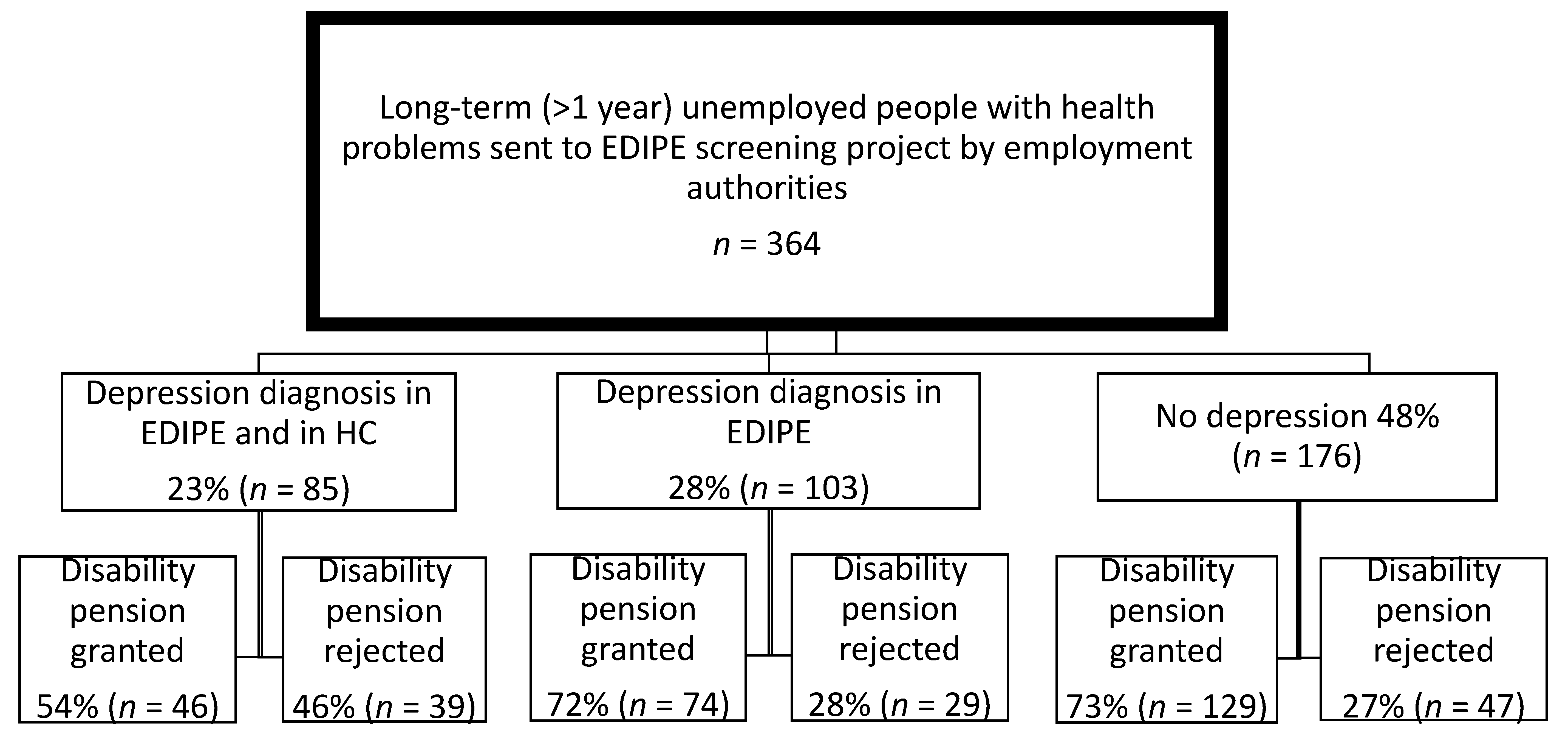
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Marmot, M. The health gap: The challenge of an unequal world. Lancet 2015, 386, 2442–2444. [Google Scholar] [CrossRef]
- Kröger, H.; Pakpahan, E.; Hoffmann, R. What causes health inequality? A systematic review on the relative importance of social causation and health selection. Eur. J. Public Health 2015, 25, 951–960. [Google Scholar] [CrossRef] [PubMed]
- Bartley, M. Unemployment and ill health: Understanding the relationship. J. Epidemiol. Community Health 1994, 48, 333–337. [Google Scholar] [CrossRef] [PubMed]
- Janlert, U. Unemployment as a disease and diseases of the unemployed. Scand. J. Work Environ. Health 1997, 23 (Suppl. S3), 79–83. Available online: www.ncbi.nlm.nih.gov/pubmed/9456072 (accessed on 4 April 2018). [PubMed]
- Jin, R.L.; Shah, C.P.; Svoboda, T.J. The impact of unemployment on health: A review of the evidence. J. Public Health Policy 1997, 18, 275–301. [Google Scholar] [CrossRef]
- Roelfs, D.J.; Shor, E.; Davidson, K.W.; Schwartz, J.E. Losing life and livelihood: A systematic review and meta-analysis of unemployment and all-cause mortality. Soc. Sci. Med. 2011, 72, 840–854. [Google Scholar] [CrossRef] [PubMed]
- Herbig, B.; Dragano, N.; Angerer, P. Health in the long-term unemployed. (Gesundheitliche Situation von langzeitarbeitslosen Menschen.). Dtsch. Arztebl. Int. 2013, 110, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Kaspersen, S.; Pape, K.; Vie, G.; Ose, S.; Krokstad, S.; Gunnell, D.; Bjorngaard, J. Health and unemployment: 14 years of follow-up on job loss in the Norwegian HUNT Study. Eur. J. Public Health 2016, 26, 312–317. [Google Scholar] [CrossRef] [PubMed]
- McKee-Ryan, F.M.; Song, Z.; Wanberg, C.R.; Kinicki, A.J. Psychological and physical well-being during unemployment: A meta-analytic study. J. Appl. Psychol. 2005, 90, 53–76. [Google Scholar] [CrossRef] [PubMed]
- Nwaru, C.A.; Nygård, C.-H.; Virtanen, P. Musculoskeletal pain and re-employment among unemployed job seekers: A three-year follow-up study. BMC Public Health 2016, 16, 531. [Google Scholar] [CrossRef] [PubMed]
- Paul, K.I.; Moser, K. Unemployment impairs mental health: Meta-analyses. J. Vocat. Behav. 2009, 74, 264–282. [Google Scholar] [CrossRef]
- Comino, E.J.; Harris, E.; Silove, D.; Manicavasagar, V.; Harris, M.F. Prevalence, detection and management of anxiety and depressive symptoms in unemployed patients attending general practitioners. Aust. N. Z. J. Psychiatry 2000, 34, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Dooley, D.; Catalano, R.; Wilson, G. Depression and unemployment: Panel findings from the Epidemiologic Catchment Area study. Am. J. Community Psychol. 1994, 22, 745–765. [Google Scholar] [CrossRef] [PubMed]
- Honkonen, T.; Virtanen, M.; Ahola, K.; Kivimäki, M.; Pirkola, S.; Isometsä, E.; Aromaa, A.; Lonnqvist, J. Employment status, mental disorders and service use in the working age population. Scand. J. Work Environ. Health 2007, 33, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Stankunas, M.; Kalediene, R.; Starkuviene, S.; Kapustinskiene, V. Duration of unemployment and depression: A cross-sectional survey in Lithuania. BMC Public Health 2006, 6, 174. [Google Scholar] [CrossRef] [PubMed]
- Andreeva, E.; Hanson, L.L.M.; Westerlund, H.; Theorell, T.; Brenner, M.H. Depressive symptoms as a cause and effect of job loss in men and women: Evidence in the context of organisational downsizing from the Swedish Longitudinal Occupational Survey of Health. BMC Public Health 2015, 15, 1045. [Google Scholar] [CrossRef] [PubMed]
- Pensola, T.; Järvikoski, A.; Järvisalo, J. Unemployment and work ability. In Dimensions of Work Ability: Results of the Health; Gould, R., Ilmarinen, J., Järvisalo, J., Koskinen, S., Eds.; Finnish Centre for Pensions (ETK)/The Social Insurance Institution (Kela)/National Public Health Institute (KTL): Helsinki, Finland, 2008; pp. 123–130, ISBN 978-951-691-096-6 (printed book), ISBN 978-951-691-097-3 (PDF). [Google Scholar]
- Lee, S.A.; Ju, Y.J.; Han, K.-T.; Choi, J.W.; Yoon, H.J.; Park, E.-C. The association between loss of work ability and depression: a focus on employment status. Int. Arch. Occup. Environ. Health 2017, 90, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Lundin, A.; Kjellberg, K.; Leijon, O.; Punnett, L.; Hemmingsson, T. The Association between Self-Assessed Future Work Ability and Long-Term Sickness Absence, Disability Pension and Unemployment in a General Working Population: A 7-Year Follow-Up Study. J. Occup. Rehabil. 2016, 26, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Szlachta, E.; Gawlik-Chmiel, B.; Kallus, K.W. Do the long-term unemployed regard themselves as able to work? J. Public Health 2012, 20, 505–511. [Google Scholar] [CrossRef]
- Kerätär, R.; Taanila, A.; Jokelainen, J.; Soukainen, J.; Ala-Mursula, L. Work disabilities and unmet needs for health care and rehabilitation among jobseekers: A community-level investigation using multidimensional work ability assessments. Scand. J. Prim. Health Care 2016, 34, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Kerätär, R.; Karjalainen, V. Pitkäaikaistyöttömillä on runsaasti hoitamattomia mielenterveyshäiriöitä. (High level of untreated mental disturbances among the long-term unemployed.). Suom. Lääkäril. (Finnish Med. J.) 2010, 65, 3683–3690. [Google Scholar]
- Åhs, A.; Burell, G.; Westerling, R. Care or not care—that is the question: Predictors of healthcare utilisation in relation to employment status. Int. J. Behav. Med. 2012, 19, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Joska, J.; Flisher, A.J. The assessment of need for mental health services. Soc. Psychiatry Psychiatr. Epidemiol. 2005, 40, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Åhs, A.M.H.; Westerling, R. Health care utilization among persons who are unemployed or outside the labour force. Health Policy 2006, 78, 178–193. [Google Scholar] [CrossRef] [PubMed]
- Työministeriö (Ministry of Labour). Pitkäaikaistyöttömien Eläkemahdollisuuksien Selvittäminen (ELMA); Eligibility for a Disability Pension-Project; Ohje nro (Instructions Number) O/2/2004 TM 2004; Ministry of Labour: Helsinki, Finland, 2004.
- World Health Organization. International Classification of Diseases (ICD-10). 2015. Available online: http://apps.who.int/classifications/icd10/browse/2016/en (accessed on 11 August 2017).
- Heikkinen, V. Long-Term Unemployed or Permanently Disabled: Types and Narratives from an Industrial Town of the 2000s, 2016. University of Tampere. Available online: http://urn.fi/URN:ISBN:978-952-03-0280-1 (accessed on 11 August 2017).
- Nurmela, K.; Heikkinen, V.; Hokkanen, R.; Joukamaa, M.; Ylinen, A.; Uitti, J.; Mattila, A.; Virtanen, P. Identification of alcohol abuse and transition from long-term unemployment to disability pension. Scand. J. Public Health 2015, 43, 518–524. [Google Scholar] [CrossRef] [PubMed]
- Employees Pensions Act (Finland). 2006. Available online: http://finlex.fi/fi/laki/ajantasa/2006/20060395 (accessed on 4 April 2018).
- Virtanen, P. Unemployment, re-employment and the use of primary health care services. Scand. J. Prim. Health Care 1993, 11, 228–233. [Google Scholar] [CrossRef] [PubMed]
- Comino, E.J.; Harris, E.; Chey, T.; Manicavasagar, V.; Wall, J.P.; Davies, G.P.; Harris, M.F. Relationship between mental health disorders and unemployment status in Australian adults. Aust. N. Z. J. Psychiatry 2003, 37, 230–235. [Google Scholar] [CrossRef] [PubMed]
- Bühler, B.; Kocalevent, R.; Berger, R.; Mahler, A.; Preiß, B.; Liwowsky, I.; Carl, P.; Hegerl, U. Treatment situation of long-term unemployed with psychological disorders. | Versorgungssituation von Langzeitarbeitslosen mit psychischen Störungen. Nervenarzt 2013, 84, 603–607. [Google Scholar] [CrossRef] [PubMed]
- Liwowsky, I.; Kramer, D.; Mergl, R.; Bramesfeld, A.; Allgaier, A.-K.; Pöppel, E.; Hegerl, U. Screening for depression in the older long-term unemployed. Soc. Psychiatry Psychiatr. Epidemiol. 2009, 44, 622–627. [Google Scholar] [CrossRef] [PubMed]
- Gustafsson, K.; Aronsson, G.; Marklund, S.; Wikman, A.; Floderus, B. Peripheral labour market position and risk of disability pension: A prospective population-based study. BMJ Open 2014, 4, e005230. [Google Scholar] [CrossRef] [PubMed]
- Lamberg, T.; Virtanen, P.; Vahtera, J.; Luukkaala, T.; Koskenvuo, M. Unemployment, depressiveness and disability retirement: A follow-up study of the Finnish HeSSup population sample. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, P.; Kivimäki, M.; Vahtera, J.; Koskenvuo, M. Employment status and differences in the one-year coverage of physician visits: Different needs or unequal access to services? BMC Health Serv. Res. 2006, 6, 123. [Google Scholar] [CrossRef] [PubMed]
- Markkula, N.; Suvisaari, J.; Saarni, S.I.; Pirkola, S.; Peña, S.; Saarni, S.; Ahola, K.; Mattila, A.K.; Viertiö, S.; Strehle, J.; et al. Prevalence and correlates of major depressive disorder and dysthymia in an eleven-year follow-up—Results from the Finnish Health 2011 Survey. J. Affect. Disord. 2015, 173, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Nurmela, K.; Mattila, A.; Heikkinen, V.; Uitti, J.; Ylinen, A.; Virtanen, P. Identification of major depressive disorder among the long-term unemployed. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Korkeila, K.; Suominen, S.; Ahvenainen, J.; Ojanlatva, A.; Rautava, P.; Helenius, H.; Koskenvuo, M. Non-response and related factors in a nation-wide health survey. Eur. J. Epidemiol. 2001, 17, 991–999. [Google Scholar] [CrossRef] [PubMed]
- Torvik, F.A.; Rognmo, K.; Tambs, K. Alcohol use and mental distress as predictors of non-response in a general population health survey: The HUNT study. Soc. Psychiatry Psychiatr. Epidemiol. 2012, 47, 805–816. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, A.J.; Vaze, A.; Rao, S. Clinical diagnosis of depression in primary care: A meta-analysis. Lancet 2009, 374, 609–619. [Google Scholar] [CrossRef]
| Depression Diagnosis in HC and EDIPE | Depression Diagnosis in EDIPE | No Depression | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | p1 | |
| 85 | 23.4 | 103 | 28.3 | 176 | 48.4 | ||
| Gender | 0.035 | ||||||
| Female | 41 | 48.2 | 37 | 35.9 | 56 | 31.8 | |
| Male | 44 | 51.8 | 66 | 64.1 | 120 | 68.2 | |
| Age | 0.662 | ||||||
| 24–39 years | 6 | 7.1 | 4 | 3.9 | 13 | 7.4 | |
| 40–49 years | 19 | 22.4 | 18 | 17.5 | 32 | 18.2 | |
| 50–59 years | 57 | 67.1 | 72 | 69.9 | 118 | 67.0 | |
| 60–63 years | 3 | 3.5 | 9 | 8.7 | 13 | 7.4 | |
| Marital status | 0.293 | ||||||
| Single | 57 | 67.1 | 74 | 71.8 | 134 | 76.1 | |
| Married/cohabiting | 28 | 32.9 | 29 | 28.2 | 42 | 23.9 | |
| Occupation | 0.050 | ||||||
| Non-manual worker | 17 | 20.5 | 16 | 16.2 | 23 | 13.3 | |
| Skilled manual worker | 54 | 65.1 | 74 | 74.7 | 112 | 64.7 | |
| Unskilled manual worker | 12 | 14.5 | 9 | 9.1 | 38 | 22.0 | |
| Duration of unemployment in quartiles | 0.003 | ||||||
| 1–6 years | 30 | 35.3 | 24 | 23.3 | 28 | 15.9 | |
| 7–10 years | 21 | 24.7 | 22 | 21.4 | 39 | 22.2 | |
| 11–13 years | 11 | 12.9 | 34 | 33.0 | 53 | 30.1 | |
| 14–35 years | 23 | 27.1 | 23 | 22.3 | 56 | 31.8 | |
| Visits to health care in quartiles (3 years prior to EDIPE) | 0.001 | ||||||
| 0–3 | 16 | 18.8 | 31 | 30.1 | 40 | 22.7 | |
| 4–7 | 16 | 18.8 | 23 | 22.3 | 48 | 27.3 | |
| 8–13 | 16 | 18.8 | 30 | 29.1 | 52 | 29.5 | |
| 14–72 | 37 | 43.5 | 19 | 18.4 | 36 | 20.5 | |
| Somatic diagnoses on EDIPE | 0.539 | ||||||
| None | 2 | 2.4 | 1 | 1.0 | 8 | 4.5 | |
| 1–3 | 42 | 49.4 | 54 | 52.4 | 88 | 50.0 | |
| ≥4 | 41 | 48.2 | 48 | 46.6 | 80 | 45.5 | |
| AUD on EDIPE | 0.775 | ||||||
| No | 42 | 49.4 | 53 | 51.5 | 95 | 54.0 | |
| Yes | 43 | 50.6 | 50 | 48.5 | 81 | 46.0 | |
| OR | 95% CI | p1 | |
|---|---|---|---|
| Model 1 | |||
| Crude model | |||
| Depression diagnosis in EDIPE and in HC | 1 | ||
| Depression diagnosis in EDIPE | 2.16 | 1.18; 3.96 | 0.012 |
| No depression | 2.33 | 1.35; 4.00 | 0.002 |
| Model 2 | |||
| Adjusted for sociodemographic characteristics: Age, gender, marital status | |||
| Depression diagnosis in EDIPE and in HC | 1 | ||
| Depression diagnosis in EDIPE | 2.05 | 1.11; 3.79 | 0.022 |
| No depression | 2.18 | 1.26; 3.79 | 0.006 |
| Model 3 | |||
| Adjusted for: Age, gender, marital status, number of visits to HC | |||
| Depression diagnosis in EDIPE and in HC | 1 | ||
| Depression diagnosis in EDIPE | 2.35 | 1.24; 4.43 | 0.008 |
| No depression | 2.44 | 1.38; 4.31 | 0.002 |
| Model 4 | |||
| Adjusted for: Age, gender, marital status, number of visits to HC, number of somatic diagnoses on EDIPE | |||
| Depression diagnosis in EDIPE and in HC | 1 | ||
| Depression diagnosis in EDIPE | 2.35 | 1.24; 4.43 | 0.008 |
| No depression | 2.45 | 1.39; 4.32 | 0.002 |
| Model 5 | |||
| Full model. Adjusted for: Age, gender, marital status, occupational status, duration of unemployment, number of visits to HC, number of somatic diagnoses on EDIPE, AUD on EDIPE | |||
| Depression diagnosis in EDIPE and in HC | 1 | ||
| Depression diagnosis in EDIPE | 2.22 | 1.14; 4.33 | 0.020 |
| No depression | 2.32 | 1.26; 4.24 | 0.007 |
| Age | 1.04 | 1.00; 1.08 | 0.045 |
| Gender (male → female) | 1.25 | 0.73; 2.13 | 0.410 |
| Marital status (married → single) | 1.42 | 0.83; 2.44 | 0.199 |
| Number of visits to HC | 1.02 | 0.99; 1.05 | 0.187 |
| Number of somatic diagnoses on EDIPE | 1.05 | 0.91; 1.21 | 0.510 |
| Occupational status (skilled manual worker → non-manual worker) | 0.38 | 0.14; 1.03 | 0.057 |
| Occupational status (unskilled manual worker → non-manual worker) | 0.41 | 0.17; 0.94 | 0.036 |
| Duration of unemployment | 1.03 | 0.98; 1.08 | 0.283 |
| AUD on EDIPE | 0.43 | 0.24; 0.70 | 0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nurmela, K.; Mattila, A.; Heikkinen, V.; Uitti, J.; Ylinen, A.; Virtanen, P. Identification of Depression and Screening for Work Disabilities among Long-Term Unemployed People. Int. J. Environ. Res. Public Health 2018, 15, 909. https://doi.org/10.3390/ijerph15050909
Nurmela K, Mattila A, Heikkinen V, Uitti J, Ylinen A, Virtanen P. Identification of Depression and Screening for Work Disabilities among Long-Term Unemployed People. International Journal of Environmental Research and Public Health. 2018; 15(5):909. https://doi.org/10.3390/ijerph15050909
Chicago/Turabian StyleNurmela, Kirsti, Aino Mattila, Virpi Heikkinen, Jukka Uitti, Aarne Ylinen, and Pekka Virtanen. 2018. "Identification of Depression and Screening for Work Disabilities among Long-Term Unemployed People" International Journal of Environmental Research and Public Health 15, no. 5: 909. https://doi.org/10.3390/ijerph15050909
APA StyleNurmela, K., Mattila, A., Heikkinen, V., Uitti, J., Ylinen, A., & Virtanen, P. (2018). Identification of Depression and Screening for Work Disabilities among Long-Term Unemployed People. International Journal of Environmental Research and Public Health, 15(5), 909. https://doi.org/10.3390/ijerph15050909





