In Hospital Stroke Mortality: Rates and Determinants in Southwestern Saudi Arabia
Abstract
1. Introduction
2. Methods
2.1. Settings
2.2. Study Area
2.3. Data Collection
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Thrift, A.G.; Thayabaranathan, T.; Howard, G.; Howard, V.J.; Rothwell, P.M.; Feigin, V.L.; Norrving, B.; Donnan, G.A.; Cadilhac, D.A. Global stroke statistics. Int. J. Stroke 2017, 12, 13–32. [Google Scholar] [CrossRef] [PubMed]
- Koennecke, H.-C.; Belz, W.; Berfelde, D.; Endres, M.; Fitzek, S.; Hamilton, F.; Kreitsch, P.; Mackert, B.-M.; Nabavi, D.; Nolte, C. Factors influencing in-hospital mortality and morbidity in patients treated on a stroke unit. Neurology 2011, 77, 965–972. [Google Scholar] [CrossRef] [PubMed]
- Candelise, L.; Gattinoni, M.; Bersano, A.; Micieli, G.; Sterzi, R.; Morabito, A.; Group, T.P.S. Stroke-unit care for acute stroke patients: An observational follow-up study. Lancet 2007, 369, 299–305. [Google Scholar] [CrossRef]
- Rocha, M.S.G.; Almeida, A.C.F.; Abath Neto, O.; Porto, M.P.; Brucki, S.M.D. Impact of stroke unit in a public hospital on length of hospitalization and rate of early mortality of ischemic stroke patients. Arq. Neuro-Psiquiatr. 2013, 71, 774–779. [Google Scholar] [CrossRef] [PubMed]
- Borhani-Haghighi, A.; Safari, R.; Heydari, S.T.; Soleimani, F.; Sharifian, M.; Kashkuli, S.Y.; Khayatghuchani, M.N.; Azadi, M.; Shariat, A.; Safari, A. Hospital mortality associated with stroke in Southern Iran. Iran. J. Med. Sci. 2013, 38, 314–320. [Google Scholar] [PubMed]
- Matsui, H.; Fushimi, K.; Yasunaga, H. Variation in risk-standardized mortality of stroke among hospitals in Japan. PLoS ONE 2015, 10, e0139216. [Google Scholar] [CrossRef] [PubMed]
- Myint, P.K.; Bachmann, M.O.; Loke, Y.K.; Musgrave, S.D.; Price, G.M.; Hale, R.; Metcalf, A.K.; Turner, D.A.; Day, D.J.; Warburton, E.A. Important factors in predicting mortality outcome from stroke: Findings from the anglia stroke clinical network evaluation study. Age Ageing 2017, 46, 83–90. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nimptsch, U.; Mansky, T. Stroke unit care and trends of in-hospital mortality for stroke in Germany 2005–2010. Int. J. Stroke 2014, 9, 260–265. [Google Scholar] [CrossRef] [PubMed]
- Reeves, M.J.; Bushnell, C.D.; Howard, G.; Gargano, J.W.; Duncan, P.W.; Lynch, G.; Khatiwoda, A.; Lisabeth, L. Sex differences in stroke: Epidemiology, clinical presentation, medical care and outcomes. Lancet Neurol. 2008, 7, 915–926. [Google Scholar] [CrossRef]
- El-Hajj, M.; Salameh, P.; Rachidi, S.; Hosseini, H. The epidemiology of stroke in the Middle East. Eur. Stroke J. 2016, 1, 180–198. [Google Scholar] [CrossRef]
- Almekhlafi, M.A. Trends in one-year mortality for stroke in a tertiary academic center in Saudi Arabia: A 5-year retrospective analysis. Ann. Saudi Med. 2016, 36, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Barker-Collo, S.; Bennett, D.A.; Krishnamurthi, R.V.; Parmar, P.; Feigin, V.L.; Naghavi, M.; Forouzanfar, M.H.; Johnson, C.O.; Nguyen, G.; Mensah, G.A. Sex differences in stroke incidence, prevalence, mortality and disability-adjusted life years: Results from the global burden of disease study 2013. Neuroepidemiology 2015, 45, 203–214. [Google Scholar] [CrossRef] [PubMed]
- Feigin, V.L.; Abajobir, A.; Abate, K.; Abd-Allah, F.; Abdulle, A.; Abera, S.; Abyu, G.; Ahmed, M.; Ärnlöv, J.; Vos, T. Global, regional and national burden of neurological disorders during 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet Neurol. 2017, 16, 877–897. [Google Scholar] [CrossRef]
- Al Khathaami, A.M.; Algahtani, H.; Alwabel, A.; Alosherey, N.; Kojan, S.; Aljumah, M. The status of acute stroke care in Saudi Arabia: An urgent call for action! Int. J. Stroke 2011, 6, 75–76. [Google Scholar] [CrossRef] [PubMed]
- Statistical Yearbook of 2016. Issue Number: 52. Available online: https://www.stats.gov.sa/en/866-0 (accessed on 22 January 2018).
- Okeng’o, K.; Chillo, P.; Gray, W.K.; Walker, R.W.; Matuja, W. Early mortality and associated factors among patients with stroke admitted to a large teaching hospital in Tanzania. J. Stroke Cerebrovasc. Dis. 2017, 26, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Ryglewicz, D.; Barañska-Gieruszczak, M.; Lechowicz, W.; Hier, D.B. High case-fatality rates in the warsaw stroke registry. J. Stroke Cerebrovasc. Dis. 1997, 6, 421–425. [Google Scholar] [CrossRef]
- Goulart, A.C.; Bensenor, I.M.; Fernandes, T.G.; Alencar, A.P.; Fedeli, L.M.; Lotufo, P.A. Early and one-year stroke case fatality in Sao Paulo, Brazil: Applying the world health organization’s stroke steps. J. Stroke Cerebrovasc. Dis. 2012, 21, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Van Asch, C.J.; Luitse, M.J.; Rinkel, G.J.; van der Tweel, I.; Algra, A.; Klijn, C.J. Incidence, case fatality and functional outcome of intracerebral haemorrhage over time, according to age, sex and ethnic origin: A systematic review and meta-analysis. Lancet Neurol. 2010, 9, 167–176. [Google Scholar] [CrossRef]
- Kalėdienė, R.; Rastenytė, D. Trends and regional inequalities in mortality from stroke in the context of health care reform in Lithuania. Medicina 2016, 52, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Alhazzani, A.A.; Mahfouz, A.A.; Abolyazid, A.Y.; Awadalla, N.J.; Aftab, R.; Faraheen, A.; Khalil, S.N. Study of stroke incidence in the aseer region, Southwestern Saudi Arabia. Int. J. Environ. Res. Public Health 2018, 15, 215. [Google Scholar] [CrossRef] [PubMed]
- Thrift, A.G.; Howard, G.; Cadilhac, D.A.; Howard, V.J.; Rothwell, P.M.; Thayabaranathan, T.; Feigin, V.L.; Norrving, B.; Donnan, G.A. Global stroke statistics: An update of mortality data from countries using a broad code of “cerebrovascular diseases”. Int. J. Stroke 2017, 12, 796–801. [Google Scholar] [CrossRef] [PubMed]
- Nkoke, C.; Lekoubou, A.; Balti, E.; Kengne, A.P. Stroke mortality and its determinants in a resource-limited setting: A prospective cohort study in Yaounde, Cameroon. J. Neurol. Sci. 2015, 358, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Nadiah, W.-A.; Amir, W.A.; Muzaimi, M.; Mustafa, M.; Naing, N.N. Determinants of mortality in first-ever stroke patients in the suburban Malaysia: A retrospective hospital-based study, 2005–2011. Iran. J. Public Health 2015, 44, 1291–1293. [Google Scholar]
- Edjoc, R.K.; Reid, R.D.; Sharma, M.; Fang, J. The prognostic effect of cigarette smoking on stroke severity, disability, length of stay in hospital and mortality in a cohort with cerebrovascular disease. J. Stroke Cerebrovasc. Dis. 2013, 22, e446–e454. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Schooling, C.M.; Chan, W.M.; Lee, S.Y.; Leung, G.M.; Lam, T.H. Smoking and hemorrhagic stroke mortality in a prospective cohort study of older Chinese. Stroke 2013, 44, 2144–2149. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.A.; Walter, J.M.; Karve, S.J.; Skolarus, L.E.; Levine, S.R.; Mulhorn, K.A. Smoking and mortality in stroke survivors: Can we eliminate the paradox? J. Stroke Cerebrovasc. Dis. 2014, 23, 1282–1290. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Yang, Y.; Jin, H.; Fan, C.; Lv, P.; Sun, W.; Peng, Q.; Zhao, M.; Jin, D.K.; Wang, J.; et al. Discrepant relationships between admission blood pressure and mortality in different stroke subtypes. J. Neurol. Sci. 2017, 383, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Ntaios, G.; Faouzi, M.; Ferrari, J.; Lang, W.; Vemmos, K.; Michel, P. An integer-based score to predict functional outcome in acute ischemic stroke the astral score. Neurology 2012, 78, 1916–1922. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.; Rudd, T.; Lewis, R.R.; Hunt, B.J. Mortality from pulmonary embolism after acute stroke: Can we do better? Age Ageing 2002, 31, 159–161. [Google Scholar] [CrossRef] [PubMed]

| Age | Males | Females | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|
| No. Died | CFR (%) | 95% CI | No. Died | CFR (%) | 95% CI | No. Died | CFR (%) | 95% CI | |
| <40– | 10 | 14.3 | 7.1–24.7 | 4 | 6.8 | 2.2–15.5 | 14 | 10.9 | 6.1–17.5 |
| 40–49 | 3 | 3.9 | 1.0–10.4 | 4 | 8.5 | 2.4–20.4 | 7 | 5.7 | 2.3–11.4 |
| 50–59 | 11 | 9.0 | 4.8–15.1 | 5 | 8.6 | 2.9–19.0 | 16 | 8.9 | 5.2–14.0 |
| 60–69 | 8 | 5.4 | 2.6–10.1 | 7 | 8.9 | 3.6–17.4 | 15 | 6.6 | 3.8–10.7 |
| 70–79 | 14 | 8.4 | 4.7–13.7 | 4 | 3.9 | 1.1–9.6 | 18 | 6.7 | 4.0–10.3 |
| 80+ | 25 | 12.9 | 8.5–18.4 | 26 | 20.5 | 13.8–28.5 | 51 | 15.9 | 12.1–20.4 |
| Total | 71 | 9.1 | 7.3–11.3 | 50 | 10.6 | 7.9–13.7 | 121 | 9.7 | 8.1–11.5 |
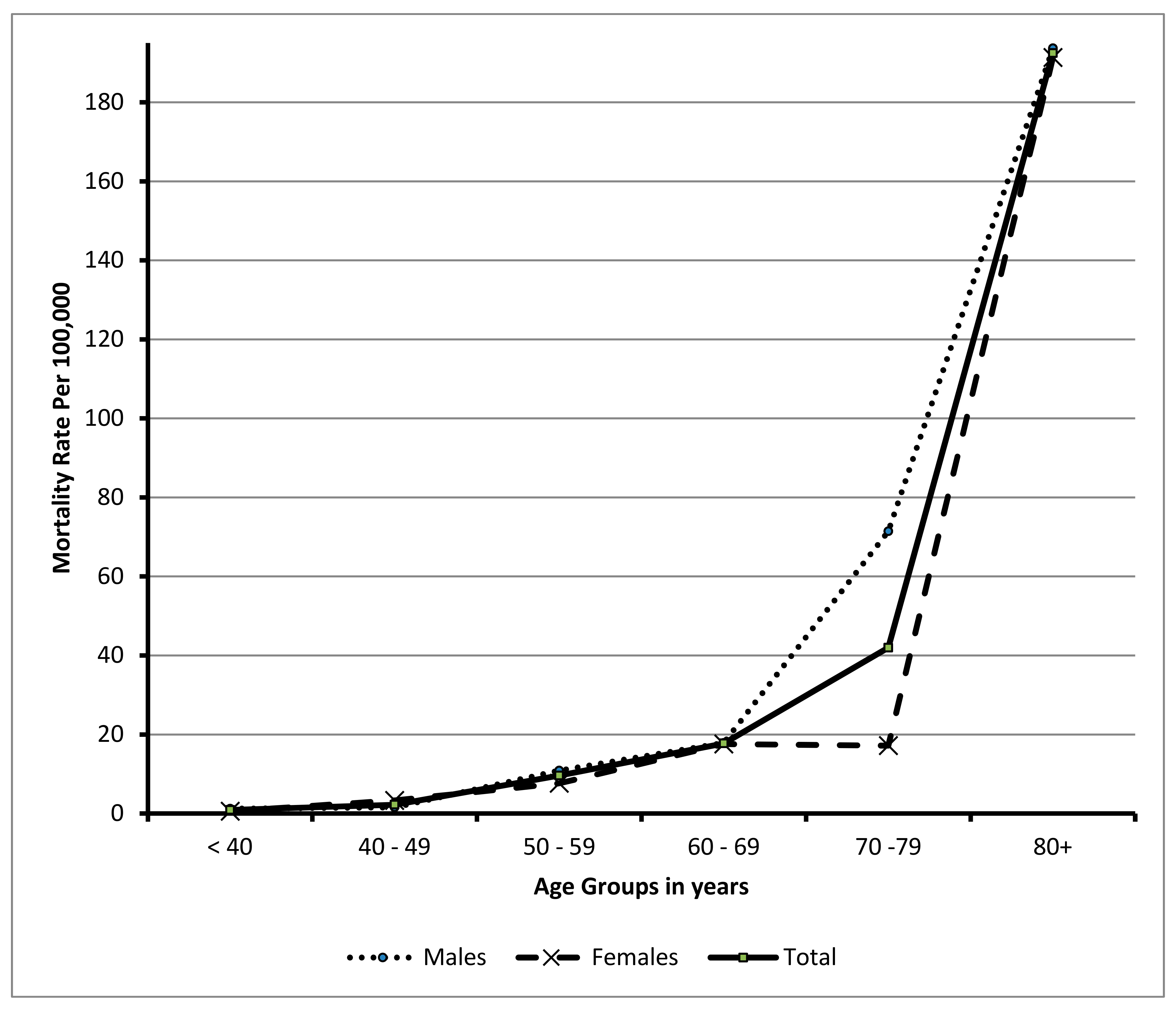
| Age Group | Males | Females | Total | |||
|---|---|---|---|---|---|---|
| Deaths/Pop. | Mortality Rate per 100,000 (95%CI) | Deaths/Pop. | Mortality Rate per 100,000 (95%CI) | Deaths/Pop. | Mortality Rate per 100,000 (95%CI) | |
| <40 | 10/813,170 | 1.230 (1.20–1.260) * | 4/719,814 | 0.560 (0.550–0.561) * | 14/1,532,984 | 0.910 (0.890–0.930) |
| 40–49 | 3/192,850 | 1.555 (1.500–1.610) * | 4/120,629 | 3.310 (3.220–3.420) * | 7/313,479 | 2.230 (2.180–2.290) |
| 50–59 | 11/101,192 | 10.870 (10.680–11.060) * | 5/65,405 | 7.644 (7.440–7.850) * | 16/166,597 | 9.604 (9.460–9.750) |
| 60–69 | 8/44,736 | 17.882 (17.530–18.240) | 7/39,806 | 17.585 (17.210–17.960) | 15/84,542 | 17.742 (17.490–18.000) |
| 70–79 | 14/19,603 | 71.417 (70.78–72.05) * | 4/23,280 | 17.18 (16.70–17.67) * | 18/42,883 | 41.97 (38.0–53.0) |
| 80+ | 25/12,909 | 193.66(186.9–200.6) | 26/13,589 | 191.33 (184.7–198.0) | 51/26,498 | 192.46 (187.7–197.3) |
| Total | 71/1,184,460 | 38.491 (38.270–38.710) * | 50/982,523 | 5.10 (5.050–5.130) * | 121/2,166,983 | 5.584 (5.550–5.610) |
| Variables | Hazard Ratio (HR) | 95.0% CI | |
|---|---|---|---|
| Lower | Upper | ||
| Socio-Demographic: | |||
| Age: 70+ vs. < 70 years | 0.950 | 0.601 | 1.500 |
| Gender: Females vs. Males | 1.317 | 0.856 | 2.025 |
| Altitude: Low vs. High | 1.220 | 0.778 | 1.913 |
| Nationality: Non-Saudi vs. Saudi | 1.644 | 0.905 | 2.985 |
| History: | |||
| Family History of stroke: Yes vs. No | 0.646 | 0.277 | 1.511 |
| Diabetes Mellitus: Yes vs. No | 0.721 | 0.429 | 1.210 |
| Hypertension: Yes vs. No * | 1.776 | 1.056 | 2.988 |
| Hypercholesterolemia: Yes vs. No | 1.208 | 0.738 | 1.977 |
| Current Smoker: Yes vs. No * | 2.363 | 1.202 | 4.643 |
| Obesity: Yes vs. No | 1.322 | 0.884 | 1.977 |
| Atrial Fibrillation: Yes vs. No | 1.016 | 0.531 | 1.943 |
| Clinical Condition on Admission: | |||
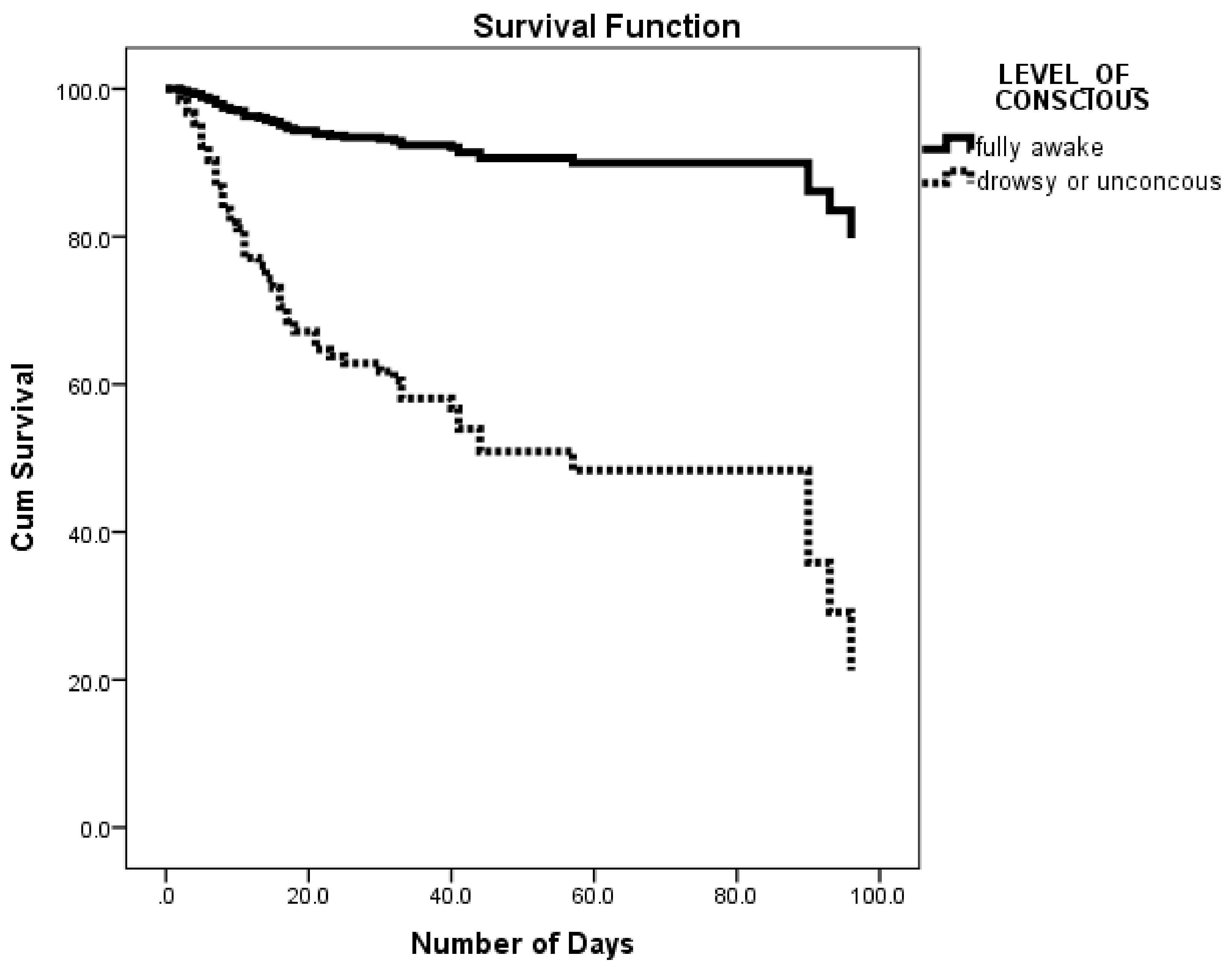
| Level of consciousness: Drowsy or unconscious vs. alert * | 6.861 | 3.942 | 11.941 |
| Mobility: Immobile vs. mobile * | 2.605 | 1.559 | 4.352 |
| Hospital arrival time: 3 h+ vs. < 3 h | 1.319 | 0.827 | 2.104 |
| In-hospital compilations: | |||
| Deep Vein Thrombosis: Yes vs. No | 0.873 | 0.197 | 3.879 |
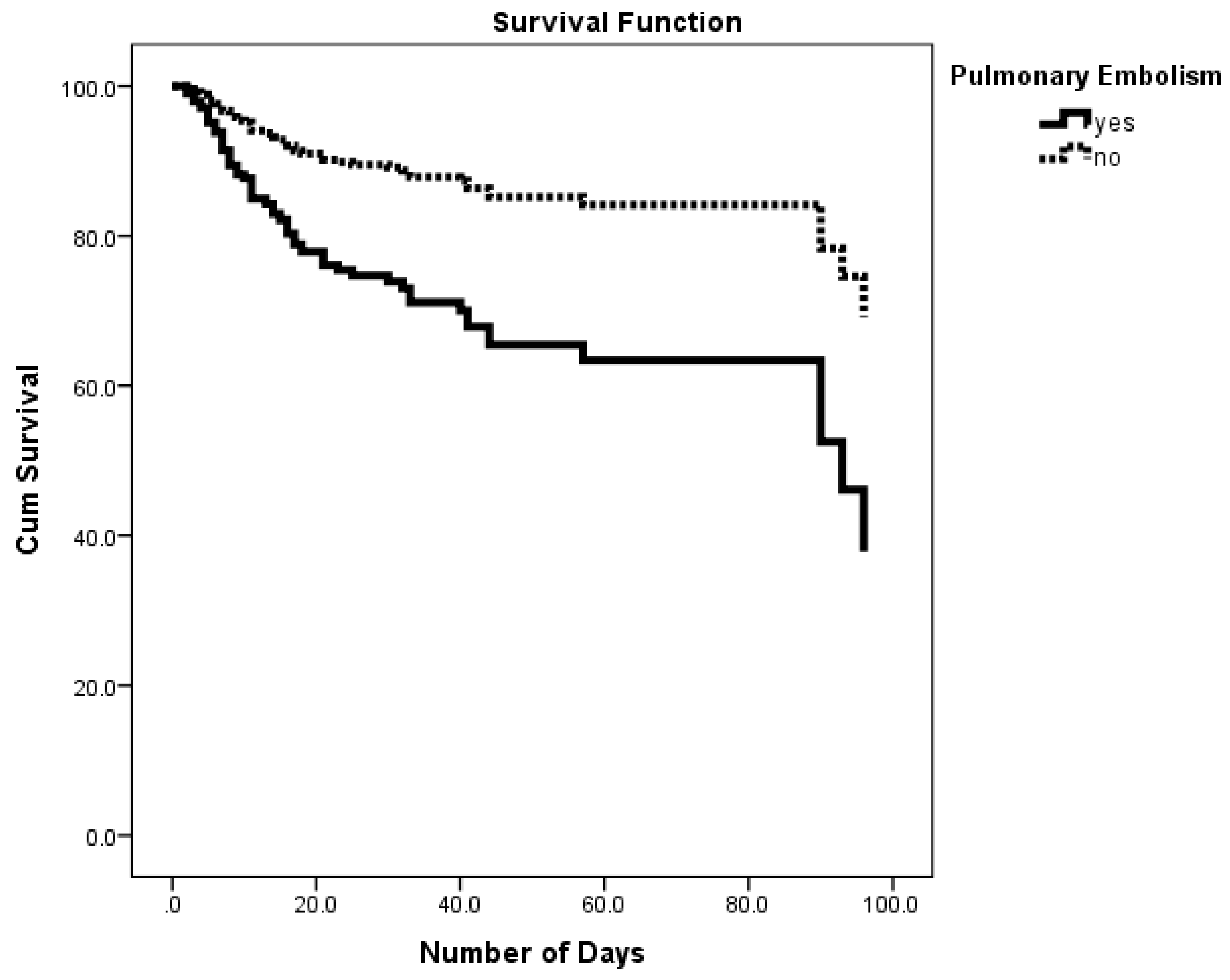
| Pulmonary Embolism: Yes vs. No * | 2.636 | 1.516 | 4.585 |
| Pneumonia: Yes vs. No | 0.700 | 0.447 | 1.096 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alhazzani, A.A.; Mahfouz, A.A.; Abolyazid, A.Y.; Awadalla, N.J.; Katramiz, K.; Faraheen, A.; Khalil, S.N.; Aftab, R. In Hospital Stroke Mortality: Rates and Determinants in Southwestern Saudi Arabia. Int. J. Environ. Res. Public Health 2018, 15, 927. https://doi.org/10.3390/ijerph15050927
Alhazzani AA, Mahfouz AA, Abolyazid AY, Awadalla NJ, Katramiz K, Faraheen A, Khalil SN, Aftab R. In Hospital Stroke Mortality: Rates and Determinants in Southwestern Saudi Arabia. International Journal of Environmental Research and Public Health. 2018; 15(5):927. https://doi.org/10.3390/ijerph15050927
Chicago/Turabian StyleAlhazzani, Adel A., Ahmed A. Mahfouz, Ahmed Y. Abolyazid, Nabil J. Awadalla, Khaled Katramiz, Aesha Faraheen, Shamsun Nahar Khalil, and Razia Aftab. 2018. "In Hospital Stroke Mortality: Rates and Determinants in Southwestern Saudi Arabia" International Journal of Environmental Research and Public Health 15, no. 5: 927. https://doi.org/10.3390/ijerph15050927
APA StyleAlhazzani, A. A., Mahfouz, A. A., Abolyazid, A. Y., Awadalla, N. J., Katramiz, K., Faraheen, A., Khalil, S. N., & Aftab, R. (2018). In Hospital Stroke Mortality: Rates and Determinants in Southwestern Saudi Arabia. International Journal of Environmental Research and Public Health, 15(5), 927. https://doi.org/10.3390/ijerph15050927





