Outcomes of Secondary Prevention among Coronary Heart Disease Patients in a High-Risk Region in Finland
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Ethical Approval
2.3. Data Analysis
3. Results
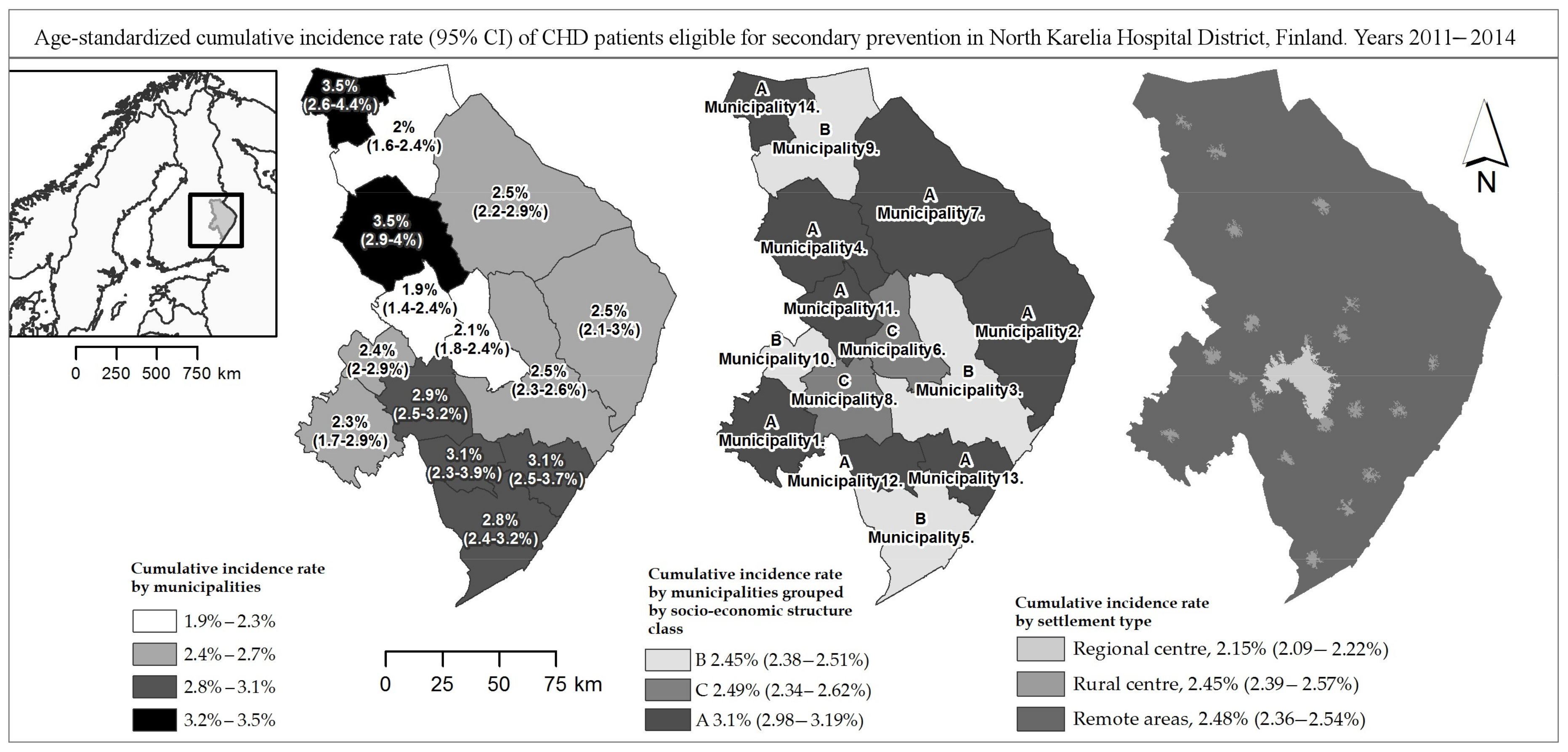
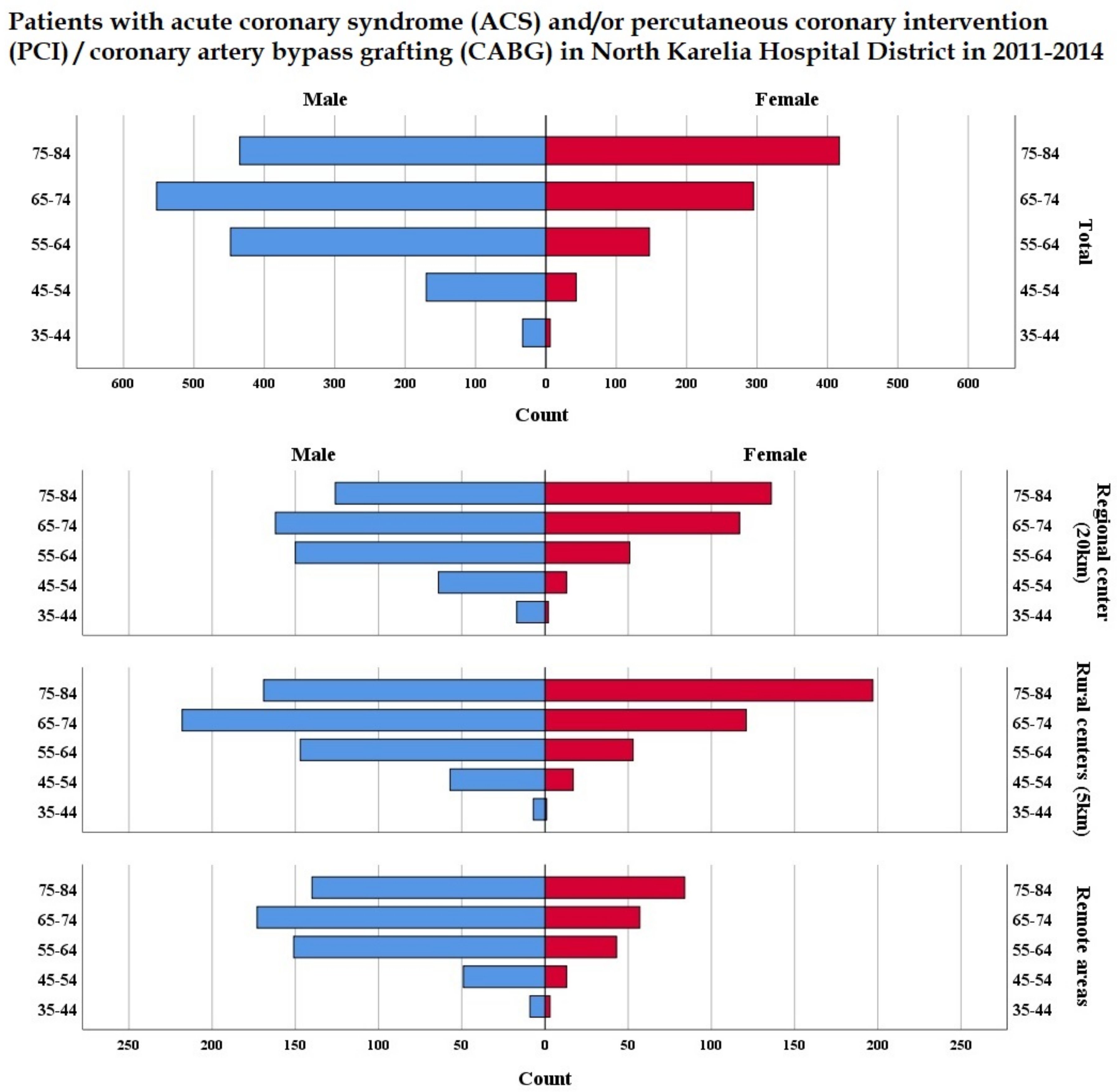
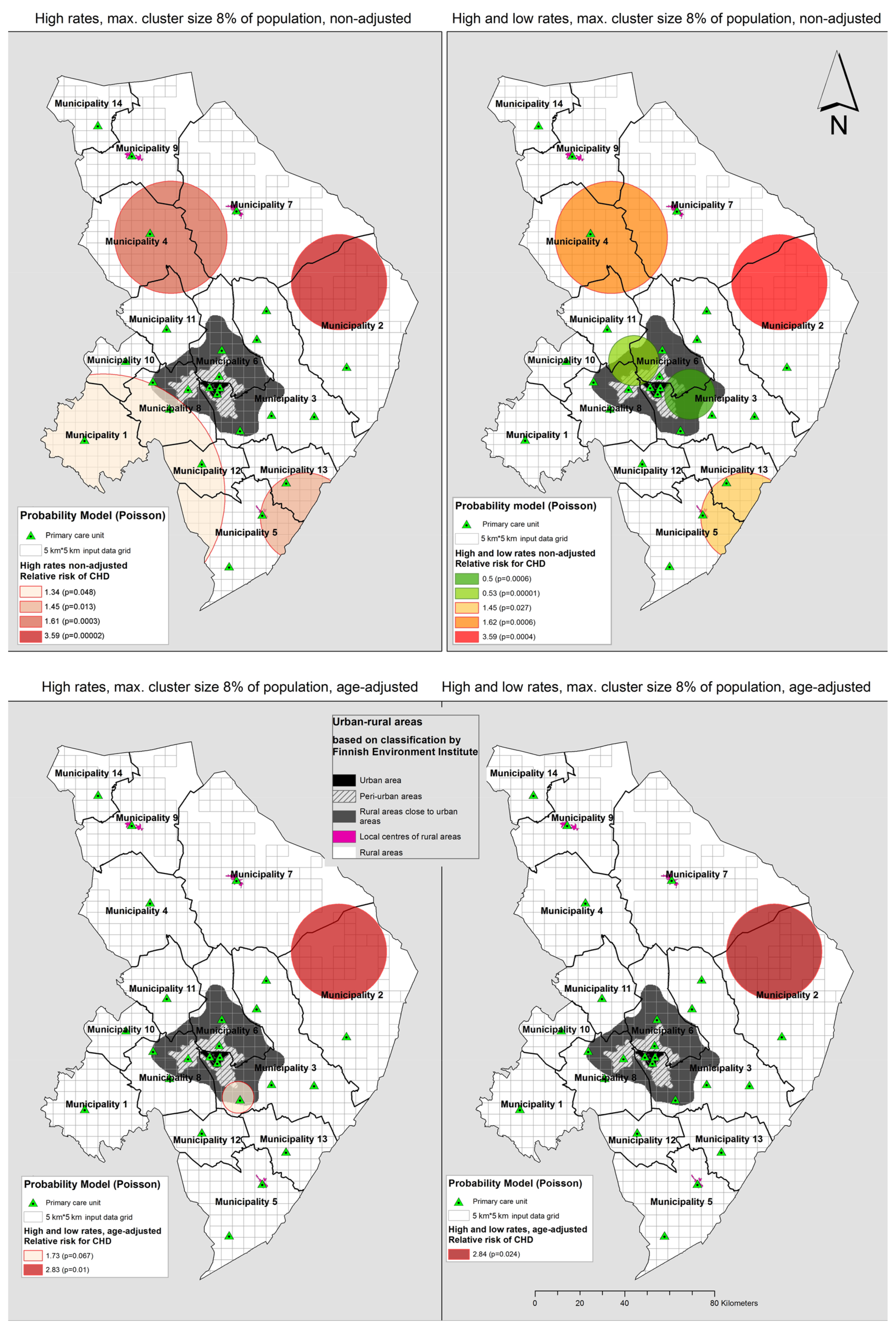
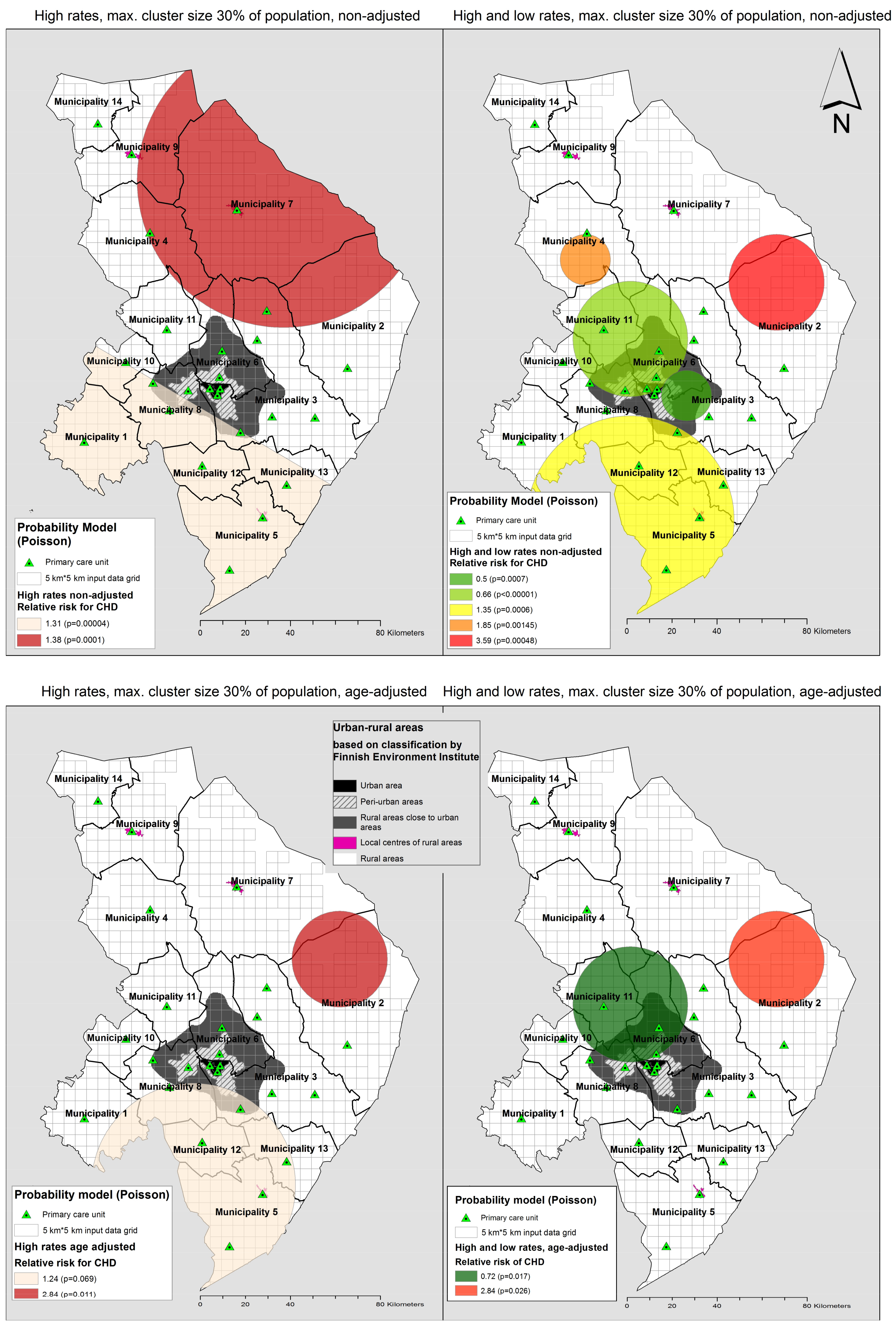
3.1. Cumulative Incidence of CHD with ACS and/or Invasive Treatment
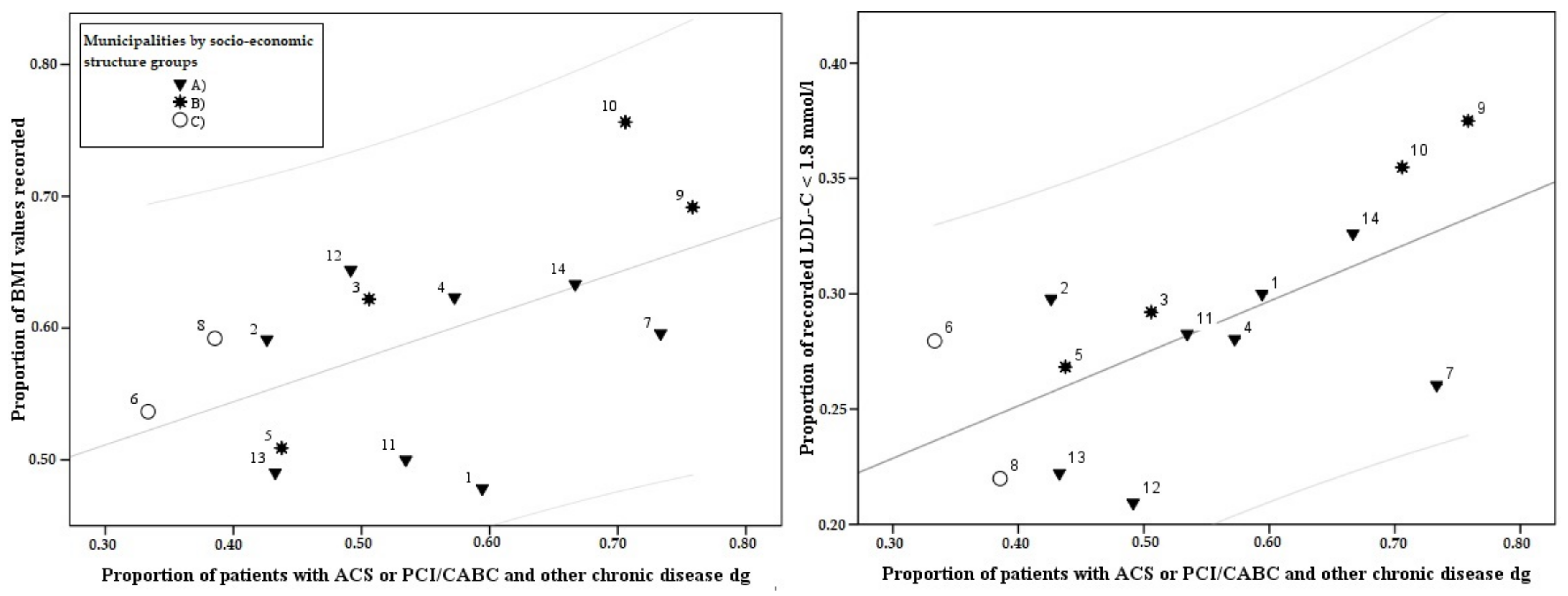
3.2. Recording Activity
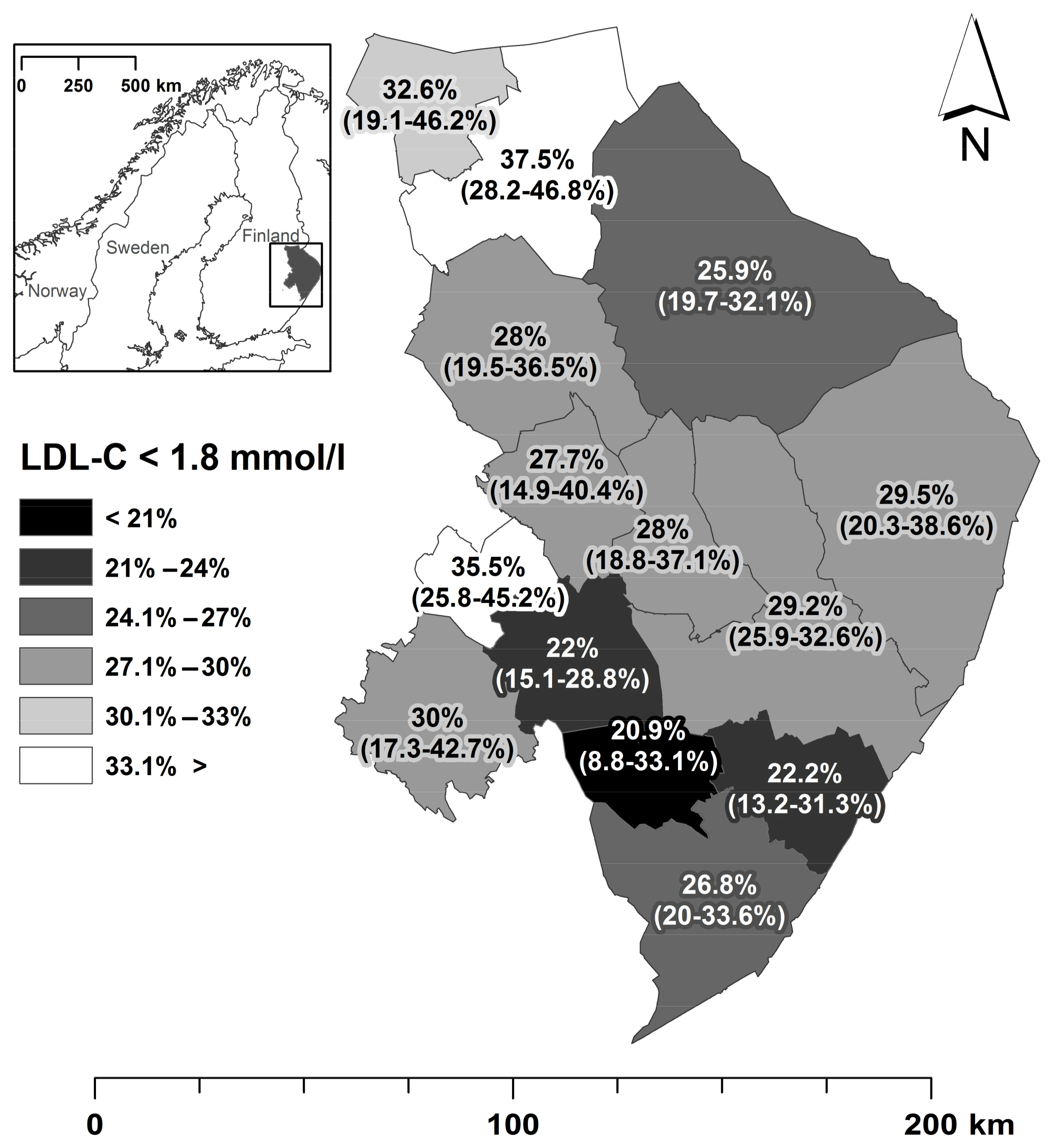
3.3. Attainment of Treatment Targets
4. Discussion
4.1. Summary of Findings
4.2. Incidence Rates
4.3. Recording Activity
4.4. Risk Factors/Attainment of Treatment Targets
4.5. Multimorbidity
4.6. Practical Usage of This Study
4.7. Strengths and Limitations of This Study
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Kotseva, K.; Wood, D.; De Bacquer, D.; De Backer, G.; Ryden, L.; Jennings, C.; Gyberg, V.; Amouyel, P.; Bruthans, J.; Castro Conde, A.; et al. EUROASPIRE IV: A European Society of Cardiology Survey on the Lifestyle, Risk Factor and Therapeutic Management of Coronary Patients from 24 European Countries. Eur. J. Prev. Cardiol. 2016, 23, 636–648. [Google Scholar] [CrossRef] [PubMed]
- Diez Roux, A.V.; Merkin, S.S.; Arnett, D.; Chambless, L.; Massing, M.; Nieto, F.J.; Sorlie, P.; Szklo, M.; Tyroler, H.A.; Watson, R.L. Neighborhood of Residence and Incidence of Coronary Heart Disease. N. Engl. J. Med. 2001, 345, 99–106. [Google Scholar] [CrossRef] [PubMed]
- Chaikiat, A.; Li, X.; Bennet, L.; Sundquist, K. Neighborhood Deprivation and Inequities in Coronary Heart Disease among Patients with Diabetes Mellitus: A Multilevel Study of 334,000 Patients. Health Place 2012, 18, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Rhudy, J.P., Jr.; Alexandrov, A.W.; Hyrkas, K.E.; Jablonski-Jaudon, R.A.; Pryor, E.R.; Wang, H.E.; Bakitas, M.A. Geographic Access to Interventional Cardiology Services in One Rural State. Heart Lung 2016, 45, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Heuschmann, P.U.; Kircher, J.; Nowe, T.; Dittrich, R.; Reiner, Z.; Cifkova, R.; Malojcic, B.; Mayer, O.; Bruthans, J.; Wloch-Kopec, D.; et al. Control of Main Risk Factors After Ischaemic Stroke Across Europe: Data from the Stroke-Specific Module of the EUROASPIRE III Survey. Eur. J. Prev. Cardiol. 2015, 22, 1354–1362. [Google Scholar] [CrossRef] [PubMed]
- Kotseva, K.; De Bacquer, D.; Jennings, C.; Gyberg, V.; De Backer, G.; Rydén, L.; Amouyel, P.; Bruthans, J.; Cifkova, R.; Deckers, J.W.; et al. Time Trends in Lifestyle, Risk Factor Control, and use of Evidence-Based Medications in Patients with Coronary Heart Disease in Europe: Results from 3 EUROASPIRE Surveys, 1999–2013. Glob. Heart 2017, 12, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Kauffman, A.B.; Olson, K.L.; Youngblood, M.L.; Zadvorny, E.B.; Delate, T.; Merenich, J.A. Clinical Pharmacy Cardiac Risk Service Study Group. Attainment of Low-Density Lipoprotein Cholesterol Goals in Coronary Artery Disease. J. Clin. Lipidol. 2010, 4, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Ho, L.; Yin, W.; Chuang, S.; Tseng, W.; Wu, Y.; Hsieh, I.; Lin, T.; Li, Y.; Huang, L.; Wang, K.; et al. Determinants for Achieving the LDL-C Target of Lipid Control for Secondary Prevention of Cardiovascular Events in Taiwan. PLoS ONE 2015, 10, e0116513. [Google Scholar] [CrossRef] [PubMed]
- Jones, P.H.; Nair, R.; Thakker, K.M. Prevalence of Dyslipidemia and Lipid Goal Attainment in Statin-Treated Subjects from 3 Data Sources: A Retrospective Analysis. J. Am. Heart Assoc. 2012, 1, e001800. [Google Scholar] [CrossRef] [PubMed]
- Doherty, P.; Petre, C.; Onion, N.; Harrison, A.; Dale, V.; Fell, J.; Cardy, K.; Tang, L. The National Audit of Cardiac Rehabilitation Annual Statistical Report 2015; British Heart Foundation: London, UK, 2015. [Google Scholar]
- De Smedt, D.; De Bacquer, D.; De Sutter, J.; Dallongeville, J.; Gevaert, S.; De Backer, G.; Bruthans, J.; Kotseva, K.; Reiner, Z.; Tokgozoglu, L.; et al. The Gender Gap in Risk Factor Control: Effects of Age and Education on the Control of Cardiovascular Risk Factors in Male and Female Coronary Patients the EUROASPIRE IV Study by the European Society of Cardiology. Int. J. Cardiol. 2016, 209, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Murphy, E.; Vellinga, A.; Byrne, M.; Cupples, M.E.; Murphy, A.W.; Buckley, B.; Smith, S.M. Primary Care Organisational Interventions for Secondary Prevention of Ischaemic Heart Disease: A Systematic Review and Meta-Analysis. Br. J. Gen. Pract. 2015, 65, e460–e468. [Google Scholar] [CrossRef] [PubMed]
- Hawkes, A.L.; Patrao, T.A.; Atherton, J.; Ware, R.S.; Taylor, C.B.; O’Neil, A.; Foreman, R.; Oldenburg, B.F. Effect of a Telephone-Delivered Coronary Heart Disease Secondary Prevention Program (Proactive Heart) on Quality of Life and Health Behaviours: Primary Outcomes of a Randomised Controlled Trial. Int. J. Behav. Med. 2013, 20, 413–424. [Google Scholar] [CrossRef] [PubMed]
- Casey, J.A.; Schwartz, B.S.; Stewart, W.F.; Adler, N.E. Using Electronic Health Records for Population Health Research: A Review of Methods and Applications. Annu. Rev. Public Health 2016, 37, 61–81. [Google Scholar] [CrossRef] [PubMed]
- Berlina, A.; Wang, S.; Greve Harbo, L.; Norlén, G.; Rasmussen, R.O. Nordregio Policy Brief. Nordic-Baltic Demographic Vulnerability Assessment at Municipal Level. Available online: http://www.nordregio.se/en/Publications/Publications-2016/Nordic-Baltic-Demographic-Vulnerability-Assessment-at-municipal-level-/ (accessed on 10 April 2018).
- Toivakka, M.; Laatikainen, T.; Kumpula, T.; Tykkylainen, M. Do the Classification of Areas and Distance Matter to the Assessment Results of Achieving the Treatment Targets among Type 2 Diabetes Patients? Int. J. Health Geogr. 2015, 14, 27. [Google Scholar] [CrossRef] [PubMed]
- Statistics Finland. Population Structure Population by Sex and Area 31.12.2015 and Increase of Population. Available online: http://www.stat.fi/til/vaerak/index_en.html (accessed on 25 September 2017).
- Kulldorff, M. A Spatial Scan Statistic. Commun. Statist. Theory Methods 1997, 26, 1481–1496. [Google Scholar] [CrossRef]
- Chen, J.; Roth, R.E.; Naito, A.T.; Lengerich, E.J.; MacEachren, A.M. Geovisual Analytics to Enhance Spatial Scan Statistic Interpretation: An Analysis of U.S. Cervical Cancer Mortality. Int. J. Health Geographics 2008, 7, 57. [Google Scholar] [CrossRef] [PubMed]
- Niemelä, K.; Vikman, S.; Kettunen, R.; Kuisma, M.; Miettinen, H.; Niemelä, M.; Pietilä, M.; Puurunen, M.; Tierala, I.; Uusitalo, L.; et al. Current Care Guidelines: Acute Coronary Syndrome: Unstable Angina and Myocardial Infarction without ST Elevation. 2014. Available online: http://www.kaypahoito.fi/web/kh/suositukset/suositus?id=hoi04058 (accessed on 15 September 2015).
- Tikkanen, M.J.; Syvänne, M.; Kesäniemi, A.; Ketola, E.; Kovalainen, P.; Kukkonen-Harjula, K.; Laatikainen, T.; Salo, M.T.; Schwalb, U.; Strandberg, T.; et al. Current Care Guidelines: Dyslipidaemias. 2013. Available online: http://www.kaypahoito.fi/web/english/guidelineabstracts/guideline?id=ccs00055 (accessed on 15 September 2015).
- Jula, A.; Kantola, I.; Korhonen, P.; Lehto, S.; Mervaala, E.; Metsärinne, K.; Strandberg, T.; Syvänne, M.; Tikkanen, I. Current Care Guidelines: Hypertension. 2014. Available online: http://www.kaypahoito.fi/web/english/ guidelineabstracts/guideline?id=ccs00014 (accessed on 15 September 2015).
- Sherman, R.L.; Henry, K.A.; Tannenbaum, S.L.; Feaster, D.J.; Kobetz, E.; Lee, D.J. Applying Spatial Analysis Tools in Public Health: An Example using SaTScan to Detect Geographic Targets for Colorectal Cancer Screening Interventions. Prev. Chronic Dis. 2014, 11, E41. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Salomaa, V.; Niemela, M.; Miettinen, H.; Ketonen, M.; Immonen-Raiha, P.; Koskinen, S.; Mahonen, M.; Lehto, S.; Vuorenmaa, T.; Palomaki, P.; et al. Relationship of Socioeconomic Status to the Incidence and Prehospital, 28-Day, and 1-Year Mortality Rates of Acute Coronary Events in the FINMONICA Myocardial Infarction Register Study. Circulation 2000, 101, 1913–1918. [Google Scholar] [CrossRef] [PubMed]
- Lahelma, E.; Palosuo, H.; Koskinen, S. Terveyden Eriarvoisuus Suomessa. Sosioekonomisten Terveyserojen Muutokset 1980–2005; Publications of the Ministry of Social Affairs and Health: Helsinki, Finland, 2007. [Google Scholar]
- Saposnik, G.; Goodman, S.G.; Leiter, L.A.; Yan, R.T.; Fitchett, D.H.; Bayer, N.H.; Casanova, A.; Langer, A.; Yan, A.T. Guidelines-Oriented Approach to Lipid-Lowering (GOALL) Registries Investigators. Applying the Evidence: Do Patients with Stroke, Coronary Artery Disease, Or both Achieve Similar Treatment Goals? Stroke 2009, 40, 1417–1424. [Google Scholar] [CrossRef] [PubMed]
- Tan, Y.Y.; Gast, G.C.; van der Schouw, Y.T. Gender Differences in Risk Factors for Coronary Heart Disease. Maturitas 2010, 65, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Chuang, S.Y.; Fang, C.C.; Huang, L.C.; Hsieh, I.C.; Pan, W.H.; Yeh, H.I.; Wu, C.C.; Yin, W.H.; Chen, J.W. Gender Disparities in Optimal Lipid Control among Patients with Coronary Artery Disease. J. Atheroscler. Thromb. 2014, 21 (Suppl. 1), S20–S28. [Google Scholar] [CrossRef] [PubMed]
- Kotseva, K.; Wood, D.; De Backer, G.; De Bacquer, D.; Pyorala, K.; Keil, U.; EUROASPIRE Study Group. EUROASPIRE III: A Survey on the Lifestyle, Risk Factors and use of Cardioprotective Drug Therapies in Coronary Patients from 22 European Countries. Eur. J. Cardiovasc. Prev. Rehabil. 2009, 16, 121–137. [Google Scholar] [CrossRef] [PubMed]
- Paulsen, M.S.; Andersen, M.; Munck, A.P.; Larsen, P.V.; Hansen, D.G.; Jacobsen, I.A.; Larsen, M.L.; Christensen, B.; Sondergaard, J. Socio-Economic Status Influences Blood Pressure Control Despite Equal Access to Care. Fam. Pract. 2012, 29, 503–510. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Laatikainen, T.; Jula, A.; Kastarinen, M.; Salomaa, V.; Borodulin, K.; Harald, K.; Peltonen, M.; Jousilahti, P.; Vartiainen, E. Blood Pressure Levels and Therapeutic Balance in FINRISK Study Areas in 1982–2012. Finnish Med. J. 2013, 68, 1803–1809. [Google Scholar]
- Statistical Information on Welfare and Health in Finland. Available online: www.goo.gl/URVr8a (accessed on 10 December 2017).
- Prugger, C.; Wellmann, J.; Heidrich, J.; De Bacquer, D.; De Backer, G.; Perier, M.C.; Empana, J.P.; Reiner, Z.; Fras, Z.; Jennings, C.; et al. Readiness for Smoking Cessation in Coronary Heart Disease Patients Across Europe: Results from the EUROASPIRE III Survey. Eur. J. Prev. Cardiol. 2015, 22, 1212–1219. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hiscock, R.; Bauld, L.; Amos, A.; Fidler, J.A.; Munafò, M. Socioeconomic Status and Smoking: A Review. Ann. N. Y. Acad. Sci. 2012, 1248, 107–123. [Google Scholar] [CrossRef] [PubMed]
- McPhail, S.M. Multimorbidity in Chronic Disease: Impact on Health Care Resources and Costs. Risk Manag. Healthc. Policy 2016, 9, 143–156. [Google Scholar] [CrossRef] [PubMed]
- Sikio, M.; Tykkylainen, M.; Tirkkonen, H.; Kekalainen, P.; Dunbar, J.; Laatikainen, T. Type 2 Diabetes Care in North Karelia Finland: Do Area-Level Socio-Economic Factors Affect Processes and Outcomes? Diabetes Res. Clin. Pract. 2014, 106, 496–503. [Google Scholar] [CrossRef] [PubMed]
- Laraia, B.A.; Karter, A.J.; Warton, E.M.; Schillinger, D.; Moffet, H.H.; Adler, N. Place Matters: Neighborhood Deprivation and Cardiometabolic Risk Factors in the Diabetes Study of Northern California (DISTANCE). Soc. Sci. Med. 2012, 74, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Ford, D.R.; Knight, A.W. The Australian Primary Care Collaboratives: An Australian General Practice Success Story. Med. J. Aust. 2010, 193, 90–91. [Google Scholar] [PubMed]
- Viitanen, J.; Hypponen, H.; Laaveri, T.; Vanska, J.; Reponen, J.; Winblad, I. National Questionnaire Study on Clinical ICT Systems Proofs: Physicians Suffer from Poor Usability. Int. J. Med. Inform. 2011, 80, 708–725. [Google Scholar] [CrossRef] [PubMed]
- Dixon, A.; Khachatryan, A.; Wallace, A.; Peckham, S.; Boyce, T.; Gillam, S. The Quality and Outcomes Framework (QOF): Does It Reduce Health Inequalities; Final Report; NIHR Service Delivery and Organisation Programme: Southampton, UK, 2010. [Google Scholar]
- Fortin, M.; Haggerty, J.; Almirall, J.; Bouhali, T.; Sasseville, M.; Lemieux, M. Lifestyle Factors and Multimorbidity: A Cross Sectional Study. BMC Public Health 2014, 14, 686. [Google Scholar] [CrossRef] [PubMed]
- De Smedt, D.; Clays, E.; Annemans, L.; Doyle, F.; Kotseva, K.; Pajak, A.; Prugger, C.; Jennings, C.; Wood, D.; De Bacquer, D. Health Related Quality of Life in Coronary Patients and Its Association with their Cardiovascular Risk Profile: Results from the EUROASPIRE III Survey. Int. J. Cardiol. 2013, 168, 898–903. [Google Scholar] [CrossRef] [PubMed]
| Multimorbid Patients | Patient with ACS or PCI/CABG only | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Both Genders | Male | Female | Both Genders | Male | Female | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |
| Number of patients | 1348 | 53% | 845 | 51% | 503 | 55% | 1208 | 47% | 800 | 49% | 408 | 45% |
| Body mass index recorded * | 873 | 65% | 540 | 64% | 333 | 66% | 656 | 54% | 438 | 55% | 218 | 53% |
| HDL cholesterol recorded | 992 | 74% | 639 | 76% | 353 | 70% | 839 | 69% | 566 | 71% | 273 | 67% |
| LDL cholesterol recorded | 1059 | 79% | 667 | 79% | 392 | 78% | 896 | 74% | 598 | 75% | 298 | 73% |
| Triglycerides recorded | 984 | 73% | 638 | 76% | 346 | 69% | 819 | 68% | 551 | 69% | 268 | 66% |
| Blood pressure recorded | 866 | 64% | 517 | 61% | 349 | 69% | 558 | 46% | 346 | 43% | 212 | 52% |
| Smoking status recorded ** | 888 | 66% | 541 | 64% | 347 | 69% | 539 | 45% | 357 | 45% | 182 | 45% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Repo, T.; Tykkyläinen, M.; Mustonen, J.; Rissanen, T.T.; Ketonen, M.; Toivakka, M.; Laatikainen, T. Outcomes of Secondary Prevention among Coronary Heart Disease Patients in a High-Risk Region in Finland. Int. J. Environ. Res. Public Health 2018, 15, 724. https://doi.org/10.3390/ijerph15040724
Repo T, Tykkyläinen M, Mustonen J, Rissanen TT, Ketonen M, Toivakka M, Laatikainen T. Outcomes of Secondary Prevention among Coronary Heart Disease Patients in a High-Risk Region in Finland. International Journal of Environmental Research and Public Health. 2018; 15(4):724. https://doi.org/10.3390/ijerph15040724
Chicago/Turabian StyleRepo, Teppo, Markku Tykkyläinen, Juha Mustonen, Tuomas T. Rissanen, Matti Ketonen, Maija Toivakka, and Tiina Laatikainen. 2018. "Outcomes of Secondary Prevention among Coronary Heart Disease Patients in a High-Risk Region in Finland" International Journal of Environmental Research and Public Health 15, no. 4: 724. https://doi.org/10.3390/ijerph15040724
APA StyleRepo, T., Tykkyläinen, M., Mustonen, J., Rissanen, T. T., Ketonen, M., Toivakka, M., & Laatikainen, T. (2018). Outcomes of Secondary Prevention among Coronary Heart Disease Patients in a High-Risk Region in Finland. International Journal of Environmental Research and Public Health, 15(4), 724. https://doi.org/10.3390/ijerph15040724




