Exposure to Suicide in High Schools: Impact on Serious Suicidal Ideation/Behavior, Depression, Maladaptive Coping Strategies, and Attitudes toward Help-Seeking
Abstract
:1. Introduction
2. Materials and Methods
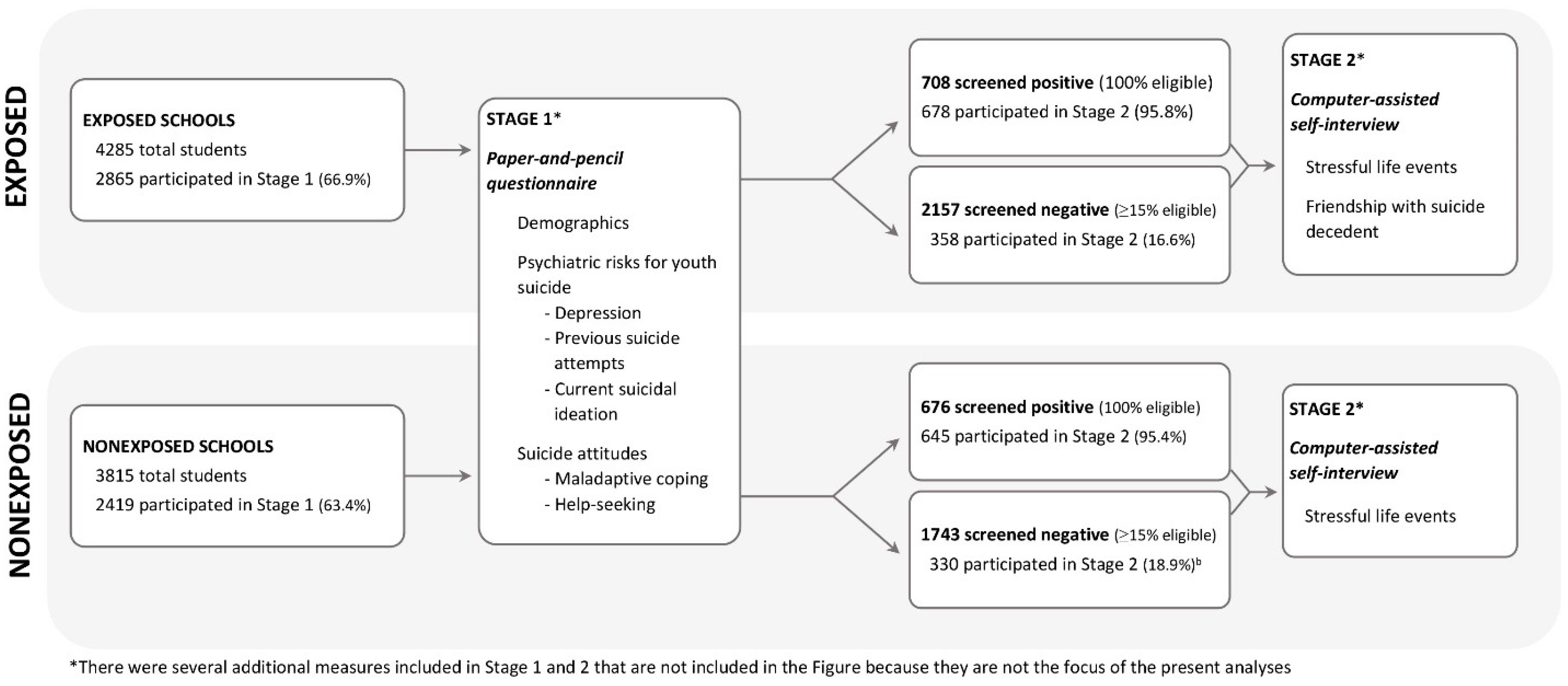
2.1. Sample
2.2. Procedure
2.3. Measures
- (1)
- How well did you know him or her? (0 = not at all; 1 = acquaintances; 2 = friends, but not close friends; 3 = close friends, current boyfriend or girlfriend, ex-boyfriend or girlfriend);
- (2)
- How often did you see him or her at school? This was a composite (highest response code) of two questions: “How often did you see him or her in class?” and “How often did you see him or her at school, other than in class?” (0 = never; 1 = less than once a week; 2 = once to four times a week; 3 = daily);
- (3)
- How often did you see him after school or talk on the phone? This was a composite of “How often did you see him or her after school or on weekends?” and “How often did you talk to him or her on the phone?” (0 = never; 1 = less than once a week; 2 = once to four times a week; 3 = daily);
- (4)
- To what extent did you confide in each other? This was a composite of “Was he or she somebody in whom you could confide?” and “Were you someone in whom he or she confided?” (0 = Not at all; 2 = somewhat; 3 = very much so).
2.4. Analytic Strategy
3. Results
3.1. Association of Exposure with Psychological Morbidity and Coping/Help-Seeking Attitudes
3.2. Association of Negative Life Events with Psychological Morbidity and Coping/Help-Seeking Attitudes
3.3. Association of Friendship with the Suicide Decedent with Psychological Morbidity and Coping/Help-Seeking Attitudes
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Centers for Disease Control and Prevention; National Center for Health Statistics. Health, United States, 2016: With Chartbook on Long-Term Trends in Health; National Center for Health Statistics: Hyattsville, MD, USA. Available online: https://www.cdc.gov/nchs/data/hus/hus16.pdf (accessed on 8 August 2017).
- Wrobleski, A. Suicide Survivors: A Guide for Those Left behind, 1st ed.; Afterwords Publishing: Minneapolis, MN, USA, 1991; p. 49. ISBN 0935585044. [Google Scholar]
- Cerel, J. We Are All Connected in Suicidology: The Continuum of “Survivorship”. Presented at the 48th Annual Conference of the American Association of Suicidology, Atlanta, GA, USA, 18 April 2015; Available online: http://www.suicidology.org/Portals/14/docs/Resources/FactSheets/2016/2016datapgsv1b.pdf?ver=2018-01-15-211057-387 (accessed on 15 December 2017).
- Centers for Disease Control and Prevention. Web-Based Injury Statistics Query and Reporting System. Available online: www.cdc.gov/injury/wisqars (accessed on 30 January 2018).
- Shneidman, E. On the Nature of Suicide, 1st ed.; Jossey-Bass: San Francisco, CA, USA, 1969; pp. 1–30. ISBN 978-0-87-589051-7. [Google Scholar]
- Insel, B.J.; Gould, M.S. Impact of modeling on adolescent suicidal behavior. Psychiatr. Clin. N. Am. 2008, 31, 293–316. [Google Scholar] [CrossRef] [PubMed]
- Abrutyn, S.; Mueller, A.S. Are suicidal behaviors contagious in adolescence? Using longitudinal data to examine suicide suggestion. Am. Sociol. Rev. 2014, 79, 211–227. [Google Scholar] [CrossRef] [PubMed]
- Baller, R.D.; Richardson, K.K. The “dark side” of the strength of weak ties: The diffusion of suicidal thoughts. J. Health Soc. Behav. 2009, 50, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Feigelman, W.; Gorman, B.S. Assessing the effects of peer suicide on youth suicide. Suicide Life Threat. Behav. 2008, 38, 181–194. [Google Scholar] [CrossRef] [PubMed]
- Ho, T.; Leung, P.W.; Hung, S.; Lee, C.; Tang, C. The mental health of the peers of suicide completers and attempters. J. Child Psychol. Psychiatry 2000, 41, 301–309. [Google Scholar] [CrossRef] [PubMed]
- Randall, J.R.; Nickel, N.C.; Colman, I. Contagion from peer suicidal behaviour in a representative sample of American adolescents. J. Affect. Disord. 2015, 186, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Swanson, S.A.; Colman, I. Association between exposure to suicide and suicidality outcomes in youth. CMAJ 2013, 185, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Cerel, J.; Maple, M.; van de Venne, J.; Moore, M.; Flaherty, C.; Brown, M. Exposure to suicide in the community: Prevalence and correlates in one U.S. state. Public Health Rep. 2016, 131, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Cerel, J.; Maple, M.; van de Venne, J.; Brown, M.; Moore, M.; Flaherty, C. Suicide exposure in the population: Perceptions of impact and closeness. Suicide Life Threat. Behav. 2017, 47, 696–798. [Google Scholar] [CrossRef] [PubMed]
- Brent, D.A.; Kerr, M.M.; Goldstein, C.; Bozigar, J.; Wartella, M.; Allan, M.J. An outbreak of suicide and suicidal behavior in a high school. J. Am. Acad. Child Adolesc. Psychiatry 1989, 28, 918–924. [Google Scholar] [CrossRef] [PubMed]
- Cox, G.R.; Bailey, E.; Jorm, A.F.; Reavley, N.J.; Templer, K.; Parker, A.; Rickwood, D.; Bhar, S.; Robinson, J. Development of suicide postvention guidelines for secondary schools: A Delphi study. BMC Public Health 2016, 16, 180. [Google Scholar] [CrossRef] [PubMed]
- Cash, S.J.; Bridge, J.A. Epidemiology of youth suicide and suicidal behavior. Curr. Opin. Pediatr. 2009, 21, 613–619. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A. Manual for the Beck Depression Inventory; Psychological Corporation: San Antonio, TX, USA, 1993. [Google Scholar]
- Tarter, R.E.; Hegedus, A.M. The Drug Use Screening Inventory: Its applications in the evaluation and treatment of alcohol and other drug abuse. Alcohol Health Res. World 1991, 15, 65–75. [Google Scholar]
- Strober, M.; Green, J.; Carlson, G. Utility of the Beck Depression Inventory with psychiatrically hospitalized adolescents. J. Consult. Clin. Psychol. 1981, 49, 482–483. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, D.; Fisher, P.; Lucas, C.P.; Dulcan, M.K.; Schwab-Stone, M.E. NIMH Diagnostic Interview Schedule for Children, version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 2000, 39, 28–38. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, D.; Scott, M.; Wilcox, H. Screening high-school students for suicide risk. J. Am. Acad. Child Adolesc. Psychiatry 2004, 43, 71–79. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.S.; King, R.; Greenwald, S.; Fisher, P.; Schwab-Stone, M.; Kramer, R.; Flisher, A.J.; Goodman, S.; Canino, G.; Shaffer, D. Psychopathology associated with suicidal ideation and attempts among children and adolescents. J. Am. Acad. Child Adolesc. Psychiatry 1998, 37, 915–923. [Google Scholar] [CrossRef] [PubMed]
- Shaffer, D.; Garland, A.; Vieland, V.; Underwood, M.; Busner, C. The impact of curriculum-based suicide prevention programs for teenagers. J. Am. Acad. Child Adolesc. Psychiatry 1991, 30, 588–596. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.S.; Velting, D.; Kleinman, M.; Lucas, C.; Thomas, J.G.; Chung, M. Teenagers’ attitudes about coping strategies and help-seeking behavior for suicidality. J. Am. Acad. Child Adolesc. Psychiatry 2004, 43, 1124–1133. [Google Scholar] [CrossRef] [PubMed]
- Coddington, R.D. Coddington Life Events Scales (CLES): Technical Manual; Multi-Health Systems Inc.: Toronto, ON, Canada, 1999. [Google Scholar]
- SAS Institute Inc. SAS, Version 9.4, SAS Institute Inc.: Cary, NC, USA, 2013.
- IBM Corp. IBM SPSS Statistics for Windows, Version 23, IBM Corp.: Armonk, NY, USA, 2015.
- Cerel, J.; McIntosh, J.L.; Neimeyer, R.A.; Maple, M.; Marshall, M. The continuum of “survivorship”: Definitional issues in the aftermath of suicide. Suicide Life Threat. Behav. 2014, 44, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Brent, D.A.; Perper, J.A.; Moritz, G.; Baugher, M.; Roth, C.; Balach, L.; Schweers, J. Stressful life events, psychopathology, and adolescent suicide: A case control study. Suicide Life Threat. Behav. 1993, 23, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Gould, M.S.; Fisher, P.; Parides, M.; Flory, M.; Shaffer, D. Psychosocial risk factors of child and adolescent completed suicide. Arch. Gen. Psychiatry 1996, 53, 1155–1162. [Google Scholar] [CrossRef] [PubMed]
- Brent, D.A.; Moritz, G.; Bridge, J.; Perper, J.; Canobbio, R. Long-term impact of exposure to suicide: A three-year controlled follow-up. J. Am. Acad. Child Adolesc. Psychiatry 1996, 35, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Lake, A.M.; Gould, M.S. Suicide clusters and suicide contagion. In A Concise Guide to Understanding Suicide: Epidemiology, Pathophysiology and Prevention, 1st ed.; Koslow, S.H., Ruiz, P., Nemeroff, C.B., Eds.; Cambridge University Press: Cambridge, UK, 2014; pp. 52–61. ISBN 978-1-10-703323-8. [Google Scholar]
- Joiner, T.E. Contagion of suicidal symptoms as a function of assortative relating and shared relationship stress in college roommates. J. Adolesc. 2003, 26, 495–504. [Google Scholar] [CrossRef]
- Gould, M.S. Suicide clusters and media exposure. In Suicide over the Life Cycle: Risk Factors, Assessment, and Treatment of Suicidal Patients; Blumenthal, S.J., Kupfer, D.J., Eds.; American Psychiatric Press: Washington, DC, USA, 1990; pp. 517–532. ISBN 978-0-88-048307-0. [Google Scholar]
- Haw, C.; Hawton, K.; Niedzwiedz, C.; Platt, S. Suicide clusters: A review of risk factors and mechanisms. Suicide Life Threat. Behav. 2013, 43, 97–108. [Google Scholar] [CrossRef] [PubMed]
- Cutler, D.M.; Glaesen, E.L.; Norberg, K.E. Explaining the rise in youth suicide. In Risky Behavior among Youths: An Economic Analysis; Gruber, J., Ed.; University of Chicago Press: Chicago, IL, USA, 2001; pp. 219–269. ISBN 978-0-22-631013-8. [Google Scholar]
- Hallfors, D.; Brodish, P.H.; Khatapoush, S.; Sanchez, V.; Cho, H.; Steckler, A. Feasibility of screening adolescents for suicide risk in “real-world” high school settings. Am. J. Public Health 2006, 96, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Peña, J.B.; Caine, E.D. Screening as an approach for adolescent suicide prevention. Suicide Life Threat. Behav. 2006, 36, 614–637. [Google Scholar] [CrossRef] [PubMed]
- Eckert, T.L.; Miller, D.N.; DuPaul, G.J.; Riley-Tillman, T.C. Adolescent suicide prevention: School psychologists’ acceptability of school-based programs. Sch. Psych. Rev. 2003, 32, 57–76. [Google Scholar]
- Miller, D.N.; Eckert, T.L.; DuPaul, G.J.; White, G.P. Adolescent suicide prevention: Acceptability of school-based programs among secondary school principals. Suicide Life Threat. Behav. 1999, 29, 72–85. [Google Scholar] [CrossRef] [PubMed]
- Scherff, A.R.; Eckert, T.L.; Miller, D.N. Youth suicide prevention: A survey of public school superintendents’ acceptability of school-based programs. Suicide Life Threat. Behav. 2005, 35, 154–169. [Google Scholar] [CrossRef] [PubMed]
- Headspace School Support Suicide Postvention Toolkit. Available online: http://www.Headspace.org.au/assets/School-Support/Compressed-Postvention-Toolkit-May-2012-FA2-LR.pdf (accessed on 22 January 2018).
- Wyman, P.A.; Brown, C.H.; LoMurray, M.; Schmeelk-Cone, K.; Petrova, M.; Yu, Q.; Walsh, E.; Tu, X.; Wang, W. An outcome evaluation of the Sources of Strength suicide prevention program delivered by adolescent peer leaders in high schools. Am. J. Public Health 2010, 100, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
| Outcome Measures | Exposed Schools (n = 2865) n % | Non-Exposed Schools (n = 2419) n % | OR or B (95% CI) | p |
|---|---|---|---|---|
| Serious suicidal ideation/Behavior | 199, 6.9% | 150, 6.2% | 1.18 (0.85–1.64) | 0.299 |
| Depression (>BDI cutoff) | 279, 9.8% | 232, 9.7% | 1.02 (0.69–1.50) | 0.930 |
| Maladaptive Coping Scale a mean (SD) | 0.699 (1.06) | 0.863 (1.17) | −0.156 (−0.316–−0.01) | 0.044 |
| -People should be able to handle their own problems without outside help. | 248, 12.6% | 411, 17.0% | 0.71 (0.57–0.87) | 0.005 |
| -Drugs and alcohol are a good way to help someone stop feeling depressed. | 162, 8.2% | 258, 10.7% | 0.72 (0.55–0.94) | 0.022 |
| -If you are depressed, it is a good idea to keep these feelings to yourself. | 107, 5.4% | 183, 7.6% | 0.77 (0.54–1.11) | 0.137 |
| -Suicide is a possible solution to problems b | 217/1916, 11.3% | 299/2343, 12.8% | 0.93 (0.70–1.23) | 0.549 |
| -I would talk to my friend without getting anyone else’s help. | 410, 20.8% | 581, 24.0% | 0.82 (0.64–1.05) | 0.094 |
| -I wouldn’t take it seriously. | 94, 4.8% | 167, 6.9% | 0.75 (0.54–1.03) | 0.069 |
| -I would keep it a secret. | 135, 6.9% | 187, 7.7% | 0.93 (0.63–1.36) | 0.659 |
| Help-seeking Scale a mean (SD) | 3.01 (1.41) | 2.83 (1.52) | 0.175 (−0.01–0.36) | 0.062 |
| -Tell my friend to see a mental health professional | 1405, 71.4% | 1703, 70.4% | 1.02 (0.84–1.25) | 0.796 |
| -Tell my friend to call a hotline. | 880, 44.7% | 1069, 44.2% | 1.09 (0.69–1.71) | 0.687 |
| -Tell my friend to talk to his/her parents. | 1354, 68.8% | 1520, 62.8% | 1.26 (0.99–1.61) | 0.062 |
| -Talk to an adult about my friend. | 1457, 74.0% | 1618, 66.9% | 1.45 (1.13–1.85) | 0.008 |
| -Get advice from another friend. | 830, 42.2% | 944, 39.0% | 1.13 (0.82–1.57) | 0.403 |
| Main Effects and Interaction Terms | Serious Suicidal Ideation/Behavior | Depression | Maladaptive Coping Strategies | Adaptive Attitudes toward Help-Seeking | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | B (95% CI) | p | B (95% CI) | p | |
| School exposure status | 0.818 (0.522–1.283) | 0.344 | 0.905 (0.560–1.462) | 0.653 | −0.147 (−0.388–0.094) | 0.213 | 0.044 (−0.271–0.360) | 0.767 |
| Negative Life Events | 1.005 (1.004–1.006) | <0.0001 | 1.005 (1.004–1.006) | <0.0001 | 0.002 (0.001–0.003) | <0.0001 | –0.001 (−0.002–−0.001) | 0.001 |
| Interaction: School exposure by negative events | 1.002 (1.001–1.004) | 0.007 | 1.001 (0.999–1.003) | 0.292 | 0.001 (−0.000–0.002) | 0.272 | 0.001 (−0.001–0.002) | 0.342 |
| Friendship Items | Serious Suicidal Ideation/Behavior + | Depression + | Maladaptive Coping Strategies ++ | Adaptive Attitudes toward Help-Seeking ++ | ||||
|---|---|---|---|---|---|---|---|---|
| n a | % a | n a | % a | Mean b | SD b | Mean b | SD b | |
| Friendship scale score + | ||||||||
| 0 (n = 867) | 56 | 6.42 | 65 | 7.58 | 0.51 | 0.95 | 2.92 | 1.49 |
| 1–4 (n = 1306) | 75 | 5.78 | 104 | 8.01 | 0.86 | 1.07 | 3.00 | 1.37 |
| 5–8 (n = 478) | 58 | 12.08 | 69 | 14.49 | 0.96 | 1.13 | 2.86 | 1.46 |
| 9–12 (n = 192) | 21 | 10.88 | 33 | 17.99 | 0.79 | 1.15 | 3.14 | 1.30 |
| How well did you know him/her? + | ||||||||
| Not at all (n = 1568) | 100 | 6.36 | 118 | 7.59 | 0.63 | 0.97 | 2.93 | 1.43 |
| Acquaintances (n = 790) | 61 | 7.67 | 85 | 10.80 | 1.01 | 1.19 | 3.08 | 1.37 |
| Friends, but not close friends (n = 410) | 43 | 10.51 | 51 | 12.51 | 0.76 | 1.03 | 2.82 | 1.51 |
| Close friends (n = 97) | 7 | 7.50 | 21 | 22.94 | 0.89 | 1.24 | 3.02 | 1.26 |
| How often did you see him/her in school? + | ||||||||
| Never (n = 938) | 59 | 6.27 | 68 | 7.31 | 0.57 | 1.02 | 2.98 | 1.45 |
| Less than once a week (n = 619) | 27 | 4.43 | 59 | 9.55 | 0.94 | 1.08 | 2.67 | 1.32 |
| Once to four times a week (n = 431) | 35 | 8.10 | 39 | 9.11 | 0.88 | 1.18 | 3.20 | 1.38 |
| Daily (n = 863) | 90 | 10.39 | 107 | 12.49 | 0.80 | 1.03 | 3.04 | 1.42 |
| How often did you see him or her after school or talk on the phone? + | ||||||||
| Never (n = 2167) | 135 | 6.24 | 174 | 8.11 | 0.72 | 1.03 | 2.96 | 1.41 |
| Less than once a week (n = 437) | 49 | 11.22 | 61 | 13.92 | 1.01 | 1.20 | 2.87 | 1.53 |
| Once to four times a week (n = 181) | 17 | 9.24 | 30 | 16.76 | 0.66 | 0.99 | 3.00 | 1.27 |
| Daily (n = 79) | 10 | 12.17 | 9 | 12.85 | 1.13 | 1.38 | 3.05 | 1.49 |
| To what extent did you confide in each other? + | ||||||||
| Not at all (n = 2402) | 151 | 6.29 | 194 | 8.15 | 0.72 | 1.04 | 2.95 | 1.42 |
| Somewhat (n = 313) | 49 | 15.69 | 57 | 18.14 | 0.97 | 1.18 | 2.89 | 1.36 |
| Very much (n = 99) | 8 | 8.45 | 16 | 16.82 | 0.87 | 1.31 | 3.20 | 1.44 |
| Friendship Items | Serious Suicidal Ideation/Behavior | Depression | Maladaptive Coping Strategies | Adaptive Attitudes toward Help-Seeking | ||||
|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p | OR (95% CI) | p | B (95% CI) | p | B (95% CI) | p | |
| Friendship scale | 1.11 (1.05–1.16) | <0.0001 | 1.14 + (1.09–1.20) | <0.001 | 0.04 (0.01–0.07) | 0.022 | 0.02 (−0.02–0.05) | 0.399 |
| How well did you know him/her? | ||||||||
| -Not at all (ref) | - | - | - | - | - | - | - | |
| -Acquaintances | 1.11 (0.77–1.59) | 0.581 | 1.44 (1.04–1.99) | 0.0030 | 0.37 (0.18–0.57) | 0.0002 | 0.10 (−0.16–0.36) | 0.448 |
| -Friends, but not close friends | 1.85 (1.19–2.87) | 0.006 | 2.20 (1.45–3.33) | 0.0002 | 0.12 (−0.13–0.37) | 0.354 | −0.10 (−0.42–0.23) | 0.558 |
| -Close friends | 1.12 (0.49–2.54) | 0.793 | 4.40 (2.49–7.79) | <0.0001 | 0.20 (−0.31–0.71) | 0.431 | 0.02 (−0.66–0.69) | 0.958 |
| How often did you see him/her in school? | 1.29 (1.12–1.49) | 0.0004 | 1.23 (1.08–1.39) | 0.0017 | 0.09 (0.01–0.17) | 0.020 | 0.06 (−0.03–0.14) | 0.208 |
| How often did you see him or her after school or talk on the phone? | 1.29 (1.08–1.55) | 0.0061 | 1.46 (1.24–1.72) | <0.0001 | 0.07 (−0.05–0.18) | 0.259 | 0.02 (−0.14–0.17) | 0.827 |
| To what extent did you confide in each other? | ||||||||
| -Not at all (ref) | - | - | - | - | - | - | - | - |
| -Somewhat | 2.68 (1.81–3.97) | <0.0001 | 2.63 (1.81–3.81) | <0.0001 | 0.22 (−0.05–0.49) | 0.112 | −0.01 (−0.36–0.34) | 0.960 |
| -A lot | 1.20 (0.56–2.57) | 0.643 | 2.24 (1.23–4.08) | 0.0086 | 0.08 (−0.37–0.54) | 0.722 | 0.25 (−0.35–0.85) | 0.415 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gould, M.S.; Lake, A.M.; Kleinman, M.; Galfalvy, H.; Chowdhury, S.; Madnick, A. Exposure to Suicide in High Schools: Impact on Serious Suicidal Ideation/Behavior, Depression, Maladaptive Coping Strategies, and Attitudes toward Help-Seeking. Int. J. Environ. Res. Public Health 2018, 15, 455. https://doi.org/10.3390/ijerph15030455
Gould MS, Lake AM, Kleinman M, Galfalvy H, Chowdhury S, Madnick A. Exposure to Suicide in High Schools: Impact on Serious Suicidal Ideation/Behavior, Depression, Maladaptive Coping Strategies, and Attitudes toward Help-Seeking. International Journal of Environmental Research and Public Health. 2018; 15(3):455. https://doi.org/10.3390/ijerph15030455
Chicago/Turabian StyleGould, Madelyn S., Alison M. Lake, Marjorie Kleinman, Hanga Galfalvy, Saba Chowdhury, and Alison Madnick. 2018. "Exposure to Suicide in High Schools: Impact on Serious Suicidal Ideation/Behavior, Depression, Maladaptive Coping Strategies, and Attitudes toward Help-Seeking" International Journal of Environmental Research and Public Health 15, no. 3: 455. https://doi.org/10.3390/ijerph15030455
APA StyleGould, M. S., Lake, A. M., Kleinman, M., Galfalvy, H., Chowdhury, S., & Madnick, A. (2018). Exposure to Suicide in High Schools: Impact on Serious Suicidal Ideation/Behavior, Depression, Maladaptive Coping Strategies, and Attitudes toward Help-Seeking. International Journal of Environmental Research and Public Health, 15(3), 455. https://doi.org/10.3390/ijerph15030455




