The Relationship between Infectious Diseases and Housing Maintenance in Indigenous Australian Households
Abstract
1. Introduction
A healthy home is a fundamental precondition of a healthy population. Important contributors to the current unsatisfactory living conditions include inadequate water and sewerage systems, waste collection, electricity and housing infrastructure (design, stock and maintenance). Children need to live in accommodation with adequate infrastructure conducive to good hygiene and study, and free of overcrowding.(‘Healthy Homes’, Australian National Indigenous Reform Agreement (2009) [1])
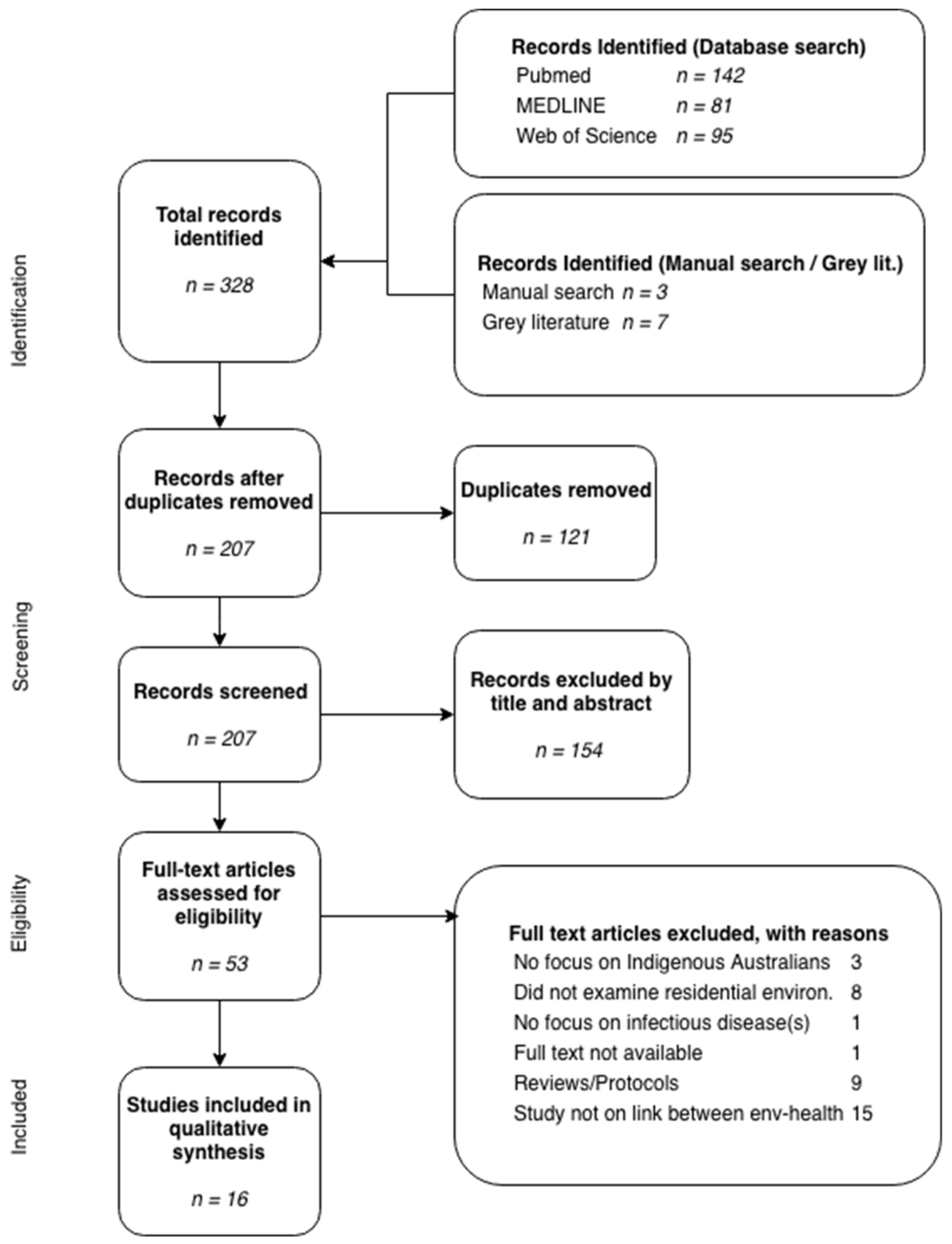
2. Materials and Methods
3. Results
3.1. Study Characteristics
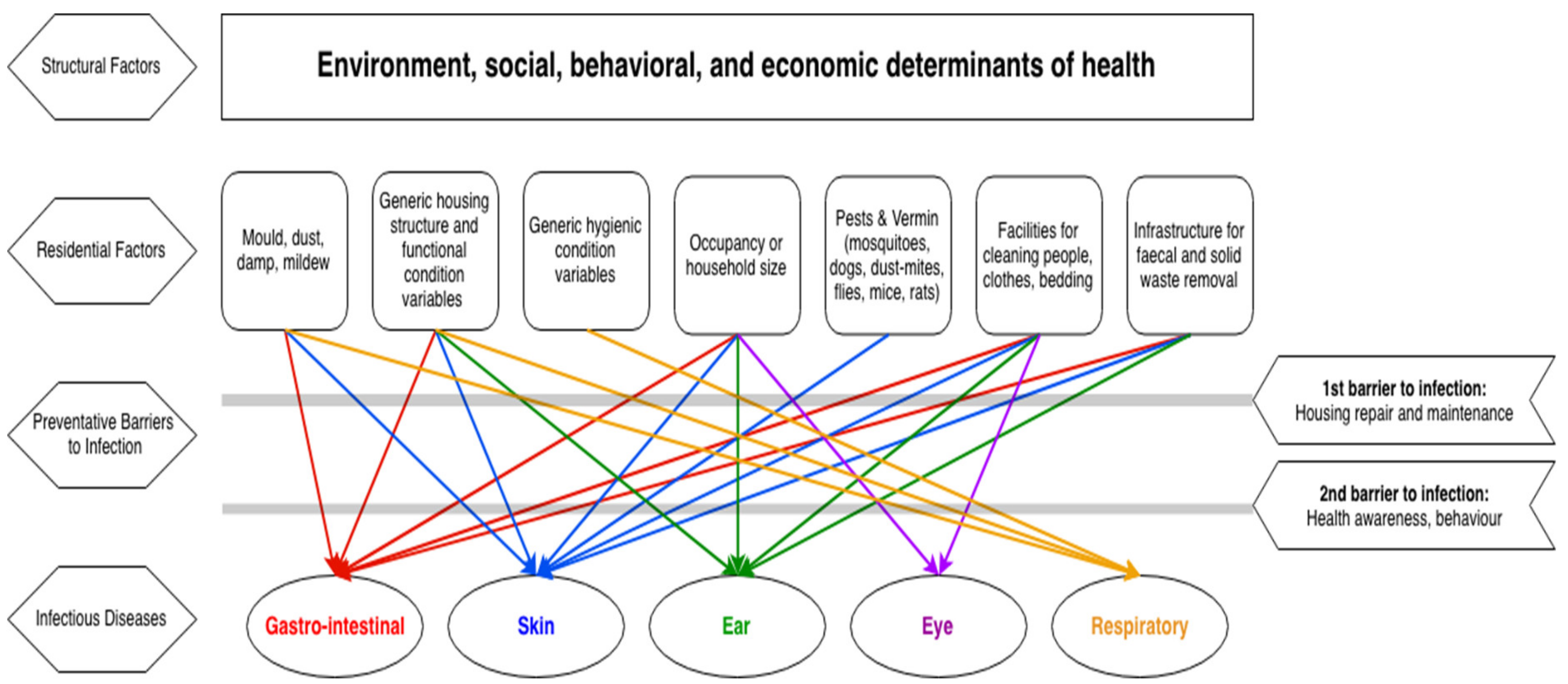
3.2. Housing Environment
3.3. Link between Housing and Infectious Disease
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- COAG. National Indigenous Reform Agreement (Closing the Gap); Council of Australian Governments: Canberra, Australia, 2009.
- APO NT. Sumission to the National Review of the National Partnership Agreement on Remote Indigenous Housing (NPARIH); Aboriginal Peak Organisations-Northern Territory (CLC, NLC, CAALAS, AMSANT and NAAJA): Darwin, Australia, 2017; Available online: http://www.amsant.org.au/apont/wp-content/uploads/2017/01/20170109-APO-NT-Submission-on-NPARIH-Remote-Housing-Review.pdf (accessed on 12 October 2017).
- Pholeros, P.; Rainow, S.; Torzillo, P. Housing for Health: Towards a Health Living Environment for Aboriginal Australia; Healthabitat: Sydney, Australia, 1993; Available online: http://www.healthabitat.com/the-healthy-living-practices (accessed on 8 May 2017).
- Healthabitat. Housing for Health–The Guide; Healthabitat: Sydney, Australia, 2013; Available online: http://www.housingforhealth.com/about/ (accessed on 11 October 2017).
- Browett, H.; Pearce, M.; Willis, E. Cost Implications of Hard Water on Health Hardware in Remote Indigenous Communities in the Central Desert Region of Australia. Int. Indig. Policy J. 2012, 3, 6. [Google Scholar] [CrossRef]
- CDC. Hygiene-Related Diseases; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2015. Available online: https://www.cdc.gov/healthywater/hygiene/disease/index.html (accessed on 12 October 2017).
- Foster, T. Unfinished business: Water, sanitation and hygiene in remote Indigenous communities in Australia’s Northern Territory. In Proceedings of the Water and Health, Chapel Hill, NC, USA, 16–20 October 2017. [Google Scholar]
- Lange, F.; Jones, K.; Ritte, R.; Brown, H.; Taylor, H. The impact of health promotion on trachoma knowledge, attitudes and practice (KAP) of staff in three work settings in remote Indigenous communities in the Northern Territory. PLoS Negl. Trop. Dis. 2017, 11, e0005503. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.M.; Birrell, A.L. Trachoma in remote Indigenous Australia: A review and public health perspective. Aust. N. Z. J. Public Health 2016, 40, S48–S52. [Google Scholar] [CrossRef] [PubMed]
- Department of Health. National Notifiable Diseases Surveillance System: Notification Rate of Shigellosis, received from State and Territory health authorities; Department of Health, Commonwealth of Australia: Canberra, Australia, 2018.
- AIHW. Aboriginal and Torres Strait Islander Health Performance Framework 2017: Supplementary Online Tables; Cat. no. WEB 170; Australian Institute of Health and Welfare: Canberra, Australia, 2017.
- National Trachoma Surveillance and Reporting Unit. Australian Trachoma Surveillance Report 2017; The Kirby Institute, UNSW: Sydney, Australia, 2018.
- DPMC. Closing the Gap Prime Minister’s Report 2017; Department of Prime Minister and Cabinet: Canberra, Australia, 2017.
- ABS. National Aboriginal and Torres Strait Islander Social Survey, 2014-15; Australian Bureau of Statistics: Canberra, Australia, 2016.
- Commonwealth of Australia. Remote Housing Review: A Review of the National Partnership Agreement on Remote Indigenous Housing and the Remote Housing Strategy (2008–2018); Department of the Prime Minister and Cabinet, Commonwealth of Australia: Canberra, Australia, 2017.
- Bailie, R.; Stevens, M.; McDonald, E.; Brewster, D.; Guthridge, S. Exploring cross-sectional associations between common childhood illness, housing and social conditions in remote Australian Aboriginal communities. BMC Public Health 2010, 10, 147–157. [Google Scholar] [CrossRef] [PubMed]
- DoH. Environmental Health Practitioner Manual: A Resource Manual for Environmental Health Practitioners Working with Aboriginal and Torres Strait Islander Communities; Department of Health: Canberra, Australia, 2010.
- Buntsma, D.; Lithgow, A.; O’Neill, E.; Palmer, D.; Morris, P.; Acworth, J.; Babl, F.R. Patterns of paediatric emergency presentations to a tertiary referral centre in the Northern Territory. Em. Med. Austr. 2017, 29, 678–685. [Google Scholar] [CrossRef] [PubMed]
- Clucas, D.B.; Carville, K.S.; Connors, C.; Currie, B.J.; Carapetis, J.R.; Andrews, R.M. Disease burden and health-care clinic attendances for young children in remote aboriginal communities of northern Australia. Bull World Health Organ. 2008, 86, 275–281. [Google Scholar] [PubMed]
- Kearns, T.; Clucas, D.; Connors, C.; Currie, B.J.; Carapetis, J.R.; Andrews, R.M. Clinic Attendances during the First 12 Months of Life for Aboriginal Children in Five Remote Communities of Northern Australia. PLoS ONE 2013, 8, e58231. [Google Scholar] [CrossRef] [PubMed]
- Commonwealth of Australia. Closing the Gap Prime Minister’s Report 2018; Department of the Prime Minister and Cabinet, Commonwealth of Australia: Canberra, Australia, 2018.
- Bailie, R. Housing. In Social Determinants of Indiegnous Health; Carson, B., Dunbar, T., Chenhall, R., Bailie, R., Eds.; Allen and Unwin: Sydney, Australia, 2007; pp. 203–230. [Google Scholar]
- Mara, D.; Lane, J.; Scott, B.; Trouba, D. Sanitation and Health. PLoS Med. 2010, 7, e1000363. [Google Scholar] [CrossRef]
- Green, B.; Johnson, C.; Adams, A. Writing narrative literature reviews for peer-reviewed journals: Secrets of the trade. J. Chiropr. Med. 2006, 5, 101–117. [Google Scholar] [CrossRef]
- Collins, J.; Fauser, B. Balancing the strengths of systematic and narrative reviews. Hum. Reprod. Update 2005, 11, 103–104. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Int. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Pholeros, P.; Lea, T.; Rainow, S.; Sowerbutts, T.; Torzillo, P.J. Improving the state of health hardware in Australian Indigenous housing: Building more houses is not the only answer. Int. J. Circumpolar Health 2013, 72, 21181. [Google Scholar] [CrossRef] [PubMed]
- Wohlin, C. Guidelines for snowballing in systematic literature studies and a replication in software engineering. In Proceedings of the 18th International Conference on Evaluation and Assessment in Software Engineering (EASE 2014), London, UK, 13–14 May 2014. [Google Scholar]
- Pappas, C.; Williams, I. Grey Literature: Its Emerging Importance. J. Hosp. Librariansh. 2011, 11, 228–234. [Google Scholar] [CrossRef]
- WHO. Infectious Diseases Webpage; World Health Organisation: Geneva, Switzerland, 2018; Available online: http://www.who.int/topics/infectious_diseases/en/ (accessed on 5 July 2018).
- ABS. 1270.0.55.004—Australian Statistical Geography Standard (ASGS): Volume 4—Significant Urban Areas, Urban Centres and Localities, Section of State; Australian Bureau of Statistics: Canberra, Australia, 2017.
- Jacoby, P.; Carville, K.S.; Hall, G.; Riley, T.V.; Bowman, J.; Leach, A.J.; Lehmann, D. Crowding and other strong predictors of upper respiratory tract carriage of otitis media-related bacteria in Australian Aboriginal and non-Aboriginal children. Pediatr. Infect. Dis. J. 2011, 30, 480–485. [Google Scholar] [CrossRef] [PubMed]
- Jacoby, P.A.; Coates, H.L.; Arumugaswamy, A.; Elsbury, D.; Stokes, A.; Monck, R.; Finucane, J.M.; Weeks, S.A.; Lehmann, D. The effect of passive smoking on the risk of otitis media in Aboriginal and non-Aboriginal children in the Kalgoorlie-Boulder region of Western Australia. Med. J. Aust. 2008, 188, 599–603. [Google Scholar] [PubMed]
- Bailie, R.S.; Stevens, M.; McDonald, E.L. The impact of housing improvement and socio-environmental factors on common childhood illnesses: A cohort study in Indigenous Australian communities. J. Epidemiol. Community Health 2012, 66, 821–831. [Google Scholar] [CrossRef] [PubMed]
- Dossetor, P.J.; Martiniuk, A.L.C.; Fitzpatrick, J.P.; Oscar, J.; Carter, M.; Watkins, R.; Elliott, E.J.; Jeffery, H.E.; Harley, D. Pediatric hospital admissions in Indigenous children: A population-based study in remote Australia. BMC Pediatr. 2017, 17, 195. [Google Scholar] [CrossRef] [PubMed]
- Andersen, M.J.; Skinner, A.; Williamson, A.B.; Fernando, P.; Wright, D. Housing conditions associated with recurrent gastrointestinal infection in urban Aboriginal children in NSW, Australia: Findings from SEARCH. Aust. N. Z. J. Public Health 2018, 42, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Melody, S.M.; Bennett, E.; Clifford, H.D.; Johnston, F.H.; Shepherd, C.C.J.; Alach, Z.; Lester, M.; Wood, L.J.; Franklin, P.; Zosky, G.R. A cross-sectional survey of environmental health in remote Aboriginal communities in Western Australia. Int. J. Environ. Health Res. 2016, 26, 525–535. [Google Scholar] [CrossRef]
- Spurling, G.K.; Askew, D.A.; Schluter, P.J.; Simpson, F.; Hayman, N.E. Household number associated with middle ear disease at an urban Indigenous health service: A cross-sectional study. Aust. J. Prim. Health 2014, 20, 285–290. [Google Scholar] [CrossRef]
- McDonald, E.; Bailie, R. Hygiene improvement: Essential to improving child health in remote Aboriginal communities. J. Paediatr. Child Health 2010, 46, 491–496. [Google Scholar] [CrossRef] [PubMed]
- Massey, P.D.; Miller, A.; Saggers, S.; Durrheim, D.N.; Speare, R.; Taylor, K.; Pearce, G.; Odo, T.; Broome, J.; Judd, J.; et al. Australian Aboriginal and Torres Strait Islander communities and the development of pandemic influenza containment strategies: Community voices and community control. Health Policy 2011, 103, 184–190. [Google Scholar] [CrossRef] [PubMed]
- McDonald, E.; Bailie, R.; Grace, J.; Brewster, D. An ecological approach to health promotion in remote Australian Aboriginal communities. Health Promot. Int. 2010, 25, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Lansingh, V.C.; Mukesh, B.N.; Keeffe, J.E.; Taylor, H.R. Trachoma control in two Central Australian Aboriginal communities: A case study. Int. Ophthalmol. 2010, 30, 367–375. [Google Scholar] [CrossRef] [PubMed]
- McDonald, E.; Bailie, R.; Grace, J.; Brewster, D. A case study of physical and social barriers to hygiene and child growth in remote Australian Aboriginal communities. BMC Public Health 2009, 9, 346. [Google Scholar] [CrossRef] [PubMed]
- NSW Health. Closing the Gap: 10 Years of Housing for Health in NSW: An Evaluation of a Healthy Housing Intervention; New South Wales Department of Health: Sydney, Australia, 2010.
- Sartbayeva, A. Housing Conditions and Children’s Health; National Centre for Longitudinal Data: Canberra, Australia, 2016. [Google Scholar]
- Vino, T.; Singh, G.R.; Davision, B.; Campbell, P.T.; Lydeamore, M.J.; Robinson, A.; McVernon, J.; Tong, S.Y.C.; Geard, N. Indigenous Australian household structure: A simple data collection tool and implications for close contact transmission of communicable diseases. PeerJ 2017, 5, e3958. [Google Scholar] [CrossRef] [PubMed]
- Senge, P. The Fifth Discipline; Doubleday/Currency: New York, NY, USA, 1990. [Google Scholar]
- Senge, P.; Sterman, J. Systems thinking and organizational learning: Acting locally and thinking globally in the organization of the future. Eur. J. Oper. Res. 1992, 59, 137–150. [Google Scholar] [CrossRef]
- Hovmand, P. Community-Based System Dynamics; Springer: New York, NY, USA, 2014. [Google Scholar]
- Freeman, M.C.; Stocks, M.E.; Cumming, O.; Jeandron, A.; Higgins, J.P.; Wolf, J.; Pruss-Ustun, A.; Bonjour, S.; Hunter, P.R.; Fewtrell, L.; et al. Hygiene and health: Systematic review of handwashing practices worldwide and update of health effects. Trop. Med. Int. Health 2014, 19, 906–916. [Google Scholar] [CrossRef] [PubMed]
| Reference | State/Territory | Study Design | Area (Rural/Urban) |
|---|---|---|---|
| Andersen et al., (2018) [36] | NSW | Cohort Study | Urban |
| Bailie et al., (2012) [34] | NT | Cohort Study | Mixed |
| Bailie et al., (2010) [16] | NT | Cross-sectional Study | Mixed |
| Dossetor et al., (2017) [35] | WA | Cohort Study | Rural |
| Jacoby et al., (2008) [33] | WA | Cohort Study | Rural |
| Lansingh (2010) [42] | SA | Case Study | Rural |
| Massey et al., (2011) [40] | Multiple | Qualitative Descriptive Study | Rural |
| McDonald, E.; Bailie, R. [39] | NT | Qualitative Descriptive Study | Rural |
| McDonald et al., (2010) [41] | NT | Qualitative Descriptive Study | Rural |
| McDonald (2009) [43] | NT | Case Study | Rural |
| Melody et al., (2016) [37] | WA | Cross-sectional Study | Rural |
| Spurling et al., (2014) [38] | QLD | Cross-sectional Study | Urban |
| Vino et al., (2017) [46] | NT | Modelling Study | Mixed |
| Jacoby et al., (2011) [32] | WA | Cohort Study | Rural |
| Sartbayeva (2016) [45] | Multiple | Research summary | Mixed |
| NSW Department of Health (2010) [44] | NSW | Cohort study | Rural |
| Disease Categories | Reported Association with Residential Environment |
|---|---|
| Gastrointestinal (e.g., intestinal infections) | POSITIVE ASSOCIATION: Crowding [37], Perception of crowding [36], structural or plumbing problems [36], damp or mildew [36], houses in need of repair/improvement [44], low availability of household cleaning equipment [34], diarrhoea/vomiting associated with poor hygienic state of food preparation and storage areas [16] NO/MINIMAL ASSOCIATION: Crowding [36], water quality [37] |
| Skin (e.g., skin infections, scabies) | POSITIVE ASSOCIATION: Crowding [16,34,37], poor temperature control [16], evidence of pests and vermin [16], houses in need of repair/improvement [45,47], infrastructure required to wash clothes and bedding [34] *, prepare and store food [34], remove human waste [34], remove rubbish [16,34], control mold [34], control dust [16] NO/MINIMAL ASSOCIATION: [for skin infection] Any infrastructure variables [16], water quality [37] |
| Ear (e.g., ear infections, hearing) | POSITIVE ASSOCIATION: Crowding [32,33,37,38], limited toilet infrastructure [16], houses in need of repair/improvement [16,47], poor hygienic condition of bedding and sleeping areas [34] |
| Eye (e.g., trachoma) | POSITIVE ASSOCIATION: Crowding [37] NO/MINIMAL ASSOCIATION: Environmental improvement [42] |
| Respiratory (e.g., lung infections) | POSITIVE ASSOCIATION: Poor overall hygienic condition of house [16], poor overall function of house [16], houses in need of repair/improvement [44], dust [37], crowding/crowding associated with influenza, flu/cold transmission [37,40,46] NEGATIVE ASSOCIATION: Infrastructure required for ‘wash people’ variable [37] |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ali, S.H.; Foster, T.; Hall, N.L. The Relationship between Infectious Diseases and Housing Maintenance in Indigenous Australian Households. Int. J. Environ. Res. Public Health 2018, 15, 2827. https://doi.org/10.3390/ijerph15122827
Ali SH, Foster T, Hall NL. The Relationship between Infectious Diseases and Housing Maintenance in Indigenous Australian Households. International Journal of Environmental Research and Public Health. 2018; 15(12):2827. https://doi.org/10.3390/ijerph15122827
Chicago/Turabian StyleAli, Shahmir H., Tim Foster, and Nina Lansbury Hall. 2018. "The Relationship between Infectious Diseases and Housing Maintenance in Indigenous Australian Households" International Journal of Environmental Research and Public Health 15, no. 12: 2827. https://doi.org/10.3390/ijerph15122827
APA StyleAli, S. H., Foster, T., & Hall, N. L. (2018). The Relationship between Infectious Diseases and Housing Maintenance in Indigenous Australian Households. International Journal of Environmental Research and Public Health, 15(12), 2827. https://doi.org/10.3390/ijerph15122827





