Socioeconomic Status and Morbidity Rate Inequality in China: Based on NHSS and CHARLS Data
Abstract
1. Introduction
2. Data and Methods
2.1. Data Sources
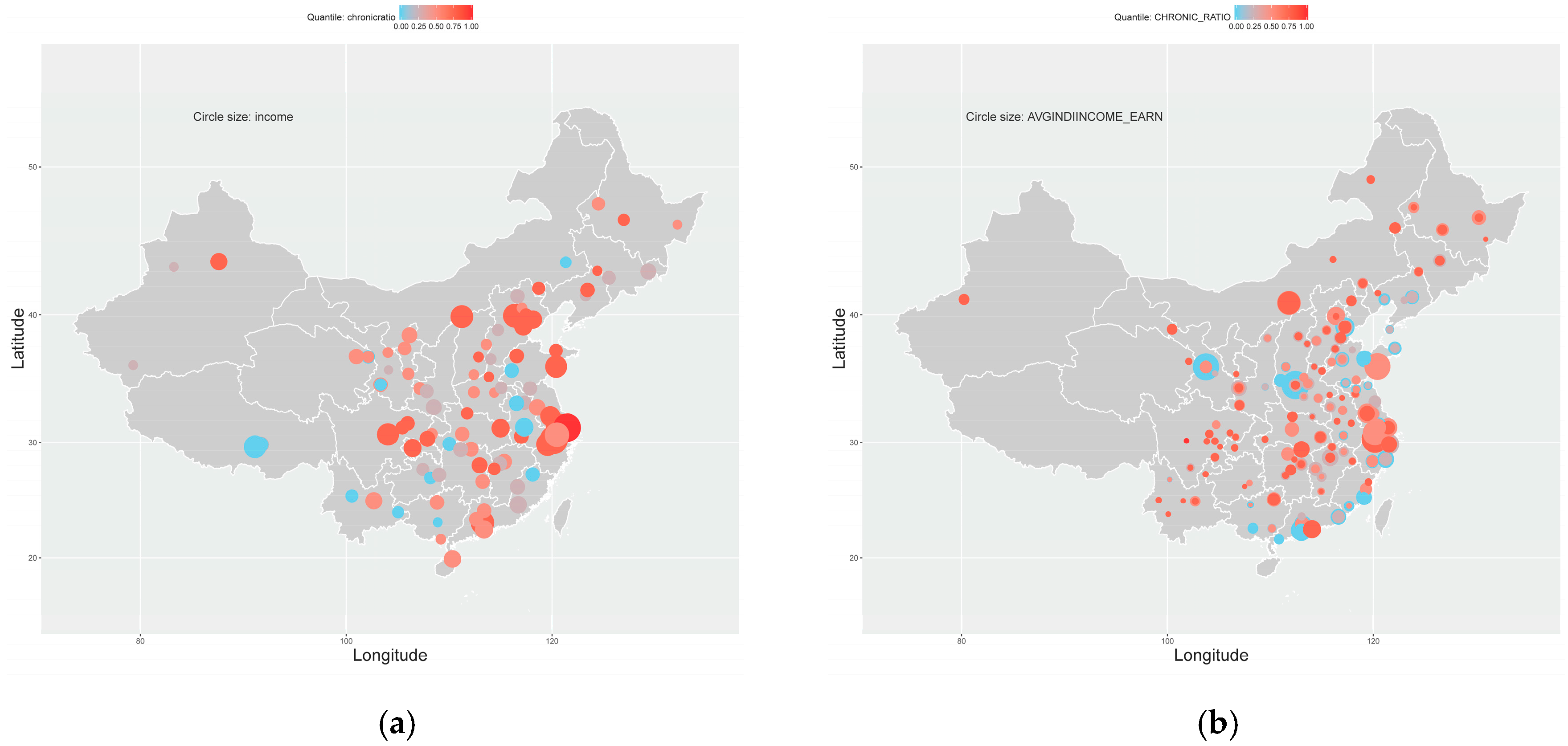
2.2. Variables
2.3. Descriptive Statistics
2.4 Model Specification
3. Results
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A: Variables and other descriptive statistics
| Variables | Codes | Unit | Variable explanation |
|---|---|---|---|
| Prevalence of chronic disease | CHRONIC_RATIO | prop | Proportion of the respondents who have at least one of the 13 kinds of chronic diseases |
| 1-year earned incomes per capita | AVGINDIINCOME_EARN | 10-thousand yuan | Annually incomes from employment per capita |
| Square of the 1-year earned incomes per capita | AVGINDIINCOME_EARN2 | 10-thousand yuan square | Square of AVGINDIINCOME_EARN |
| Average education years | AVGEDU | year | Approximate education years |
| Average age | AVGAGE | year | Average age |
| Marriage rate | MARITAL_RATIO | prop | Ratio of married respondents |
| Marriage years | MARITAL_AVELEN | year | Years of current or the latest marriage |
| Drinking rate | DRINK1Y_RATIO | prop | Ratio of the respondents who ever drank in the past 1 year |
| Smoking rate | SMOKENOW_RATIO | prop | Ratio of smoking respondents |
| Smoking frequency | AVGSMOKENUM | integer | Number of cigarettes smoked per day |
| 1-year inpatient expenditure | AVGHOSP1Y_REALEXP | yuan | Out-of-pocket inpatient expenditure in the past 1 year |
| 1-month outpatient expenditure | AVGOUTP1M_REALEXP | yuan | Out-of-pocket outpatient expenditure in the past 1 month |
| 1-week food consumption | AVGEXP1W_FOOD | yuan | Food consumptions in the past 1 week |
| Coverage rate of health insurance | INSURANCE_RATIO | prop | Ratio of the respondents who are covered by any kind of health insurance plans |
| Coverage rate of public health insurance | INSGOV_RATIO | prop | Ratio of the respondents who are covered by government or public health insurance plans |
| 1-year total consumption | AVGEXP1Y_TOTAL | yuan | Total amount of consumptions in the past 1 year |
| Children support rate | CHILDCARE_RATIO | prop | Ratio of the respondents who receive any kind of supports from children or grandchildren |
| Children co-residence rate | CHILDCORESD_RATIO | prop | Ratio of the respondents living with children or grandchildren |
| Children living-nearby rate | CHILDLVNEAR_RATIO | prop | Ratio of the respondents whose children live nearby |
| Children financial support rate | TRANSCHILD_RATIO | prop | Ratio of the respondents who receive financial support from children |
| Working rate | WORK_RATIO | prop | Ratio of the respondents who reported they are still working de facto |
| Agricultural-work rate | JOBSTATUS_AGRI_RATIO | prop | Ratio of the respondents who reported they are doing agricultural jobs |
| Non-agricultural employment rate | JOBSTATUS_NAGE_RATIO | prop | Ratio of the respondents who reported they are employed by non-agricultural jobs |
| Non-agricultural self-employment rate | JOBSTATUS_NAGS_RATIO | prop | Ratio of the respondents who reported they are self-employed by non-agricultural jobs |
| Unemployment rate | JOBSTATUS_UNEM_RATIO | prop | Ratio of the respondents who reported they are unemployed but not retired yet |
| Never-worked rate | JOBSTATUS_NEWK_RATIO | prop | Ratio of the respondents who reported they never worked before |
| Index | NHSS | CHARLS | ||||||
|---|---|---|---|---|---|---|---|---|
| Year | Counties | Illnessratio | Illnessday | Chronicratio | Year | Cities | CHRONIC_RATIO | |
| Gini | 1998 | 94 | 0.2316 | 0.2512 | 0.2790 | 2011 | 126 | 0.0744 |
| 2003 | 95 | 0.1998 | 0.2395 | 0.2312 | 2013 | 126 | 0.0640 | |
| 2008 | 93 | 0.2514 | 0.2837 | 0.2196 | 2015 | 126 | 0.0511 | |
| Theil-I | 1998 | 94 | 0.0874 | 0.1026 | 0.1215 | 2011 | 126 | 0.0089 |
| 2003 | 95 | 0.0635 | 0.0909 | 0.0860 | 2013 | 126 | 0.0065 | |
| 2008 | 93 | 0.1026 | 0.1287 | 0.0763 | 2015 | 126 | 0.0041 | |
| Theil-II | 1998 | 94 | 0.0852 | 0.1003 | 0.1286 | 2011 | 126 | 0.0091 |
| 2003 | 95 | 0.0670 | 0.0956 | 0.0932 | 2013 | 126 | 0.0067 | |
| 2008 | 93 | 0.0994 | 0.1275 | 0.0799 | 2015 | 126 | 0.0041 | |
| Coef of Variation | 1998 | 94 | 0.4418 | 0.4808 | 0.5048 | 2011 | 126 | 0.1326 |
| 2003 | 95 | 0.3603 | 0.4360 | 0.4189 | 2013 | 126 | 0.1141 | |
| 2008 | 93 | 0.4825 | 0.5375 | 0.3977 | 2015 | 126 | 0.0901 | |
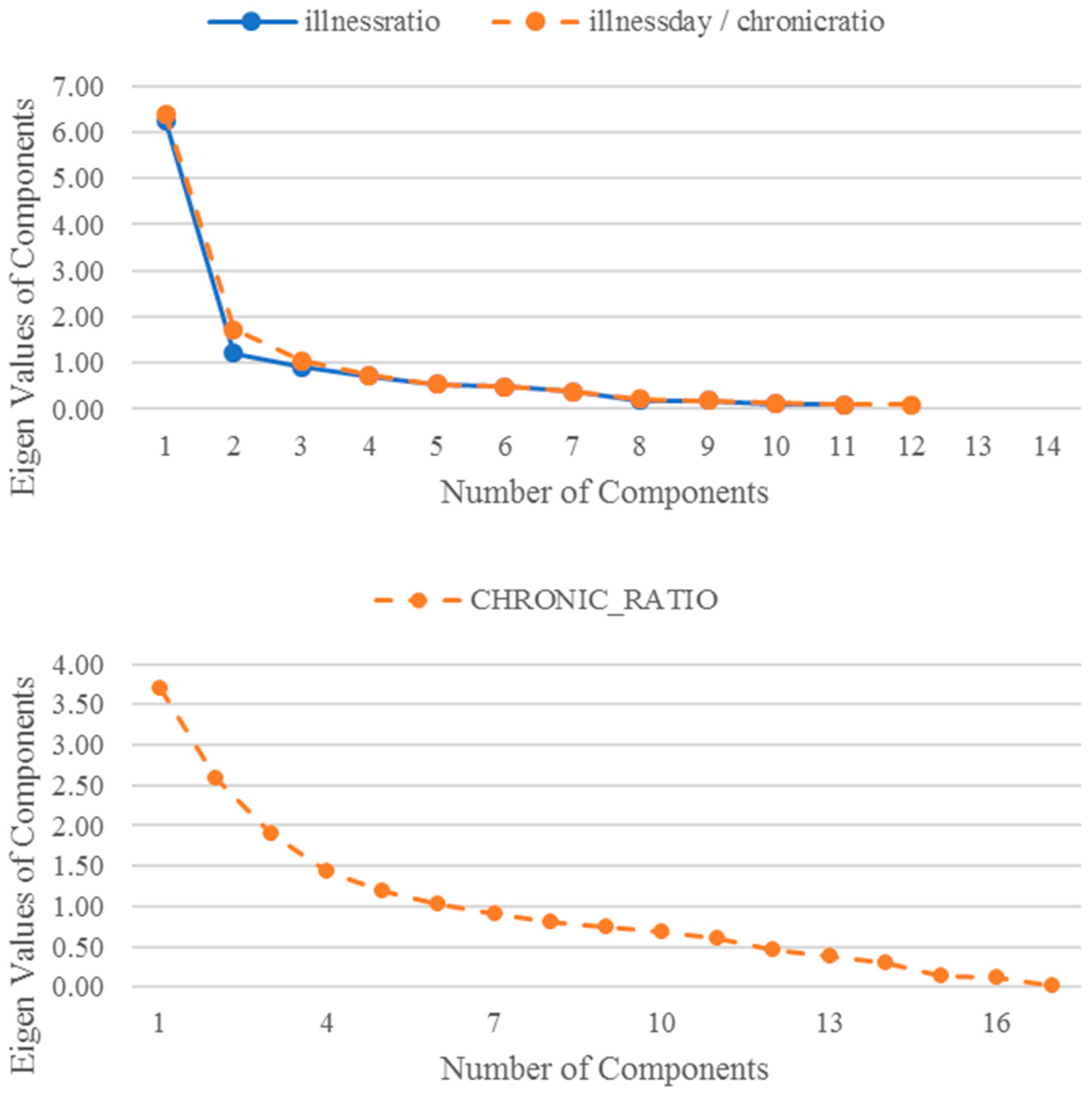
Appendix B: PCA Results
| Components | RC2 | RC1 | RC3 |
|---|---|---|---|
| Names | Medical Burden | Urbanization | Geographic Accessibility |
| urban | 0.1699 | 0.8565 | 0.2240 |
| expend | 0.7731 | 0.5070 | 0.1652 |
| medicost | 0.8623 | 0.2998 | 0.1742 |
| male | −0.3136 | −0.6983 | 0.0610 |
| age65 | 0.5439 | 0.6531 | −0.0027 |
| average | 0.6634 | 0.5976 | 0.1000 |
| time10 | 0.0881 | 0.1195 | 0.9264 |
| permedicost | 0.6268 | 0.2827 | 0.2826 |
| perhospitalcost | 0.6812 | 0.5051 | 0.2325 |
| insurance | 0.7841 | 0.0106 | −0.1891 |
| washroom | 0.1589 | 0.8759 | 0.1772 |
| Components | RC3 | RC1 | RC2 | RC4 |
|---|---|---|---|---|
| Names | Urbanization | Medical Burden | Geographic Accessibility | Health Insurance |
| urban | 0.8140 | 0.3303 | 0.2173 | −0.0703 |
| expend | 0.4763 | 0.6673 | 0.1357 | 0.4397 |
| medicost | 0.2633 | 0.7471 | 0.1083 | 0.4842 |
| male | −0.7305 | −0.0573 | −0.1031 | −0.3919 |
| age65 | 0.6501 | 0.4076 | 0.0325 | 0.3698 |
| average | 0.5901 | 0.4928 | 0.1219 | 0.4591 |
| distance | 0.2185 | 0.0655 | 0.9288 | −0.0077 |
| time10 | 0.0766 | 0.1292 | 0.9450 | 0.0397 |
| permedicost | 0.1898 | 0.8772 | 0.0679 | 0.0250 |
| perhospitalcost | 0.4583 | 0.6838 | 0.1624 | 0.2964 |
| insurance | 0.0677 | 0.2284 | −0.0312 | 0.8704 |
| washroom | 0.8474 | 0.2864 | 0.1460 | −0.0374 |
| Components | RC5 | RC1 | RC2 | RC3 | RC4 | RC6 | RC7 |
|---|---|---|---|---|---|---|---|
| Names | Children Support | Family Relations | Consumption | Physical Burden | Drinking | Medical Burden | Un−Employment |
| AVGAGE | −0.2146 | 0.8811 | 0.0671 | 0.0786 | −0.0063 | 0.1024 | −0.0350 |
| MARITAL_RATIO | −0.1523 | −0.4380 | −0.3284 | 0.1957 | 0.3946 | 0.1868 | 0.2155 |
| MARITAL_AVELEN | −0.1560 | 0.8706 | −0.0073 | −0.1443 | 0.0626 | 0.0763 | 0.1515 |
| DRINK1Y_RATIO | −0.2836 | −0.0658 | 0.0067 | 0.0926 | 0.7237 | −0.0122 | −0.1155 |
| AVGHOSP1Y_REALEXP | 0.1042 | 0.2534 | 0.3165 | 0.1663 | 0.1429 | 0.5617 | −0.0350 |
| AVGOUTP1M_REALEXP | −0.1089 | −0.0278 | 0.1028 | −0.0954 | −0.0570 | 0.7873 | 0.1441 |
| AVGEXP1W_FOOD | 0.0023 | 0.0675 | 0.9361 | −0.0117 | 0.0353 | 0.1028 | 0.0147 |
| AVGEXP1Y_TOTAL | 0.0320 | 0.0371 | 0.9127 | 0.1526 | 0.0583 | 0.1972 | −0.0049 |
| CHILDCARE_RATIO | 0.9551 | −0.1080 | −0.0514 | 0.0988 | −0.0629 | 0.0202 | −0.0128 |
| CHILDCORESD_RATIO | 0.7243 | −0.2237 | 0.2799 | −0.1026 | −0.2160 | −0.1179 | 0.0216 |
| CHILDLVNEAR_RATIO | 0.9489 | −0.1397 | −0.0571 | 0.0848 | −0.0784 | 0.0073 | −0.0054 |
| TRANSCHILD_RATIO | −0.2022 | 0.6391 | 0.0789 | −0.2419 | 0.2643 | 0.0540 | 0.3319 |
| WORK_RATIO | 0.0219 | −0.1650 | −0.1095 | −0.5946 | 0.3037 | −0.4071 | 0.3917 |
| JOBSTATUS_NAGE_RATIO | 0.1384 | −0.1395 | 0.0788 | 0.7640 | 0.1820 | 0.0212 | −0.1084 |
| JOBSTATUS_NAGS_RATIO | −0.0906 | −0.2229 | 0.0255 | 0.6041 | −0.0895 | −0.3563 | 0.4260 |
| JOBSTATUS_UNEM_RATIO | −0.0371 | −0.2112 | 0.0018 | 0.0694 | −0.0347 | −0.1339 | −0.7833 |
| JOBSTATUS_NEWK_RATIO | −0.0098 | −0.3213 | −0.1421 | 0.0629 | −0.6985 | 0.0012 | −0.1844 |
Appendix C: Other Results
| NHSS | CHARLS | ||||||
|---|---|---|---|---|---|---|---|
| Illnessratio | Illnessday | Chronicratio | CHRONIC_RATIO | ||||
| income | 4.857 | income | 4.875 | income | 4.875 | AVGINDIINCOME_EARN | 15.597 |
| income2 | 2.298 | income2 | 2.304 | income2 | 2.304 | AVGINDIINCOME_EARN2 | 11.190 |
| edu | 7.238 | edu | 7.388 | edu | 7.388 | AVGEDU | 2.210 |
| RC1 | 3.934 | RC1 | 4.309 | RC1 | 4.309 | RC1 | 1.107 |
| RC2 | 4.764 | RC2 | 1.881 | RC2 | 1.881 | RC2 | 1.053 |
| RC3 | 1.992 | RC3 | 3.564 | RC3 | 3.564 | RC3 | 2.815 |
| RC4 | 2.091 | RC4 | 2.091 | RC4 | 1.049 | ||
| RC5 | 1.022 | ||||||
| RC6 | 1.354 | ||||||
| RC7 | 1.281 | ||||||
| Variable | Individual Fixed Effect (FGLS) ⱡ | Individual Random Effect (FGLS) ⱴ | Two-way Fixed Effect (FGLS) ⱡ | Pooling (FGLS) | Pooling (OLS) |
|---|---|---|---|---|---|
| illnessratio | |||||
| (Intercept) | 21.8469 *** | 10.0209 ** | 24.5788 *** | 13.0202 *** | 13.0202 *** |
| (4.4718) | (3.9618) | (4.6590) | (4.0368) | (4.0368) | |
| income | −0.3118 | 0.1051 | −0.5214 | −0.2278 | −0.2278 |
| (0.3252) | (0.3149) | (0.3371) | (0.3391) | (0.3391) | |
| income2 | 0.2167 *** | 0.1758 *** | 0.2243 *** | 0.1756 *** | 0.1756 *** |
| (0.0379) | (0.0387) | (0.0378) | (0.0395) | (0.0395) | |
| edu | −0.1521 | 0.6774 | −0.4592 | 0.2953 | 0.2953 |
| (0.5851) | (0.5469) | (0.5938) | (0.5557) | (0.5557) | |
| RC2 (medical burden) | 1.9514 ** | 0.6978 | 2.3577 ** | 1.7011 ** | 1.7011 ** |
| (0.8429) | (0.8103) | (1.0439) | (0.8601) | (0.8601) | |
| RC1 (urbanization) | 0.9746 | 0.0438 | 1.4062 | 0.5049 | 0.5049 |
| (0.8793) | (0.7792) | (0.8967) | (0.7816) | (0.7816) | |
| RC3 (geographic accessibility) | 0.0508 | −0.4741 | 0.4391 | −0.1480 | −0.1480 |
| (0.5704) | (0.5538) | (0.5890) | (0.5562) | (0.5562) | |
| illnessday | |||||
| (Intercept) | 1631.8347 *** | 744.3945 ** | 1706.3932 *** | 1068.9368 *** | 1068.9368 *** |
| (401.3076) | (351.3749) | (415.9300) | (360.3742) | (360.3742) | |
| income | −13.7166 | 3.3721 | −26.7318 | −34.9995 | −34.9995 |
| (28.749) | (27.7268) | (30.0394) | (30.0065) | (30.0065) | |
| income2 | 18.7594 *** | 16.8128 *** | 19.0379 *** | 17.7110 *** | 17.7110 *** |
| (3.3440) | (3.3296) | (3.3100) | (3.4914) | (3.4914) | |
| edu | −20.0401 | 62.9851 | −37.8590 | 19.5179 | 19.5179 |
| (53.0576) | (48.5439) | (52.7612) | (49.5975) | (49.5975) | |
| RC3 (urbanization) | 174.3866 ** | 32.8512 | 183.2006** | 84.5007 | 84.5007 |
| (76.2881) | (65.5659) | (75.7176) | (65.7198) | (65.7198) | |
| RC1 (health burden) | 54.1368 | −59.3752 | 155.9446 ** | 55.7788 | 55.7788 |
| (69.9565) | (68.4793) | (76.2863) | (72.2603) | (72.2603) | |
| RC2 (geographic accessibility) | 34.8607 | 20.7914 | 41.7407 | 38.9836 | 38.9836 |
| (52.4659) | (48.0439) | (51.8061) | (47.7470) | (47.7470) | |
| RC4 (health insurance) | 171.5954 *** | 135.6597 *** | 247.2420 *** | 200.8171 *** | 200.8171 *** |
| (49.6029) | (46.1464) | (69.9900) | (50.3339) | (50.3339) | |
| chronicratio | |||||
| (Intercept) | 16.9854 *** | 13.0889 *** | 16.9771 *** | 14.5350 *** | 14.5350 *** |
| (3.0980) | (2.7301) | (3.1958) | (2.7004) | (2.7004) | |
| income | −0.5160 ** | −0.4471** | −0.5789 ** | −0.7147 *** | −0.7147 *** |
| (0.2219) | (0.2074) | (0.2308) | (0.2249) | (0.2249) | |
| income2 | 0.0865 *** | 0.0789 *** | 0.0868 *** | 0.0974 *** | 0.0974 *** |
| (0.0258) | (0.0246) | (0.0254) | (0.0262) | (0.0262) | |
| edu | −0.3765 | 0.0614 | −0.4943 | −0.1397 | −0.1397 |
| (0.4096) | (0.3752) | (0.4054) | (0.3717) | (0.3717) | |
| RC3 (urbanization) | 4.0814 *** | 3.1392 *** | 4.1033 *** | 3.3727 *** | 3.3727 *** |
| (0.5889) | (0.5082) | (0.5818) | (0.4925) | (0.4925) | |
| RC1 (health burden) | 2.0875 *** | 1.6458 *** | 2.9994 *** | 2.2899 *** | 2.2899 *** |
| (0.5400) | (0.5160) | (0.5862) | (0.5415) | (0.5415) | |
| RC2 (geographic accessibility) | 0.5926 | 0.5248 | 0.6255 | 0.5997 * | 0.5997 * |
| (0.4050) | (0.3805) | (0.3981) | (0.3578) | (0.3578) | |
| RC4 (health insurance) | 2.5506 *** | 2.4239 *** | 3.3971 *** | 2.6387 *** | 2.6387 *** |
| (0.3829) | (0.3520) | (0.5378) | (0.3772) | (0.3772) | |
| Variable | Individual Fixed Effect (FGLS) ⱡ | Individual Random Effect (FGLS) ⱴ | Two-way Fixed Effect (FGLS) ⱡ | Pooling (FGLS) | Pooling (OLS) |
|---|---|---|---|---|---|
| CHRONIC_RATIO | |||||
| (Intercept) | 0.9415 *** | 0.7798 *** | 0.9772 *** | 0.7906 *** | 0.7906 *** |
| (0.0549) | (0.0480) | (0.0515) | (0.0460) | (0.0460) | |
| AVGINDIINCOME_EARN | −0.1982 *** | −0.1724 *** | −0.1482 *** | −0.2609 *** | −0.2609 *** |
| (0.0452) | (0.0342) | (0.0433) | (0.0493) | (0.0493) | |
| AVGINDIINCOME_EARN2 | 0.0882 *** | 0.0792 *** | 0.0670 *** | 0.1081 *** | 0.1081 *** |
| (0.0253) | (0.0187) | (0.0239) | (0.0285) | (0.0285) | |
| AVGEDU | −0.0768 ** | 0.0221 | −0.0509 | 0.0338 | 0.0338 |
| (0.0362) | (0.0405) | (0.0340) | (0.0379) | (0.0379) | |
| RC5 (children support) | −0.0137 *** | −0.0203 *** | −0.0059 | −0.0217 *** | −0.0217 *** |
| (0.0039) | (0.0033) | (0.0039) | (0.0041) | (0.0041) | |
| RC1 (family relations) | 0.0409 *** | 0.0462 *** | 0.0090 | 0.0333 *** | 0.0333 *** |
| (0.0037) | (0.0032) | (0.0060) | (0.0042) | (0.0042) | |
| RC2 (consumption) | 0.0236 *** | 0.0163 *** | 0.0119 *** | 0.0295 *** | 0.0295 *** |
| (0.0037) | (0.0030) | (0.0039) | (0.0041) | (0.0041) | |
| RC3 (physical burden) | 0.0150 ** | 0.0026 | 0.0070 | 0.0074 | 0.0074 |
| (0.0065) | (0.0060) | (0.0062) | (0.0068) | (0.0068) | |
| RC4 (drinking) | 0.0192 *** | 0.0109 *** | 0.0107 ** | 0.0122 *** | 0.0122 *** |
| (0.0043) | (0.0039) | (0.0042) | (0.0041) | (0.0041) | |
| RC6 (medical burden) | 0.0244 *** | 0.0148 *** | 0.0158 *** | 0.0241 *** | 0.0241 *** |
| (0.0042) | (0.0031) | (0.0041) | (0.0047) | (0.0047) | |
| RC7 (unemployment) | 0.0013 | 0.0043 | −0.0051 | 0.0023 | 0.0023 |
| (0.0041) | (0.0031) | (0.0042) | (0.0046) | (0.0046) | |
| NHSS | |||
| Illnessratio | Illnessday | Chronicratio | |
| Shapiro-Wilk | 0.000 | 0.003 | 0.091 |
| Lilliefor | 0.007 | 0.002 | 0.321 |
| Pearson Chi-square | 0.321 | 0.001 | 0.371 |
| Anderson-Darling | 0.001 | 0.001 | 0.256 |
| Cramer-von Mises | 0.002 | 0.002 | 0.295 |
| CHARLS | |||
| CHRONIC_RATIO | |||
| Shapiro-Wilk | 0.151 | ||
| Lilliefor | 0.401 | ||
| Pearson Chi-square | 0.569 | ||
| Anderson-Darling | 0.134 | ||
| Cramer-von Mises | 0.239 | ||
References
- Myers, G.C. Differential Mortality in the United States: A Study in Socioeconomic Epidemiology; Kitagawa, E.M., Hauser, P.M., Eds.; Harvard University Press: Cambridge, MA, USA, 1973; Volume 69, pp. 654–662. [Google Scholar]
- Elo, I.T.; Preston, S.H. Educational differentials in mortality: United States, 1979–1985. Soc. Sci. Med. 1996, 42, 47. [Google Scholar] [CrossRef]
- Bassuk, S.S.; Berkman, L.F.; Amick, B.C. Socioeconomic Status and Mortality among the Elderly: Findings from Four US Communities. Am. J. Epidemiol. 2002, 155, 520–533. [Google Scholar] [CrossRef]
- Mustard, C.A.; Derksen, S.; Berthelot, J.-M.; Wolfson, M.; Roos, L.L. Age-specific education and income gradients in morbidity and mortality in a Canadian province. Soc. Sci. Med. 1997, 45, 383–397. [Google Scholar] [CrossRef]
- Marmot, M.G.; Shipley, M.J.; Rose, G. Inequalities in death-specific explanations of a general pattern? Lancet 1984, 323, 1003–1006. [Google Scholar] [CrossRef]
- Davey, S.G.; Hart, C.; Hole, D.; Mackinnon, P.; Gillis, C.; Watt, G.; Blane, D.; Hawthorne, V. Education and occupational social class: Which is the more important indicator of mortality risk? J. Epidemiol. Community Health 1998, 52, 153–160. [Google Scholar] [CrossRef]
- Zhu, H.; Xie, Y. Socioeconomic differentials in mortality among the oldest old in China. Res. Aging 2007, 29, 125–143. [Google Scholar] [CrossRef]
- Luo, Y.; Zhang, Z.; Gu, D. Education and mortality among older adults in China. Soc. Sci. Med. 2015, 127, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Huisman, M.; Kunst, A.E.; Mackenbach, J.P. Socioeconomic inequalities in morbidity among the elderly: A European overview. Soc. Sci. Med. 2003, 57, 861–873. [Google Scholar] [CrossRef]
- Crimmins, E.M.; Hayward, M.D.; Saito, Y. Changing mortality and morbidity rates and the health status and life expectancy of the older population. Demography 1994, 31, 159–175. [Google Scholar] [CrossRef]
- Elo, I.T. Social class differentials in health and mortality: Patterns and explanations in comparative perspective. Annu. Rev. Sociol. 2009, 35, 553–572. [Google Scholar] [CrossRef]
- Han, C. Health implications of socioeconomic characteristics, subjective social status, and perceptions of inequality: An empirical study of china. Soc. Indic. Res. 2014, 119, 495–514. [Google Scholar] [CrossRef]
- Kwon, S. Economic segmentation and health inequalities in urban post-reform China. Aims Public Health 2016, 3, 487. [Google Scholar] [CrossRef] [PubMed]
- Mirowsky, J.; Ross, C.E. Education, Social Status, and Health; Transaction Publishers: Piscataway, NJ, USA, 2003. [Google Scholar]
- Ross, C.E.; Mirowsky, J. Does medical insurance contribute to socioeconomic differentials in health? Milbank Q. 2000, 78, 291–321. [Google Scholar] [CrossRef] [PubMed]
- Ross, C.E.; Wu, C.-L. The links between education and health. Am. Sociol. Rev. 1995, 719–745. [Google Scholar] [CrossRef]
- Wang, H.; Yu, Y. Increasing health inequality in China: An empirical study with ordinal data. J. Econ. Inequal. 2016, 14, 41–61. [Google Scholar] [CrossRef]
- Winkleby, M.A.; Jatulis, D.E.; Frank, E.; Fortmann, S.P. Socioeconomic status and health: How education, income, and occupation contribute to risk factors for cardiovascular disease. Am. J. Public Health 1992, 82, 816–820. [Google Scholar] [CrossRef]
- Anderson, N.B.; Armstead, C.A. Toward understanding the association of socioeconomic status and health: A new challenge for the biopsychosocial approach. Psychosom. Med. 1995, 57, 213–225. [Google Scholar] [CrossRef]
- Evans, G.W.; Kantrowitz, E. Socioeconomic status and health: The potential role of environmental risk exposure. Annu. Rev. Public Health 2002, 23, 303–331. [Google Scholar] [CrossRef]
- Luo, W.; Xie, Y. Socio-economic disparities in mortality among the elderly in China. Popul. Stud. 2014, 68, 305–320. [Google Scholar] [CrossRef]
- Rosenbaum, E. Racial/ethnic differences in asthma prevalence: The role of housing and neighborhood environments. J. Health Soc. Behav. 2008, 49, 131–145. [Google Scholar] [CrossRef]
- Feinstein, J.S. The relationship between socioeconomic status and health: A review of the literature. Milbank Q. 1993, 279–322. [Google Scholar] [CrossRef]
- Mackenbach, J.P.; Stronks, K.; Kunst, A.E. The contribution of medical care to inequalities in health: Differences between socio-economic groups in decline of mortality from conditions amenable to medical intervention. Soc. Sci. Med. 1989, 29, 369–376. [Google Scholar] [CrossRef]
- Von dem Knesebeck, O.; Lschen, G.; Cockerham, W.C.; Siegrist, J. Socioeconomic status and health among the aged in the United States and Germany: A comparative cross-sectional study. Soc. Sci. Med. 2003, 57, 1643–1652. [Google Scholar] [CrossRef]
- Lutfey, K.; Freese, J. Toward some fundamentals of fundamental causality: Socioeconomic status and health in the routine clinic visit for diabetes. Am. J. Sociol. 2005, 110, 1326–1372. [Google Scholar] [CrossRef]
- Lantz, P.M.; Lynch, J.W.; House, J.S.; Lepkowski, J.M.; Mero, R.P.; Musick, M.A.; Williams, D.R. Socioeconomic disparities in health change in a longitudinal study of US adults: The role of health-risk behaviors. Soc. Sci. Med. 2001, 53, 29–40. [Google Scholar] [CrossRef]
- Lynch, J.W.; Kaplan, G.A.; Cohen, R.D.; Tuomilehto, J.; Salonen, J.T. Do cardiovascular risk factors explain the relation between socioeconomic status, risk of all-cause mortality, cardiovascular mortality, and acute myocardial infarction? Am. J. Epidemiol. 1996, 144, 934–942. [Google Scholar] [CrossRef] [PubMed]
- Blane, D.; Brunner, E.; Wilkinson, R.; Wilkinson, R.G. Health and Social Organization: Towards a Health Policy for the Twenty-First Century; Psychology Press: Hove, UK, 1996. [Google Scholar]
- Marmot, M.G.; Theorell, T.; Siegrist, J. Work and Coronary Heart Disease; BMJ Books: London, UK, 2002. [Google Scholar]
- Smith, G.D.; Dorling, D.; Gordon, D.; Shaw, M. The widening health gap: What are the solutions? Crit. Public Health 1999, 9, 151–170. [Google Scholar] [CrossRef]
- Potente, C.; Monden, C. Disability pathways preceding death in England by socio-economic status. Popul. Stud. A J. Demogr. 2018, 72, 175–190. [Google Scholar] [CrossRef]
- Liao, Y.; Mcgee, D.L.; Kaufman, J.S.; Cao, G.; Cooper, R.S. Socioeconomic status and morbidity in the last years of life. Am. J. Public Health 1999, 89, 569–572. [Google Scholar] [CrossRef]
- Huijts, T.; Eikemo, T.A.; Skalicka, V. Income-related health inequalities in the Nordic countries: Examining the role of education, occupational class, and age. Soc. Sci. Med. 2010, 71, 1964–1972. [Google Scholar] [CrossRef]
- Knesebeck, O.V.D.; Verde, P.E.; Dragano, N. Education and health in 22 European countries. Soc. Sci. Med. 2006, 63, 1344–1351. [Google Scholar] [CrossRef] [PubMed]
- Lei, X.; Yin, N.; Zhao, Y. Socioeconomic status and chronic diseases: The case of hypertension in China. China Econ. Rev. 2012, 23, 105–121. [Google Scholar] [CrossRef]
- Fang, X.; Jing, R.; Zeng, G.; Linnan, H.W.; Zhu, X.; Linnan, M. Socioeconomic status and the incidence of child injuries in China. Soc. Sci. Med. 2014, 102, 33–40. [Google Scholar] [CrossRef] [PubMed]
- Riley, J.C. The risk of being sick: Morbidity trends in four countries. Popul. Dev. Rev. 1990, 403–432. [Google Scholar] [CrossRef]
- Ki, M.; Lee, Y.H.; Kim, Y.-S.; Shin, J.-Y.; Lim, J.; Nazroo, J. Socioeconomic inequalities in health in the context of multimorbidity: A Korean panel study. PLoS ONE 2017, 12, e0173770. [Google Scholar] [CrossRef] [PubMed]
- Beaumaster, S.; Chien, S.; Lau, S.; Lin, A.; Phillps, D.; Wilkens, J.; Lee, J. Harmonized CHARLS Documentation, Version C.; Center for Economic and Social Research, USCDornsife: Santa Monica, CA, USA, 2018. [Google Scholar]
- Beydoun, M.A.; Popkin, B.M.J.S.S. The impact of socio-economic factors on functional status decline among community-dwelling older adults in China. Medicine 2005, 60, 2045–2057. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Liu, H.; Zhang, Y.; Shen, K.; Zeng, Y.J.H.E. The impact of health insurance on health outcomes and spending of the elderly: Evidence from china’s new cooperative medical scheme. Health Econ. 2015, 24, 672–691. [Google Scholar] [CrossRef]
- Elwellsutton, T.; Jiang, C.Q.; Zhang, W.S.; Cheng, K.K.; Lam, T.H.; Leung, G.; Schooling, C.M.J.S.S. P2-395 Socioeconomic influences at different life stages on self-rated health in Guangzhou, China. Medicine 2011, 73, 1884–1892. [Google Scholar]
- Kempen, G.I.; Brilman, E.I.; Ranchor, A.V.; Ormel, J.J.S.S. Morbidity and quality of life and the moderating effects of level of education in the elderly. Medicine 1999, 49, 143–149. [Google Scholar] [CrossRef]
- Bell, A.C.; Adair, L.S.; Popkin, B.M.J.S.S. Understanding the role of mediating risk factors and proxy effects in the association between socio-economic status and untreated hypertension. Medicine 2004, 59, 275–283. [Google Scholar]
- Huisman, M.; Kunst, A.E.; Andersen, O.; Bopp, M.; Borgan, J.K.; Borrell, C.; Costa, G.; Deboosere, P.; Desplanques, G.; Donkin, A.; et al. Socioeconomic inequalities in mortality among elderly people in 11 European populations. J. Epidemiol. Community Health 2004, 58, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Filmer, D.; Pritchett, L.J.S.S. The impact of public spending on health: Does money matter? Medicine 1999, 49, 1309. [Google Scholar] [CrossRef]
- Rosenberg, M.W. Accessibility to health care: A North-American perspective. Prog. Hum. Geogr. 1983, 7, 78–87. [Google Scholar] [CrossRef]
- Eggleston, K.; Ling, L.; Qingyue, M.; Lindelow, M.; Wagstaff, A. Health service delivery in China: A literature review. Health Econ. 2008, 17, 149–165. [Google Scholar] [CrossRef] [PubMed]
- Lancaster, T. The incidental parameter problem since 1948. J. Econom. 2000, 95, 391–413. [Google Scholar] [CrossRef]
- Gordon, D.; Howe, L.D.; Galobardes, B.; Matijasevich, A.; Johnston, D.; Onwujekwe, O.; Patel, R.; Webb, E.A.; Lawlor, D.A.; Hargreaves, J.R. Authors’ response to alternatives to principal components analysis to derive asset-based indices to measure socio-economic position in low- and middle-income countries: The case for multiple correspondence analysis. Int. J. Epidemiol. 2012, 41, 1209–1210. [Google Scholar] [CrossRef]
- Kolenikov, S.; Angeles, G. Socioeconomic status measurement with discrete proxy variables: Is principle component analysis a reliable answer? Rev. Income Wealth 2010, 55, 128–165. [Google Scholar] [CrossRef]
- Vyas, S.; Kumaranayake, L. Constructing socio-economic status indices: How to use principal components analysis. Health Policy Plan. 2006, 21, 459–468. [Google Scholar] [CrossRef]
- Zell, J.A.; Cinar, P.; Mobasher, M.; Ziogas, A.; Meyskens, F.L., Jr.; Anton-Culver, H. Survival for patients with invasive cutaneous melanoma among ethnic groups: The effects of socioeconomic status and treatment. J. Clin. Oncol. 2008, 26, 66–75. [Google Scholar] [CrossRef]
- Giri, N.C. Multivariate Statistical Analysis: Revised and Expanded; CRC Press: Boca Raton, FL, USA, 2003. [Google Scholar]

| Variables | Codes | Unit | Variable Explanation | |
|---|---|---|---|---|
| Dependent variable | Two-week incidence rate | illnessratio | % | Number of injuries per two weeks in every 100 respondents |
| Prevalence of chronic diseases | chronicratio | % | Number of chronic illness cases in every 100 years of age 15 and over | |
| Number of sick days per thousand people | illnessday | day | Average number of sick days in two weeks per 1000 people | |
| Socioeconomic characteristics | Income per capita | income | 10 thousand | Average annual income per capita |
| Average years of education | edu | year | The years required by a respondent to obtain his/her highest degree | |
| Demographic characteristics | Average age in county | average | age | The average age of all age group weighted by group size |
| Older population proportion | age65 | % | Proportion of the population over 65 years old | |
| Male population proportion | male | % | Proportion of male population | |
| Urban flag | urban | Urban = 1, rural = 0 | ||
| Consumption and health service characteristics | Annual consumption | expend | yuan | Total annual consumption per capita |
| Average of medical treatment costs | permedicost | yuan | Average annual medical treatment costs | |
| Average hospitalization expense | perhospitalcost | yuan | Average hospitalization expense of each time | |
| Health expenditure per capita | medicost | yuan | Proportion of family health expenditure to total living expenses | |
| Accessibility and affordability of health services | Accessibility of distance to the nearest hospital | distance | % | Proportion of the population whose distance from the nearest hospital to their home is less than 1 km |
| Accessibility of time to the nearest hospital | time10 | % | Proportion of the population whose time cost to the nearest hospital is less than 10 min | |
| Coverage of social health insurance plans | insurance | % | Proportion of the population covered by social health insurance plans | |
| Environment factor | Hygienic toilets shares | washroom | % | Proportion of hygienic toilets |
| Variables | Mean | Stdev | Min | Pct 25% | Median | Pct 75% | Max |
|---|---|---|---|---|---|---|---|
| NHSS (282 observations in 3 years) | |||||||
| illnessratio | 16.35 | 7.53 | 3.71 | 11.43 | 14.70 | 19.29 | 53.20 |
| illnessday | 1328.88 | 691.82 | 231.00 | 854.75 | 1167.50 | 1589.25 | 4128.00 |
| chronicratio | 14.14 | 6.38 | 2.89 | 9.84 | 12.97 | 17.97 | 33.55 |
| income * | 0.00 | 2.56 | −4.98 | −1.57 | −0.64 | 1.14 | 11.07 |
| income2 | 6.54 | 15.14 | 0.00 | 0.61 | 1.97 | 5.80 | 122.54 |
| edu | 7.39 | 1.91 | 1.70 | 6.15 | 7.00 | 8.74 | 11.65 |
| CHARLS (378 observations in 3 years) | |||||||
| CHRONIC_RATIO | 0.75 | 0.10 | 0.45 | 0.68 | 0.75 | 0.82 | 0.98 |
| AVGINDIINCOME_EARN | 0.44 | 0.32 | 0.03 | 0.21 | 0.35 | 0.59 | 1.81 |
| AVGINDIINCOME_EARN2 | 0.30 | 0.47 | 0.00 | 0.05 | 0.12 | 0.35 | 3.29 |
| AVGEDU | 1.17 | 0.16 | 1.00 | 1.07 | 1.12 | 1.20 | 1.94 |
| NHSS | ||||
| Year | Counties | Illnessratio | Illnessday | Chronicratio |
| 1998 | 94 | 0.2316 | 0.2512 | 0.2790 |
| 2003 | 95 | 0.1998 | 0.2395 | 0.2312 |
| 2008 | 93 | 0.2514 | 0.2837 | 0.2196 |
| CHARLS | ||||
| Year | Cities | CHRONIC_RATIO | ||
| 2011 | 126 | 0.0744 | ||
| 2013 | 126 | 0.0640 | ||
| 2015 | 126 | 0.0511 | ||
| Variable | Individual Fixed Effect (FGLS) ⱡ | Individual Random Effect (FGLS) ⱴ | Two-way Fixed Effect (FGLS) ⱡ | Pooling (FGLS) | Pooling (OLS) |
|---|---|---|---|---|---|
| illnessratio | |||||
| income | −0.3118 | 0.1051 | −0.5214 | −0.2278 | −0.2278 |
| (0.3252) | (0.3149) | (0.3371) | (0.3391) | (0.3391) | |
| income2 | 0.2167 *** | 0.1758 *** | 0.2243 *** | 0.1756 *** | 0.1756 *** |
| (0.0379) | (0.0387) | (0.0378) | (0.0395) | (0.0395) | |
| edu | −0.1521 | 0.6774 | −0.4592 | 0.2953 | 0.2953 |
| (0.5851) | (0.5469) | (0.5938) | (0.5557) | (0.5557) | |
| illnessday | |||||
| income | −13.7166 | 3.3721 | −26.7318 | −34.9995 | −34.9995 |
| (28.7490) | (27.7268) | (30.0394) | (30.0065) | (30.0065) | |
| income2 | 18.7594 *** | 16.8128 *** | 19.0379 *** | 17.7110 *** | 17.7110 *** |
| (3.3440) | (3.3296) | (3.3100) | (3.4914) | (3.4914) | |
| edu | −20.0401 | 62.9851 | −37.8590 | 19.5179 | 19.5179 |
| (53.0576) | (48.5439) | (52.7612) | (49.5975) | (49.5975) | |
| chronicratio | |||||
| income | −0.5160** | −0.4471** | −0.5789** | −0.7147 *** | −0.7147 *** |
| (0.2219) | (0.2074) | (0.2308) | (0.2249) | (0.2249) | |
| income2 | 0.0865 *** | 0.0789 *** | 0.0868 *** | 0.0974 *** | 0.0974 *** |
| (0.0258) | (0.0246) | (0.0254) | (0.0262) | (0.0262) | |
| edu | −0.3765 | 0.0614 | −0.4943 | −0.1397 | −0.1397 |
| (0.4096) | (0.3752) | (0.4054) | (0.3717) | (0.3717) | |
| Variable | Individual Fixed Effect (FGLS) ⱡ | Individual Random Effect (FGLS) ⱴ | Two-way Fixed Effect (FGLS) ⱡ | Pooling (FGLS) | Pooling (OLS) |
|---|---|---|---|---|---|
| CHRONIC_RATIO | |||||
| AVGINDIINCOME_EARN | −0.1982 *** | −0.1724 *** | −0.1482 *** | −0.2609 *** | −0.2609 *** |
| (0.0452) | (0.0342) | (0.0433) | (0.0493) | (0.0493) | |
| AVGINDIINCOME_EARN2 | 0.0882 *** | 0.0792 *** | 0.0670 *** | 0.1081 *** | 0.1081 *** |
| (0.0253) | (0.0187) | (0.0239) | (0.0285) | (0.0285) | |
| AVGEDU | −0.0768 ** | 0.0221 | −0.0509 | 0.0338 | 0.0338 |
| (0.0362) | (0.0405) | (0.0340) | (0.0379) | (0.0379) | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiang, Y.; Zheng, H.; Zhao, T. Socioeconomic Status and Morbidity Rate Inequality in China: Based on NHSS and CHARLS Data. Int. J. Environ. Res. Public Health 2019, 16, 215. https://doi.org/10.3390/ijerph16020215
Jiang Y, Zheng H, Zhao T. Socioeconomic Status and Morbidity Rate Inequality in China: Based on NHSS and CHARLS Data. International Journal of Environmental Research and Public Health. 2019; 16(2):215. https://doi.org/10.3390/ijerph16020215
Chicago/Turabian StyleJiang, Yunyun, Haitao Zheng, and Tianhao Zhao. 2019. "Socioeconomic Status and Morbidity Rate Inequality in China: Based on NHSS and CHARLS Data" International Journal of Environmental Research and Public Health 16, no. 2: 215. https://doi.org/10.3390/ijerph16020215
APA StyleJiang, Y., Zheng, H., & Zhao, T. (2019). Socioeconomic Status and Morbidity Rate Inequality in China: Based on NHSS and CHARLS Data. International Journal of Environmental Research and Public Health, 16(2), 215. https://doi.org/10.3390/ijerph16020215





