A Comparison of Stress Perception in International and Local First Semester Medical Students Using Psychometric, Psychophysiological, and Humoral Methods
Abstract
1. Introduction
2. Materials and Methods
- an oral examination;
- a seminar; and
- a relaxing situation that served as the baseline measurement.
3. Results
3.1. Sample Description
3.2. Differences between International and Local Students
3.3. Differences over the Course of the Semester
3.4. Comparison between Current Sample and Norm Values
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Prins, J.T.; van der Heijden, F.M.; Hoekstra-Weebers, J.E.; Bakker, A.B.; van de Wiel, H.B.; Jacobs, B.; Gazendam-Donofrio, S.M. Burnout, engagement and resident physicians’ self-reported errors. Psychol. Health Med. 2009, 14, 654–666. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; West, C.P.; Satele, D.; Boone, S.; Tan, L.; Sloan, J.; Shanafelt, T.D. Burnout among US medical students, residents, and early career physicians relative to the general US Population. Acad. Med. 2014, 89, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Erschens, R.; Keifenheim, K.E.; Herrmann-Werner, A.; Loda, T.; Schwille-Kiuntke, J.; Bugaj, T.J.; Nikendei, C.; Huhn, D.; Zipfel, S.; Junne, F. Professional burnout among medical students: Systematic literature review and meta-analysis. Med. Teach. 2018, 14, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lee, R.T.; Ashforth, B.E. On the meaning of maslach’s three dimensions of burnout. J. Appl. Psychol. 1990, 75, 743–747. [Google Scholar] [CrossRef] [PubMed]
- Maslach, C.; Jackson, S.E. Maslach Burnout Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1981. [Google Scholar]
- Voltmer, E.; Rosta, J.; Aasland, O.G.; Spahn, C. Study-related health and behavior patterns of medical students: A longitudinal study. Med. Teach. 2010, 32, 422–428. [Google Scholar] [CrossRef] [PubMed]
- Erschens, R.; Herrmann-Werner, A.; Keifenheim, K.E.; Loda, T.; Bugaj, T.J.; Nikendei, C.; Lammerding-Köppel, M.; Zipfel, S.; Junne, F. Differential determination of perceived stress in medical students and high-school graduates due to private and training-related stressors. PLoS ONE 2018. [Google Scholar] [CrossRef] [PubMed]
- Dyrbye, L.N.; Thomas, M.R.; Huntington, J.L. Personal life events and medical student burnout: A multicenter study. Acad. Med. 2006, 81, 374–384. [Google Scholar] [CrossRef]
- Ishak, W.W.; Lederer, S.; Mandili, C.; Nikravesh, R.; Seligman, L.; Vasa, M.; Ogunyemi, D.; Bernstein, C.A. Burnout during residency training: A literature review. J. Grad. Med. Educ. 2009, 1, 236–242. [Google Scholar] [CrossRef]
- McManus, I.C.; Livingston, G.; Katona, C. The attractions of medicine: The generic motivations of medical school applicants in relation to demography, personality and achievement. BMC Med. Educ. 2006, 6, 11. [Google Scholar] [CrossRef]
- Herrmann-Werner, A.; Junne, F.; Stuber, F.; Huhn, D.; Nikendei, C.; Seifried-Dubon, T.; Zipfel, S.; Erschens, R. Reducing stress and promoting social integration of international medical students through a tandem program: Results of a prospective-program evaluation. Int. J. Environ. Res. Public Health 2018, 15, 1959. [Google Scholar] [CrossRef]
- Andrade, M.S. International students in english-speaking universities. Adjustment factors. J. Res. Int. Educ. 2006, 5, 131–154. [Google Scholar] [CrossRef]
- Sawir, E. Language difficulties of international students in australia: The effects of prior learning experience. Int. Educ. J. 2005, 6, 567–580. [Google Scholar]
- Shields, P.H. A survey and analysis of student academic support programs in medical schools focus: Underrepresented minority students. J. Natl. Med. Assoc. 1994, 86, 373–377. [Google Scholar] [PubMed]
- McManus, I.C.; Richards, P.; Winder, B.C.; Sproston, K.A.; Styles, V. Medical school applicants from ethnic minority groups: Identifying if and when they are disadvantaged. BMJ 1995, 310, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Kurré, J.; Scholl, J.; Bullinger, M.; Petersen-Ewert, C. Integration and health-related quality of life of undergraduate medical students with migration backgrounds—Results of a survey. Ger. Med. Sci. Psycho-Soc. Med. 2011, 8, Doc7. [Google Scholar]
- Camm, A.J.M.M.; Malik, M.; Bigger, J.T.G.B.; Breithardt, G.; Cerutti, S.; Cohen, R.; Coumel, P.; Fallen, E.; Kennedy, H.; Kleiger, R.E.; et al. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circ. J. 1996, 93, 1043–1065. [Google Scholar]
- Hottenrott, K. Training with the Heart Rate Monitor; Meyer & Meyer Sport: Aachen, Germany, 2007. [Google Scholar]
- Bigger, J.T.; Fleiss, J.L.; Steinman, R.C.; Rolnitzky, L.M.; Kleiger, R.E.; Rottman, J.N. Frequency domain measures of heart period variability and mortality after myocardial infarction. Circ. J. 1992, 85, 164–171. [Google Scholar] [CrossRef]
- Mazurak, N.; Stein, J.; Kipphan, S.; Muth, E.R.; Teufel, M.; Zipfel, S.; Enck, P. Heart rate variability in anorexia nervosa and the irritable bowel syndrome. Neurogastroenterol. Motil. 2011, 23, 470–478. [Google Scholar] [CrossRef]
- Kofman, O.; Meiran, N.; Greenberg, E.; Balas, M.; Cohen, H. Enhanced performance on executive functions associated with examination stress: Evidence from task-switching and Stroop paradigms. Cogn. Emot. 2006, 20, 577–595. [Google Scholar] [CrossRef]
- Dimitriev, D.A.; Saperova, E.V.; Dimitriev, A.D. State anxiety and nonlinear dynamics of heart rate variability in students. PLoS ONE 2016, 11. [Google Scholar] [CrossRef]
- Sapolsky, R.M.; Romero, L.M.; Munck, A.U. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocr. Rev. 2000, 21, 55–89. [Google Scholar] [CrossRef] [PubMed]
- Weiner, H. Perturbing the Organism: The Biology of Stressful Experience; University of Chicago Press: Chicago, IL, USA, 1992. [Google Scholar]
- Miller, G.E.; Chen, E.; Zhou, E. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol. Bull. 2007, 133, 25–45. [Google Scholar] [CrossRef] [PubMed]
- McEwen, B.S. The neurobiology of stress: From serendipity to clinical relevance. Brain Res. 2000, 886, 172–189. [Google Scholar] [CrossRef]
- Heim, C.; Ehlert, U.; Hellhammer, D. The potential role of hypocortisolism in the pathophysiology of stress-related bodily disorders. Psychoneuroendocrinology 2000, 25, 1–35. [Google Scholar] [CrossRef]
- Kirschbaum, C.; Tietze, A.; Skoluda, N.; Dettenborn, L. Hair as a retrospective calendar of cortisol production—Increased cortisol incorporation into hair in the third trimester of pregnancy. Psychoneuroendocrinology 2009, 24, 32–37. [Google Scholar] [CrossRef] [PubMed]
- Stalder, T.; Kirschbaum, C. Analysis of cortisol in hair—State of the art and future directions. Brain Behav. Immun. 2012, 26, 1019–1029. [Google Scholar] [CrossRef] [PubMed]
- Dowlati, Y.; Herrmann, N.; Swardfager, W.; Thomson, S.; Oh, P.I.; van Uum, S.; Koren, G.; Lactôt, K. Relationship between hair cortisol concentrations and depressive symptoms in patients with coronary artery disease. Neuropsychiatr. Dis. Treat. 2010, 6, 393–400. [Google Scholar]
- Huhn, D.; Eckart, W.; Karimian-Jazi, K.; Amr, A.; Herzog, W.; Nikendei, C. Voluntary peer-led exam preparation course for international first year students: Tutees’ perceptions. BMC Med. Educ. 2015, 15. [Google Scholar] [CrossRef]
- Maslach, C.; Jackson, S.E.; Leiter, M.P. Maslach burnout inventory. In Manual, 3rd ed.; Consulting Psychologists Press: Palo Alto, CA, USA, 1996. [Google Scholar]
- Schaufeli, W.B.; Martínez, I.M.; Pinto, A.M.; Salanova, M.; Bakker, A.B. Burnout and engagement in university students. A cross-national study. J. Cross-Cult. Psychol. 2002, 33, 464–481. [Google Scholar] [CrossRef]
- Gumz, A.; Erices, R.; Brähler, E.; Zenger, M. Factorial structure and psychometric criteria of the German translation of the Maslach burnout inventory—Student version by schaufeli et al. (mbi-ss). Psychother. Psychosom. Med. Psychol. 2013, 63, 77–84. [Google Scholar]
- Levenstein, S.; Prantera, C.; Varvo, V.; Scribano, M.L.; Berto, E.; Luzi, C.; Andreoli, A. Development of the perceived stress questionnaire: A new tool for psychosomatic research. J. Psychosom. Res. 1993, 37, 19–32. [Google Scholar] [CrossRef]
- Fliege, H.; Rose, M.; Arck, P.; Levenstein, S.; Klapp, B.F. Validation of the “perceived stress questionnaire” (PSQ) in a german sample. Diagnostica 2001, 47, 142–152. [Google Scholar] [CrossRef]
- Löwe, B.; Spitzer, R.L.; Zipfel, S.; Herzog, W. Gesundheitsfragebogen für Patienten (PHQ-D). Available online: https://www.klinikum.uni-heidelberg.de/fileadmin/Psychosomatische_Klinik/pdf_Material/PHQ_Komplett_Fragebogen1.pdf (accessed on 6 December 2018).
- Gräfe, K.; Zipfel, S.; Herzog, W.; Löwe, B. Screening psychischer störungen mit dem “gesundheitsfragebogen für patienten (PHQ-D)”. Diagnostica 2004, 50, 171–181. [Google Scholar] [CrossRef]
- Hojat, M.; Mangione, S.; Nasca, T.J.; Cohen, M.J.M.; Gonnella, J.S.; Erdmann, J.B. The Jefferson scale of physician empathy: Development and preliminary psychometric data. Educ. Psychol. Meas. 2001, 61, 349–365. [Google Scholar] [CrossRef]
- Neumann, M.; Scheffer, C.; Tauschel, D.; Lutz, G.; Wirtz, M.; Edelhäuser, F. Physician empathy: Definition, outcome-relevance and its measurement in patient care and medical education. GMS J. Med. Educ. 2012, 29, Doc11. [Google Scholar]
- Schwarzer, R.; Jerusalem, M. Generalized self-efficacy scale. In Measures in Health Psychology: A User’s Portfolio; Nfer-Nelson: Windsor, UK, 1995; pp. 35–37. [Google Scholar]
- Hinz, A.; Schumacher, J.; Albani, C.; Schmid, G.; Brähler, E. Standardization of the general self-efficacy scale in the German population. Diagnostica 2006, 52, 26–32. [Google Scholar] [CrossRef]
- Giles, D.; Draper, N.; Neil, W. Validity of the polar v800 heart rate monitor to measure RR intervals at rest. Eur. J. Appl. Physiol. 2016, 116, 563–571. [Google Scholar] [CrossRef]
- World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. J. Am. Med. Assoc. 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Cohen, J. A power primer. Psychol. Bull. 1992, 112, 155–159. [Google Scholar] [CrossRef]
- Rief, W.; Nanke, A.; Klaiberg, A.; Braehler, E. Base rates for panic and depression according to the brief patient health questionnaire: A population-based study. J. Affect. Disord. 2004, 82, 271–276. [Google Scholar] [CrossRef]
- Preusche, I.; Wagner-Menghin, M. Rising to the challenge: Cross-cultural adaptation and psychometric evaluation of the adapted German version of the Jefferson scale of physician empathy for students (JSPR-s). Adv. Health Sci. Educ. 2013, 18, 573–587. [Google Scholar] [CrossRef] [PubMed]
- Agelink, M.W.; Malessa, R.; Baumann, B.; Majewski, T.; Akila, F.; Zeit, T.; Ziegler, D. Standardized tests of heart rate variability: Normal ranges obtained from 309 healthy humans, and effects of age, gender, and heart rate. Clin. Autonomic Res. Off. J. Clin. Autonomic Res. Soc. 2001, 11, 99–108. [Google Scholar] [CrossRef]
- Abell, J.G.; Stalder, T.; Ferrie, J.E.; Shipley, M.J.; Kirschbaum, C.; Kivimäki, M.; Kumari, M. Assessing cortisol from hair samples in a large observational cohort: The Whitehall II study. Psychoneuroendocrinology 2016, 73, 148–156. [Google Scholar] [CrossRef] [PubMed]
- Bugaj, T.J.; Müksch, C.; Ehrenthal, J.C.; Köhl-Hackert, N.; Schauenburg, H.; Huber, J.; Schmid, C.; Erschens, R.; Junne, F.; Herzog, W.; et al. Stress in medical students: A cross-sectional study on the relevance of attachment style and structural integration. Psychother. Psych. Med. 2016, 66, 88–92. [Google Scholar] [CrossRef]
- Koehl-Hackert, N.; Schultz, J.-H.; Nikendei, C.; Moltner, A.; Gedrose, B.; van den Bussche, H.; Junger, J. Belastet in den Beruf—Empathie und Burnout bei Medizinstudierenden am Ende des Praktischen Jahres [Burdened into the job—Final-year students’ empathy and burnout]. Z. Evidenz Fortbild. Qual. Gesundheitswesen 2012, 106, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Huhn, D.; Huber, J.; Ippen, F.M.; Eckart, W.; Junne, F.; Zipfel, S.; Herzog, W.; Nikendei, C. International medical students’ expectations and worries at the beginning of their medical education: A qualitative focus group study. BMC Med. Educ. 2016, 16, 33. [Google Scholar] [CrossRef] [PubMed]
- Galchenko, I.; van de Vijver, F.J.R. The role of perceived cultural distance in the acculturation of exchange students in Russia. Int. J. Intercult. Relat. 2007, 31, 181–197. [Google Scholar] [CrossRef]
- Huhn, D.; Resch, F.; Duelli, R.; Moltner, A.; Huber, J.; Karimian Jazi, K.; Amr, A.; Eckart, W.; Herzog, W.; Nikendei, C. Examination performances of German and international medical students in the preclinical studying-term—A descriptive study. GMS J. Med. Educ. 2014, 31, Doc29. [Google Scholar]
- Wass, V.; Roberts, C.; Hoogenboom, R.; Jones, R.; Van der Vleuten, C. Effect of ethnicity on performance in a final objective structured clinical examination: Qualitative and quantitative study. BMJ 2003, 326, 800–803. [Google Scholar] [CrossRef]
- Haq, I.; Higham, J.; Morris, R.; Dacre, J. Effect of ethnicity and gender on performance in undergraduate medical examinations. Med. Educ. 2005, 39, 1126–1128. [Google Scholar] [CrossRef]
- Woolf, K.; Haq, I.; McManus, I.C.; Higham, J.; Dacre, J. Exploring the underperformance of male and minority ethnic medical students in first year clinical examinations. Adv. Health Sci. Educ. Theory Prac. 2008, 13, 607–616. [Google Scholar] [CrossRef] [PubMed]
- Liddell, M.J.; Koritsas, S. Effect of medical students’ ethnicity on their attitudes towards consultation skills and final year examination performance. Med. Educ. 2004, 38, 187–198. [Google Scholar] [CrossRef]
- Ferguson, E.; James, D.; Madeley, L. Learning in practice. Factors associated with success in medical school: Systematic review of the literature. BMJ 2002, 324, 952–957. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Page, L.; Zhang, K.; Steinecke, A.; Beaudreau, J.; Moses, A.; Terrell, C. Minorities in Medical Education; Association of American Medical Colleges: Washington, DC, USA, 2005. [Google Scholar]
- Neumann, M.; Edelhäuser, F.; Tauschel, D.; Fischer, M.R.; Wirtz, M.; Woopen, C.; Haramati, A.; Scheffer, C. Empathy decline and its reasons: A systematic review of studies with medical students and residents. Acad. Med. 2011, 86, 996–1009. [Google Scholar] [CrossRef] [PubMed]
- Sayers, B.M. Analysis of heart rate variability. Ergonomics 1973, 16, 17–32. [Google Scholar] [PubMed]
- Staufenbiel, S.M.; Penninx, B.W.; Spijker, A.T.; Elzinga, B.M.; van Rossum, E.F. Hair cortisol, stress exposure, and mental health in humans: A systematic review. Psychoneuroendocrinology 2013, 38, 1220–1235. [Google Scholar] [CrossRef] [PubMed]


| Students’ Cultural Background | N | Male | Female | Mage | SDage |
|---|---|---|---|---|---|
| Local | 20 | 7 | 13 | 19.80 | 2.12 |
| International | 17 | 7 | 10 | 20.67 | 3.94 |
| All | 37 | 14 | 23 | 20.21 | 3.10 |
| International Students’ Origin | |||||
| Europe | 6 | ||||
| Southeast Asia | 4 | ||||
| Latin America | 3 | ||||
| Middle East | 2 | ||||
| Africa | 1 | ||||
| South Asia | 1 |
| Psychometric Measure | Nationality | N | MT1 | SDT1 | Mean Rank | Rank-Sum | U | r | MT2 | SDT2 | Mean Rank | Rank-Sum | U | r | MT3 | SDT3 | Mean Rank | Rank-Sum | U | r |
| MBI, ‘emotional exhaustion’ | local | 20 | 2.12 | 0.93 | 17.60 | 352.0 | −0.856 | 0.14 | 2.46 | 1.02 | 22.08 | 441.5 | −1.510 | 0.25 | 2.35 | 1.20 | 21.00 | 420.0 | −1.596 | 0.27 |
| international | 16 | 2.40 | 1.00 | 20.65 | 351.0 | 1.73 | 1.05 | 16.64 | 299.5 | 1.66 | 1.04 | 15.38 | 246.0 | |||||||
| MBI, ‘cynicism’ | local | 20 | 0.41 | 0.73 | 19.13 | 382.5 | −0.087 | 0.01 | 0.64 | 0.95 | 21.00 | 420.0 | −0.930 | 0.16 | 0.69 | 0.89 | 21.60 | 432.0 | −2.140 | 0.36 |
| international | 16 | 0.53 | 0.93 | 18.85 | 320.5 | 0.28 | 0.54 | 17.83 | 321.0 | 0.23 | 0.49 | 14.63 | 234.0 | |||||||
| MBI, ‘professional efficacy’ | local | 20 | 4.65 | 0.71 | 16.75 | 335.0 | −1.378 | 0.23 | 4.60 | 0.71 | 23.08 | 461.5 | −2.096 | 0.35 | 4.67 | 0.86 | 22.13 | 442.5 | −2.314 | 0.39 |
| international | 16 | 4.94 | 0.61 | 21.65 | 368.0 | 3.92 | 1.07 | 15.53 | 279.5 | 3.97 | 0.92 | 13.97 | 223.5 | |||||||
| PSQ-20 | local | 20 | 0.42 | 0.08 | 17.43 | 348.5 | −0.962 | 0.16 | 0.42 | 0.72 | 19.95 | 399.0 | −0.582 | 0.10 | 0.43 | 0.13 | 18.85 | 377.0 | −0.224 | 0.04 |
| international | 16 | 0.44 | 0.11 | 20.85 | 354.5 | 0.41 | 0.12 | 17.88 | 304.0 | 0.41 | 0.08 | 18.06 | 289.0 | |||||||
| JSPE-S | local | 20 | 111.85 | 10.19 | 22.53 | 450.5 | −2.154 | 0.36 | 110.60 | 11.34 | 22.15 | 443.0 | −1.921 | 0.32 | 110.35 | 10.77 | 22.50 | 450.0 | −2.549 | 0.42 |
| international | 16 | 101.86 | 14.51 | 14.85 | 252.5 | 99.75 | 15.81 | 15.29 | 260.0 | 100.19 | 15.37 | 13.50 | 216.0 | |||||||
| PHQ-9 | local | 20 | 4.65 | 3.54 | 19.90 | 398.0 | −0.553 | 0.09 | 4.60 | 3.17 | 22.88 | 457.5 | −2.385 | 0.40 | 4.45 | 3.20 | 22.63 | 452.5 | −2.665 | 0.44 |
| international | 16 | 4.19 | 3.02 | 17.94 | 305.0 | 1.88 | 2.47 | 14.44 | 245.5 | 1.94 | 2.72 | 13.34 | 213.5 | |||||||
| GSE | local | 20 | 29.73 | 3.35 | 17.68 | 353.5 | −0.812 | 0.14 | 30.35 | 4.45 | 18.28 | 365.5 | −0.444 | 0.07 | 31.95 | 4.11 | 18.98 | 379.5 | −0.304 | 0.05 |
| international | 16 | 30.50 | 3.54 | 20.56 | 349.5 | 30.75 | 3.84 | 19.85 | 337.5 | 32.19 | 4.02 | 17.91 | 286.5 | |||||||
| Psychophysiological measure | Nationality | N | Mrest | SDrest | Mean Rank | Rank-Sum | U | r | Mseminar | SDseminar | Mean Rank | Rank-Sum | U | r | Mexam | SDexam | Mean Rank | Rank-Sum | U | r |
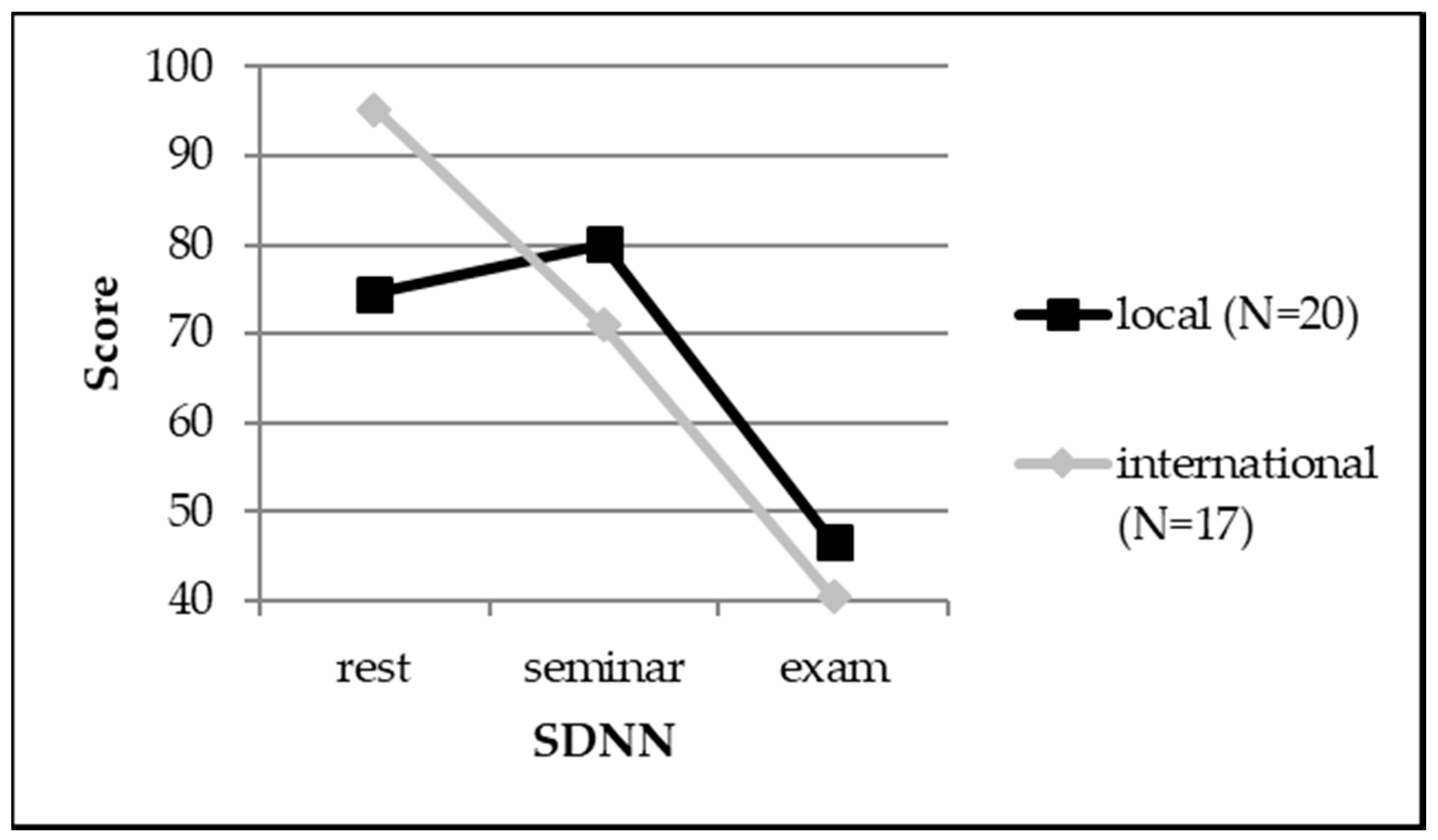
| SDNN (ms) | local | 20 | 74.56 | 26.24 | 16.20 | 324.0 | −1.707 | 0.28 | 80.13 | 30.86 | 20.70 | 414.0 | −1.036 | 0.17 | 46.58 | 19.94 | 20.25 | 405.0 | −0.762 | 0.13 |
| international | 17 | 95.20 | 40.37 | 22.29 | 379.0 | 70.94 | 28.52 | 17.00 | 289.0 | 40.46 | 17.15 | 17.53 | 298.0 | |||||||
| RMSSD (ms) | local | 20 | 59.45 | 35.31 | 18.40 | 368.0 | −0.366 | 0.06 | 47.21 | 29.68 | 19.90 | 398.0 | −0.549 | 0.09 | 15.47 | 9.25 | 19.75 | 395.0 | −0.457 | 0.08 |
| international | 17 | 60.25 | 29.56 | 19.71 | 335.0 | 38.64 | 17.74 | 17.94 | 305.0 | 13.72 | 7.61 | 18.12 | 308.0 | |||||||
| pNN50 (%) | local | 20 | 30.85 | 24.64 | 18.30 | 366.0 | −0.427 | 0.07 | 21.95 | 20.23 | 19.90 | 398.0 | −0.549 | 0.09 | 2.28 | 2.83 | 20.35 | 407.0 | −0.823 | 0.14 |
| international | 17 | 31.58 | 19.69 | 19.82 | 337.0 | 16.31 | 12.77 | 17.94 | 305.0 | 1.65 | 2.14 | 17.41 | 296.0 | |||||||
| LF (ms²) | local | 20 | 1716 | 1409 | 17.75 | 355.0 | −0.762 | 0.13 | 1784 | 1250 | 19.15 | 383.0 | −0.091 | 0.02 | 840.0 | 660.1 | 20.35 | 407.0 | −0.823 | 0.14 |
| international | 17 | 1932 | 1409 | 20.47 | 348.0 | 1782 | 1636 | 18.82 | 320.0 | 654.8 | 644.5 | 17.41 | 296.0 | |||||||
| HF (ms²) | local | 20 | 1657 | 1941 | 17.70 | 354.0 | −0.792 | 0.13 | 1163 | 1509 | 18.75 | 375.0 | −0.152 | 0.03 | 165.1 | 193.7 | 19.80 | 396.0 | −0.488 | 0.08 |
| international | 17 | 1655 | 1582 | 20.53 | 349.0 | 785 | 866 | 19.29 | 328.0 | 136.3 | 138.6 | 18.06 | 307.0 | |||||||
| LF/HF | local | 20 | 2.28 | 1.93 | 19.20 | 384.0 | −0.122 | 0.02 | 3.62 | 2.37 | 20.45 | 409.0 | −0.884 | 0.15 | 7.52 | 5.16 | 19.95 | 399.0 | −0.579 | 0.10 |
| international | 17 | 2.04 | 1.64 | 18.76 | 319.0 | 3.02 | 2.14 | 17.29 | 294.0 | 6.21 | 2.84 | 17.88 | 304.0 | |||||||
| Humoral measure | Nationality | N | MT1 | SDT1 | Mean Rank | Rank-Sum | U | r | MT2 | SDT2 | Mean Rank | Rank-Sum | U | r | ||||||
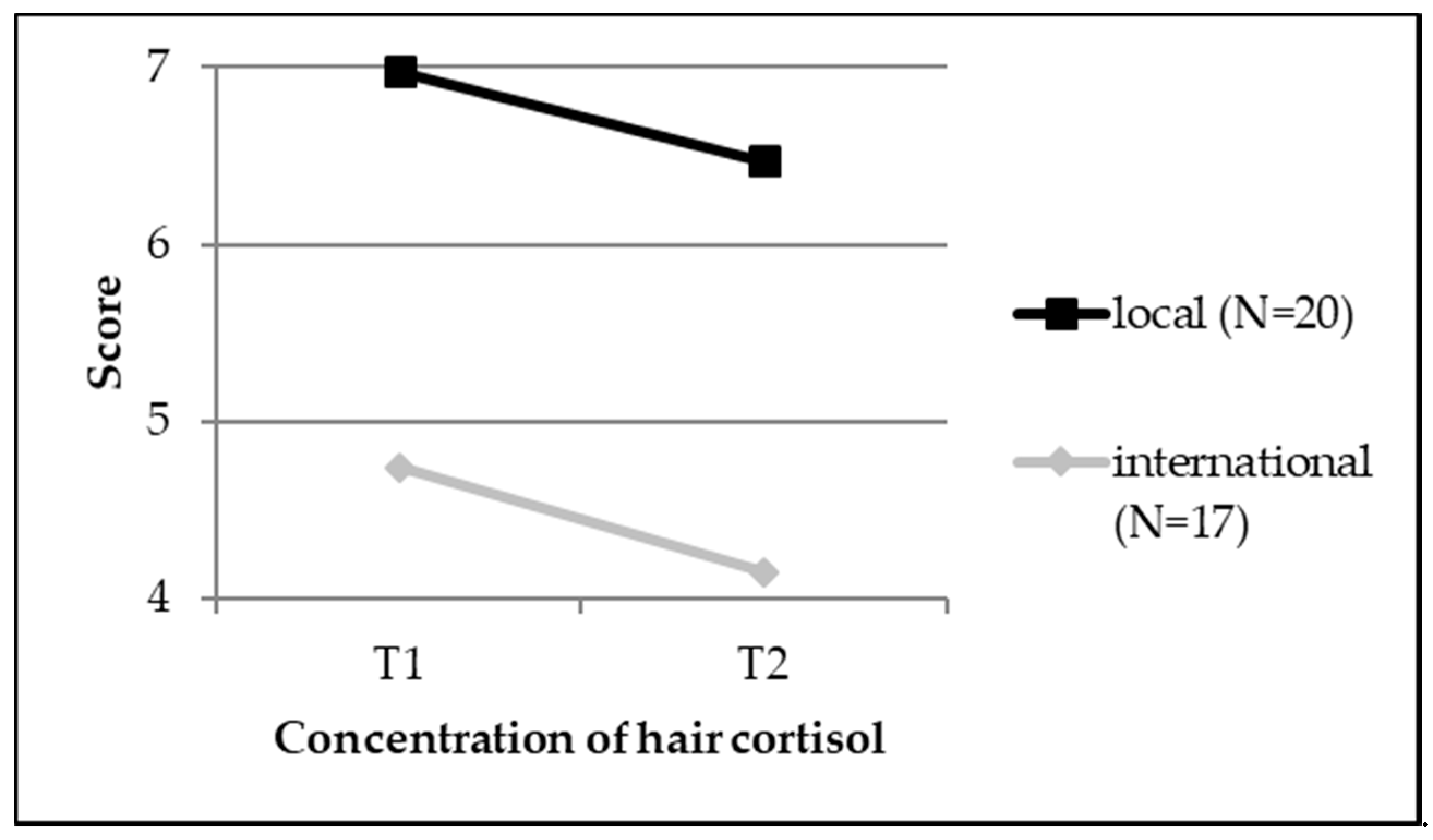
| Hair cortisol (pg/mg) | local | 20 | 6.98 | 7.53 | 20.50 | 410.0 | −0.585 | 0.10 | 6.47 | 5.12 | 21.25 | 425.0 | −1.371 | 0.23 | ||||||
| international | 17 | 4.74 | 2.53 | 18.39 | 331.0 | 4.15 | 2.27 | 16.35 | 278.0 |
| Psychometric Measure | Nationality | N | MT1 | SDT1 | Mean Rank | MT2 | SDT2 | Mean Rank | MT3 | SDT3 | Mean Rank | df | Chi2 |
| MBI, ‘emotional exhaustion’ | local | 20 | 2.12 | 0.93 | 1.93 | 2.46 | 1.02 | 2.18 | 2.35 | 1.20 | 1.90 | 2 | 0.97 |
| international | 16 | 2.40 | 1.00 | 2.59 | 1.73 | 1.05 | 1.75 | 1.66 | 1.04 | 1.66 | 2 | 9.56 | |
| MBI, ‘cynicism’ | local | 20 | 0.41 | 0.73 | 1.68 | 0.64 | 0.95 | 2.05 | 0.69 | 0.89 | 2.28 | 2 | 5.65 |
| international | 16 | 0.53 | 0.93 | 2.16 | 0.28 | 0.54 | 1.84 | 0.23 | 0.49 | 2.00 | 2 | 1.67 | |
| MBI, ‘professional efficacy’ | local | 20 | 4.65 | 0.71 | 2.03 | 4.60 | 0.71 | 1.80 | 4.67 | 0.86 | 2.18 | 2 | 1.54 |
| international | 16 | 4.94 | 0.61 | 2.78 | 3.92 | 1.07 | 1.50 | 3.97 | 0.92 | 1.72 | 2 | 16.03 | |
| PSQ-20 | local | 20 | 0.42 | 0.08 | 1.95 | 0.42 | 0.12 | 2.03 | 0.43 | 0.13 | 2.03 | 2 | 0.076 |
| international | 16 | 0.44 | 0.11 | 2.31 | 0.41 | 0.12 | 1.91 | 0.41 | 0.08 | 1.78 | 2 | 2.59 | |
| JSPE-S | local | 20 | 111.85 | 10.19 | 2.00 | 110.60 | 11.34 | 2.08 | 110.35 | 10.77 | 1.93 | 2 | 0.25 |
| international | 16 | 101.86 | 14.51 | 2.19 | 99.75 | 15.81 | 1.94 | 100.19 | 15.37 | 1.88 | 2 | 0.90 | |
| PHQ-9 | local | 20 | 4.65 | 3.54 | 1.95 | 4.60 | 3.17 | 2.05 | 4.45 | 3.20 | 2.00 | 2 | 0.12 |
| international | 16 | 4.19 | 3.02 | 2.72 | 1.88 | 2.47 | 1.69 | 1.94 | 2.72 | 1.59 | 2 | 14.25 | |
| GSE | local | 20 | 29.73 | 3.35 | 1.65 | 30.35 | 4.45 | 1.90 | 31.95 | 4.11 | 2.45 | 2 | 8.12 |
| international | 16 | 30.50 | 3.54 | 1.63 | 30.75 | 3.84 | 1.81 | 32.19 | 4.02 | 2.56 | 2 | 9.00 | |
| Psychophysiological Measure | Nationality | N | Mrest | SDrest | Mean Rank | Mseminar | SDseminar | Mean Rank | Mexam | SDexam | Mean Rank | df | Chi2 |
| SDNN (ms) | local | 20 | 74.56 | 26.24 | 2.25 | 80.13 | 30.86 | 2.45 | 46.58 | 19.94 | 1.30 | 2 | 15.10 * |
| international | 17 | 95.20 | 40.37 | 2.76 | 70.94 | 28.52 | 2.00 | 40.46 | 17.15 | 1.24 | 2 | 19.88 * | |
| RMSSD (ms) | local | 20 | 59.45 | 35.31 | 2.65 | 47.21 | 29.68 | 2.30 | 15.47 | 9.25 | 1.05 | 2 | 28.30 * |
| international | 17 | 60.25 | 29.56 | 2.82 | 38.64 | 17.74 | 2.12 | 13.72 | 7.61 | 1.06 | 2 | 26.82 * | |
| pNN50 (%) | local | 20 | 30.85 | 24.64 | 2.75 | 21.95 | 20.23 | 2.15 | 2.28 | 2.83 | 1.10 | 2 | 27.90 * |
| international | 17 | 31.58 | 19.69 | 2.71 | 16.31 | 12.77 | 2.12 | 1.65 | 2.14 | 1.18 | 2 | 20.24 * | |
| LF (ms²) | local | 20 | 1716 | 1409 | 2.35 | 1784 | 1250 | 2.30 | 840.0 | 660.1 | 1.35 | 2 | 12.70 * |
| international | 17 | 1932 | 1409 | 2.53 | 1782 | 1636 | 2.24 | 654.8 | 644.5 | 1.24 | 2 | 15.65 * | |
| HF (ms²) | local | 20 | 1657 | 1941 | 2.65 | 1163 | 1509 | 2.30 | 165.1 | 193.7 | 1.05 | 2 | 28.30 * |
| international | 17 | 1655 | 1582 | 2.76 | 785 | 866 | 2.06 | 136.3 | 138.6 | 1.18 | 2 | 21.53 * | |
| LF/HF | local | 20 | 2.28 | 1.93 | 1.30 | 3.62 | 2.37 | 1.90 | 7.52 | 5.16 | 2.80 | 2 | 22.80 * |
| international | 17 | 2.04 | 1.64 | 1.24 | 3.02 | 2.14 | 1.82 | 6.21 | 2.84 | 2.94 | 2 | 25.53 * | |
| Humoral measure | Nationality | N | MT1 | SDT1 | Mean Rank | MT2 | SDT2 | Mean Rank | df | Chi2 | |||
| Hair cortisol (pg/mg) | local | 20 | 6.98 | 7.53 | 1.50 | 6.47 | 5.12 | 1.50 | 1 | 0.00 | |||
| international | 17 | 4.74 | 2.53 | 1.59 | 4.15 | 2.27 | 1.41 | 1 | 0.53 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huhn, D.; Schmid, C.; Erschens, R.; Junne, F.; Herrmann-Werner, A.; Möltner, A.; Herzog, W.; Nikendei, C. A Comparison of Stress Perception in International and Local First Semester Medical Students Using Psychometric, Psychophysiological, and Humoral Methods. Int. J. Environ. Res. Public Health 2018, 15, 2820. https://doi.org/10.3390/ijerph15122820
Huhn D, Schmid C, Erschens R, Junne F, Herrmann-Werner A, Möltner A, Herzog W, Nikendei C. A Comparison of Stress Perception in International and Local First Semester Medical Students Using Psychometric, Psychophysiological, and Humoral Methods. International Journal of Environmental Research and Public Health. 2018; 15(12):2820. https://doi.org/10.3390/ijerph15122820
Chicago/Turabian StyleHuhn, Daniel, Carolin Schmid, Rebecca Erschens, Florian Junne, Anne Herrmann-Werner, Andreas Möltner, Wolfgang Herzog, and Christoph Nikendei. 2018. "A Comparison of Stress Perception in International and Local First Semester Medical Students Using Psychometric, Psychophysiological, and Humoral Methods" International Journal of Environmental Research and Public Health 15, no. 12: 2820. https://doi.org/10.3390/ijerph15122820
APA StyleHuhn, D., Schmid, C., Erschens, R., Junne, F., Herrmann-Werner, A., Möltner, A., Herzog, W., & Nikendei, C. (2018). A Comparison of Stress Perception in International and Local First Semester Medical Students Using Psychometric, Psychophysiological, and Humoral Methods. International Journal of Environmental Research and Public Health, 15(12), 2820. https://doi.org/10.3390/ijerph15122820





