Differing Contributions of Classical Risk Factors to Type 2 Diabetes in Multi-Ethnic Malaysian Populations
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Samples
2.2. Risk Factor Selection
2.3. Questionnaire-Derived Variables
2.4. Anthropometric Measurements
2.5. Missing Data Handling
2.6. Statistical Analyses
3. Results
History of Diabetes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. IDF Diabetes Atlas, 8th ed.; International Diabetes Federation: Brussels, Belgium, 2017. [Google Scholar]
- Hu, F.B. Globalization of diabetes: The role of diet, lifestyle, and genes. Diabetes Care 2011, 34, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.C.; Malik, V.; Jia, W.; Kadowaki, T.; Yajnik, C.S.; Yoon, K.H.; Hu, F.B. Diabetes in Asia: Epidemiology, risk factors, and pathophysiology. JAMA 2009, 301, 2129–2140. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, N.; Attia, J.; Oldmeadow, C.; Scott, R.J.; Holliday, E.G. The architecture of risk for type 2 diabetes: Understanding Asia in the context of global findings. Int. J. Endocrinol. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- McEvoy, C.T.; Cardwell, C.R.; Woodside, J.V.; Young, I.S.; Hunter, S.J.; McKinley, M.C. A Posteriori Dietary Patterns Are Related to Risk of Type 2 Diabetes: Findings from a Systematic Review and Meta-Analysis. J. Acad. Nutr. Diet. 2014, 114, 1759–1775. [Google Scholar] [CrossRef] [PubMed]
- Misra, A.; Sharma, R.; Gulati, S.; Joshi, S.R.; Sharma, V.; Ibrahim, A.; Joshi, S.; Laxmaiah, A.; Kurpad, A.; Raj, R.K.; et al. Consensus dietary guidelines for healthy living and prevention of obesity, the metabolic syndrome, diabetes, and related disorders in Asian Indians. Diabetes Technol. Ther. 2011, 13, 683–694. [Google Scholar]
- Wang, Y.; Mi, J.; Shan, X.Y.; Wang, Q.; Ge, K.Y. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. Int. J. Obes. 2007, 31, 177–188. [Google Scholar] [CrossRef]
- Weeratunga, P.; Jayasinghe, S.; Perera, Y.; Jayasena, G.; Jayasinghe, S. Per capita sugar consumption and prevalence of diabetes mellitus—Global and regional associations. BMC Public Health 2014, 14, 186. [Google Scholar]
- Ramachandran, A.; Snehalatha, C.; Baskar, A.D.; Mary, S.; Kumar, C.K.; Selvam, S.; Catherine, S.; Vijay, V. Temporal changes in prevalence of diabetes and impaired glucose tolerance associated with lifestyle transition occurring in the rural population in India. Diabetologia 2004, 47, 860–865. [Google Scholar]
- Ng, S.W.; Norton, E.C.; Popkin, B.M. Why have physical activity levels declined among Chinese adults? Findings from the 1991–2006 China Health and Nutrition Surveys. Soc. Sci. Med. 2009, 68, 1305–1314. [Google Scholar] [CrossRef]
- Chen, Z.; Pereira, M.A.; Seielstad, M.; Koh, W.P.; Tai, E.S.; Teo, Y.Y.; Liu, J.; Hsu, C.; Wang, R.; Odegaard, A.O.; et al. Joint effects of known type 2 diabetes susceptibility Loci in genome-wide association study of singapore chinese: The singapore chinese health study. PLoS ONE 2014, 9, e87762. [Google Scholar]
- Chen, P.; Takeuchi, F.; Lee, J.Y.; Li, H.; Wu, J.Y.; Liang, J.; Long, J.; Tabara, Y.; Goodarzi, M.O.; Pereira, M.A.; et al. Multiple nonglycemic genomic loci are newly associated with blood level of glycated hemoglobin in East Asians. Diabetes 2014, 63, 2551–2562. [Google Scholar] [CrossRef] [PubMed]
- Institute for Public Health. National Health and Morbidity Survey (NHMS) 2015; Institute for Public Health, Ministry of Health: Kuala Lumpur, Malaysia, 2015. [Google Scholar]
- International Diabetes Federation. IDF Diabetes Atlas, 7th ed.; International Diabetes Federation: Brussels, Belgium, 2015. [Google Scholar]
- Department of Statistics Malaysia. Population Distribution and Basic Demographic Characteristics 2010; Department of Statistics Malaysia: Putrajaya, Malaysia, 2011.
- Jamal, R.; Syed Zakaria, S.Z.; Kamaruddin, M.A.; Jalal, A.N.; Ismail, N.; Kamil, N.M.; Abdullah, N.; Baharudin, N.; Hussin, N.H.; Othman, H.; et al. The Malaysian Cohort Group, Cohort profile: The Malaysian Cohort (TMC) project: A prospective study of non-communicable diseases in a multi-ethnic population. Int. J. Epidemiol. 2014, 44, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, N.; Abdul Murad, N.A.; Attia, J.; Oldmeadow, C.; Mohd Haniff, E.A.; Syafruddin, S.E.; Abd Jalal, N.; Ismail, N.; Ishak, M.; Jamal, R.; et al. Characterizing the genetic risk for Type 2 diabetes in a Malaysian multi-ethnic cohort. Diabet. Med. 2015, 32, 1377–1384. [Google Scholar] [CrossRef] [PubMed]
- Wilson, P.W.; Meigs, J.B.; Sullivan, L.; Fox, C.S.; Nathan, D.M.; D’Agostino, R.B., Sr. Prediction of incident diabetes mellitus in middle-aged adults: The Framingham Offspring Study. Arch. Intern. Med. 2007, 167, 1068–1074. [Google Scholar] [CrossRef] [PubMed]
- Carlsson, S.; Ahlbom, A.; Lichtenstein, P.; Andersson, T. Shared genetic influence of BMI, physical activity and type 2 diabetes: A twin study. Diabetologia 2013, 56, 1031–1035. [Google Scholar] [CrossRef]
- Hu, F.B.; Sigal, R.J.; Rich-Edwards, J.W.; Colditz, G.A.; Solomon, C.G.; Willett, W.C.; Speizer, F.E.; Manson, J.E. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: A prospective study. JAMA 1999, 282, 1433–1439. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health 18–64 Years Old; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Hall, M.H.; Muldoon, M.F.; Jennings, J.R.; Buysse, D.J.; Flory, J.D.; Manuck, S.B. Self-reported sleep duration is associated with the metabolic syndrome in midlife adults. Sleep 2008, 31, 635–643. [Google Scholar] [CrossRef]
- Holliday, E.G.; Magee, C.A.; Kritharides, L.; Banks, E.; Attia, J. Short sleep duration is associated with risk of future diabetes but not cardiovascular disease: A prospective study and meta-analysis. PLoS ONE 2013, 8, e82305. [Google Scholar] [CrossRef]
- Shan, Z.; Ma, H.; Xie, M.; Yan, P.; Guo, Y.; Bao, W.; Rong, Y.; Jackson, C.L.; Hu, F.B.; Liu, L. Sleep duration and risk of type 2 diabetes: A meta-analysis of prospective studies. Diabetes Care 2015, 38, 529–537. [Google Scholar]
- Shamsuddin, N.; Koon, P.B.; Zakaria, S.Z.S.; Noor, M.I.; Jamal, R. Reliability and Validity of Malay Language Version of International Physical Activity Questionnaire (IPAQ-M) among the Malaysian Cohort Participants. Int. J. Public Health Res. 2015, 5, 643–653. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic; Report of a WHO Consultation; WHO: Geneva, Switzerland, 2000; p. 16. [Google Scholar]
- World Health Organization. Waist Circumference and Waist-Hip Ratio; Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2008; p. 47. [Google Scholar]
- National Cholesterol Education Program. Third Report of the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (ATP III Final Report); National Institute of Health: Bethesda, MD, USA, 2002; p. 280.
- World Health Organization. Obesity—Preventing and Managing the Global Epidemic: Report of a WHO Consultation on Obesity; World Health Organization: Geneva, Switzerland, 1998; p. 158. [Google Scholar]
- Royston, P.; White, I.R. Multiple Imputation by Chained Equations (MICE): Implementation in Stata. J. Stat. Softw. 2011, 45. [Google Scholar] [CrossRef]
- Rubin, D.B. Multiple Imputation after 18 Years. J. Am. Stat. Assoc. 1996, 91, 473–489. [Google Scholar] [CrossRef]
- Greenland, S.; Daniel, R.; Pearce, N. Outcome Modelling strategies in epidemiology: Traditional Methods and Basic alternatives. Int. J. Epidemiol. 2016, 45, 565–575. [Google Scholar] [CrossRef]
- Kaur, P.; Radhakrishna, E.; Sankarasubbaiyan, S.; Rao, S.R.; Kondalsamy-Chennakesavan, S.; Rao, T.V.; Gupte, M.D. A comparison of anthropometric indices for predicting hypertension and type 2 diabetes in a male industrial population of Chennai, South India. Ethn. Dis. 2008, 18, 31–36. [Google Scholar] [PubMed]
- Cheng, C.H.; Ho, C.C.; Yang, C.F.; Huang, Y.C.; Lai, C.H.; Liaw, Y.P. Waist-to-hip ratio is a better anthropometric index than body mass index for predicting the risk of type 2 diabetes in Taiwanese population. Nutr. Res. 2010, 30, 585–593. [Google Scholar] [CrossRef] [PubMed]
- Xin, Z.; Liu, C.; Niu, W.Y.; Feng, J.P.; Zhao, L.; Ma, Y.H.; Hua, L.; Yang, J.K. Identifying obesity indicators which best correlate with type 2 diabetes in a Chinese population. BMC Public Health 2012, 12, 732. [Google Scholar]
- Cleves, M.A.; Rock, L. From the help desk: Comparing areas under receiver operating characteristic curves from two or more probit or logit models. Stata J. 2002, 2, 301–313. [Google Scholar] [CrossRef]
- Alberti, K.G.; Zimmet, P.; Shaw, J. International Diabetes Federation: A consensus on Type 2 diabetes prevention. Diabet. Med. 2007, 24, 451–463. [Google Scholar] [CrossRef]
- Willey, K.A.; Singh, M.A.F. Battling insulin resistance in elderly obese people with type 2 diabetes: Bring on the heavy weights. Diabetes Care 2003, 26, 1580–1588. [Google Scholar] [CrossRef]
- Landi, F.; Onder, G.; Bernabei, R. Sarcopenia and diabetes: Two sides of the same coin. J. Am. Med. Dir. Assoc. 2013, 14, 540–541. [Google Scholar] [CrossRef]
- Aravindalochanan, V.; Kumpatla, S.; Rengarajan, M.; Rajan, R.; Viswanathan, V. Risk of diabetes in subjects with sedentary profession and the synergistic effect of positive family history of diabetes. Diabetes Technol. Ther. 2014, 16, 26–32. [Google Scholar]
- Chen, G.; Li, M.; Xu, Y.; Chen, N.; Huang, H.; Liang, J.; Li, L.; Wen, J.; Lin, L.; Yao, J. Impact of family history of diabetes on beta-cell function and insulin resistance among Chinese with normal glucose tolerance. Diabetes Technol. Ther. 2012, 14, 463–468. [Google Scholar]
- Bjorntorp, P. “Portal” adipose tissue as a generator of risk factors for cardiovascular disease and diabetes. Arteriosclerosis 1990, 10, 493–496. [Google Scholar] [CrossRef]
- Bjorntorp, P. Metabolic implications of body fat distribution. Diabetes Care 1991, 14, 1132–1143. [Google Scholar] [CrossRef]
- Diez, J.J.; Iglesias, P. The role of the novel adipocyte-derived hormone adiponectin in human disease. Eur. J. Endocrinol. 2003, 148, 293–300. [Google Scholar] [CrossRef]
- Despres, J.P.; Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 2006, 444, 881–887. [Google Scholar] [CrossRef]
- Lear, S.A.; Humphries, K.H.; Kohli, S.; Chockalingam, A.; Frohlich, J.J.; Birmingham, C.L. Visceral adipose tissue accumulation differs according to ethnic background: Results of the Multicultural Community Health Assessment Trial (M-CHAT). Am. J. Clin. Nutr. 2007, 86, 353–359. [Google Scholar] [CrossRef]
- Deurenberg-Yap, M.; Schmidt, G.; van Staveren, W.A.; Hautvas, J.G.; Deurenberg, P. Body fat measurement among Singaporean Chinese, Malays and Indians: A comparative study using a four-compartment model and different two-compartment models. Br. J. Nutr. 2001, 85, 491–498. [Google Scholar] [CrossRef]
- Deurenberg, P.; Deurenberg-Yap, M.; Guricci, S. Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes. Rev. 2002, 3, 141–146. [Google Scholar] [CrossRef]
- Lutsey, P.L.; Pereira, M.A.; Bertoni, A.G.; Kandula, N.R.; Jacobs, D.R., Jr. Interactions between race/ethnicity and anthropometry in risk of incident diabetes: The multi-ethnic study of atherosclerosis. Am. J. Epidemiol. 2010, 172, 197–204. [Google Scholar] [CrossRef]
- Htet, A.S.; Bjertness, M.B.; Sherpa, L.Y.; Kjollesda, M.K.; Oo, W.M.; Meyer, H.E.; Stigum, H.; Bjertness, E. Urban-rural differences in the prevalence of non-communicable diseases risk factors among 25–74 years old citizens in Yangon Region, Myanmar: A cross sectional study. BMC Public Health 2016, 16, 1225. [Google Scholar]
- Institute for Public Health. National Health and Morbidity Survey 2011 (NHMS 2011); Volume II: Non Communicable Diseases; IPH: Kuala Lumpur, Malaysia, 2011; p. 188. [Google Scholar]
- Noor Hassim, I.; Norazman, M.R.; Diana, M.; Khairul Hazdi, Y.; Rosnah, I. Cardiovascular risk assessment between urban and rural population in Malaysia. Med. J. Malays. 2016, 71, 331–337. [Google Scholar]
- O’Connor, A.; Wellenius, G. Rural-urban disparities in the prevalence of diabetes and coronary heart disease. Public Health 2012, 126, 813–820. [Google Scholar] [CrossRef]
- Ferrie, J.E.; Kivimaki, M.; Akbaraly, T.N.; Tabak, A.; Abell, J.; Davey Smith, G.; Virtanen, M.; Kumari, M.; Shipley, M.J. Change in Sleep Duration and Type 2 Diabetes: The Whitehall II Study. Diabetes Care 2015, 38, 1467–1472. [Google Scholar]
- Gottlieb, D.J.; Punjabi, N.M.; Newman, A.B.; Resnick, H.E.; Redline, S.; Baldwin, C.M.; Nieto, F.J. Association of sleep time with diabetes mellitus and impaired glucose tolerance. Arch. Intern. Med. 2005, 165, 863–867. [Google Scholar] [CrossRef]
- Van Leeuwen, W.M.; Hublin, C.; Sallinen, M.; Harma, M.; Hirvonen, A.; Porkka-Heiskanen, T. Prolonged sleep restriction affects glucose metabolism in healthy young men. Int. J. Endocrinol. 2010, 2010, 108641. [Google Scholar] [CrossRef]
- Tan, N.Y.Q.; Chew, M.; Tham, Y.C.; Nguyen, Q.D.; Yasuda, M.; Cheng, C.Y.; Wong, T.Y.; Sabanayagam, C. Associations between sleep duration, sleep quality and diabetic retinopathy. PLoS ONE 2018, 13, e0196399. [Google Scholar] [CrossRef]
- Prince, S.A.; Adamo, K.B.; Hamel, M.E.; Hardt, J.; Connor Gorber, S.; Tremblay, M.A. A comparison of direct versus self-report measures for assessing physical activity in adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 56. [Google Scholar] [CrossRef]
- Shephard, R.J. Limits to the measurement of habitual physical activity by questionnaires. Br. J. Sports Med. 2003, 37, 197–206. [Google Scholar] [CrossRef]
- Kelly, P.; Doherty, A.; Berry, E.; Hodges, S.; Batterham, A.M.; Foster, C. Can we use digital life-log images to investigate active and sedentary travel behaviour? Results from a pilot study. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 44. [Google Scholar] [CrossRef]
- Ewald, B.; McEvoy, M.; Attia, J. Pedometer counts superior to physical activity scale for identifying health markers in older adults. Br. J. Sports Med. 2010, 44, 756–761. [Google Scholar] [CrossRef]
- Villegas, R.; Liu, S.; Gao, Y.T.; Yang, G.; Li, H.; Zheng, W.; Shu, X.O. Prospective study of dietary carbohydrates, glycemic index, glycemic load, and incidence of type 2 diabetes mellitus in middle-aged Chinese women. Arch. Intern. Med. 2007, 167, 2310–2316. [Google Scholar] [CrossRef]
- Malik, V.S.; Schulze, M.B.; Hu, F.B. Intake of sugar-sweetened beverages and weight gain: A systematic review. Am. J. Clin. Nutr. 2006, 84, 274–288. [Google Scholar] [CrossRef]
- Odegaard, A.O.; Koh, W.P.; Yuan, J.M.; Gross, M.D.; Pereira, M.A. Western-style fast food intake and cardiometabolic risk in an Eastern country. Circulation 2012, 126, 182–188. [Google Scholar] [CrossRef]
- Sedgwick, P. Nested case-control studies: Advantages and disadvantages. Br. Med. J. 2014, 348, g1532. [Google Scholar] [CrossRef]
- Stern, M.P.; Williams, K.; Haffner, S.M. Identification of persons at high risk for type 2 diabetes mellitus: Do we need the oral glucose tolerance test? Ann. Intern. Med. 2002, 136, 575–581. [Google Scholar] [CrossRef]
- Ye, X.; Zong, G.; Liu, X.; Liu, G.; Gan, W.; Zhu, J.; Lu, L.; Sun, L.; Li, H.; Hu, F.B.; et al. Development of a new risk score for incident type 2 diabetes using updated diagnostic criteria in middle-aged and older chinese. PLoS ONE 2014, 9, e97042. [Google Scholar]
- Wulan, S.N.; Westerterp, K.R.; Plasqui, G. Ethnic differences in body composition and the associated metabolic profile: A comparative study between Asians and Caucasians. Maturitas 2010, 65, 315–319. [Google Scholar] [CrossRef]
- Ling, C.; Groop, L. Epigenetics: A molecular link between environmental factors and type 2 diabetes. Diabetes 2009, 58, 2718–2725. [Google Scholar] [CrossRef]
- Jacobsen, S.C.; Brons, C.; Bork-Jensen, J.; Ribel-Madsen, R.; Yang, B.; Lara, E.; Hall, E.; Calvanese, V.; Nilsson, E.; Jorgensen, S.W.; et al. Effects of short-term high-fat overfeeding on genome-wide DNA methylation in the skeletal muscle of healthy young men. Diabetologia 2012, 55, 3341–3349. [Google Scholar] [CrossRef]
- Nitert, M.D.; Dayeh, T.; Volkov, P.; Elgzyri, T.; Hall, E.; Nilsson, E.; Yang, B.T.; Lang, S.; Parikh, H.; Wessman, Y.; et al. Impact of an exercise intervention on DNA methylation in skeletal muscle from first-degree relatives of patients with type 2 diabetes. Diabetes 2012, 61, 3322–3332. [Google Scholar] [CrossRef]
- Ronn, T.; Volkov, P.; Davegardh, C.; Dayeh, T.; Hall, E.; Olsson, A.H.; Nilsson, E.; Tornberg, A.; Dekker Nitert, M.; Eriksson, K.F.; et al. A six months exercise intervention influences the genome-wide DNA methylation pattern in human adipose tissue. PLoS Genet. 2013, 9, e1003572. [Google Scholar]
- Chambers, J.C.; Loh, M.; Lehne, B.; Drong, A.; Kriebel, J.; Motta, V.; Wahl, S.; Elliott, H.R.; Rota, F.; Scott, W.R.; et al. Epigenome-wide association of DNA methylation markers in peripheral blood from Indian Asians and Europeans with incident type 2 diabetes: A nested case-control study. Lancet Diabetes Endocrinol. 2015, 3, 526–534. [Google Scholar]
| Malay (n = 1323) | Chinese (n = 1344) | Indian (n = 1410) | ||||
|---|---|---|---|---|---|---|
| T2D | Control | T2D | Control | T2D | Control | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Gender | ||||||
| Male | 285 (47.5) *** | 252 (34.9) | 343 (52.5) *** | 153 (22.2) | 401 (56.6) *** | 221 (31.5 |
| Female | 315 (52.5) | 471 (65.2) | 311 (47.6) | 537 (77.8) | 307 (43.4) | 481 (68.5) |
| Age group, years | ||||||
| Less than 50 | 200 (33.3) *** | 424 (58.6) | 215 (32.9) *** | 434 (62.9) | 293 (41.4) *** | 486 (69.2) |
| 50–60 | 321 (53.5) | 243 (33.6) | 265 (40.5) | 209 (30.3) | 337 (47.6) | 174 (24.8) |
| More than 60 | 79 (13.2) | 56 (7.8) | 174 (26.6) | 47 (6.8) | 78 (11.0) | 42 (6.0) |
| Location | ||||||
| Rural | 164 (27.3) * | 162 (22.4) | 9 (1.4) | 8 (1.2) | 97 (13.7) *** | 38 (5.4) |
| Urban | 436 (72.7) | 561 (77.6) | 645 (98.6) | 682 (98.8) | 611 (86.3) | 664 (94.6) |
| Family History of Diabetes (FHD) | ||||||
| Negative | 192 (32) | 257 (35.6) | 204 (33.6) ** | 291 (42.2) | 148 (20.9) *** | 199 (28.4) |
| Positive | 408 (68) | 466 (64.5) | 403 (66.4) | 399 (57.8) | 560 (79.1) | 501 (71.6) |
| BMI category, kg/m2 | ||||||
| Normal (<25) | 153 (25.5) *** | 266 (36.8) | 260 (39.8) *** | 510 (73.9) | 241 (34.0) | 271 (38.6) |
| Pre-obese (25–29.9) | 268 (44.7) | 313 (43.3) | 267 (40.8) | 152 (22.0) | 292 (41.2) | 275 (39.2) |
| Obese (>30) | 179 (29.8) | 144 (19.9) | 127 (19.4) | 28 (4.1) | 175 (24.7) | 156 (22.2) |
| Waist-to-Hip Ratio (WHR) | ||||||
| Low risk (<0.95 M, <0.80 F) | 223 (37.2) *** | 392 (54.2) | 232 (35.5) *** | 407 (59.0) | 207 (29.2) *** | 315 (44.9) |
| Moderate risk (0.96–1 M, 0.81–0.85 F) | 104 (17.3) | 151 (20.9) | 127 (19.4) | 166 (24.1) | 141 (19.9) | 177 (25.2) |
| High risk (>1 M, >0.85 F) | 273 (45.5) | 180 (24.9) | 295 (45.1) | 117 (17.0) | 360 (50.9) | 210 (29.9) |
| Physical activity1 | ||||||
| Active | 44 (10.6) | 52 (14.9) | 17 (7.6) | 30 (8.1) | 64 (17.7) | 77 (14.7) |
| Inactive | 373 (89.5) | 298 (85.1) | 206 (92.4) | 342 (91.9) | 297 (82.3) | 447 (85.3) |
| Average sleep duration1 | ||||||
| Less than 6 h | 83(19.9) | 78(22.3) | 26(11.7) | 28(7.5) | 52(14.4) *** | 84(16.0) |
| 6–7 h | 159(38.1) | 118(33.7) | 38(17.0) | 92(24.7) | 95(26.3) | 172(32.8) |
| 7–8 h | 93(22.3) | 92 (26.3) | 86(8.6) | 145(39.0) | 95(26.3) | 136(26.0) |
| 8–9 h | 58(13.9) | 39 (11.1) | 52(23.3) | 82(22.0) | 73(20.2) | 102(19.5) |
| 9–10 h | 17(4.1) | 16 (4.6) | 15(6.7) | 17(4.6) | 22(6.1) | 24(4.6) |
| More than 10 h | 7(1.7) | 7(2.0) | 6(2.7) | 8(2.2) | 24(6.7) | 6(1.2) |
| Complete-Case OR (95% CI) | ||||
|---|---|---|---|---|
| Malays (767) | Chinese (595) | Indians (885) | Combined 1 | |
| Age 50–60 (Ref: <50) | 2.48 (1.77, 3.48) p < 0.001 | 1.11 (0.70, 1.78) p = 0.652 | 2.62 (1.87, 3.68) p < 0.001 | 2.13 (1.73, 2.62) p < 0.001 |
| Age > 60 | 1.95 (1.02, 3.72) p = 0.043 | 3.35 (1.79,6.24) p < 0.001 | 2.23 (1.24, 4.03) p = 0.008 | 2.71 (1.91, 3.85) p < 0.001 |
| Gender: Female (Ref: Male) | 1.15 (0.79,1.68) p = 0.469 | 1.57 (0.93, 2.65) p = 0.092 | 0.96 (0.66, 1.41) p = 0.851 | 1.13 (0.89, 1.42) p = 0.314 |
| WHR | 3.01 (2.30, 3.93) p < 0.001 | 6.28 (4.27, 9.25) p < 0.001 | 3.23 (2.46, 4.23) p < 0.001 | 3.63 (3.07, 4.28) p < 0.001 |
| Physical inactivity (Ref: Physical activity) | 1.21 (0.74, 2.00) p = 0.446 | 1.07 (0.49, 2.32) p = 0.874 | 0.94 (0.61, 1.45) p = 0.790 | 1.10 (0.82, 1.48) p = 0.538 |
| Location: Rural (Ref: Urban) | 1.67 (1.05, 2.67) p = 0.031 | 1.28 (0.29, 5.53) p = 0.744 | 2.6 (1.61, 4.22) p < 0.001 | 1.91 (1.39, 2.64) p < 0.001 |
| Positive FHD (Ref: Negative FHD) | 0.77 (0.52, 1.12) p = 0.175 | 1.90 (1.22, 2.96) p = 0.005 | 1.64 (1.13,2.38) p = 0.009 | 1.32 (1.06, 1.64) p = 0.013 |
| Average sleep duration (Ref: 7–8 h) | ||||
| Less than 6 h | 0.92 (0.58, 1.48) p = 0.740 | 0.89 (0.40, 1.96) p = 0.769 | 0.85 (0.51, 1.41) p = 0.534 | 0.83 (0.61, 1.13) p = 0.229 |
| 6–7 h | 1.38 (0.91, 2.10) p = 0.128 | 0.59 (0.33, 1.05) p = 0.072 | 0.85 (0.56, 1.29) p = 0.449 | 0.94 (0.73, 1.21) p = 0.633 |
| 8–9 h | 1.09 (0.62, 1.93) p = 0.771 | 0.80 (0.46, 1.39) p = 0.422 | 1.11 (0.69, 1.77) p = 0.673 | 0.98 (0.73, 1.31) p = 0.873 |
| 9–10 h | 0.71 (0.31, 1.65); p = 0.432 | 0.87 (0.32, 2.36) p = 0.781 | 1.43 (0.69, 2.96) p = 0.333 | 0.98 (0.61, 1.58) p = 0.941 |
| More than 10 h | 0.61 (0.19, 1.98) p = 0.418 | 0.71 (0.19, 2.68) p = 0.610 | 7.10 (2.38, 21.17) p < 0.001 | 1.81 (0.93, 3.51) p = 0.079 |
| Pseudo R2 (%) | 0.16 | 0.29 | 0.22 | 0.21 |
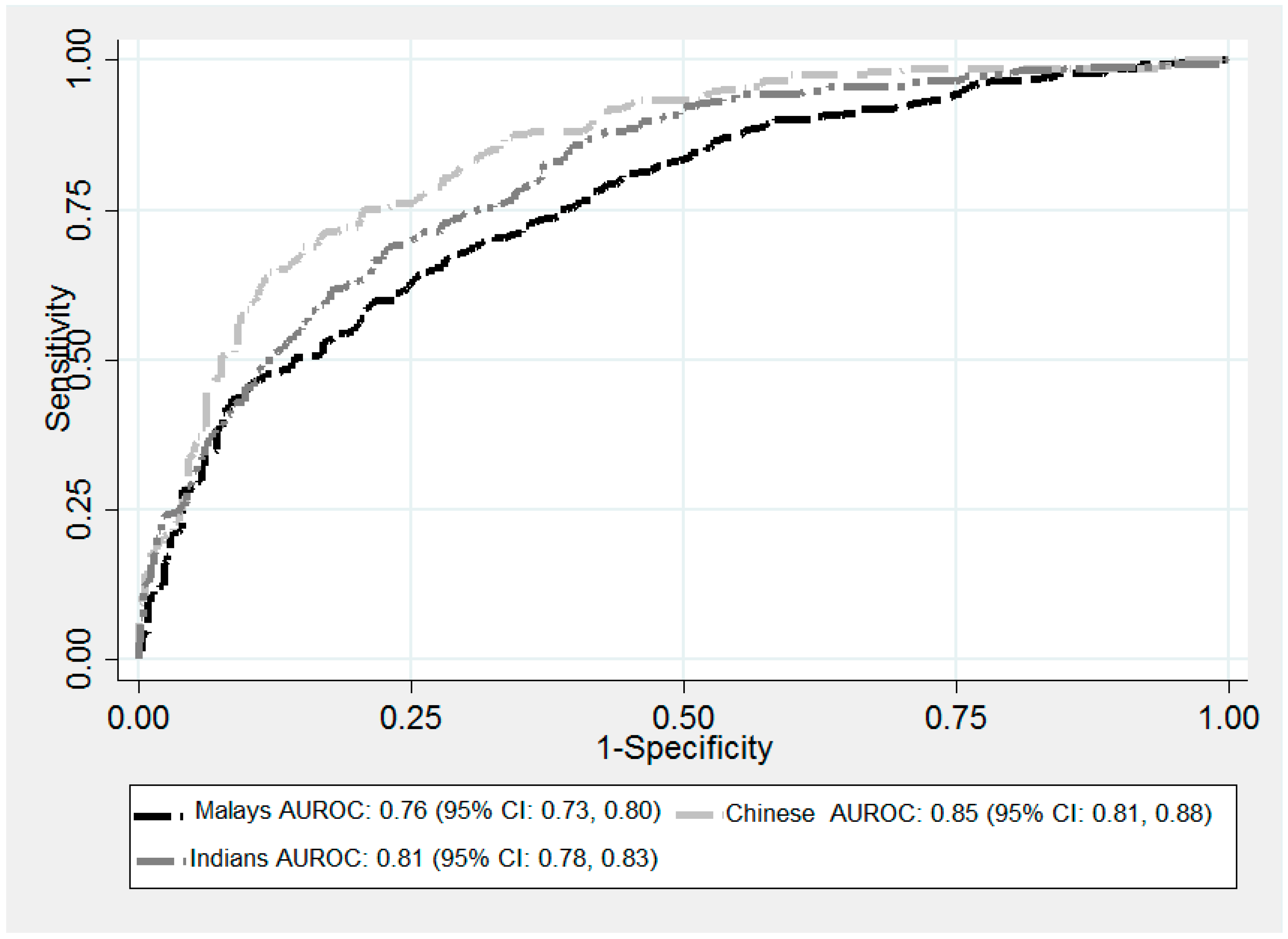
| ROC (95% CI) | 0.76 (0.73, 0.80) | 0.85 (0.81, 0.88) | 0.81 (0.78, 0.83) | 0.80 (0.78, 0.82) |
| Multiple Imputation OR (95% CI) | ||||
|---|---|---|---|---|
| Malays (1323) | Chinese (1344) | Indians (1410) | Combined 1 (4077) | |
| Age 50–60 (Ref: <50) | 2.46 (2.30, 2.62) p < 0.001 | 1.19 (1.08, 1.30) p < 0.001 | 2.64 (2.47, 2.82) p < 0.001 | 2.14 (2.05, 2.23) p < 0.001 |
| Age > 60 (Ref: <50) | 1.97 (1.73, 2.23) p < 0.001 | 3.66 (3.25, 4.13) p < 0.001 | 2.08 (1.86, 2.33) p < 0.001 | 2.73 (2.55, 2.92) p < 0.001 |
| Gender: Female (Ref: Male) | 1.13 (1.05, 1.22) p = 0.001 | 1.51 (1.37, 1.67) p < 0.001 | 0.95 (0.88, 1.03) p = 0.204 | 1.11 (1.06, 1.16) p < 0.001 |
| WHR | 3.01 (2.85, 3.17) p < 0.001 | 6.01 (5.58, 6.47) p < 0.001 | 3.22 (3.05, 3.40) p < 0.001 | 3.60 (3.49, 3.72) p < 0.001 |
| Physical inactivity (Ref: Physical activity) | 1.19 (1.08, 1.32) p < 0.001 | 1.14 (0.98, 1.33) p = 0.093 | 1.01 (0.93, 1.10) p = 0.810 | 1.14 (1.07, 1.21) p < 0.001 |
| Location: Rural (Ref: Urban) | 1.71 (1.56, 1.88) p < 0.001 | 1.80 (1.35, 2.39) p < 0.001 | 2.51 (2.29, 2.76) p < 0.001 | 1.93 (1.81, 2.06) p < 0.001 |
| Positive FHD (Ref: Negative FHD) | 0.75 (0.70, 0.81) p < 0.001 | 1.88 (1.72, 2.05) p < 0.001 | 1.60 (1.48, 1.72) p < 0.001 | 1.30 (1.25, 1.81) p < 0.001 |
| Average sleep duration (Ref: 7–8 h) | ||||
| Less than 6 h | 0.89 (0.81, 0.98) p = 0.015 | 0.88 (0.76, 1.03) p = 0.106 | 0.88 (0.80, 0.97) p = 0.014 | 0.83 (0.78, 0.88) p < 0.001 |
| 6–7 h | 1.39 (1.28, 1.51) p < 0.001 | 0.65 (0.58, 0.72) p < 0.001 | 0.85 (0.78, 0.93) p < 0.001 | 0.96 (0.91, 1.01) p = 0.106 |
| 8–9 h | 1.11 (0.99, 1.24) p = 0.08 | 0.78 (0.70, 0.87) p < 0.001 | 1.10 (1.00, 1.21); p = 0.036 | 0.97 (0.91, 1.02) p = 0.236 |
| 9–10 h | 0.72 (0.61, 0.85) p < 0.001 | 0.85 (0.70, 1.03) p = 0.10 | 1.42 (1.23, 1.64) p < 0.001 | 0.98 (0.89, 1.07) p = 0.653 |
| More than 10 h | 0.61 (0.49, 0.77) p < 0.001 | 0.76 (0.59, 0.97) p = 0.97 | 7.18 (5.79, 890) p < 0.001 | 1.83 (1.61, 2.08) p < 0.001 |
| Pseudo R2 (%) | 0.16 | 0.29 | 0.22 | 0.21 |
| 0.76 (0.76, 0.77) | 0.84 (0.84, 0.85) | 0.80 (0.80, 0.81) | 0.80 (0.79, 0.80) | |
| AUC (95% CI) | Malay: 0.76 (0.73, 0.80) | Chinese: 0.84 (0.81, 0.88) | Indian: 0.80 (0.78, 0.83) | Global Test of All Ancestral Groups |
|---|---|---|---|---|
| Malay: 0.76 (0.73, 0.80) | p = 0.0004 | p = 0.052 | p = 0.0018 | |
| Chinese: 0.84 (0.81, 0.88) | p = 0.0004 | p = 0.065 | ||
| Indian: 0.80 (0.78, 0.83) | p = 0.052 | p = 0.065 |
| Interaction | OR (95% CI) p-Value |
|---|---|
| Age group by Ancestral group (Ref: Aged < 50, Malay) | |
| Aged 50–60 years by Chinese | 0.52 (0.32, 0.85) p = 0.009 |
| Aged 50–60 years by Indian | 1.06 (0.69, 1.62) p = 0.804 |
| Aged more than 60 years by Chinese | 2.06 (0.93, 4.57) p = 0.075 |
| Aged more than 60 years by Indian | 0.95 (0.44, 2.06) p = 0.891 |
| Gender by Ancestral group (Ref: Male, Malay) | |
| Female by Chinese | 0.5 (0.32, 0.8) p = 0.003 |
| Female by Indian | 0.6 (0.4, 0.89) p = 0.011 |
| Waist-to-Hip Ratio by Ancestral group (Ref: Low risk (<0.95 M, <0.80 F), Malay) | |
| Moderate risk (0.96–1 M, 0.81–0.85 F) by Chinese | 1.15 (0.64, 2.07) p = 0.630 |
| Moderate risk (0.96–1 M, 0.81–0.85 F) by Indian | 1.11 (0.66, 1.88) p = 0.694 |
| High risk (>1 M, >0.85 F) by Chinese | 2.10 (1.23, 3.57) p = 0.006 |
| High risk (>1 M, >0.85 F) by Indian | 1.24 (0.78, 1.97) p = 0.362 |
| Physical Activity by Ancestral group (Ref: Active, Malay) | |
| Inactive by Chinese | 0.72 (0.34, 1.53) p = 0.390 |
| Inactive by Indian | 0.54 (0.31, 0.95) p = 0.032 |
| Locality by Ancestral groups (Ref: Urban, Malay) | |
| Rural by Chinese | 0.93 (0.3, 2.94) p = 0.905 |
| Rural by Indian | 1.51 (0.84, 2.73) p = 0.167 |
| Family History of T2D by Ancestral group (Ref: Negative FHD, Malay) | |
| Positive FHD by Chinese | 2.96 (1.82, 4.81) p < 0.001 |
| Positive FHD by Indian | 2.43 (1.53, 3.85) p < 0.001 |
| Sleep duration categories by Ancestral group (Ref: Sleep duration 7–8 h, Malay) | |
| Sleep duration less than 6 h by Chinese | 1.49 (0.72, 3.09) p = 0.287 |
| Sleep duration less than 6 h by Indian | 0.84 (0.46, 1.54) p = 0.578 |
| Sleep duration 6–7 h by Chinese | 0.52 (0.29, 0.95) p = 0.032 |
| Sleep duration 6–7 h by Indian | 0.59 (0.35, 1.00) p = 0.049 |
| Sleep duration 8–9 h by Chinese | 0.73 (0.37, 1.41) p = 0.345 |
| Sleep duration 8–9 h by Indian | 0.7 (0.37, 1.32) p = 0.266 |
| Sleep duration 9–10 h by Chinese | 1.42 (0.50, 4.04) p = 0.517 |
| Sleep duration 9–10 h by Indian | 1.25 (0.47, 3.31) p = 0.656 |
| Sleep duration more than 10 h by Chinese | 1.28 (0.27, 5.96) p = 0.755 |
| Sleep duration more than 10 h by Indian | 5.79 (1.38, 24.23) p = 0.016 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abdullah, N.; Abdul Murad, N.A.; Attia, J.; Oldmeadow, C.; Kamaruddin, M.A.; Abd Jalal, N.; Ismail, N.; Jamal, R.; Scott, R.J.; Holliday, E.G. Differing Contributions of Classical Risk Factors to Type 2 Diabetes in Multi-Ethnic Malaysian Populations. Int. J. Environ. Res. Public Health 2018, 15, 2813. https://doi.org/10.3390/ijerph15122813
Abdullah N, Abdul Murad NA, Attia J, Oldmeadow C, Kamaruddin MA, Abd Jalal N, Ismail N, Jamal R, Scott RJ, Holliday EG. Differing Contributions of Classical Risk Factors to Type 2 Diabetes in Multi-Ethnic Malaysian Populations. International Journal of Environmental Research and Public Health. 2018; 15(12):2813. https://doi.org/10.3390/ijerph15122813
Chicago/Turabian StyleAbdullah, Noraidatulakma, Nor Azian Abdul Murad, John Attia, Christopher Oldmeadow, Mohd Arman Kamaruddin, Nazihah Abd Jalal, Norliza Ismail, Rahman Jamal, Rodney J. Scott, and Elizabeth G. Holliday. 2018. "Differing Contributions of Classical Risk Factors to Type 2 Diabetes in Multi-Ethnic Malaysian Populations" International Journal of Environmental Research and Public Health 15, no. 12: 2813. https://doi.org/10.3390/ijerph15122813
APA StyleAbdullah, N., Abdul Murad, N. A., Attia, J., Oldmeadow, C., Kamaruddin, M. A., Abd Jalal, N., Ismail, N., Jamal, R., Scott, R. J., & Holliday, E. G. (2018). Differing Contributions of Classical Risk Factors to Type 2 Diabetes in Multi-Ethnic Malaysian Populations. International Journal of Environmental Research and Public Health, 15(12), 2813. https://doi.org/10.3390/ijerph15122813






