Developing Behaviour Change Interventions for Improving Access to Health and Hygiene for People with Disabilities: Two Case Studies from Nepal and Malawi
Abstract
1. Introduction
2. Approaches to Designing New Interventions
2.1. The Medical Research Council’s Framework
- Identifying the desired outcome
- Identifying how to bring about change based on theory and evidence
- Testing the feasibility of the intervention to ensure that it is acceptable and can be delivered as intended
- Evaluation of the intervention through both impact and process evaluations
2.2. Behaviour Centred Design
3. Case Studies
3.1. Case Study 1: Designing an Intervention to Improve Uptake of Referral for Ear and Hearing Services for Children in Malawi
3.1.1. Study Aim and Setting
3.1.2. Assess: Systematic Review
3.1.3. Build: Formative Research
- Fear and uncertainty about the referral hospital
- Procedural problems within the camps leading to lack of understanding about the referral
- Distance to the hospital
- Low awareness and understanding of hearing loss
- Lack of and cost of transport
3.1.4. Create: Designing the Intervention
(1) Focus Group Discussion and Theory of Change Development
- Developing a long-term goal for the project
- Backwards mapping from the long-term goal to outcomes and intermediate outcomes required to reach the long-term goal
- Discussing possible activities (interventions) to achieve the prioritised outcomes
- Prioritisation of suggested activities (interventions) in terms of cost, feasibility, acceptability and sustainability
(2) Proposed Interventions
- A photograph/pictorial information booklet providing information about the process of going to the hospital for ear and hearing services
- Counsellors trained to deliver information booklet in camp settings, including one “expert” mother (i.e., mother of a child with ear and/or hearing issue who has attended QECH for referral previously) who would provide peer support and a community health worker
- Text message reminders for caregivers who had been referred to QECH
(3) Engagement with Creative Team
- Draft 1 and 2 reviewed by LSHTM researchers
- Draft 3 reviewed by eight stakeholders from Malawi (six from original ToC workshop)
- Draft 4 reviewed by target population (caregivers of children with ear and hearing issues from Thyolo district) through a focus group discussion). Caregivers were asked to reflect on suitability of the images, comprehensibility of the text, and usefulness of the components of the booklet.
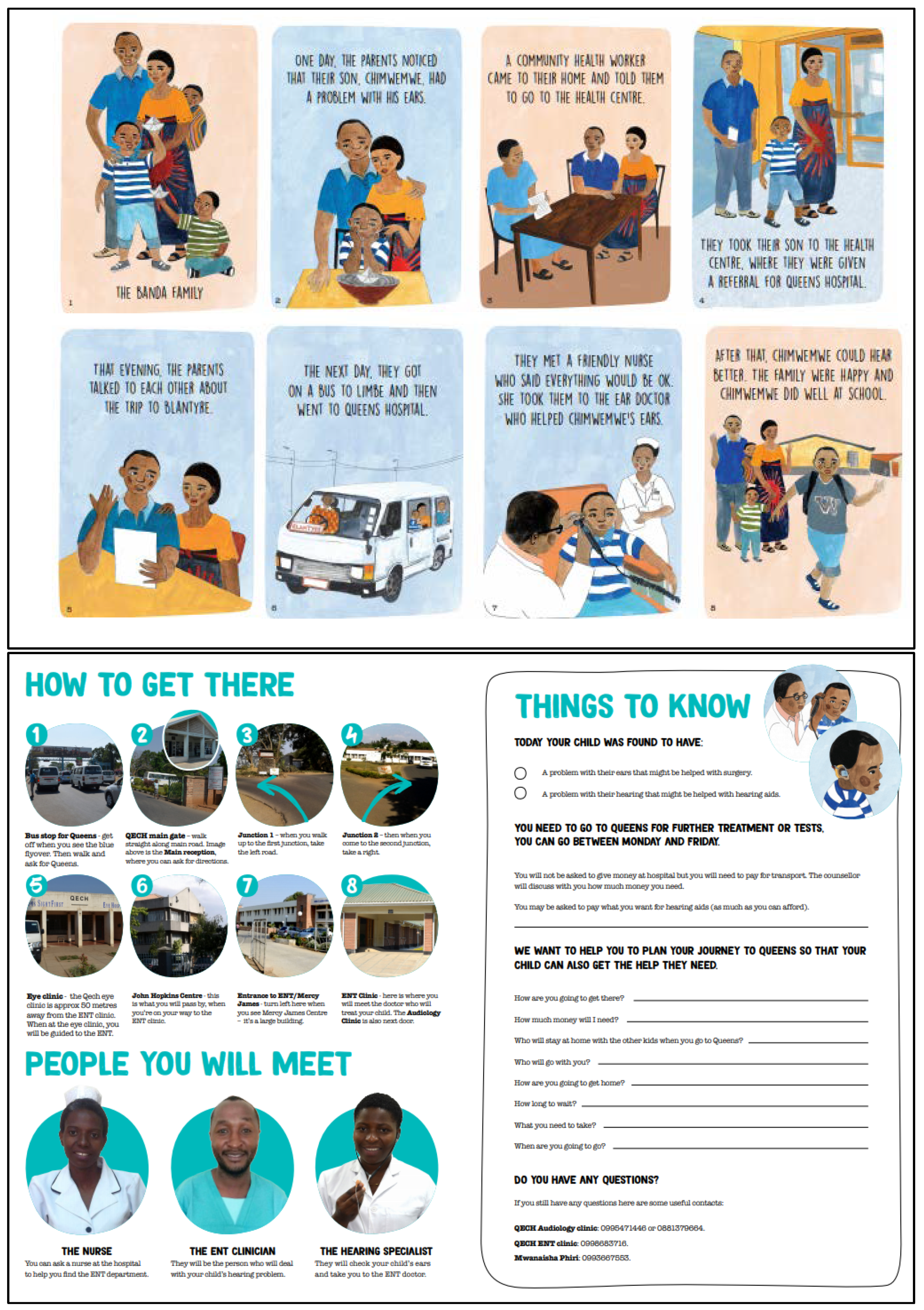
(4) Intervention
- A booklet with three main parts (Figure 2): (1) An illustrated storyline of “The Banda Family” going through the process of being referred and attending the referral at QECH; (2) Information on how to get to the hospital including photographs of key landmarks that caregivers would see on the way to the ENT department; (3) Action planning stage that was tailored to each caregiver—including how they plan to go, how much money they need, and what they need to take with them. This booklet would be delivered by a trained “expert mother” (i.e., mother of a child with ear and/or hearing issue who has attended QECH for referral previously) at the point at which the referral was made (in camps).
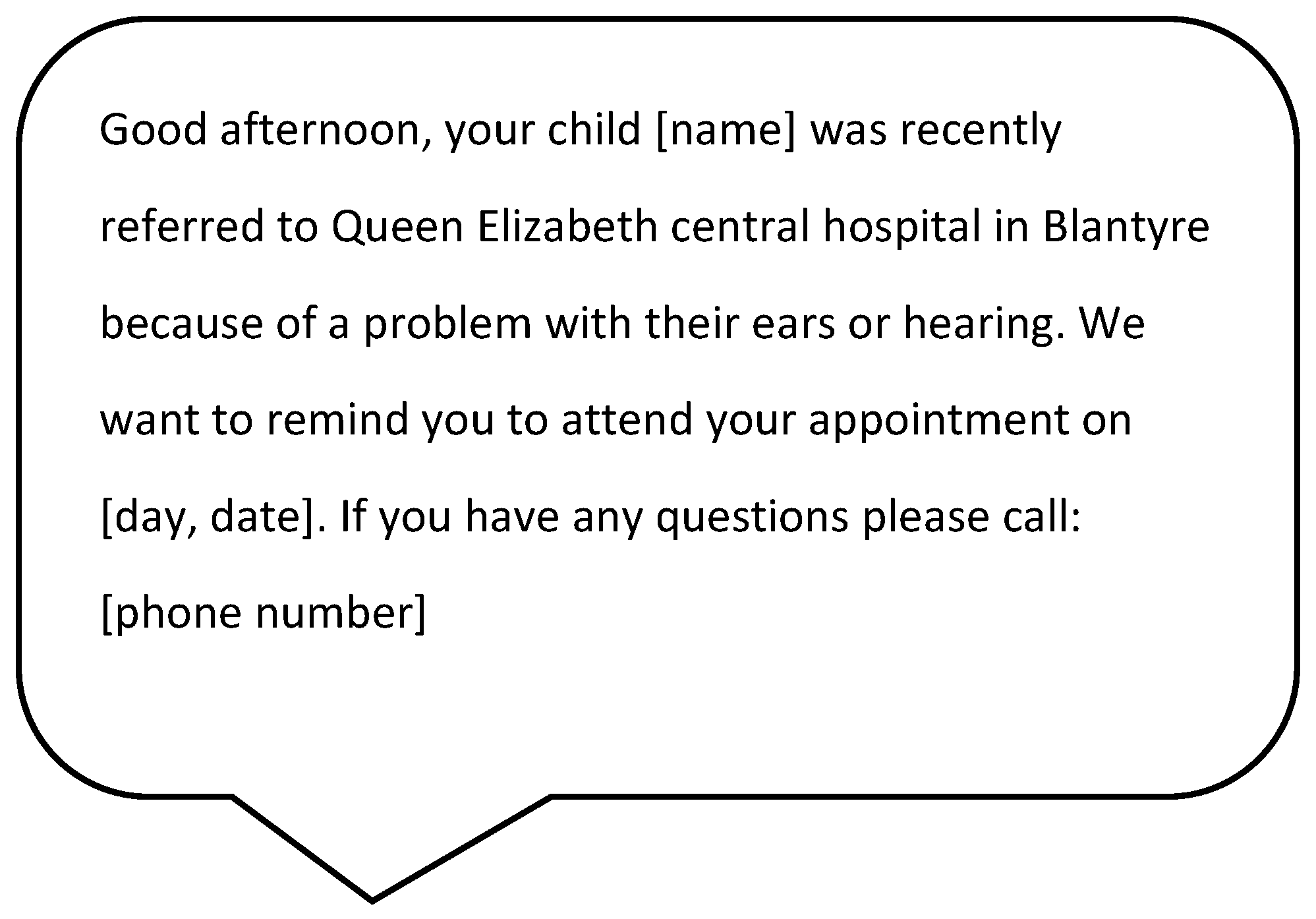
- A text-message reminder to be sent two weeks after the referral (Figure 3).
3.1.5. Deliver: Feasibility Studies
3.2. Case Study 2: Designing an Intervention to Improve Menstrual Hygiene Management of People with Intellectual Impairments in Nepal
3.2.1. Study Aim and Setting
3.2.2. Assess: Systematic Review
3.2.3. Build: Formative Research
- Limited MHM training, information and support. MHM information is often withheld from people with an intellectual impairment because of perceived levels of understanding. Carers have no support, information or guidance on how to manage another person’s menstrual cycle, leading many to feel overwhelmed.
- Limited ability to communicate verbally, understand menstruation and related social norms. Some people with intellectual impairments are unable to communicate verbally that they have pre-menstrual symptoms and may not understand the reason for these. Carers do not always provide pain relief for menstrual cramps. During menstruation some participants are frightened, withdrawn, or refused to eat. Some showed their menstrual blood or hygiene products to others and are abused for doing so.
- Poor access to existing MHM interventions. In Nepal, MHM interventions are predominantly delivered through school and community mechanisms. Many research participants with an intellectual impairment do not attend school so cannot access these. Some carers are unable to leave their home because of caring duties, so are unable to access the MHM information delivered through the community.
3.2.4. Create: Designing the Intervention
(1) Focus Group Discussion and Theory of Change Development
(2) Engagement with Creative Team
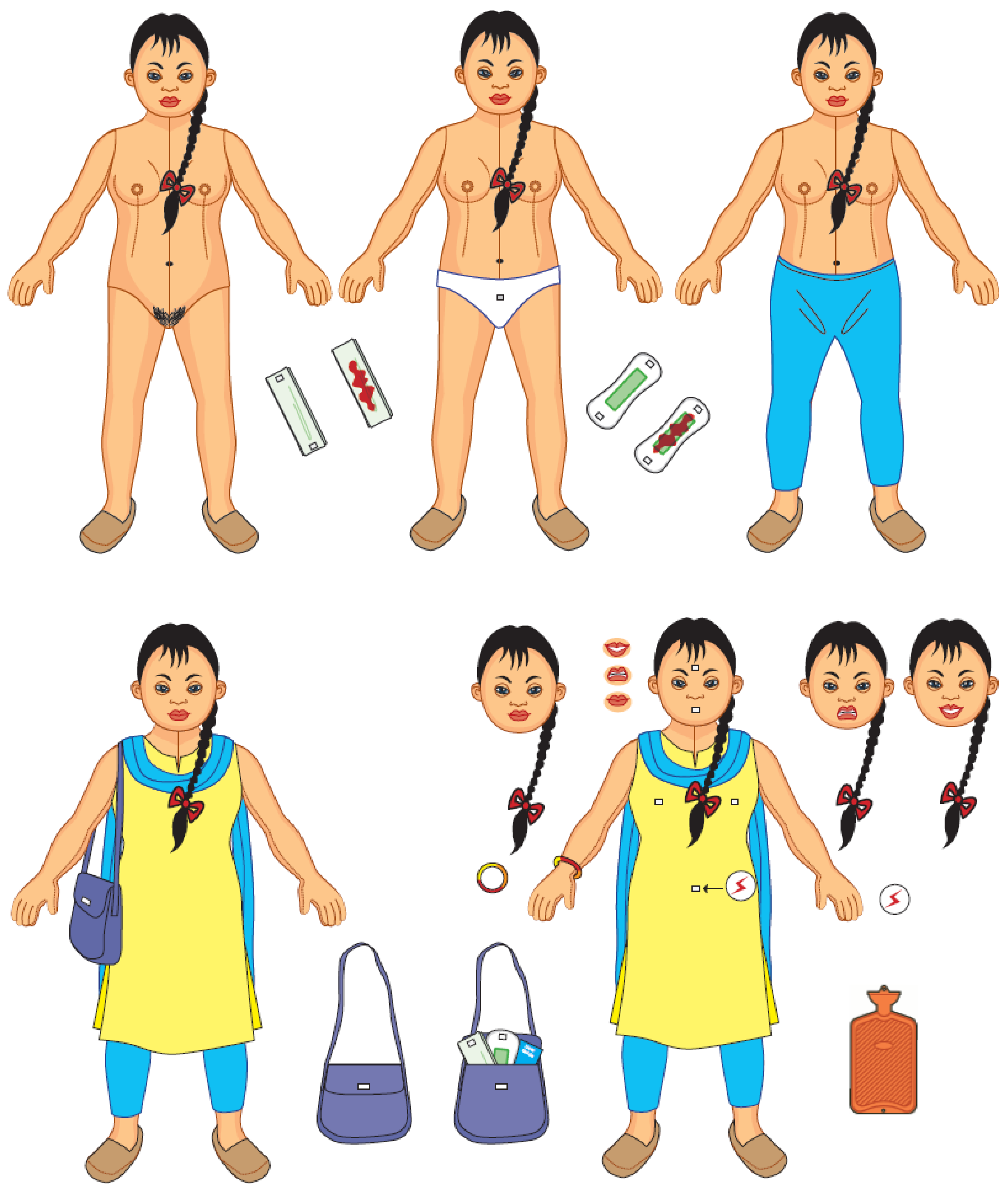
(3) Intervention Concept
(4) Touchpoints
(5) Intervention
3.2.5. Deliver: Feasibility Study
3.2.6. Comparison of Intervention Design Processes
4. Discussion
4.1. Key Lessons, Implications for Research and Practice
4.2. Challenges
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- World Health Organization. World Report on Disability. 2012. Available online: http://www.who.int/disabilities/world_report/2011/report/en/ (accessed on 16 February 2018).
- United Nations. Convention of the Rights of Persons with Disabilities and Optional Protocol; United Nations: New York, NY, USA, 2006. [Google Scholar]
- Banks, L.M.; Kuper, H.; Polack, S. Poverty and disability in low- and middle-income countries: A systematic review. PLoS ONE 2017, 12, e0189996. [Google Scholar] [CrossRef] [PubMed]
- Sen, A. The Idea of Justice; Harvard University Press: Cambridge, MA, USA, 2009. [Google Scholar]
- Hashemi, G.; Kuper, H.; Wickenden, M. SDGs, Inclusive Health and the path to Universal Health Coverage. Disabil. Glob. South 2017, 4, 108–1111. [Google Scholar]
- Iemmi, V.; Blanchet, K.; Gibson, L.J.; Kumar, K.S.; Rath, S.; Hartley, S.; Murthy, G.V.S.; Patel, V.; Weber, J.; Kuper, H. Community-based rehabilitation for people with physical and mental disabilities in low- and middle-income countries: A systematic review and meta-analysis. J. Dev. Eff. 2016, 8, 368–387. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations General Assembly: Geneva, Switzerland, 2015. [Google Scholar]
- Bright, T.; Felix, L.; Kuper, H.; Polack, S. A systematic review of strategies to increase access to health services among children in low and middle income countries. BMC Health Serv. Res. 2017, 17, 252. [Google Scholar] [CrossRef] [PubMed]
- Bright, T.; Felix, L.; Kuper, H.; Polack, S. Systematic review of strategies to increase access to health services among children over five in low- and middle-income countries. Trop. Med. Int. Health 2018, 23, 476–507. [Google Scholar] [CrossRef] [PubMed]
- Bedford, J.; Mackey, S.; Parvin, A.; Muhit, M.; Murthy, G.V. Reasons for non-uptake of referral: Children with disabilities identified through the Key Informant Method in Bangladesh. Disabil. Rehabil. 2013, 35, 2164–2170. [Google Scholar] [CrossRef] [PubMed]
- Nesbitt, R.C.; Mackey, S.; Kuper, H.; Muhit, M.; Murthy, G.V.S. Predictors of referral uptake in children with disabilities in Bangladesh—Exploring barriers as a first step to improving referral provision. Disabil. Rehabil. 2012, 34, 1089–1095. [Google Scholar] [CrossRef]
- Bright, T.; Mulwafu, W.; Thindwa, R.; Zuurmond, M.; Polack, S. Reasons for low uptake of referrals to ear and hearing services for children in Malawi. PLoS ONE 2017, 12, e0188703. [Google Scholar] [CrossRef] [PubMed]
- Eide, A.H.; Mannan, H.; Khogali, M.; Rooy, G.V.; Swartz, L.; Munthali, A.; Hem, K.G.; MacLachlan, M.; Dyrstad, K. Perceived barriers for accessing health services among individuals with disability in four African countries. PLoS ONE 2015, 10, e0125915. [Google Scholar] [CrossRef]
- Peters, D.H.; Garg, A.; Bloom, G.; Walker, D.G.; Brieger, W.R.; Rahman, M.H. Poverty and access to health care in developing countries. Ann. N. Y. Acad. Sci. 2008, 1136, 161–171. [Google Scholar] [CrossRef]
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new Medical Research Council guidance. BMJ 2008, 337, a1655. [Google Scholar] [CrossRef] [PubMed]
- Aunger, R.; White, S.; Greenland, K.; Curtis, V. Behaviour Centred Design: A Practitioners Manual. 2017. Available online: https://www.lshtm.ac.uk/sites/default/files/2017-03/BCD%20Manual.pdf (accessed on 26 July 2018).
- Medical Research Council. Developing and Evaluating Complex Interventions: New Guidance. 2006. Available online: https://mrc.ukri.org/documents/pdf/complex-interventions-guidance/ (accessed on 26 July 2018).
- Aunger, R.; Curtis, V. Behaviour Centred Design: Towards an applied science of behaviour change. Health Psychol. Rev. 2016, 10, 425–446. [Google Scholar] [CrossRef] [PubMed]
- Greenland, K.; Chipungu, J.; Curtis, V.; Schmidt, W.P.; Siwale, Z.; Mudenda, M.; Chilekwa, J.; Lewis, J.J.; Chilengi, R. Multiple behaviour change intervention for diarrhoea control in Lusaka, Zambia: A cluster randomised trial. Lancet Glob. Health 2016, 4, e966–e977. [Google Scholar] [CrossRef]
- White, S.; Schmidt, W.; Sahanggamu, D.; Fatmaningrum, D.; van Liere, M.; Curtis, V. Can gossip change nutrition behaviour? Results of a mass media and community-based intervention trial in East Java, Indonesia. Trop. Med. Int. Health 2016, 21, 348–364. [Google Scholar] [CrossRef] [PubMed]
- Omprasad, G. Food hygiene intervention to improve food hygiene behaviours, and reduce food contamination in Nepal: An exploratory trial. Ph.D. Thesis, Medicine, London School of Hygiene & Tropical Medicine, London, UK, 2015. [Google Scholar] [CrossRef]
- Biran, A.; Schmidt, W.-P.; Varadharajan, K.S.; Rajaraman, D.; Kumar, R.; Greenland, K.; Gopalan, B.; Aunger, R.; Curtis, V. Effect of a behaviour-change intervention on handwashing with soap in India (SuperAmma): A cluster-randomised trial. Lancet Glob. Health 2014, 2, e145–e154. [Google Scholar] [CrossRef]
- Bright, T.; Wallace, S.; Kuper, H. A Systematic Review of Access to Rehabilitation for People with Disabilities in Low- and Middle-Income Countries. Int. J. Environ. Res. Public Health 2018, 15, 2165. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Deafness and Hearing Loss. 2018. Available online: http://www.who.int/mediacentre/factsheets/fs300/en/ (accessed on 16 April 2018).
- Mulwafu, W.; Kuper, H.; Viste, A.; Goplen, F.K. Feasibility and acceptability of training community health workers in ear and hearing care in Malawi: A cluster randomised controlled trial. BMJ Open 2017, 7, e016457. [Google Scholar] [CrossRef]
- Murthy, G.V.; Mactaggart, I.; Mohammad, M.; Islam, J.; Noe, C.; Khan, A.I.; Foster, A. Assessing the prevalence of sensory and motor impairments in childhood in Bangladesh using key informants. Arch. Dis. Child. 2014, 99, 1103–1108. [Google Scholar] [CrossRef]
- Center for Theory of Change. What Is Theory of Change? 2017. Available online: http://www.theoryofchange.org/what-is-theory-of-change/ (accessed on 27 June 2018).
- JMP; World Health Organization; UNICEF. Post-2015 WASH Targets and Indicators. Available online: https://www.unicef.org/wash/files/4_WSSCC_JMP_Fact_Sheets_4_UK_LoRes.pdf (accessed on 25 July 2018).
- Madans, J.H.; Loeb, M.E.; Altman, B.M. Measuring disability and monitoring the UN Convention on the Rights of Persons with Disabilities: the work of the Washington Group on Disability Statistics. BMC Public Health 2011, 11. [Google Scholar] [CrossRef]
- White, S.; Kuper, H.; Itimu-Phiri, A.; Holm, R.; Biran, A. A Qualitative Study of Barriers to Accessing Water, Sanitation and Hygiene for Disabled People in Malawi. PLoS ONE 2016, 11, e0155043. [Google Scholar] [CrossRef] [PubMed]
- Groce, N.; Bailey, N.; Lang, R.; Trani, J.; Kett, M. Water and sanitation issues for persons with disabilities in low- and middle-income countries: A literature review and discussion of implications for global health and international development. J. Water Health 2011, 9, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Wilbur, J.; Jones, H.; Gosling, L.; Groce, N.; Challenger, E. Undoing inequity: Inclusive water, sanitation and hygiene programmes that deliver for all in Uganda and Zambia. In Proceedings of the 36th WEDC International Conference, Nakuru, Kenya, 14–17 October 2013. [Google Scholar]
- Western Association of Schools and Colleges (WASC). As We Grow up MHM Videos (Indian Sign Language); Western Association of Schools and Colleges (WASC): Burlingame, CA, USA, 2018. [Google Scholar]
- Western Association of Schools and Colleges (WASC). As We Grow up: A Tactile Book on Menstrual Hygiene Management; Western Association of Schools and Colleges (WASC): Burlingame, CA, USA, 2018. [Google Scholar]
- De Silva, M.J.; Breuer, E.; Lee, L.; Asher, L.; Chowdhary, N.; Lund, C.; Patel, V. Theory of Change: A theory-driven approach to enhance the Medical Research Council’s framework for complex interventions. Trials 2014, 15, 267. [Google Scholar] [CrossRef]
- Asher, L.; Fekadu, A.; Hanlon, C.; Mideksa, G.; Eaton, J.; Patel, V.; De Silva, M.J. Development of a Community-Based Rehabilitation Intervention for People with Schizophrenia in Ethiopia. PLoS ONE 2015, 10, e0143572. [Google Scholar] [CrossRef] [PubMed]
- Rajaraman, D.; Varadharajan, K.S.; Greenland, K.; Curtis, V.; Kumar, R.; Schmidt, W.-P.; Aunger, R.; Biran, A. Implementing effective hygiene promotion: lessons from the process evaluation of an intervention to promote handwashing with soap in rural India. BMC Public Health 2014, 14, 1179. [Google Scholar] [CrossRef]
- Devine, C. The Moon, the Stars, and A Scar: Body Mapping Stories of Women Living with HIV/AIDS. Available online: https://www.researchgate.net/publication/312022551_The_Moon_the_Stars_and_a_Scar_Bodymapping_stories_of_women_living_with_HIVAIDS (accessed on 5 December 2018).
- LSHTM; International Centre for Evidence in Disability; CBM; CSF; Hambisela. Getting to know Cerebral Palsy. Working with Parent Groups—A Training Resource for Facilitators, Parents, Caregivers, and Persons with Cerebral Palsy; LSHTM: London, UK, 2013. [Google Scholar]
- De Jager, A.; Tewson, A.; Ludlow, B.; Boydell, K. Embodied Ways of Storying the Self: A Systematic Review of Body-Mapping. Forum Qual. Soc. Res. 2016, 17. [Google Scholar] [CrossRef]
- Wickenden, M.; Kembhavi-Tam, G. Ask us too! Doing participatory research with disabled children in the global south. Childhood 2014, 21, 400–417. [Google Scholar] [CrossRef]
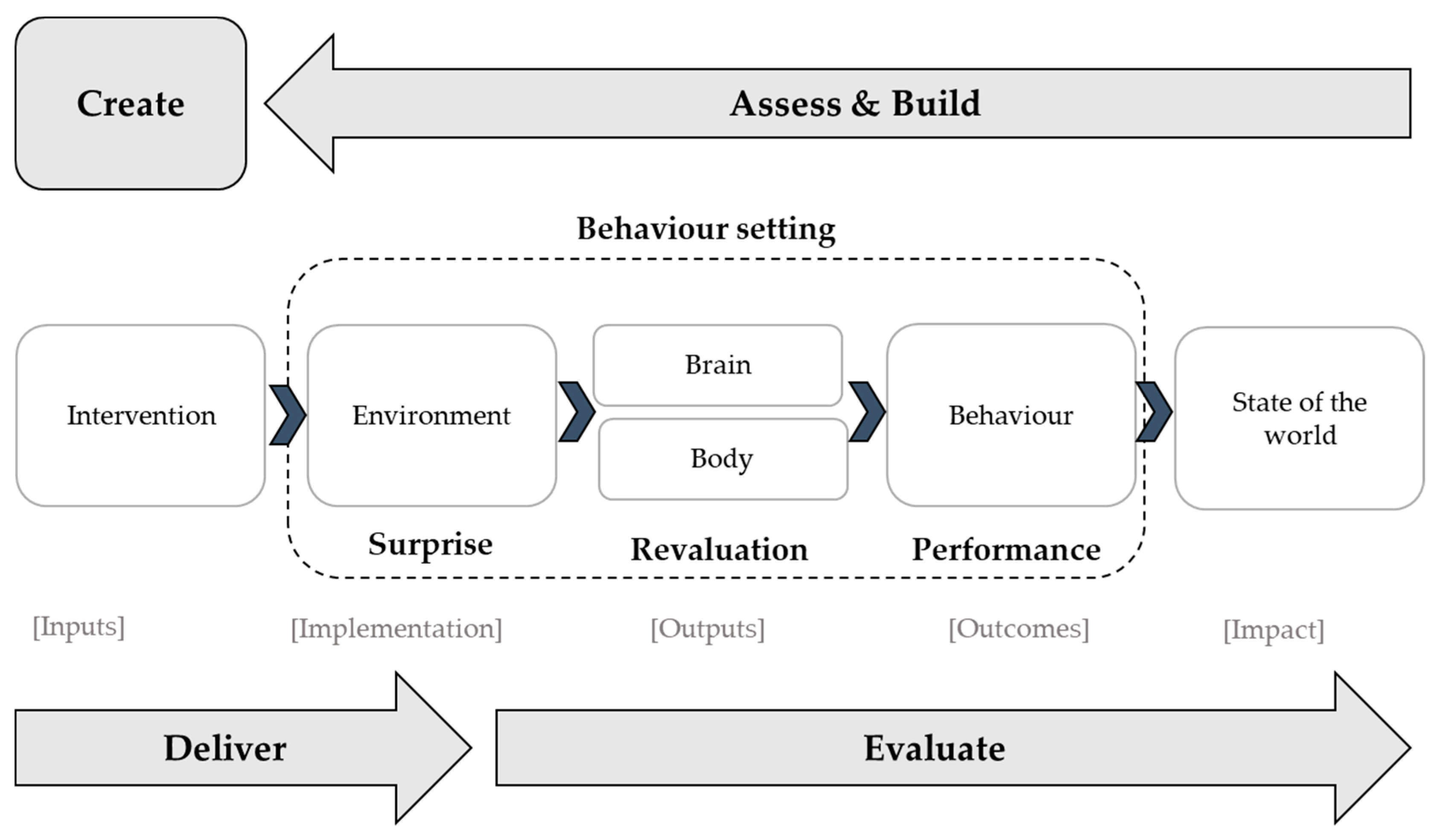

| BCD | MRC | |
|---|---|---|
| Step 1 | Assess and build | Identifying the desired outcome |
| Step 2 | Create | Identifying how to bring about change based on theory and evidence |
| Step 3 | Deliver | Testing the feasibility of the intervention to ensure that it is acceptable and can be delivered as intended; |
| Step 4 | Evaluate | Evaluation of the intervention through both impact and process evaluations. |
| Barrier | Outcome | Proposed Interventions | |
|---|---|---|---|
| 1 | Fear and uncertainty about the referral hospital | Reduced fear about hospital | Peer support/counseling Information about hospital procedures communicated effectively during outreach |
| 2 | Procedural problems within the camps leading to lack of understanding about the referral | Sufficient information about referral | Information provided through:
|
| 3 | Low awareness and understanding of hearing loss/hearing loss is not prioritised | Improved awareness and understanding about ear and hearing health; hearing loss is prioritised | Ear/hearing day advocacy event Education of “gatekeepers” in the community (e.g., community leaders) |
| 4 | Distance to the hospital | Service available closer to the community | Expand outreach camps in the community |
| 5 | Lack and cost of transport | Transport is available | Group transport provided with community escort |
| Relevant Intervention Component | Target Group | Target Behaviour | Human Motive | Relevant Intervention Training Activity |
|---|---|---|---|---|
| Menstrual storage and shoulder bag, menstrual bin | Person with an intellectual impairment | Use a menstrual product | Comfort, dignity | Bishesta doll, role play |
| Pain symbol bangle | Use pain relief for menstrual cramps | Comfort, reward | ||
| Menstrual shoulder bag, visual stories | Does not show menstrual blood in public | Affiliate, dignity | Bishesta doll, role play ‘Reading’ visual stories with carers | |
| Menstrual storage and shoulder bag, menstrual bin | Carer | Provide enough menstrual products | Nurture, affiliate, reward | Emo-demos (surprising and motivating demonstrations and activities), peer-to-peer support, competition to become ‘Bishesta households’, guiding the person they care for through Bishesta doll role play and ‘reading’ visual stories, household monitoring visits/ad-hoc support |
| Menstrual calendar, visual stories | Provide pain relief for menstrual cramps | Nurture, reward | ||
| Menstrual calendar, visual stories | Provide emotional support | Nurture, reward |
| Stage | Malawi | Nepal |
|---|---|---|
| Assess | Systematic review of relevant literature | Systematic review of relevant literature |
| Build | Formative research:
| Formative research:
|
| Create |
|
|
| Deliver | Feasibility study | Feasibility study |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilbur, J.; Bright, T.; Mahon, T.; Hameed, S.; Torondel, B.; Mulwafu, W.; Kuper, H.; Polack, S. Developing Behaviour Change Interventions for Improving Access to Health and Hygiene for People with Disabilities: Two Case Studies from Nepal and Malawi. Int. J. Environ. Res. Public Health 2018, 15, 2746. https://doi.org/10.3390/ijerph15122746
Wilbur J, Bright T, Mahon T, Hameed S, Torondel B, Mulwafu W, Kuper H, Polack S. Developing Behaviour Change Interventions for Improving Access to Health and Hygiene for People with Disabilities: Two Case Studies from Nepal and Malawi. International Journal of Environmental Research and Public Health. 2018; 15(12):2746. https://doi.org/10.3390/ijerph15122746
Chicago/Turabian StyleWilbur, Jane, Tess Bright, Thérèse Mahon, Shaffa Hameed, Belen Torondel, Wakisa Mulwafu, Hannah Kuper, and Sarah Polack. 2018. "Developing Behaviour Change Interventions for Improving Access to Health and Hygiene for People with Disabilities: Two Case Studies from Nepal and Malawi" International Journal of Environmental Research and Public Health 15, no. 12: 2746. https://doi.org/10.3390/ijerph15122746
APA StyleWilbur, J., Bright, T., Mahon, T., Hameed, S., Torondel, B., Mulwafu, W., Kuper, H., & Polack, S. (2018). Developing Behaviour Change Interventions for Improving Access to Health and Hygiene for People with Disabilities: Two Case Studies from Nepal and Malawi. International Journal of Environmental Research and Public Health, 15(12), 2746. https://doi.org/10.3390/ijerph15122746





