Focusing on Coal Workers’ Lung Diseases: A Comparative Analysis of China, Australia, and the United States
Abstract
1. Introduction
2. The Situation of Coal Workers’ Lung Diseases in China, Australia, and the USA
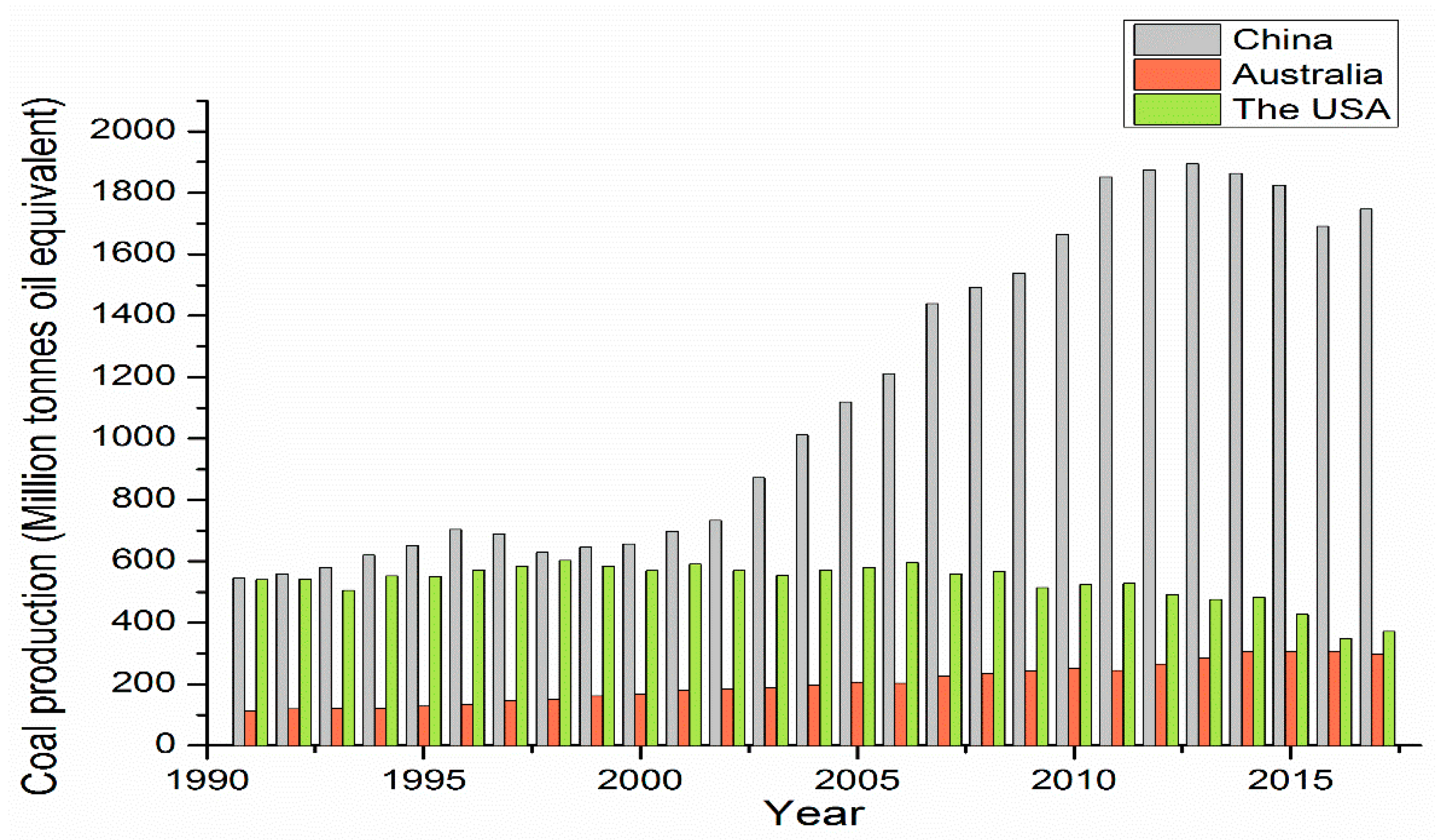
2.1. Coal Production in China, Australia, and the USA
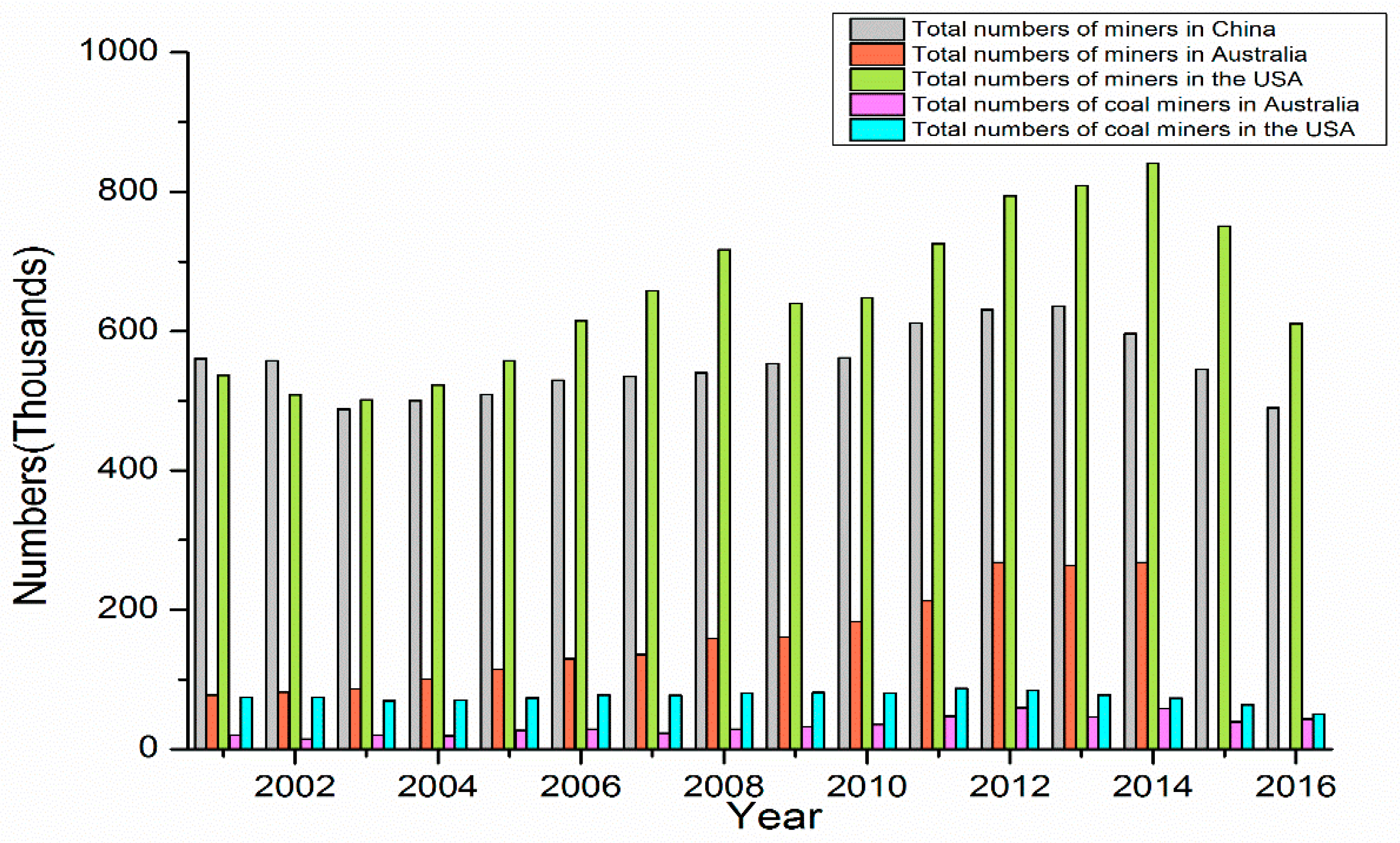
2.2. Coal Miners in China, Australia, and the USA
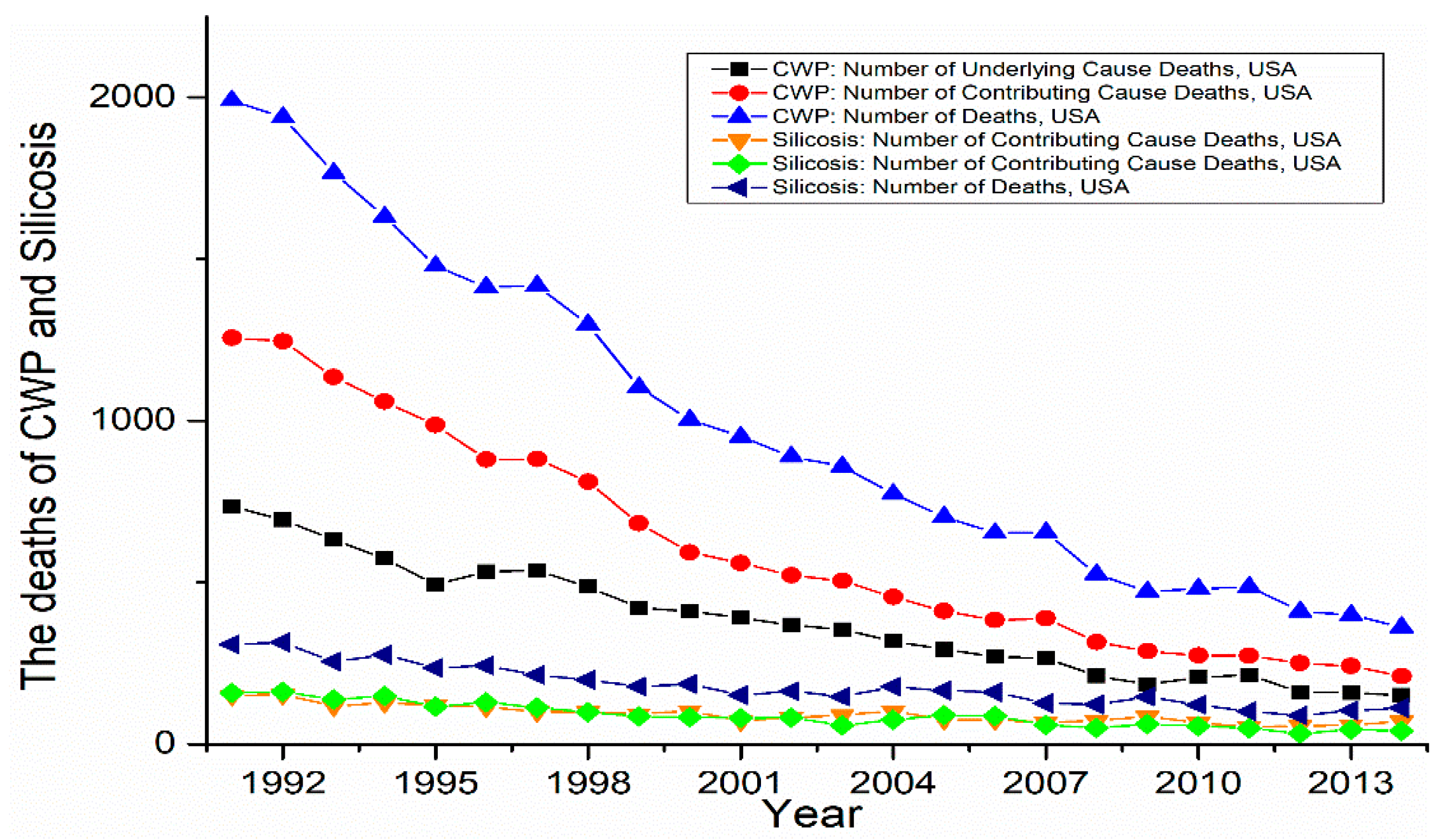
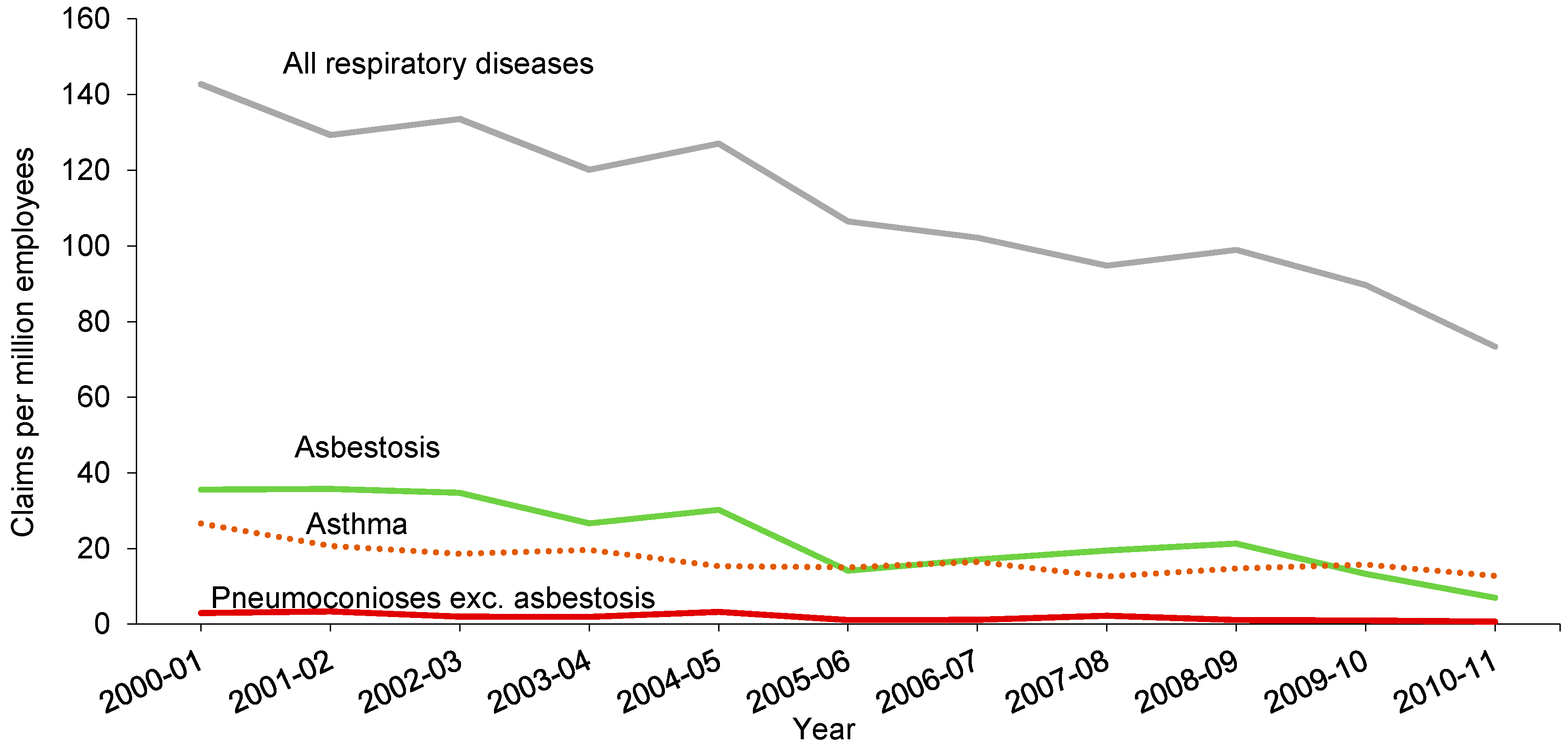
2.3. The Pneumoconiosis of Coal Miners in China, Australia, and the USA
3. Comparative Analysis of China, Australia, and the USA
3.1. The Coal Dust Management
3.1.1. The Geological Conditions of Coal Mine
3.1.2. The Mitigation of Coal Dust
3.1.3. The Monitoring of Respirable Coal Dust
3.2. The Health Management of Coal Workers’ Lung Diseases
3.2.1. The Health Examination for Coal Workers
3.2.2. The Participants of Health Management
3.2.3. The Compensations of Coal Workers with Lung Diseases
4. Conclusions and Suggestions
- China is the primary coal-producing country in the world and also has the largest number of coal workers, which is more than five times the number of workers in the USA and Australia. This means that more people are at risk of exposure to coal dust. At the same time, the Chinese coal mines were characterised as consisting of more small and state-owned mines compared with the large, private coal mines in the USA and Australia. These small mines are reporting more serious diseases due to the absence of lung disease management.
- The number of cases of lung disease in coal workers is rising every year in China; more than 20,000 new cases of CWP and silicosis have been appearing per year since 2010. In contrast, the number of cases and deaths due to lung diseases generally declined or was kept at a stable, low level in the USA and Australia, where the prevalence of CWP in Australia was still lower than 0.5%.
- The geological conditions of China, when compared with the USA and Australia, fundamentally disadvantages the country for coal mining; most coal mines need to be underground coal mines that compete with complex fault systems, and the coal rank and soft host rock increase dust production.
- Methods and standards for the mitigation of coal dust, including the main mining methods, engineering controls, and respiratory protective equipment, are weaker and less implemented in China compared with the USA and Australia, especially within the small coal mines. Meanwhile, the USA is the leading developer of new mitigation methods.
- A disparity in the occupational exposure limit existed among the three countries, where China and Australia have relatively low requirements compared to the USA. China was lagging behind the USA and Australia in terms of physical monitoring devices usage of respirable dust and inspection implements.
- The examination and diagnosis of lung diseases in China were less effective due to the lack of access to medical support such as mobile units or integrated health services compared with the USA and Australia. Likewise, there was a gap between the training of B readers/medical practitioners in the USA and China, which affects the precision of lung disease diagnoses. In addition, Australia has a more cooperative, integrated awareness of the examination and diagnoses of lung diseases than China.
- In China, the governance of occupational diseases occurred solely through the governments, which differed with the cooperative governance in the USA and Australia, where the government, industries, coal workers, unions, and so on had a higher degree of involvement and more effective issue resolution.
- Compared with the USA and Australia, the consequences for coal operators implicated in cases of occupational diseases were relatively lenient, and there is ineffective compensation for coal workers with lung diseases. Additionally, the health coverage for retired coal workers was not adequate in China.
- To increase health awareness, keeping pace with safety management.
- To accelerate technological control of mitigation of coal dust.
- To update and popularise the monitoring devices of coal dust and perfect inspection management.
- To strengthen the health examinations for coal workers.
- To advocate cooperative governance for occupational diseases.
- To reform regulation, simplify the process, and enhance the implementation of compensations for coal workers with lung diseases.
- To improve the health management of retired coal workers.
- To establish a complete and efficient data system for the health assessment of occupational diseases
Author Contributions
Funding
Conflicts of Interest
References
- British Petroleum (BP). BP Energy Outlook. Available online: https://www.bp.com/en/global/corporate/energy-economics/energy-outlook/energy-outlook-downloads.html (accessed on 15 June 2018).
- British Petroleum (BP). BP Statistical Review of World Energy. Available online: https://www.bp.com/en/global/corporate/media/reports-and-publications.html (accessed on 10 June 2018).
- National Bureau of Statistics of China (NBSC). The Portion of Energy Consumption. Available online: http://www.stats.gov.cn/tjsj/ndsj/2017/indexch.htm (accessed on 5 June 2018).
- Diagnostic Pathology. Coal. Available online: http://www.diagnosticpathology.eu/content/minfib/Coal.php (accessed on 26 October 2018).
- GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 385, 117–171. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Global Health Risks. 2009. Available online: http://www.who.int/healthinfo/global_burden_disease/GlobalHealthRisks_report_full.pdf (accessed on 8 June 2018).
- International Labour Organization (LIO). Occupational Health: Silicosis. Available online: http://www.ilo.org/safework/areasofwork/occupational-health/WCMS_108566/lang--en/index.htm (accessed on 5 July 2018).
- Zhang, Z.; Zhao, Y.; Sun, D. China’s occupational health challenges. Occup. Med. 2017, 67, 87–90. [Google Scholar] [CrossRef] [PubMed]
- National Health and Family Planning Commission (NHFPC). National Occupational Diseases Report for 2015. Available online: http://www.nhfpc.gov.cn/jkj/s5899t/201712/c46227a95f054f5fa75a40e4db05bb37.shtml (accessed on 5 May 2018).
- People. The Numbers of Coal Miners Workers’ Pneumoconiosis. Available online: http://env.people.com.cn/n/2015/0209/c1010-26530066.html (accessed on 6 June 2018).
- Wang, X.; Meng, F.-B. Statistical analysis of large accidents in China’s coal mines in 2016. Nat. Hazards 2018, 92, 311–325. [Google Scholar] [CrossRef]
- Perret, J.L.; Plush, B.; Lachapelle, P.; Hinks, T.S.; Walter, C.; Clarke, P.; Irving, L.; Brady, P.; Dharmage, S.C.; Stewart, A. Coal mine dust lung disease in the modern era. Respirology 2017, 22, 662–670. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention (CDC). One Hundred Years of Federal Mining Safety and Health. Available online: https://www.cdc.gov/niosh/mining/userfiles/works/pdfs/2010-128.pdf (accessed on 25 July 2018).
- Mo, J.; Wang, L.; Au, W.; Su, M. Prevalence of coal workers’ pneumoconiosis in China: A systematic analysis of 2001–2011 studies. Int. J. Hyg. Environ. Health 2014, 217, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Laney, A.S.; Attfield, M.D. Coal workers’ pneumoconiosis and progressive massive fibrosis are increasingly more prevalent among workers in small underground coal mines in the United States. Occup. Environ. Med. 2010, 67, 428–431. [Google Scholar] [CrossRef] [PubMed]
- Joy, G.J.; Colinet, J.F.; Landen, D. Coal workers’ pneumoconiosis prevalence disparity between Australia and the United States. Min. Eng. 2012, 64, 65–71. [Google Scholar]
- Cohen, R.A. Is the increasing prevalence and severity of coal workers’ pneumoconiosis in the United States due to increasing silica exposure? Occup. Environ. Med. 2010, 67, 649–650. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Yano, E.; Nonaka, K.; Wang, M.; Wang, Z. Respiratory impairments due to dust exposure: A comparative study among workers exposed to silica, asbestos, and coalmine dust. Am. J. Ind. Med. 2010, 31, 495–502. [Google Scholar] [CrossRef]
- Ji, Y.; Ren, T.; Wynne, P.; Wan, Z.; Ma, Z.; Wang, Z. A comparative study of dust control practices in Chinese and Australian longwall coal mines. Int. J. Min. Sci. Technol. 2016, 26, 199–208. [Google Scholar] [CrossRef]
- He, X.; Song, L. Status and future tasks of coal mining safety in China. Saf. Sci. 2012, 50, 894–898. [Google Scholar] [CrossRef]
- Shen, L.; Gao, T.-M.; Cheng, X. China’s coal policy since 1979: A brief overview. Energy Policy 2012, 40, 274–281. [Google Scholar] [CrossRef]
- State Administration of Work Safety (SAWS). Research on the Labor-Management on Coal Mine Workers; SAWS: Beijing, China, 2013.
- National Energy Administration (NEA). The Capacity of Coal Production in 2017. Available online: http://www.nea.gov.cn/ztzl/mtscnlgg/index.htm (accessed on 8 May 2018).
- Andrews-Speed, P.; Yang, M.; Shen, L.; Cao, S. The regulation of China’s township and village coal mines: A study of complexity and ineffectiveness. J. Clean. Prod. 2003, 11, 185–196. [Google Scholar] [CrossRef]
- McGrath-Champ, S. Labour management space, and restructuring of the Australian coal industry. Environ. Plan. A. 1993, 25, 1295–1318. [Google Scholar] [CrossRef]
- Goodman, J.; Worth, D. The minerals boom and Australia’s ’resource curse’. J. Aust. Polit. Econ. 2008, 61, 201–219. [Google Scholar]
- Darling, P. SME Mining Engineering Handbook; SME: Englewood, CO, USA, 2011; Volume 1. [Google Scholar]
- Connolly, E.; Orsmond, D. The Mining Industry: From Bust to Boom; Reserve Bank of Australia: Sydney, Australia, 2011.
- Riley, C.I. Chris Top U.S. Coal Company Peabody Energy Files for Bankruptcy. Available online: https://money.cnn.com/2016/04/13/news/companies/peabody-coal-bankruptcy/index.html (accessed on 9 October 2018).
- Center for Disease Control and Prevention (CDC). Statistics: All Mining. Available online: https://www.cdc.gov/niosh/mining/statistics/allmining.html (accessed on 9 May 2018).
- Bureau of Labor Statistics (BLS). Employment, Hours, and Earnings from the Current Employment Statistics Survey (National). Available online: https://data.bls.gov/timeseries/CES1021210001 (accessed on 6 August 2018).
- Australia Industry and Skills Committee (AISC). Coal Mining. Available online: https://nationalindustryinsights.aisc.net.au/industries/mining-drilling-and-civil-infrastructure/coal-mining (accessed on 10 July 2018).
- Australia Bureau of Statistics (ABC). Mining Operations, Australia. Available online: http://www.abs.gov.au/Mining (accessed on 1 November 2018).
- Chen, H.; Feng, Q.; Long, R.; Qi, H. Focusing on coal miners’ occupational disease issues: A comparative analysis between China and the United States. Saf. Sci. 2013, 51, 217–222. [Google Scholar] [CrossRef]
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2015 and 2016. Available online: http://www.moh.gov.cn/jkj/s5899t/201712/c46227a95f054f5fa75a40e4db05bb37.shtml (accessed on 2 July 2018).
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2014. Available online: http://www.nhfpc.gov.cn/jkj/s5899t/201512/c5a99f823c5d4dd48324c6be69b7b2f9.shtml (accessed on 25 August 2018).
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2013. Available online: http://www.chinacdc.cn/jlm/wdwsdxgbd/201407/t20140701_98951.htm (accessed on 25 August 2018).
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2012. Available online: http://www.moh.gov.cn/jkj/s5899t/201309/9af5b88cc6ea40d592e8a5e0aa76914a.shtml. (accessed on 26 October 2018).
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2011. Available online: http://www.nhfpc.gov.cn/jkj/s5899t/201309/14ddbd8fcd7b4385a1d0a6351b5cebfc.shtml (accessed on 26 October 2018).
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2010. Available online: http://www.cnki.com.cn/Article/CJFDTotal-ZYWS201103002.htm (accessed on 26 October 2018).
- Chinese Center for Disease Control and Prevention (CCDCP). Report on Occupational Disease Prevention in 2009. Available online: http://www.nhfpc.gov.cn/zwgk/jdjd/201304/b1b28f32be3f451781483d9ac6c59b25.shtml (accessed on 26 October 2018).
- Ministry of Health (MOH). Report on Occupational Disease Prevention in 2008. Available online: http://www.moh.gov.cn/mohbgt/s9511/200905/40893.shtml (accessed on 25 October 2018).
- Ministry of Health (MOH). Report on Occupational Disease Prevention in 2007. Available online: http://www.moh.gov.cn/mohbgt/pw10808/200805/35672.shtml (accessed on 25 October 2018).
- National Health and Family Planning Commission (NHFPC). Report on Occupational Disease Prevention in 2006. Available online: http://www.nhfpc.gov.cn/mohwsbwstjxxzx/s7967/200805/34857.shtml (accessed on 25 October 2018).
- National Health and Family Planning Commission (NHFPC). Report on Occupational Disease Prevention in 2005. Available online: http://www.nhfpc.gov.cn/zwgk/jdjd/201304/fe828bd2d44e47569a859c7ae36f7ba5.shtml (accessed on 25 October 2018).
- Yin, Y. A trend analysis on the national pneumoconiosis epidemics in 2003. China Occup. Med. 2005, 32, 20–22. [Google Scholar]
- Center for Disease Control and Prevention (CDC). Coal Workers’ Health Surveillance Program (CWHSP) Data Query System. Available online: https://webappa.cdc.gov/ords/cwhsp-database.html (accessed on 4 December 2018).
- Center for Disease Control and Prevention (CDC). Coal Workers’ Pneumoconiosis. Available online: https://wwwn.cdc.gov/eworld/Grouping/Coal_Workers_Pneumoconiosis/93#Mortality%20Data (accessed on 1 April 2018).
- Blackley, D.J. Resurgence of progressive massive fibrosis in coal miners—Eastern Kentucky, 2016. MMWR Morb. Mortal. Wkly Rep. 2016, 65, 1385–1389. [Google Scholar] [CrossRef] [PubMed]
- Blackley, D.J.; Halldin, C.N.; Laney, A.S. Continued Increase in Prevalence of Coal Workers’ Pneumoconiosis in the United States, 1970–2017. Am. J. Public Health 2018, 108, 1220–1222. [Google Scholar] [CrossRef] [PubMed]
- Australian Government. Occupational Respiratory Diseases in Australia; Australian Government: Canberra, Australia, 2006; pp. 1–21.
- Australian Institute of Health and Welfare. GRIM (General Record of Incidence of Mortality) Books; AIHW: Canberra, Australia, 2005.
- Smith, D.R.; Leggat, P.A. 24 years of pneumoconiosis mortality surveillance in Australia. J. Occup. Health 2006, 48, 309–313. [Google Scholar] [CrossRef] [PubMed]
- Safe Work Australia (SWA). Occupational Disease Indicators; SWA: Canberra, Australia, 2014.
- Parliamentary Committees. Inquiry into the re-identification of Coal Workers’ Pneumoconiosis in Queensland; Parliamentary Committees: Brisbane, Australia, 2017.
- United States Government Accountability Office (USGAO). MINE SAFETY: Reports and Key Studies Support the Scientific Conclusions Underlying the Proposed Exposure Limit for Respirable Coal Mine Dust. Available online: http://www.gao.gov/assets/600/593780.pdf (accessed on 9 December 2018).
- Zhang, M.; Wang, D.; Zheng, Y.-D.; Du, X.-Y.; Chen, S.-Y. Analyses on the characteristics and the trends of pneumoconiosis notified between 1997 and 2009, in China. Chin. J. Ind. Hyg. Occup. Dis. 2013, 31, 321–334. [Google Scholar]
- Ma, S.Q.; Wu, S.S. Comparison of the present situation of coal workers’ pneumoconiosis control between the USA and China. J. North China Inst. Sci. Techonol. 2015, 12, 42–46. [Google Scholar]
- Laney, A.S.; Weissman, D.N. Respiratory diseases caused by coal mine dust. J. Occup. Environ. Med. 2014, 56, S18. [Google Scholar] [CrossRef] [PubMed]
- Hu, S. The Number of Chinese Coal Mines in 2017. Available online: http://www.sohu.com/a/220181037_823383 (accessed on 3 May 2018).
- Energy Information Administration (EIA). Coal Production and Number of Mines by State and Mine Type, 2014–2015; EIA: Washington, DC, USA, 2017.
- Coal Services. NSW Coal Industry Statistics. Available online: https://www.coalservices.com.au/mining/news-and-events/industry-newsletters/nsw-coal-industry-statistics/ (accessed on 2 June 2018).
- Department of Natural Resources and Mines (DNRM). Queensland Coal–Mines and Advanced Projects. Available online: https://www.dnrm.qld.gov.au/__data/assets/pdf_file/0011/238079/coal-mines-advanced-projects.pdf (accessed on 3 July 2018).
- Castranova, V.; Vallyathan, V. Silicosis and coal workers’ pneumoconiosis. Environ. Health Perspect. 2000, 108 (Suppl. 4), 675–684. [Google Scholar] [PubMed]
- Chen, W.; Yang, J.; Chen, J.; Bruch, J. Exposures to silica mixed dust and cohort mortality study in tin mines: Exposure-response analysis and risk assessment of lung cancer. Am. J. Ind. Med. 2006, 49, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Gamble, J.; Reger, R.; Glenn, R. A Critical Review of Coal Workers Pneumoconiosis (CWP) and Coal Rank for Evaluation of Safe Exposure Levels in Coal Mining. J. Clin. Toxicol. 2012, 1, 2161-0495. [Google Scholar] [CrossRef]
- Bennett, J.; Dick, J.; Kaplan, Y.; Shand, P.; Shennan, D.; Thomas, D.; Washington, J. The relationship between coal rank and the prevalence of pneumoconiosis. Occup. Environ. Med. 1979, 36, 206–210. [Google Scholar] [CrossRef]
- Australia Government. Coal. Available online: http://www.ga.gov.au/data-pubs/data-and-publications-search/publications/australian-minerals-resource-assessment/coal (accessed on 3 June 2018).
- Seaton, A.; Dodgson, J.; Dick, J.; Jacobsen, M. Quartz and pneumoconiosis in coalminers. Lancet 1981, 318, 1272–1275. [Google Scholar] [CrossRef]
- Song, X.; Mu, X. The safety regulation of small-scale coal mines in China: Analysing the interests and influences of stakeholders. Energy Policy 2013, 52, 472–481. [Google Scholar] [CrossRef]
- Andrews-Speed, P.; Ma, G.; Shao, B.; Liao, C. Economic responses to the closure of small-scale coal mines in Chongqing, China. Resour. Pol. 2005, 30, 39–54. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention (CDC). Advanced Measurement Methods in Mining. Available online: https://www.cdc.gov/niosh/mining/UserFiles/works/pdfs/ammim.pdf (accessed on 9 July 2018).
- Jeffrey, S.B.; Craig, E.C. Respiratory Protective Equipment. Available online: https://doi.org/10.1002/0471435139.hyg032.pub2 (accessed on 19 June 2018).
- Noone, P. Respiratory protective equipment. Occup. Med. 2011, 61, 449. [Google Scholar] [CrossRef]
- University of Western Australia (UWA). Respiratory Protection. Available online: http://www.safety.uwa.edu.au/topics/physical/protective-equipment/respiratory (accessed on 6 April 2018).
- Che, Y.H.; Guo, J.F.; Dong, S.X. A comparison of sino-American test standards of respiratory protective equipment. Test Stand. 2014, 9, 86–88. [Google Scholar]
- Borak, J.; Brosseau, L.M. The past and future of occupational exposure limits. J. Occup. Environ. Hyg. 2015, 12 (Suppl. 1), S1–S3. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.H. Difference of health standards for coal dust concentration in workplace air at home and abroad. Occup. Health 2015, 31, 714–717. [Google Scholar]
- Mine Safety and Health Administration (MSHA). Final Rule: Lowering Mines’ Exposure to Respirable Coal Mine Dust, Including Continuous Personal Dust Monitors. Fed. Reg. 2014, 79, 24814–24994. [Google Scholar]
- Mine Safety and Health Administration (MSHA). Respirable Dust Rule: A Historic Step Forward in the Effort to End Black Lung Disease. Available online: https://arlweb.msha.gov/regs/fedreg/final/2014finl/2014-09084.asp (accessed on 23 June 2018).
- Hua, F. The Deaths Caused by Coal Workers’ Pneumoconiosis Were Two Times Than Coal Mine Accidents. Available online: http://news.ifeng.com/mainland/detail_2010_11/10/3054464_0.shtml (accessed on 6 May 2018).
- Qu, M.Z.; Wei, L.L.; Wang, J. Comparison study on dust sampling methods between China and the United States. Technol. Innov. Appl. 2014, 34, 47. [Google Scholar]
- Chen, G. Comparison study on monitoring, assessment and management methods of dust occupational exposure between China and USA. J. Saf. Sci. Technol. 2017, 13, 66–69. [Google Scholar]
- United States Department of Labor (USDOL). First Phase of MSHA’s Respirable Coal Mine Dust Rule Goes into Effect. Available online: https://www.dol.gov/newsroom/releases/msha/msha20141426 (accessed on 23 October 2018).
- MKAQ. Coal Mine Safety Regulation. Available online: http://www.mkaq.org/html/2016/04/02/358178_3.shtml (accessed on 24 July 2018).
- MKAQ. The Detection of Coal Mine Dust. Available online: http://www.mkaq.org/item/294965.aspx (accessed on 2 January 2018).
- Ban, J. Review of major international occupational safety and health events in 2016. Labor Prot. 2017, 2, 41–45. [Google Scholar]
- Zhang, L.Y. Design and implementation of real-time detection system for coal mine dust concentration. Colliery Mech. Electr. Technol. 2016, 1, 19–24. [Google Scholar]
- Cui, K.; Shen, F.; Han, B.; Yuan, J.; Suo, X.; Qin, T.; Liu, H.; Chen, J. Comparison of the cumulative incidence rates of coal workers’ pneumoconiosis between 1970 and 2013 among four state-owned colliery groups in China. Int. J. Environ. Res. Public Health 2015, 12, 7444–7456. [Google Scholar] [CrossRef] [PubMed]
- Shen, F.; Yuan, J.; Sun, Z.; Hua, Z.; Qin, T.; Yao, S.; Fan, X.; Chen, W.; Liu, H.; Chen, J. Risk identification and prediction of coal workers’ pneumoconiosis in Kailuan Colliery Group in China: A historical cohort study. PLoS ONE 2013, 8, e82181. [Google Scholar] [CrossRef] [PubMed]
- Han, L.; Han, R.; Ji, X.; Wang, T.; Yang, J.; Yuan, J.; Wu, Q.; Zhu, B.; Zhang, H.; Ding, B.; et al. Prevalence characteristics of coal workers’ pneumoconiosis (CWP) in a state-owned mine in Eastern China. Int. J. Environ. Res. Public Health 2015, 12, 7856–7867. [Google Scholar] [CrossRef] [PubMed]
- Antao, V.; Petsonk, E.; Sokolow, L.; Wolfe, A.; Pinheiro, G.; Hale, J.; Attfield, M. Rapidly progressive coal workers’ pneumoconiosis in the United States: Geographic clustering and other factors. Occup. Environ. Med. 2005, 62, 670–674. [Google Scholar] [CrossRef] [PubMed]
- Love Save Pneumoconiosis (LSP). Report on the Living Conditions of Migrant Workers of Pneumoconiosis in China. Available online: http://www.daaiqingchen.org/list.php?fid=68 (accessed on 9 February 2018).
- Zhu, Y.; Chen, P.Y.; Zhao, W. Injured workers in China: Injustice, conflict and social unrest. Int. Lab. Rev. 2014, 153, 635–647. [Google Scholar] [CrossRef]
- National Health and Family Planning Commission (NHFPC). Report on China Health Development. Available online: http://www.nhfpc.gov.cn/guihuaxxs/s10743/201806/44e3cdfe11fa4c7f928c879d435b6a18.shtml (accessed on 3 March 2018).
- National Health and Family Planning Commission (NHFPC). China Occupational Health Statistics Yearbook; NHFPC: Beijing China, 2013.
- National People’s Congress (NPC). Regulations on the Prevention and Control of Pneumoconiosis; NPC: Beijing, China, 2017.
- Center for Disease Control and Prevention (CDC). NIOSH Announces Free, Confidential Screenings for Coal Miners. Available online: https://www.cdc.gov/niosh/updates/upd-03-01-18.html (accessed on 10 April 2018).
- Zhang, X.; Wang, Z.; Li, T. The current status of occupational health in China. Environ. Health Prevent. Med. 2010, 15, 263. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.-R.; Christiani, D.C. Occupational lung disease in China. Int. J. Occup. Environ. Health 2003, 9, 320–325. [Google Scholar] [CrossRef] [PubMed]
- Center for Disease Control and Prevention (CDC). Pneumoconiosis Prevalence Among Working Coal Miners Examined in Federal Chest Radiograph Surveillance Programs—United States, 1996–2002. Available online: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5215a3.htm (accessed on 19 March 2018).
- Queensland Government. Coal Workers’ Pneumoconiosis. Available online: https://www.business.qld.gov.au/industries/mining-energy-water/resources/safety-health/mining/medicals/pneumoconiosis/government-response (accessed on 8 March 2018).
- Donham, K.J.; Thelin, A. Agricultural Medicine: Rural Occupational and Environmental Health, Safety, and Prevention; John Wiley & Sons: Hoboken, NJ, USA, 2016. [Google Scholar]
- Fidler, D. Global Health Governance: Overview of the Role of International Law in Protecting and Promoting Global Public Health; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Coal Services. Background–Standing Dust Committee. Available online: https://www.coalservices.com.au/mining/workplace-safety-and-compliance/industry-working-groups/standing-dust-committee/ (accessed on 7 February 2018).
- Coal Services. Coal Services has Representation on Various Industry Working Groups. Available online: https://www.coalservices.com.au/mining/workplace-safety-and-compliance/industry-working-groups/ (accessed on 5 July 2018).
- Huang, Y. Governing Health in Contemporary China; Routledge: Abingdon, UK, 2015. [Google Scholar]
- Li, M. Protection for migrant workers under evolving occupational health and safety regimes in China. Ind. Relat. 2017, 72, 56–76. [Google Scholar] [CrossRef]
- Ramesh, M.; Wu, X.; He, A.J. Health governance and healthcare reforms in China. Health Policy Plan. 2013, 29, 663–672. [Google Scholar] [CrossRef] [PubMed]
- Central People’s Government (CPG). The Adjustment on Occupational Health Functions of the Ministry of Health to the State Administration of Work Safety. Available online: http://www.gov.cn/jrzg/2010-12/27/content_1773727.htm (accessed on 27 May 2018).
- Queensland WorkCover. Coal Workers’ Pneumoconiosis: How Your Workers’ Compensation Claim is Processed by WorkCover. Available online: https://www.worksafe.qld.gov.au/__data/assets/pdf_file/0010/130132/5851-CWP-how-your-claim-is-processed-by-workcover.pdf (accessed on 8 July 2018).
- New South Wales (NSW). Workers Compensation Benefits Guide; State Insurance Regulatory Authority: Gosford, Australia, 2018.
- United States Department of Labor (USDOL). Division of Coal Mine Workers’ Compensation (DCMWC). Available online: https://www.dol.gov/owcp/dcmwc/ (accessed on 5 June 2018).
- National People’s Congress (NPC). Regulations on Worker’s Compensation Insurance. Available online: http://www.npc.gov.cn/npc/ztxw/tctjcxsbtxjs/2014-05/20/content_1863711.htm (accessed on 16 March 2018).
- National Health and Family Planning Commission (NHFPC). Interpretation on the Improvement of Prevention and Treatment for Migrant Workers of Pneumoconiosis. Available online: http://www.nhfpc.gov.cn/jkj/s5899t/201601/2b9c07cea7cb484b86362933db466d66.shtml (accessed on 4 February 2018).
- United States Department of Labor (USDOL). Employment Law Guide. Available online: https://webapps.dol.gov/elaws/elg/blklung.htm (accessed on 5 January 2018).
- Song, Z.; Niu, D.; Xiao, X. Focus on the current competitiveness of coal industry in China: Has the depression time gone? Resour. Pol. 2017, 51, 172–182. [Google Scholar] [CrossRef]
| Years | Occupational Diseases | Pneumoconiosis | Coal Workers’ Pneumoconiosis | Silicosis | Lung Disease of Coal Workers | The Proportion of CWP and Silicosis among Pneumoconiosis |
|---|---|---|---|---|---|---|
| 2003 | 10,571 | 8361 | 4255 | 2836 | 4561 | 84.81% |
| 2004 | - | 8743 | - | - | - | - |
| 2005 | 12,212 | 9173 | 4358 | 3967 | 4477 | 90.76% |
| 2006 | 11,519 | 8783 | 3503 | - | - | - |
| 2007 | 14,296 | 10,963 | 5351 | 4447 | 6554 | 89.37% |
| 2008 | 13,744 | 10,829 | 4924 | 4748 | 5471 | 89.32% |
| 2009 | 18,128 | 14,495 | 7397 | 5922 | 7502 | 91.89% |
| 2010 | 27,240 | 23,812 | 12,564 | 9870 | 13,968 | 94.21% |
| 2011 | 29,879 | 26,401 | 14,000 | 11,122 | - | 95.16% |
| 2012 | 27,420 | 24,206 | 12,405 | 10,592 | 13,399 | 95.01% |
| 2013 | 26,393 | 23,152 | 13,955 | 8095 | 15,078 | 95.24% |
| 2014 | 29,972 | 26,873 | 13,846 | 11,471 | 11,396 | 94.21% |
| 2015 | 29,180 | 26,081 | 14,152 | 10,343 | 11,625 | 93.92% |
| 2016 | 31,789 | 27,992 | 16,658 | 10,072 | 13,070 | 95.49% |
| Category | Countries | China | The USA | Australia |
|---|---|---|---|---|
| Coal mine type (numbers) | Surface coal mine (N) | 439 (in 2017) | 1055 (in 2015) | NSW (22); QLD (37) (2017) |
| Underground coal mine (N) | 7223 (in 2017) | 405 (in 2015) | NSW (20); QLD (13) (2017) | |
| Geological condition | Structural geology |
|
|
|
| Rank of reserved coal |
|
|
| |
| Mitigation of coal dust | Main mining methods |
|
|
|
| Main engineering control methods |
|
|
| |
| Respiratory protective equipment | Particulate respirators: (GB2626-2006)
| Particulate respirators: (42 CFR Part 84)
| Particulate respirators: (AS/NZS 1715 and 1716)
| |
| Monitoring of coal dust | Occupational exposure limit |
|
| Two main states of a coal mine (TWA)
free silica: 0.1 mg/m3
free silica: 0.1 mg/m3 |
| Monitoring devices |
|
|
| |
| Common sampling methods |
|
|
|
| Category | China | The USA | Australia |
|---|---|---|---|
| Periodic health examination |
|
|
|
| Participants |
|
|
|
| Pattern of governance | Government-dominated governance | Co-governance | Co-governance |
| Standard of radiograph | Chinese National Diagnosis Criteria of Pneumoconiosis (GBZ 70-2009) | International Labour Office (ILO) International Classification of Radiographs of Pneumoconiosis | International Labour Office (ILO) International Classification of Radiographs of Pneumoconiosis |
| Insurance |
|
|
|
| Compensation |
|
|
|
| Retiring coal mine workers |
|
|
|
| Penalty of Violation | If coal mines conceal the occupational diseases, punish the coal mines fine of 10,000 to 50,000 RMB, warning or order date of expiration correction, or demotion or dismissal of operators | Operators who knowingly conceal or dispose of any property to avoid the payment of benefits under the Act may be guilty of a misdemeanour and, if convicted, subject to a fine of $1000, imprisonment for up to one year, or both. | The penalty for the discharge of obligations for operators involving exposure to a harmful substance (update 2018): fine of 750 penalty units, to be consistent with the existing maximum penalty unit amount 126,000 AUD and have right of prosecuting an operator or shut down a mine or suspend or cancel statutory certificates of competency (QLD) |
| Health assessment methods |
|
|
|
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Han, S.; Chen, H.; Harvey, M.-A.; Stemn, E.; Cliff, D. Focusing on Coal Workers’ Lung Diseases: A Comparative Analysis of China, Australia, and the United States. Int. J. Environ. Res. Public Health 2018, 15, 2565. https://doi.org/10.3390/ijerph15112565
Han S, Chen H, Harvey M-A, Stemn E, Cliff D. Focusing on Coal Workers’ Lung Diseases: A Comparative Analysis of China, Australia, and the United States. International Journal of Environmental Research and Public Health. 2018; 15(11):2565. https://doi.org/10.3390/ijerph15112565
Chicago/Turabian StyleHan, Shuai, Hong Chen, Maggie-Anne Harvey, Eric Stemn, and David Cliff. 2018. "Focusing on Coal Workers’ Lung Diseases: A Comparative Analysis of China, Australia, and the United States" International Journal of Environmental Research and Public Health 15, no. 11: 2565. https://doi.org/10.3390/ijerph15112565
APA StyleHan, S., Chen, H., Harvey, M.-A., Stemn, E., & Cliff, D. (2018). Focusing on Coal Workers’ Lung Diseases: A Comparative Analysis of China, Australia, and the United States. International Journal of Environmental Research and Public Health, 15(11), 2565. https://doi.org/10.3390/ijerph15112565





