Assessment of Health-Related Quality of Life between People with Parkinson’s Disease and Non-Parkinson’s: Using Data Drawn from the ‘100 for Parkinson’s’ Smartphone-Based Prospective Study
Abstract
1. Introduction
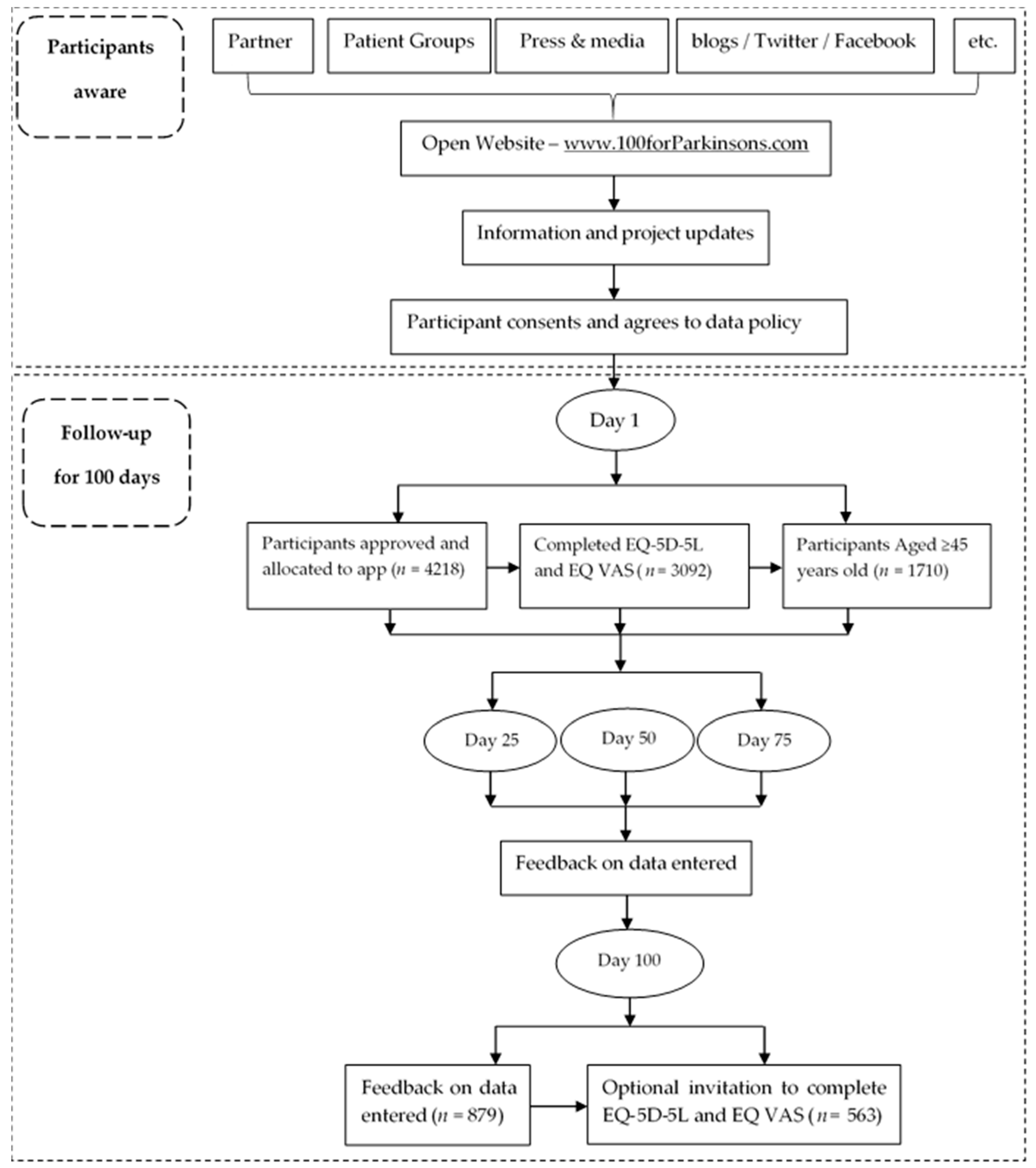
2. Materials and Methods
2.1. Data Source
2.2. Research Ethics
2.3. EQ-5D
2.4. Study Variables
2.5. Statistical Analyses
3. Results
3.1. Characteristics of the Study Population
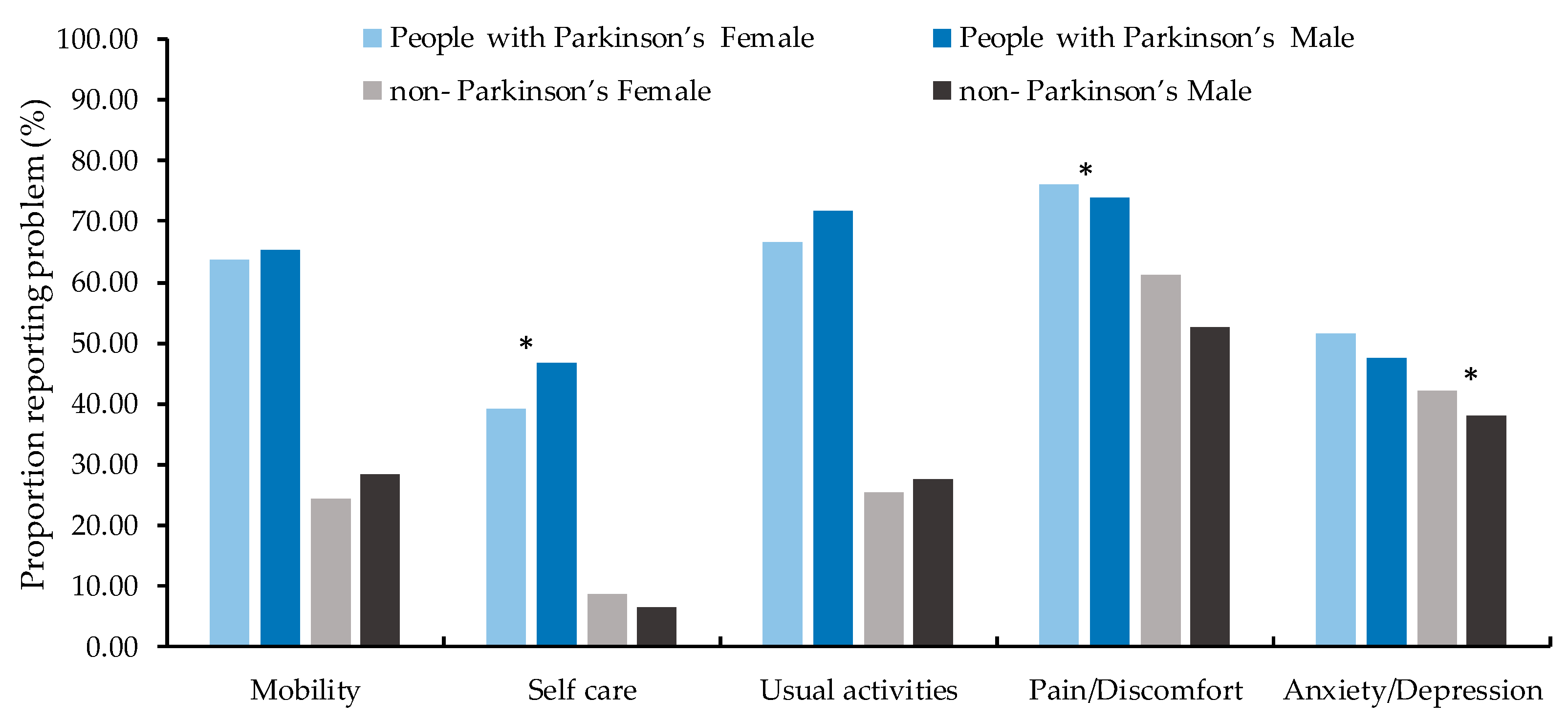
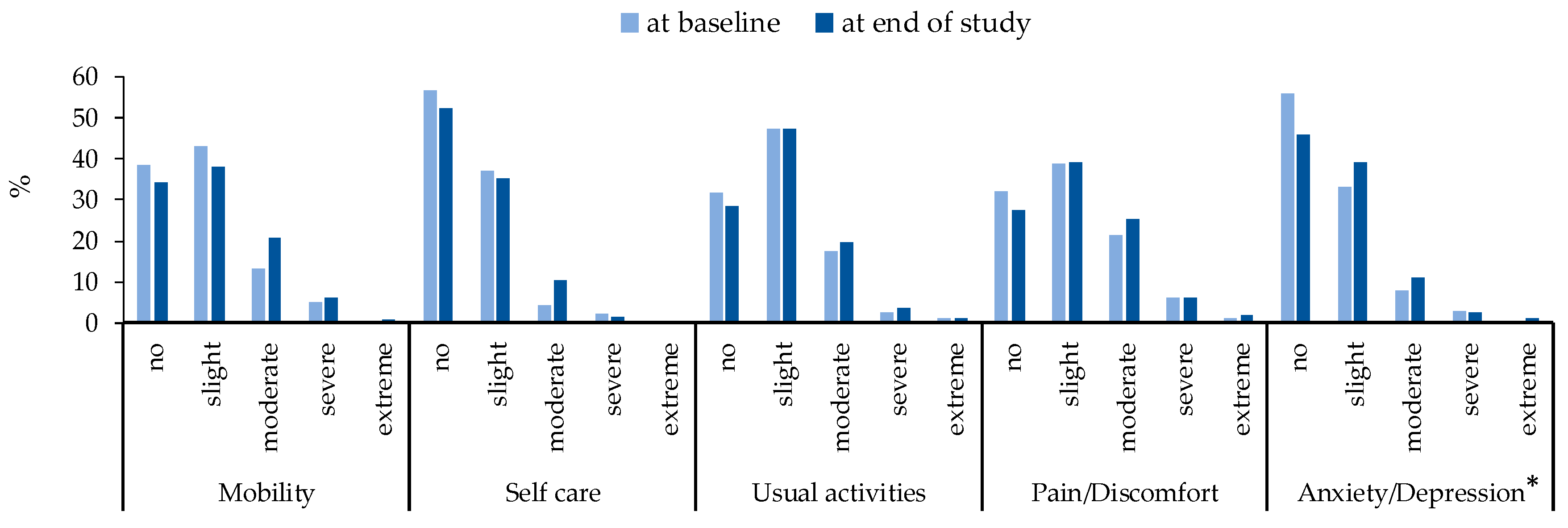
3.2. Main Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Nussbaum, R.L.; Ellis, C.E. Alzheimer’s Disease and Parkinson’s Disease. N. Engl. J. Med. 2003, 348, 1356–1364. [Google Scholar] [CrossRef] [PubMed]
- Lewitt, P.A. Levodopa for the Treatment of Parkinson’s Disease. N. Engl. J. Med. 2008, 359, 2468–2476. [Google Scholar] [CrossRef] [PubMed]
- Dorsey, E.R.; Constantinescu, R.; Thompson, J.P.; Biglan, K.M.; Holloway, R.G.; Kieburtz, K.; Marshall, F.J.; Ravina, B.M.; Schifitto, G.; Siderowf, A. Projected Number of People with Parkinson Disease in the Most Populous Nations, 2005 through 2030. Neurology 2007, 68, 384–386. [Google Scholar] [CrossRef] [PubMed]
- Duncan, G.W.; Khoo, T.K.; Coleman, S.Y.; Brayne, C.; Yarnall, A.J.; O’Brien, J.T.; Barker, R.A.; Burn, D.J. The Incidence of Parkinson’s Disease in the North-East of England. Age Ageing 2014, 43, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Linder, J.; Stenlund, H.; Forsgren, L. Incidence of Parkinson’s Disease and Parkinsonism in Northern Sweden: A Population-Based Study. Mov. Disord. 2010, 25, 341–348. [Google Scholar] [CrossRef] [PubMed]
- Alves, G.; Müller, B.; Herlofson, K.; Hogenesch, I.; Telstad, W.; Aarsland, D.; Tysnes, O.B.; Larsen, J.P. Incidence of Parkinson’s Disease in Norway: The Norwegian Parkwest Study. J. Neurol. Neurosurg. Psychiatry 2009, 80, 851. [Google Scholar] [CrossRef] [PubMed]
- Fahn, S. Description of Parkinson’s Disease as a Clinical Syndrome. Ann. N. Y. Acad. Sci. 2003, 991, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Schrag, A.; Marjan, J.; Niall, Q. What Contributes to Quality of Life in Patients with Parkinson’s Disease? J. Neurol. Neurosurg. Psychiatry 2000, 69, 289. [Google Scholar] [CrossRef]
- Skorvanek, M.; Martinez-Martin, P.; Kovacs, N.; Zezula, I.; Rodriguez-Violante, M.; Corvol, J.C.; Taba, P.; Seppi, K.; Levin, O.; Schrag, A.E. Relationship between the Mds-Updrs and Quality of Life in Parkinson’s Disease. J. Neurol. Sci. 2015, 353, 87–91. [Google Scholar] [CrossRef] [PubMed]
- Chaudhuri, K.R.; Healy, D.G.; Schapira, A.H. Non-Motor Symptoms of Parkinson’s Disease: Diagnosis and Management. Lancet Neurol. 2017, 5, 235–245. [Google Scholar] [CrossRef]
- Martinez-Martin, P. What is quality of life and how do we measure it? Relevance to Parkinson’s disease and movement disorders. Mov. Disord. 2017, 32, 382–392. [Google Scholar] [CrossRef] [PubMed]
- Brazier, J.; Ratcliffe, J.; Saloman, J.; Tsuchiya, A. Measuring and Valuing Health Benefits for Economic Evaluation. Available online: http://dx.doi.org/10.1093/med/9780198725923.001.0001 (accessed on 10 November 2016).
- Brooks, R. A new facility for the measurement of health-related quality of life. Health Policy 1990, 3, 199–208. [Google Scholar]
- OFcom. Facts and Figures. Available online: http://media.ofcom.org.uk/facts/ (accessed on 3 July 2015).
- Druce, K.L.; McBeth, J.; van der Veer, S.N.; Selby, D.A.; Vidgen, B.; Georgatzis, K.; Hellman, B.; Lakshminarayana, R.; Chowdhury, A.; Schultz, D.M.; et al. Recruitment and Ongoing Engagement in a UK Smartphone Study Examining the Association Between Weather and Pain: Cohort Study. JMIR Mhealth Uhealth 2017, 5, e168. [Google Scholar] [CrossRef] [PubMed]
- Respiratory Institute. Asthma Mobile Health Study. Available online: http://apps.icahn.mssm.edu/asthma/ (accessed on 15 September 2015).
- University of Rochester Medical Center. Apple Highlights Parkinson’s App with URMC Ties. Available online: https://www.urmc.rochester.edu/news/story/4268/apple-highlights-parkinsons-app-with-urmc-ties.aspx (accessed on 9 March 2015).
- Stanford Medicine. My-heart Counts iPhone Application. Available online: https://med.stanford.edu/myheartcounts.html (accessed on 15 September 2015).
- Mulhern, B.; O’Gorman, H.; Rotherham, N.; Brazier, J. Comparing the measurement equivalence of EQ-5D-5L across different modes of administration. Health Qual. Life Outcomes 2014, 17, 191. [Google Scholar] [CrossRef] [PubMed]
- Bot, B.M.; Suver, C.; Neto, E.C.; Kellen, M.; Klein, A.; Bare, C.; Doerr, M.; Pratap, A.; Wilbanks, J.; Dorsey, E.R.; et al. The mPower study, Parkinson disease mobile data collected using ResearchKit. Sci. Data 2016, 3, 160011. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. BMJ 2017, 335, 806–808. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.F.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and Preliminary Testing of the New Five-Level Version of Eq-5d (Eq-5d-5l). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Van Hout, B.; Janssen, M.F.; Feng, Y.S.; Kohlmann, T.; Busschbach, J.; Golicki, D.; Lloyd, A.; Scalone, L.; Kind, P.; Pickard, A.S. Interim Scoring for the Eq-5d-5l: Mapping the Eq-5d-5l to Eq-5d-3l Value Sets. Value Health 2012, 15, 708–715. [Google Scholar] [CrossRef] [PubMed]
- McCaffrey, N.; Kaambwa, B.; Currow, D.C.; Ratcliffe, J. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual. Life Outcomes 2016, 14, 133. [Google Scholar] [CrossRef] [PubMed]
- Jecmenica-Lukic, M.V.; Pekmezovic, T.D.; Petrovic, I.N.; Dragasevic, N.T.; Kostić, V.S. Factors associated with deterioration of health-related quality of life in multiple system atrophy: 1-year follow-up study. Acta Neurol. Belg. 2018, 11, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Clayton, T.; A Bakhai, A. Interaction Clinical Trials: A Practical Guide to Design, Analysis and Reporting; Wang, D., Bakhai, A., Eds.; Remedica: Chicago, IL, USA, 2006; pp. 305–316, ISBN-10 1901346722, ISBN-13 9781901346722. [Google Scholar]
- EQ-5D. EQ-5D-5L|About. Available online: https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ (accessed on 18 April 2017).
- Parkin, D.; Rice, N.; Devlin, N. Statistical analysis of EQ-5D profiles: Does the use of value sets bias inference? Med. Decis. Mak. 2010, 5, 556. [Google Scholar] [CrossRef] [PubMed]
- Golicki, D.; Niewada, M.; Buczek, J.; Karlinska, A.; Kobayashi, A.; Janssen, M.F.; Pickard, A.S. Validity of EQ-5D-5L in stroke. Qual. Life Res. 2015, 4, 845–850. [Google Scholar] [CrossRef] [PubMed]
- Garciagordillo, M.A.; Colladomateo, D.; Olivares, P.R.; Adsuar, J.C. Application of Eq-5d-5l Questionnaire in Patients Suffering from Urinary Incontinence. Actas Urol. Esp. 2016, 7, 457–462. [Google Scholar]
- Hinz, A.; Kohlmann, T.; Stöbel-Richter, Y.; Zenger, M.; Brähler, E. The quality of life questionnaire EQ-5D-5L: Psychometric properties and normative values for the general German population. Qual. Life Res. 2014, 2, 443–447. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, L.H.; Tran, B.X.; Hoang, L.Q.N.; Tran, T.T.; Latkin, C.A. Quality of life profile of general Vietnamese population using EQ-5D-5L. Health Qual. Life Outcomes 2017, 15, 199. [Google Scholar] [CrossRef] [PubMed]
- Szende, A.; Janssen, B.; Cabases, J. Population Norms for the EQ-5D. In Self-Reported Population Health: An International Perspective Based on EQ-5D; Szende, A., Janssen, B., Cabases, J., Eds.; Springer: Dordrecht, The Netherlands, 2014; p. 21. ISBN 978-94-007-7595-1. [Google Scholar]
- Lees, A.J.; Hardy, J.; Revesz, T. Parkinson’s disease. Lancet 2009, 373, 2055–2066. [Google Scholar] [CrossRef]
- Pimenta, M.; Moreira, D.; Nogueira, T.; Silva, C.; Pinto, E.B.; Valenca, G.T.; Almeida, L.R.S. Anxiety Independently Contributes to Severity of Freezing of Gait in People with Parkinson’s Disease. J. Neuropsychiatry Clin. Neurosci. 2018, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Dissanayaka, N.N.; Sellbach, A.; Silburn, P.A.; O’Sullivan, J.D.; Marsh, R.; Mellick, G.D. Factors associated with depression in Parkinson’s disease. J. Affect Disord. 2011, 132, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Sophie, M.; Ford, B. Management of pain in Parkinson’s disease. CNS Drugs 2012, 11, 937. [Google Scholar] [CrossRef] [PubMed]
- Ford, B. Pain in Parkinson’s disease. Mov. Disord. 2010, S1, S98–S103. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.; Devlin, N.; Herdman, M. Assessing the health of the general population in England: How do the three- and five-level versions of EQ-5D compare? Health Qual. Life Outcomes 2015, 13, 171. [Google Scholar] [CrossRef] [PubMed]
- Golicki, D.; Niewada, M. EQ-5D-5L Polish population norms. Arch. Med. Sci. 2017, 1, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Collado, M.D.; García, G.M.A.; Olivares, P.R.; Adsuar, J.C. Normative Values of Eq-5d-5l for Diabetes Patients from Spain. Nutr. Hosp. 2015, 32, 1595–1602. [Google Scholar]
| Variables | Parkinson’s | Non-Parkinson’s | χ2 | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Gender | 61.61 | <0.001 | ||||
| Female | 483 | 47.73 | 434 | 67.60 | ||
| Male | 529 | 52.27 | 208 | 32.40 | ||
| Education | 3.27 | 0.195 | ||||
| Up to 16 years old | 166 | 16.40 | 87 | 13.55 | ||
| Up to 18 years old | 109 | 10.77 | 64 | 9.97 | ||
| University/College/Equivalent | 737 | 72.83 | 491 | 76.48 | ||
| Do you smoke tobacco? | 1.36 | 0.714 | ||||
| No, never | 638 | 63.04 | 392 | 61.06 | ||
| No, but used to | 330 | 32.61 | 218 | 33.96 | ||
| Yes, occasionally/weekly | 21 | 2.08 | 13 | 2.02 | ||
| Yes, daily | 23 | 2.27 | 19 | 2.96 | ||
| How often do you have a drink containing alcohol? | 1.36 | 0.714 | ||||
| No, never | 155 | 15.32 | 65 | 10.12 | ||
| Monthly or less | 185 | 18.28 | 101 | 15.73 | ||
| 2–4 times per month | 197 | 19.47 | 136 | 21.18 | ||
| 2–3 times per week | 248 | 24.50 | 184 | 28.66 | ||
| 4 or more times per week | 227 | 22.43 | 156 | 24.31 | ||
| Do you have other long-term health conditions? | 3.35 | 0.067 | ||||
| No | 578 | 57.11 | 335 | 52.18 | ||
| Yes | 434 | 42.89 | 307 | 47.82 | ||
| Do you live alone? | 0.68 | 0.411 | ||||
| No | 876 | 86.56 | 547 | 85.20 | ||
| Yes | 136 | 13.44 | 95 | 14.80 | ||
| Variables | Parkinson’s | Non-Parkinson’s | χ2 | p | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| Mobility | 244.51 | <0.001 | ||||
| Level 1 | 374 | 35.62 | 489 | 74.09 | ||
| Level 2 | 424 | 40.38 | 120 | 18.18 | ||
| Level 3 | 190 | 18.10 | 32 | 4.85 | ||
| Level 4 | 56 | 5.33 | 18 | 2.73 | ||
| Level 5 | 6 | 0.57 | 1 | 0.15 | ||
| Self-care | 245.69 | <0.001 | ||||
| Level 1 | 597 | 56.86 | 607 | 91.97 | ||
| Level 2 | 347 | 33.05 | 35 | 5.31 | ||
| Level 3 | 87 | 8.29 | 9 | 1.36 | ||
| Level 4 | 17 | 1.62 | 8 | 1.21 | ||
| Level 5 | 2 | 0.18 | 1 | 0.15 | ||
| Usual Activity | 305.39 | <0.001 | ||||
| Level 1 | 323 | 30.75 | 487 | 73.79 | ||
| Level 2 | 465 | 44.29 | 124 | 18.79 | ||
| Level 3 | 202 | 19.24 | 32 | 4.85 | ||
| Level 4 | 47 | 4.48 | 12 | 1.82 | ||
| Level 5 | 13 | 1.24 | 5 | 0.7 | ||
| Pain/Discomfort | 86.51 | <0.001 | ||||
| Level 1 | 264 | 25.14 | 274 | 41.52 | ||
| Level 2 | 458 | 43.62 | 296 | 44.85 | ||
| Level 3 | 264 | 25.14 | 69 | 10.45 | ||
| Level 4 | 57 | 5.43 | 19 | 2.88 | ||
| Level 5 | 7 | 0.67 | 2 | 0.30 | ||
| Anxiety/Depression | 17.37 | 0.002 | ||||
| Level 1 | 531 | 50.57 | 390 | 59.09 | ||
| Level 2 | 366 | 34.85 | 205 | 31.06 | ||
| Level 3 | 127 | 12.10 | 59 | 8.94 | ||
| Level 4 | 23 | 2.19 | 4 | 0.61 | ||
| Level 5 | 3 | 0.29 | 2 | 0.30 | ||
| Summary | EQ-5D-5L | p | EQ-VAS | p | ||
|---|---|---|---|---|---|---|
| At Baseline | At End of Study | At Baseline | At End of Study | |||
| Parkinson’s | 0.042 | 0.855 | ||||
| Mean | 0.70 | 0.66 | 73.40 | 72.13 | ||
| SD | 0.19 | 0.22 | 17.87 | 18.62 | ||
| Median | 0.73 | 0.70 | 78.00 | 76.00 | ||
| Q1 | 0.62 | 0.58 | 62.00 | 65.00 | ||
| Q3 | 0.84 | 0.78 | 86.00 | 85.00 | ||
| Non-Parkinson’s | 0.346 | 0.960 | ||||
| Mean | 0.83 | 0.82 | 82.66 | 83.58 | ||
| SD | 0.16 | 0.19 | 14.66 | 12.26 | ||
| Median | 0.84 | 0.84 | 86.00 | 86.00 | ||
| Q1 | 0.75 | 0.74 | 79.00 | 77.00 | ||
| Q3 | 1.00 | 1.00 | 92.50 | 93.00 | ||
| EQ-5D | Model 1 | Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| Mean Difference | 95%CI | p | Mean Difference | 95%CI | p | |||
| Lower | Upper | Lower | Upper | |||||
| EQ-5D-5L values (Non-Parkinson’s vs. Parkinson’s) | ||||||||
| Baseline | 0.13 | 0.10 | 0.17 | <0.001 | 0.15 | 0.12 | 0.18 | <0.001 |
| End of study | 0.16 | 0.12 | 0.18 | <0.001 | 0.17 | 0.14 | 0.20 | <0.001 |
| EQ VAS scores (Non-Parkinson’s vs. Parkinson’s) | ||||||||
| Baseline | 9.25 | 6.56 | 11.95 | <0.001 | 10.18 | 7.40 | 12.96 | <0.001 |
| End of study | 11.45 | 8.76 | 14.14 | <0.001 | 12.19 | 9.41 | 14.97 | <0.001 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, X.; Wang, D.; Hellman, B.; Janssen, M.F.; Bakker, G.; Coghlan, R.; Hursey, A.; Matthews, H.; Whetstone, I. Assessment of Health-Related Quality of Life between People with Parkinson’s Disease and Non-Parkinson’s: Using Data Drawn from the ‘100 for Parkinson’s’ Smartphone-Based Prospective Study. Int. J. Environ. Res. Public Health 2018, 15, 2538. https://doi.org/10.3390/ijerph15112538
Fan X, Wang D, Hellman B, Janssen MF, Bakker G, Coghlan R, Hursey A, Matthews H, Whetstone I. Assessment of Health-Related Quality of Life between People with Parkinson’s Disease and Non-Parkinson’s: Using Data Drawn from the ‘100 for Parkinson’s’ Smartphone-Based Prospective Study. International Journal of Environmental Research and Public Health. 2018; 15(11):2538. https://doi.org/10.3390/ijerph15112538
Chicago/Turabian StyleFan, Xiaojing, Duolao Wang, Bruce Hellman, Mathieu F. Janssen, Gerben Bakker, Rupert Coghlan, Amelia Hursey, Helen Matthews, and Ian Whetstone. 2018. "Assessment of Health-Related Quality of Life between People with Parkinson’s Disease and Non-Parkinson’s: Using Data Drawn from the ‘100 for Parkinson’s’ Smartphone-Based Prospective Study" International Journal of Environmental Research and Public Health 15, no. 11: 2538. https://doi.org/10.3390/ijerph15112538
APA StyleFan, X., Wang, D., Hellman, B., Janssen, M. F., Bakker, G., Coghlan, R., Hursey, A., Matthews, H., & Whetstone, I. (2018). Assessment of Health-Related Quality of Life between People with Parkinson’s Disease and Non-Parkinson’s: Using Data Drawn from the ‘100 for Parkinson’s’ Smartphone-Based Prospective Study. International Journal of Environmental Research and Public Health, 15(11), 2538. https://doi.org/10.3390/ijerph15112538





