Electronic Cigarettes and Smoking Cessation in the Perioperative Period of Cardiothoracic Surgery: Views of Australian Clinicians
Abstract
:1. Introduction
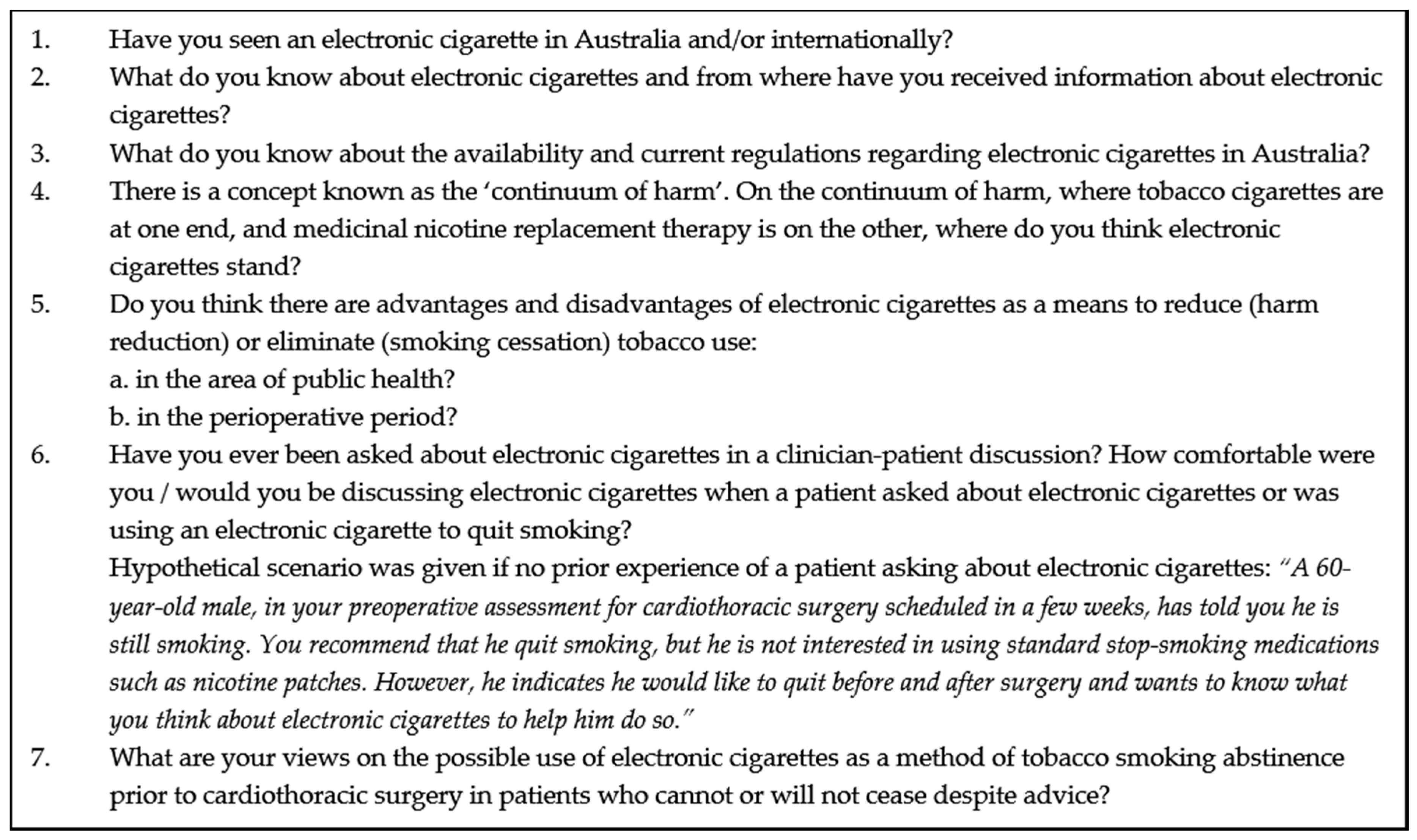
2. Methods
2.1. Design and Data Collection
2.2. Data Analysis
3. Results
3.1. Electronic Cigarettes Were Unlikely to Be Safe but Still Safer than Tobacco Cigarettes
“What have I picked up? From a medical point of view? Nowhere. This is from a media point of view—it’s a nicotine replacement, so it deals with cravings.” (S12)
“It’s going to take years to get a handle on whether they are better or worse. Maybe it will cause other things we don’t even know about.” (S1)
“You can get NRT on a prescription, and over the counter. That could work for electronic cigarettes too.” (A6)
3.2. Electronic Cigarettes May Have a Harm Reduction Role in the Context of Public Health
“Electronic cigarettes are nicotine and flavour. Even if the flavour is poisonous, it’s probably better than 3000 other chemicals in a tobacco cigarette.” (A5)
“Electronic cigarettes still promote the oral component, so it would be too easy to slip back to smoking. And their use suggests that it’s still socially acceptable to put them in your mouth, renormalising smoking again.” (S11)
“I think people want to stop smoking. There’s those who can do it cold turkey or with nicotine replacement, but some need the hand-to-mouth kind of behaviour to continue. Whichever gets them off the cigarette.” (S6)
3.3. Electronic Cigarettes Were a Potential Smoking Cessation Tool for the Extraordinary Circumstances of Surgery
“I see so many patients who they stop from 60 a day to nil just by not relenting. That’s probably part of the reason, maybe the motivation and the mental attitude to that. So, if they want to do it, they can do it without the electronic cigarette.” (S15)
“I have concerns about the flavours, because you don’t know what’s in it. They’re inhaling a whole cocktail of things before the anaesthetic.” (A4)
“If using electronic cigarettes was a way of getting higher concentrations of nicotine as a single hit, which some people seem to need, that would be worthwhile, because other means of nicotine therapy are delivered too slow, compared to tobacco cigarettes.” (A12)
“I think there are patients who are so habituated to smoking that if electronic cigarette use is the only way they can stop, I accept that.” (S10)
3.4. Patient-Clinician Discussions Were Influenced by Clinician Views about Electronic Cigarettes and Clinicians’ Professional Role
“I would tell the patient that it’s good that they’re showing steps to try and stop smoking, but they would need to talk to their surgeon about electronic cigarettes. They’re not harmless.” (P5)
“I would talk to the surgeons and ask what their opinion was. I would have to get more information because I wouldn’t want to recommend something that I know nothing about.” (N9)
“You have to use whatever means are appropriate to protect the patient from themselves and to optimise their surgical outcome in the short term and their life outcome in the long term.” (S14)
“I would be comfortable recommending an electronic cigarette because I think it achieves the outcome that we want for the patient.” (A14)
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Warner, D.O. Perioperative abstinence from cigarettes—Physiologic and clinical consequences. Anesthesiology 2006, 104, 356–367. [Google Scholar] [CrossRef] [PubMed]
- Parsons, A.; Daley, A.; Begh, R.; Aveyard, P. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: Systematic review of observational studies with meta-analysis. BMJ 2010, 340. [Google Scholar] [CrossRef] [PubMed]
- Rigotti, N.A.; Clair, C. Managing tobacco use: The neglected cardiovascular disease risk factor. Eur. Heart J. 2013, 34, 3259–3267. [Google Scholar] [CrossRef] [PubMed]
- Fiore, M.C.; Bailey, W.C.; Cohen, S.J. Treating Tobacco Use and Dependence. Clinical Practice Guideline; 2008. Available online: https://www.ncbi.nlm.nih.gov/books/NBK63952/ (accessed on 5 October 2018).
- Royal Australian College of General Practitioners. Supporting Smoking Cessation: A Guide for Health Professionals. 2014. Available online: https://www.racgp.org.au/your-practice/guidelines/smoking-cessation/ (accessed on 5 October 2018).
- National Institute for Health and Care Excellence. Smoking: Acute, Maternity and Mental Health Services (PH48). 2013. Available online: https://www.nice.org.uk/guidance/ph48 (accessed on 5 October 2018).
- Nolan, M.B.; Warner, D.O. Perioperative tobacco use treatments: putting them into practice. BMJ 2017, 358. [Google Scholar] [CrossRef] [PubMed]
- Luxton, N.A.; MacKenzie, R.; Shih, P. Smoking cessation care in cardiothoracic surgery: A qualitative study exploring the views of Australian clinicians. Heart Lung Circ. 2018, S1443–9506. [Google Scholar] [CrossRef] [PubMed]
- Borderud, S.P.; Li, Y.; Burkhalter, J.E.; Sheffer, C.E.; Ostroff, J.S. Electronic cigarette use among patients with cancer: Characteristics of electronic cigarette users and their smoking cessation outcomes. Cancer 2014, 120, 3527–3535. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Busch, A.M.; Leavens, E.L.; Wagener, T.L.; Buckley, M.L.; Tooley, E.M. Prevalence, reasons for use, and risk perception of electronic cigarettes among post-acute coronary syndrome smokers. J. Cardiopulm. Rehabil. Prev. 2016, 36, 352–357. [Google Scholar] [CrossRef] [PubMed]
- Kalkhoran, S.; Kruse, G.R.; Rigotti, N.A.; Rabin, J.; Ostroff, J.S.; Park, E.R. Electronic cigarette use patterns and reasons for use among smokers recently diagnosed with cancer. Cancer Med. 2018. [Google Scholar] [CrossRef] [PubMed]
- Moysidou, A.; Farsalinos, K.; Voudris, V.; Merakou, K.; Kourea, K.; Barbouni, A. Knowledge and perceptions about nicotine, nicotine replacement therapies and electronic cigarettes among healthcare professionals in Greece. Int. J. Environ. Res. Public Health 2016, 13, 514. [Google Scholar] [CrossRef] [PubMed]
- Sherratt, F.C.; Newson, L.; Field, J.K. Electronic cigarettes: A survey of perceived patient use and attitudes among members of the British thoracic oncology group. Respir. Res. 2016, 55. [Google Scholar] [CrossRef] [PubMed]
- Kanchustambham, V.; Saladi, S.; Rodrigues, J.; Fernandes, H.; Patolia, S.; Santosh, S. The knowledge, concerns and healthcare practices among physicians regarding electronic cigarettes. J. Community Hosp. Inter. Med. Perspect 2017, 7, 144–150. [Google Scholar] [CrossRef] [PubMed]
- Nickels, A.S.; Warner, D.O.; Jenkins, S.M.; Tilburt, J.; Hays, J.T. Beliefs, practices, and self-efficacy of US physicians regarding smoking cessation and electronic cigarettes: A national survey. Nicotine Tob. Res. 2017, 19, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Kim, Y.I.; Kim, S.J.; Kim, J.S.; Chong, S.; Park, Y.S.; Song, S.-Y.; Lee, J.H.; Ahn, H.K.; Kim, E.Y.; et al. Lung cancer specialist physicians’ attitudes towards e-cigarettes: A nationwide survey. PLoS ONE 2017, 12, e0172568. [Google Scholar] [CrossRef] [PubMed]
- Singh, B.; Hrywna, M.; Wackowski, O.A.; Delnevo, C.D.; Jane Lewis, M.; Steinberg, M.B. Knowledge, recommendation, and beliefs of e-cigarettes among physicians involved in tobacco cessation: A qualitative study. Prev. Med. Rep. 2017, 8, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Baldassarri, S.R.; Chupp, G.L.; Leone, F.T.; Warren, G.W.; Toll, B.A. Practise patterns and perceptions of chest health care providers on electronic cigarette use: An in-depth discussion and report of survey results. J. Smok. Cess. 2018, 13, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Glasser, A.M.; Collins, L.; Pearson, J.L.; Abudayyeh, H.; Niaura, R.S.; Abrams, D.B.; Villanti, A.C. Overview of electronic nicotine delivery systems: A systematic review. Am. J. Prev. Med. 2017, 52, e33–e66. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Electronic Nicotine Delivery Systems and Electronic Non-Nicotine Delivery Systems (ENDS/ENNDS). 2017. Available online: http://www.who.int/tobacco/communications/statements/eletronic-cigarettes-january-2017/en/ (accessed on 5 October 2018).
- Chapman, S.; Bareham, D.; Maziak, W. The gateway effect of e-cigarettes; Reflections on main criticisms. Nicotine. Tob. Res. 2018. [Google Scholar] [CrossRef] [PubMed]
- Glantz, S.A.; Bareham, D.W. E-Cigarettes: Use, effects on smoking, risks, and policy implications. Annu. Rev. Public Health 2018, 39, 215–235. [Google Scholar] [CrossRef] [PubMed]
- National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on the Review of the Health Effects of Electronic Nicotine Delivery Systems. Public Health Consequences of E-Cigarettes; Eaton, D.L., Kwan, L.Y., Stratton, K., Eds.; National Academies Press: Washington, DC, USA, 2018. [Google Scholar]
- Rahman, M.A.; Hann, N.; Wilson, A.; Mnatzaganian, G.; Worrall-Carter, L. E-cigarettes and smoking cessation: evidence from a systematic review and meta-analysis. PLoS ONE 2015, 10, e0122544. [Google Scholar] [CrossRef] [PubMed]
- Hartmann-Boyce, J.; Begh, R.; Aveyard, P. Electronic cigarettes for smoking cessation. BMJ 2018, 360. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence. Stop Smoking Interventions and Services NICE Guideline (NG92). 2018. Available online: https://www.nice.org.uk/guidance/ng92 (accessed on 5 October 2018).
- Adkison, S.E.; O’Connor, R.J.; Bansal-Travers, M.; Hyland, A.; Borland, R.; Yong, H.H.; Cummings, K.M.; McNeill, A.; Thrasher, J.F.; Hammond, D.; et al. Electronic nicotine delivery systems: International tobacco control four-country survey. Am. J. Prev. Med. 2013, 44, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Yong, H.H.; Borland, R.; Balmford, J.; McNeill, A.; Hitchman, S.; Driezen, P.; Thompson, M.E.; Fong, G.T.; Cummings, K.M. Trends in e-cigarette awareness, trial, and use under the different regulatory environments of Australia and the United Kingdom. Nicotine Tob. Res. 2015, 17, 1203–1211. [Google Scholar] [CrossRef] [PubMed]
- Australian Institute of Health and Welfare. National Drug Strategy Household Survey 2016: Detailed Findings. Available online: https://www.aihw.gov.au/getmedia/15db8c15-7062-4cde-bfa4-3c2079f30af3/21028a.pdf.aspx?inline=true (accessed on 5 October 2018).
- NSW Smoking & Health Survey 2015, Cancer Institute NSW, Sydney, 2017. Available online: https://www.cancer.nsw.gov.au/how-we-help/reports-and-publications/nsw-smoking-and-health-survey-2015 (accessed on 5 October 2018).
- Ministry of Health, New Zealand. Regulation of E-Cigarettes and Emerging Tobacco and Nicotine-Delivery Products. 2017. Available online: https://www.health.govt.nz/about-ministry/legislation-and-regulation/regulatory-impact-statements/regulation-e-cigarettes-and-emerging-tobacco-and-nicotine-delivery-products (accessed on 5 October 2018).
- Therapeutic Goods Administration. Electronic Cigarettes. Available online: https://www.tga.gov.au/community-qa/electronic-cigarettes (accessed on 5 October 2018).
- The Department of Health. E-Cigarettes. Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/mc16-031907-reduce-the-harm-from-tobacco (accessed on 5 October 2018).
- Parliament of Australia. Submission from Cancer Council Australia and the National Heart Foundation of Australia to Standing Committee on Health, Aged Care and Sport Inquiry into the Use and Marketing of Electronic Cigarettes and Personal Vaporisers in Australia. 2017. Available online: https://www.cancer.org.au/content/pdf/CancerControlPolicy/Submissions/Inquiry_into_e-cigarettes.pdf (accessed on 5 October 2018).
- Parliament of Australia. Royal Australasian College of Surgeons. Inquiry into the use and marketing of electronic cigarettes and personal vaporisers in Australia, Submission 329, 2017. Available online: https://www.aph.gov.au/Parliamentary_Business/Committees/House/Health_Aged_Care_and_Sport/ElectronicCigarettes/Submissions?main_0_content_1_RadGrid1ChangePage=15_20 (accessed on 5 October 2018).
- The Department of Health. Statement on E-Cigarettes in Australia. Available online: https://canceraustralia.gov.au/sites/default/files/statement_on_e-cigarettes_february_2018_0.pdf (accessed on 5 October 2018).
- Royal College of Physicians. Policy on E-Cigarettes. 2018. Available online: https://www.racp.edu.au/docs/default-source/advocacy-library/policy-on-electronic-cigarettes.pdf (accessed on 5 October 2018).
- Kadimpati, S.; Nolan, M.; Warner, D.O. Attitudes, beliefs, and practices regarding electronic nicotine delivery systems in patients scheduled for elective surgery. Mayo Clin. Proc. 2015, 90, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Nolan, M.; Leischow, S.; Croghan, I.; Kadimpati, S.; Hanson, A.; Schroeder, D.; Warner, D.O. Feasibility of Electronic Nicotine Delivery Systems in Surgical Patients. Nicotine Tob. Res. 2016, 18, 1757–1762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, S.M.; Tenney, R.; Wallace, A.W.; Arjomandi, M. E-cigarettes versus nicotine patches for perioperative smoking cessation: a pilot randomized trial. PeerJ 2018. [Google Scholar] [CrossRef] [PubMed]
- An, L.C.; Foldes, S.S.; Alesci, N.L.; Bluhm, J.H.; Bland, P.C.; Davern, M.E.; Schillo, B.A.; Ahluwalia, J.S.; Manley, M.W. The impact of smoking-cessation intervention by multiple health professionals. Am. J. Prev. Med. 2008, 34, 54–60. [Google Scholar] [CrossRef] [PubMed]
- Prestwich, A.; Moore, S.; Kotze, A.; Budworth, L.; Lawton, R.; Kellar, I. How can smoking cessation be induced before surgery? A systematic review and meta-analysis of behavior change techniques and other intervention characteristics. Front. Psychol. 2017, 8. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Health Information. Healthcare Quarterly, Activity and Performance—Emergency Department, Ambulance, Admitted Patients and Elective Surgery. 2016. Available online: http://search.bhi.nsw.gov.au/s/search.html?query=cardiothoracic+surgery+2016&x=0&y=0&collection=nsw_health_bhi (accessed on 5 October 2018).
- NSW Health. Managing Nicotine Dependence: A Guide for NSW Health Staff. 2015. Available online: https://www.health.nsw.gov.au/tobacco/Pages/tools-for-health-professionals.aspx (accessed on 5 October 2018).
- National Statement on Ethical Conduct in Human Research. (Updated 2018). The National Health and Medical Research Council, the Australian Research Council and Universities Australia; Commonwealth of Australia, Canberra, 2007. Available online: https://nhmrc.gov.au/about-us/publications/national-statement-ethical-conduct-human-research-2007-updated-2018#block-views-block-file-attachments-content-block-1 (accessed on 5 October 2018).
- NVivo Qualitative Data Analysis Software (Version 11); QSR International Pty Ltd.: Melbourne, Australia, 2010.
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef] [Green Version]
- Guest, G.; MacQueen, K.; Namey, E. Applied Thematic Analysis; Sage Publications: London, UK, 2012. [Google Scholar]
- Green, J.; Thorogood, N. Qualitative Methods for Health Research; Sage Publications: London, UK, 2018. [Google Scholar]
- Australian Institute of Health and Welfare. Australia’s Health 2018; Australia’s Health Series No. 16; AUS 221; AIHW: Canberra, Australia, 2018. Available online: https://www.aihw.gov.au/reports/australias-health/australias-health-2018/contents/table-of-contents (accessed on 5 October 2018).
- Stead, L.F.; Buitrago, D.; Preciado, N.; Sanchez, G.; Hartmann-Boyce, J.; Lancaster, T. Physician advice for smoking cessation. Cochrane Database Syst. Rev. 2013. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Medical Board of Australia. Doctors the Most Trusted Profession: Board Research. 2016. Available online: https://www.medicalboard.gov.au/news/2016-11-10-media-statement.aspx (accessed on 5 October 2018).
- Rice, V.H.; Heath, L.; Livingstone-Banks, J.; Hartmann-Boyce, J. Nursing interventions for smoking cessation. Cochrane Database Syst. Rev. 2017, 12. [Google Scholar] [CrossRef] [PubMed]
- Brennan, N.; Barnes, R.; Calnan, M.; Corrigan, O.; Dieppe, P.; Entwistle, V. Trust in the health-care provider–patient relationship: A systematic mapping review of the evidence base. Int. J. Qual. Health Care 2013, 25, 682–688. [Google Scholar] [CrossRef] [PubMed]
- Warner, D.O.; LeBlanc, A.; Kadimpati, S.; Vickers, K.S.; Shi, Y.; Montori, V.M. Decision aid for cigarette smokers scheduled for elective surgery. Anesthesiology 2015, 123, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Warner, D.O. Helping surgical patients quit smoking: Why, when, and how. Anesth. Analg. 2005, 101, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Wolfenden, L.; Wiggers, J.; Knight, J.; Campbell, E. Smoking and surgery: An opportunity for health improvement. Aust. N. Z. J. Public Health 2007, 31, 386–387. [Google Scholar] [CrossRef] [PubMed]
- Wolfenden, L.; Campbell, E.; Wiggers, J.; Walsh, R.A.; Bailey, L.J. Helping hospital patients quit: What the evidence supports and what guidelines recommend. Prev. Med. 2008, 46, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Yong, H.H.; Borland, R.; Balmford, J.; Hitchman, S.C.; Cummings, K.M.; Driezen, P.; Thompson, M.E. Prevalence and correlates of the belief that electronic cigarettes are a lot less harmful than conventional cigarettes under the different regulatory environments of Australia and the United Kingdom. Nicotine Tob. Res. 2017, 19, 258–263. [Google Scholar] [CrossRef] [PubMed]
- Rojewski, A.M.; Baldassarri, S.; Cooperman, N.A.; Gritz, E.R.; Leone, F.T.; Piper, M.E.; Toll, B.A.; Warren, G.W. Exploring issues of comorbid conditions in people who smoke. Nicotine Tob. Res. 2016, 18, 1684–1696. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.; Abramson, M.J.; Bonevski, B.; Taylor, S.; Poole, S.G.; Weeks, G.R.; Dooley, M.J.; George, J. Quitting experiences and preferences for a future quit attempt: A study among inpatient smokers. BMJ Open 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Bureau of Health Information. Healthcare Quarterly, Activity and Performance—Emergency Department, Ambulance, Admitted Patients and Elective Surgery. 2016. Available online: http://www.bhi.nsw.gov.au/BHI_reports/healthcare_quarterly (accessed on 5 October 2018).
- Parliament of Australia. Inquiry into the Use and Marketing of Electronic Cigarettes and Personal Vaporisers in Australia. 2018. Available online: https://www.aph.gov.au/Parliamentary_Business/Committees/House/Health_Aged_Care_and_Sport/ElectronicCigarettes/Report (accessed on 5 October 2018).
| Characteristic | Surgeons | Anaesthetists | Nurses | Physiotherapists |
|---|---|---|---|---|
| Gender (male), n (%) | 15 (100%) | 13 (87%) | 1 (9%) | 1 (9%) |
| Age (year), n (%) | ||||
| <40 | 5 (45%) | |||
| >40 | 15 (100%) | 15 (100%) | 11 (100%) | 6 (55%) |
| Current work setting, n (%) | ||||
| Public hospital | 15 (100%) | 15 (100%) | 8 (73%) | 5 (45%) |
| Self-reported time working in cardiothoracic surgical area (year), n (%) | ||||
| <10 | 2 (13%) | 11 (73%) | 4 (36%) | 7 (64%) |
| >10 | 13 (87%) | 4 (27%) | 7 (64%) | 4 (36%) |
| Theme | Sub Theme | Categories | Professions and Frequency | |||
|---|---|---|---|---|---|---|
| Anaesthetists (n = 15) | Surgeons (n = 15) | Nurses (n = 11) | Physiotherapists (n = 11) | |||
| Electronic cigarettes were unlikely to be safe but still safer than tobacco cigarettes | Limited knowledge of electronic cigarettes | Media was the main source of information | 15 | 15 | 11 | 11 |
| Electronic cigarettes should be banned or regulated until further evidence available | 2 | 5 | 3 | 0 | ||
| Unsure of how electronic cigarettes should be regulated due to lack of evidence | 10 | 9 | 8 | 11 | ||
| Electronic cigarettes should be available over-the-counter/tobacconist | 2 | 1 | 0 | 0 | ||
| Electronic cigarettes may have a harm reduction role in the context of public health | Positive views of electronic cigarettes | Electronic cigarettes as the lesser of two evils | 8 | 7 | 4 | 6 |
| Hand to mouth similarities as an alternative form of nicotine replacement therapy (NRT) | 4 | 5 | 2 | 2 | ||
| Negative views of electronic cigarettes | Electronic cigarettes were too similar to tobacco cigarettes | 3 | 3 | 5 | 3 | |
| Electronic cigarettes were a potential smoking cessation tool for the extraordinary circumstances of surgery | Electronic cigarettes as an alternative to tobacco smoking | If patients had tried other methods and were unable to quit | 5 | 4 | 3 | 4 |
| As a bridge off tobacco smoking before surgery | 4 | 6 | 2 | 2 | ||
| Clinicians’ preferred methods outweighed potential role of electronic cigarettes | Preference for evidence-based methods of NRT | 2 | 2 | 5 | 1 | |
| No nicotine in any form allowed for their patients prior to surgery | 1 | 2 | 1 | 0 | ||
| Unknown effects of vaping on patients’ airways | 3 | 1 | 0 | 4 | ||
| Patient-clinician discussions were influenced by clinician views about electronic cigarettes and clinicians’ professional role | Consider patient short-term use of electronic cigarettes before surgery | Comfortable with discussing electronic cigarette short-term patient use to help stop tobacco smoking prior to surgery | 8 | 7 | 1 | 2 |
| Discourage patient use of electronic cigarettes | Comfortable with discussing the lack of evidence being their reason for not recommending electronic cigarettes | 1 | 4 | 2 | 1 | |
| Unsure and would seek advice | Emphasis on patient’s choice to use electronic cigarettes due to lack of own knowledge | 6 | 4 | 8 | 8 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luxton, N.A.; Shih, P.; Rahman, M.A. Electronic Cigarettes and Smoking Cessation in the Perioperative Period of Cardiothoracic Surgery: Views of Australian Clinicians. Int. J. Environ. Res. Public Health 2018, 15, 2481. https://doi.org/10.3390/ijerph15112481
Luxton NA, Shih P, Rahman MA. Electronic Cigarettes and Smoking Cessation in the Perioperative Period of Cardiothoracic Surgery: Views of Australian Clinicians. International Journal of Environmental Research and Public Health. 2018; 15(11):2481. https://doi.org/10.3390/ijerph15112481
Chicago/Turabian StyleLuxton, Nia A., Patti Shih, and Muhammad Aziz Rahman. 2018. "Electronic Cigarettes and Smoking Cessation in the Perioperative Period of Cardiothoracic Surgery: Views of Australian Clinicians" International Journal of Environmental Research and Public Health 15, no. 11: 2481. https://doi.org/10.3390/ijerph15112481
APA StyleLuxton, N. A., Shih, P., & Rahman, M. A. (2018). Electronic Cigarettes and Smoking Cessation in the Perioperative Period of Cardiothoracic Surgery: Views of Australian Clinicians. International Journal of Environmental Research and Public Health, 15(11), 2481. https://doi.org/10.3390/ijerph15112481






