Knowledge, Attitudes and Perceptions towards Vitamin D in a UK Adult Population: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Population and Timeline
2.2. Questionnaire
2.3. Statistical Analysis.
3. Results
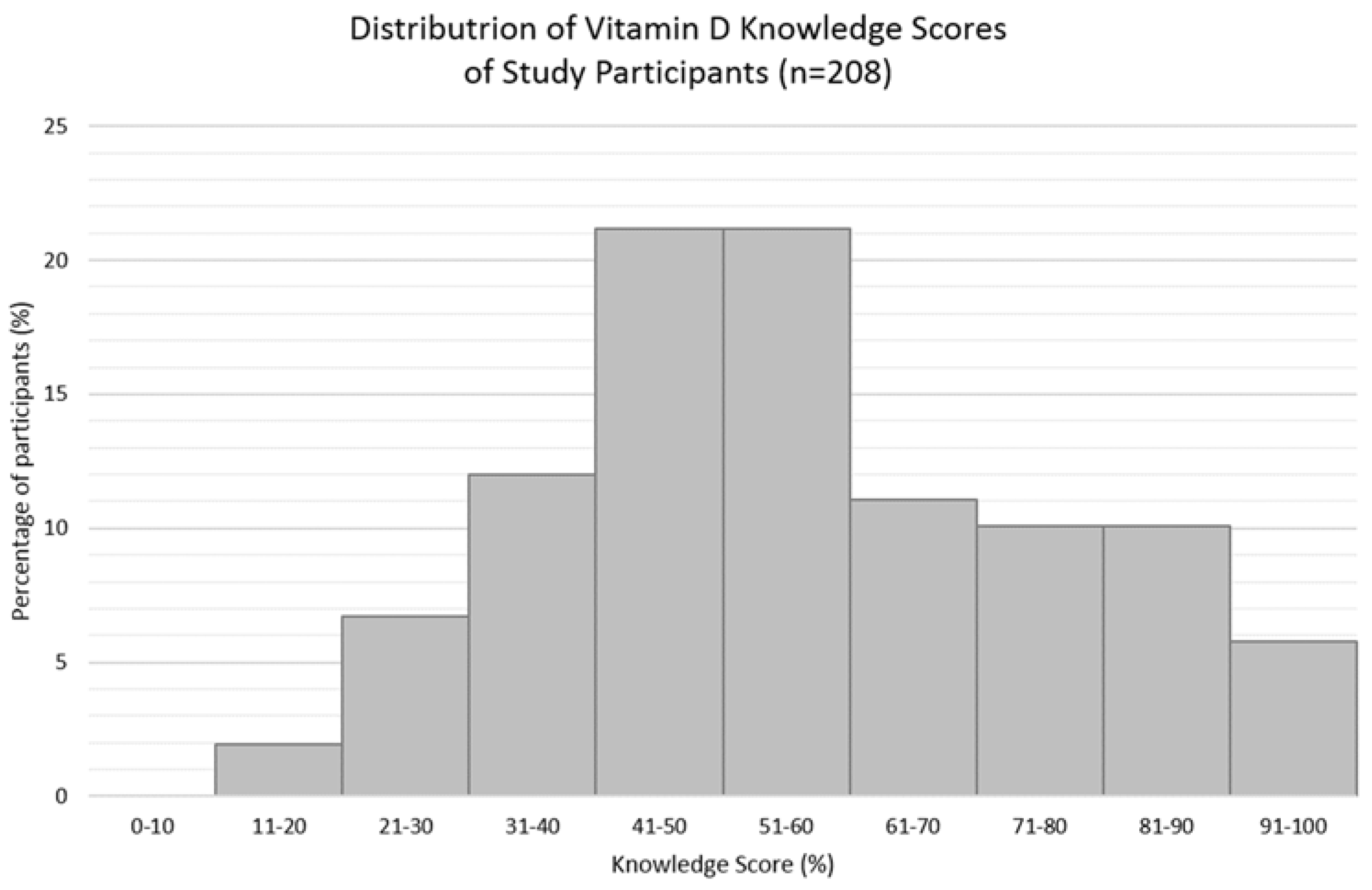
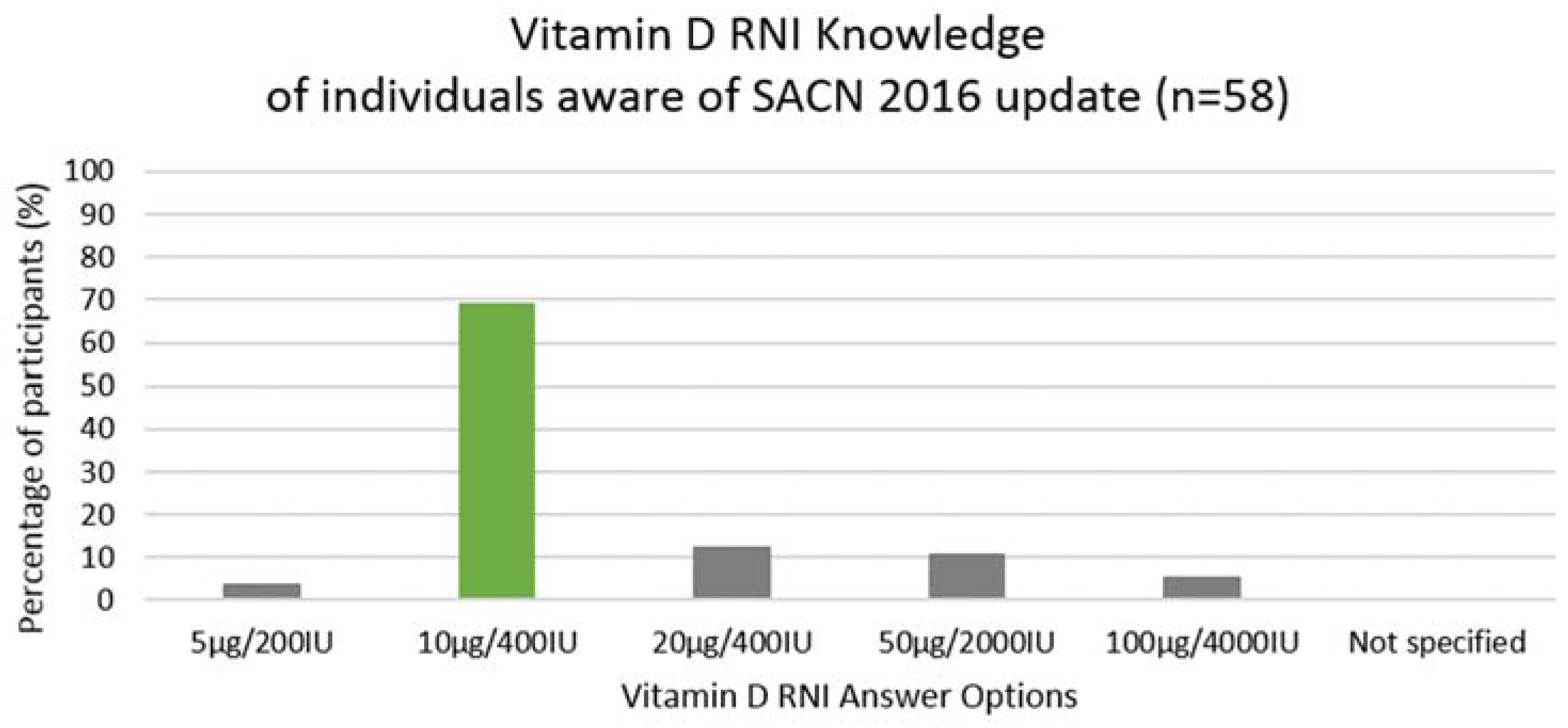
3.1. Vitamin D Knowledge
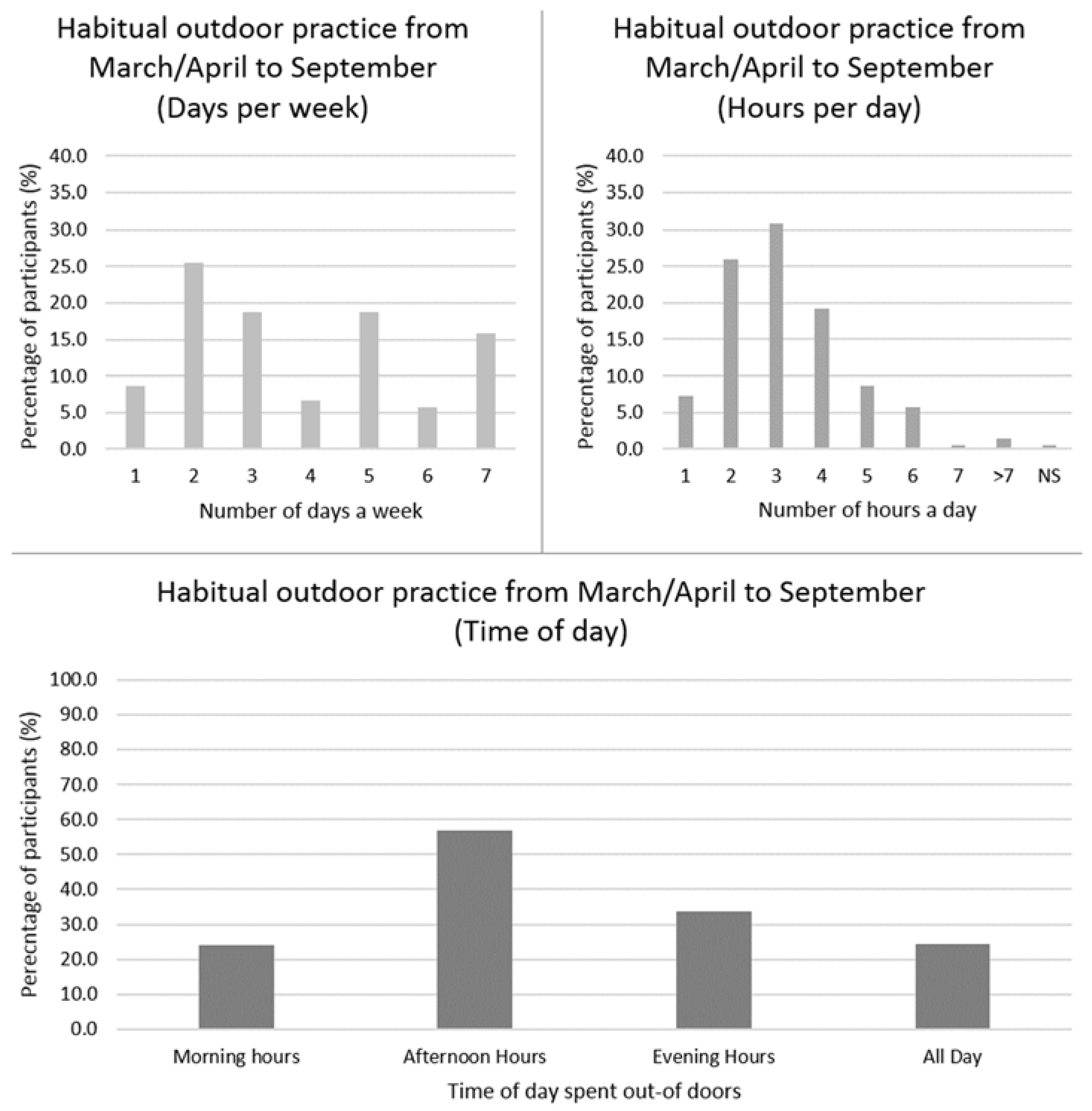
3.2. Perceptions and Practices towards Sun Exposure and Vitamin D
3.3. Attitudes towards Vitamin D
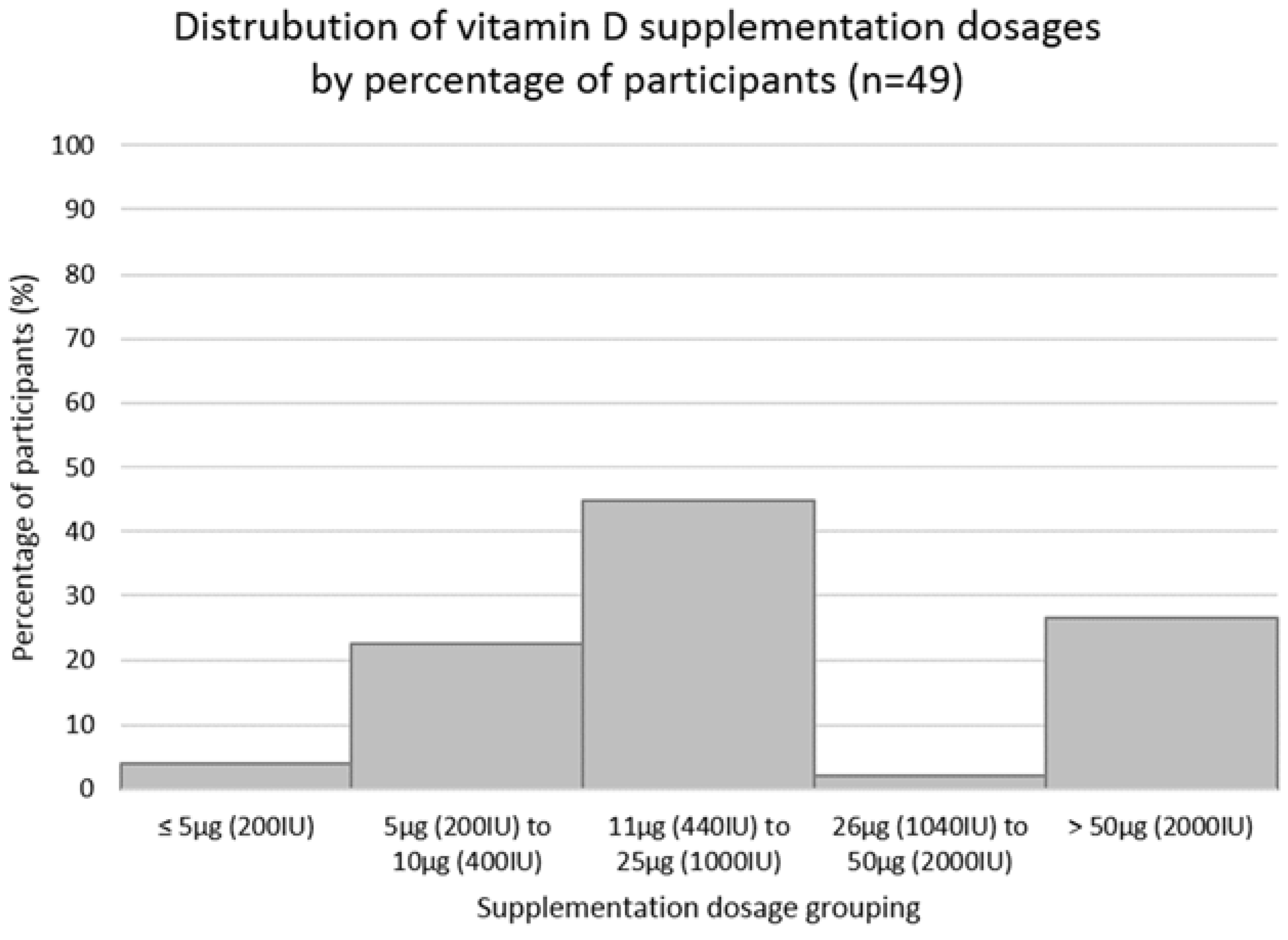
3.4. Perceptions and Practices to Vitamin D Supplementation and Food Fortification
4. Discussion
4.1. Vitamin D Knowledge
4.2. Attitudes towards Sun Exposure and Vitamin D
4.3. Perceptions to Food Fortification and Vitamin D Supplementation
4.4. Factors Contributing to Supplement Use
4.5. Public Health Implications
4.6. Limitations & Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Holick, M.; Chen, T. Vitamin D deficiency: A worldwide problem with health consequences. Am. J. Clin. Nutr. 2008, 87, 1080S–1086S. [Google Scholar] [CrossRef] [PubMed]
- Souberbielle, J.; Body, J.; Lappe, J.; Plebani, M.; Shoenfeld, Y.; Wang, T.; Bischoff-Ferrari, H.; Cavalier, E.; Ebeling, P.; Fardellone, P.; et al. Vitamin D and musculoskeletal health, cardiovascular disease, autoimmunity and cancer: Recommendations for clinical practice. Autoimmun. Rev. 2010, 9, 709–715. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The National Diet and Nutrition Survey: Results from Years 1, 2, 3 and 4 (Combined) of the Rolling Programme (2008/2009–2011/2012). Available online: https://www.gov.uk/government/statistics/national-diet-and-nutrition-survey-results-from-years-1-to-4-combined-of-the-rolling-programme-for-2008-and-2009-to-2011-and-2012 (accessed on 5 April 2018).
- Vitamin D and Health Report (SACN). Available online: https://www.gov.uk/government/publications/sacn-vitamin-d-and-health-report (accessed on 5 April 2018).
- Del Valle, H.B.; Yaktine, A.L.; Taylor, C.L.; Ross, A.C. Dietary Reference Intakes for Calcium and Vitamin D; The National Academies Press: Washington, DC, USA, 2011. [Google Scholar]
- Holick, M.F.; Binkley, N.C.; Bischoff-Ferrari, H.A.; Gordon, C.M.; Hanley, D.A.; Heaney, R.P.; Murad, M.H.; Weaver, C.M. Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J. Clin. Endocrinol. Metab. 2011, 96, 1911–1930. [Google Scholar] [CrossRef] [PubMed]
- Bellavia, D.; Costa, V.; De Luca, A.; Maglio, M.; Pagani, S.; Fini, M.; Giavaresi, G. Vitamin D level between calcium-phosphorus homeostasis and immune system: New perspective in osteoporosis. Curr. Osteoporos. Rep. 2016, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Holick, M.F. Vitamin D: Extraskeletal health. Endocrinol. Metab. Clin. N. Am. 2010, 39, 381–400. [Google Scholar] [CrossRef] [PubMed]
- Van Schoor, N.; Lips, P. Worldwide vitamin D status. Best Pract. Res. Clin. Endocrinol. Metab. 2011, 25, 671–680. [Google Scholar] [CrossRef] [PubMed]
- Kotta, S.; Gadhvi, D.; Jakeways, N.; Saeed, M.; Sohanpal, R.; Hull, S.; Famakin, O.; Martineau, A.; Griffiths, C. “Test me and treat me”—Attitudes to vitamin D deficiency and supplementation: A qualitative study. Br. Med. J. Open 2015, 5, e007401. [Google Scholar] [CrossRef] [PubMed]
- Al-Mutairi, N.; Nair, V.; Issa, B. Photoprotection and vitamin D status: A study on awareness, knowledge and attitude towards sun protection in general population from Kuwait, and its relation with vitamin D levels. Indian J. Dermatol. Venereol. Leprol. 2012, 78, 342–349. [Google Scholar] [CrossRef] [PubMed]
- O’Mahony, L.; Stepien, M.; Gibney, M.; Nugent, A.; Brennan, L. The potential role of vitamin D enhanced foods in improving vitamin D status. Nutrients 2011, 3, 1023–1041. [Google Scholar] [CrossRef] [PubMed]
- Kung, A.; Lee, K. Knowledge of vitamin D and perceptions and attitudes toward sunlight among Chinese middle-aged and elderly women: A population survey in Hong Kong. BMC Public Health 2006, 6, 226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Boland, S.; Irwin, J.; Johnson, A. A survey of university students’ Vitamin D—Related knowledge. J. Nutr. Educ. Behav. 2015, 47, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Vu, L.; Van Der Pols, J.; Whiteman, D.; Kimlin, M.; Neale, R. Knowledge and attitudes about vitamin D and impact on sun protection practices among urban office workers in Brisbane, Australia. Cancer Epidemiol. Biomark. Prev. 2010, 19, 1784–1789. [Google Scholar] [CrossRef] [PubMed]
- Aljefree, N.; Lee, P.; Ahmed, F. Exploring knowledge and attitudes about vitamin D among adults in Saudi Arabia: A qualitative study. Healthcare 2017, 5, 76. [Google Scholar] [CrossRef] [PubMed]
- Deschasaux, M.; Jean-Claude Souberbielle, J.C.; Partula, V.; Lécuyer, L.; Gonzalez, R.; Srour, B.; Guinot, C.; Malvy, D.; Latino-Martel, P.; Druesne-Pecollo, N.; et al. What do people know and believe about vitamin D? Nutrients 2016, 8, 718. [Google Scholar] [CrossRef] [PubMed]
- Arora, H.; Dixit, V.; Srivastava, N. Evaluation of knowledge, practices of vitamin D and attitude towards sunlight among Indian students. Asian J. Pharm. Clin. Res. 2016, 9, 308–313. [Google Scholar]
- Ho-Pham, L.T.; Nguyen, M.T. Survey on knowledge and attitudes on vitamin D and sunlight exposure in an urban population in Vietnam. J. ASEAN Fed. Endocr. Soc. 2012, 27, 191–195. [Google Scholar] [CrossRef]
- Bonevski, B.; Bryant, J.; Lambert, S.; Brozek, I.; Rock, V. The ABC of Vitamin D: A qualitative study of the knowledge and attitudes regarding vitamin D deficiency amongst selected population groups. Nutrients 2013, 5, 915–927. [Google Scholar] [CrossRef] [PubMed]
- BOS Online Survey Tool. Available online: https://www.onlinesurveys.ac.uk/ (accessed on 1 April 2018).
- Vandenbroucke, J.P.; von Elm, E.; Altman, D.G.; Gøtzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Int. J. Surg. 2014, 12, 1500–1524. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spiro, A.; Buttriss, J. Vitamin D: An overview of vitamin D status and intake in Europe. Nutr. Bull. 2014, 4, 322–350. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J. Introduction to Health Behaviour Theory; Jones & Bartlett Learning: Burlington, MA, USA, 2013; ISBN1 1449689752. ISBN2 9781449689759. [Google Scholar]
- The National Diet and Nutrition Survey: Results from Years 5 and 6 (Combined) of the Rolling Programme (2012/2013–2013/2014). Available online: http://doc.ukdataservice.ac.uk/doc/6533/mrdoc/pdf/6533_ndns_yrs5-6_uk_user_guide.pdf (accessed on 5 April 2018).
- Tylavsky, F.A.; Cheng, S.; Lyytikainen, A.; Viljakainen, H.; Lamberg-Allardt, C. Strategies to improve vitamin D status in northern European children: Exploring the merits of vitamin D fortification and supplementation. J. Nutr. 2006, 136, 1130–1134. [Google Scholar] [CrossRef] [PubMed]
- Vitamin D Blood Levels of Canadians. Statistics Canada. 2013. Available online: https://www150.statcan.gc.ca/n1/pub/82-624-x/2013001/article/11727-eng.htm (accessed on 6 May 2018).
- Habib, F.M.; Al-Motairi, Q.A.; Al-Mutairi, W.M. Vitamin D deficiency: Knowledge and practice among Saudi females. Glob. Adv. Res. J. Med. Med. Sci. 2014, 3, 95–101. [Google Scholar]
- Kiely, M.; Cashman, K.D. The ODIN project: Development of food-based approaches for prevention of vitamin D deficiency throughout life. Nutr. Bull. 2015, 40, 235–246. [Google Scholar] [CrossRef] [Green Version]
- Improving Health Literacy to Reduce Health Inequalities. Available online: https://www.gov.uk/government/publications/local-action-on-health-inequalities-improving-health literacy (accessed on 6 May 2018).
- Vitamin D: Supplement Use in Specific Population Groups. Available online: https://www.nice.org.uk/Guidance/PH56 (accessed on 6 April 2018).
- Mistry, K.; Minkovitz, C.; Riley, A.; Johnson, S.; Grason, H.; Dubay, L.; Guyer, B. A new framework for childhood health promotion: The role of policies and programs in building capacity and foundations of early childhood health. Am. J. Public Health 2012, 102, 1688–1696. [Google Scholar] [CrossRef] [PubMed]
- Cancer Research UK. Sun, UV and Cancer. Available online: https://www.cancerresearchuk.org/about-cancer/causes-of-cancer/sun-uv-and-cancer (accessed on 6 April 2018).
| Demographic | Sub-Group | n (%) |
|---|---|---|
| Age | <65 years ≥65 years Not specified | 201 (96) 6 (3) 2 (1) |
| µ (±SD) (in years) | 34.9 (±12.3) years | |
| WHO BMI Category | Underweight (<18.5 kg/m2) Normal weight (18.5–24.9 kg/m2) Overweight (25.0–29.9 kg/m2) Obese (>30.0 kg/m2) Not specified | 9 (4) 114 (54) 52 (25) kg/m2 20 (10) 14 (7) |
| µ (±SD) (in kg/m2) | 24.5 (±4.3) | |
| Gender | Female Male Not specified | 171 (82) 35 (17) 3 (1) |
| Female-Specific Factors | Menopausal Breast-feeding Pregnant | 19 (9) 4 (2) 2 (1) |
| Location | Scotland England Northern Ireland Wales Not specified | 126 (60) 53 (25) 18 (9) 4 (2) 8 (4) |
| Education Level Attained | Undergraduate/Bachelor degree Master’s degree High school Postgraduate degree Other Doctoral degree Trade school Didn’t finish high school | 84 (40) 53 (25) 32 (15) 14 (7) 14 (7) 8 (4) 3 (1) 1 (1) |
| Nutrition-Related Qualification | Yes No Not specified | 41 (20) 165 (79) 3 (1) |
| Ethnicity | Caucasian (White) Asian Black/African American Latino Native Middle Eastern Not specified | 187 (89.5) 8 (4) 2 (1) 2 (1) 2 (1) 1 (0.5) 7 (3) |
| Skin Type | Type 1—light/pale white Type 2—white/fair Type 3—white to moderate brown Type 4—moderate brown Type 5—brown/dark brown Type 6—very dark brown to black/black Not specified | 27 (13) 84 (40) 79 (38) 12 (6) 1 (0.5) 1 (0.5) 5 (2) |
| Answer | Correct (✓) Incorrect (✘) | n (%) | |
|---|---|---|---|
| 1. Overall vitamin D sources (multiple answers *): | Sun Supplement Food Exercise Air Water Don’t know | ✓ ✓ ✓ ✘ ✘ ✘ ✘ | 206 (99) 181 (87) 175 (84) 1 (0.5) 0 (0) 0 (0) 1 (0.5) |
| 2. Best vitamin D source (one answer): | Sunlight Food Supplement Don’t know Water Air Exercise | ✓ ✘ ✘ ✘ ✘ ✘ ✘ | 181 (87) 13 (6) 9 (4) 5 (2) 0 (0) 0 (0) 0 (0) |
| 3. Vitamin D food sources (multiple answers *): | Oily Fish Fortified foods Egg yolks Dairy products Vegetables Red meat Fruit Nuts Chicken Don’t know Not specified | ✓ ✓ ✓ ✘ ✘ ✓ ✘ ✘ ✓ ✘ - | 110 (53) 91 (44) 86 (41) 61 (29) 46 (22) 30 (14) 24 (11) 20 (10) 2 (1) 41 (20) 1 (0.5) |
| 4. Are dietary sources sufficient to maintain vitamin D levels (one answer): | Yes No Unsure Not specified | ✘ ✓ ✘ - | 27 (13) 142 (68) 36 (17) 3 (1) |
| 5. Factors affecting synthesis from sunlight (multiple answers *): | Season Skin Pigmentation Sunscreen use Time of day Cloud cover Latitude Pollution Smoking High-fat diet None of the above Don’t know | ✓ ✓ ✓ ✓ ✓ ✓ ✓ ✘ ✘ ✘ ✘ | 137 (66) 121 (58) 114 (55) 101 (49) 100 (48) 72 (35) 42 (20) 26 (13) 18 (9) 3 (2) 32 (15) |
| 6. Vitamin D health benefits (multiple answers *): | Bone health Prevention of osteoporosis Prevention of rickets Skin health Hair growth Vision None of the above Don’t know | ✓ ✓ ✓ ✘ ✘ ✘ ✘ ✘ | 171 (82) 144 (69) 121 (58) 76 (37) 44 (21) 37 (18) 4 (2) 15 (7) |
| 7. Aware of updated UK vitamin D recommendations (one answer): | No Yes Not Specified | ✘ ✓ ✘ | 146 (70) 58 (28) 4 (2) |
| 8. Vitamin D RNI (one answer): | 5 µg/200 IU 10 µg/400 IU 20 µg/800 IU 50 µg/2000 IU 100 µg/4000 IU Not specified | ✘ ✓ ✘ ✘ ✘ ✘ | 14 (7) 81 (39) 51 (25) 31 (15) 23 (11) 8 (4) |
| 9. Individuals most at risk of vitamin D deficiency (multiple answers *): | Individuals not outdoors often Institutionalised individuals Cover up skin when out Individuals with dark skin Individuals who don’t eat fish None of the above Not Specified | ✓ ✓ ✓ ✓ ✘ ✘ ✘ | 183 (88) 142 (68) 130 (63) 61 (29) 35 (17) 4 (2) 12 (6) |
| 10. Time of year able to receive sufficient synthesis (one answer): | March/April to September All-year October to March Unsure | ✓ ✘ ✘ ✘ | 163 (78) 30 (14) 1 (1) 14 (7) |
| Answers | n (%) | |
|---|---|---|
| Usual practice in sunlight: | Seek direct sun Shade Cover-up/wear clothing Don’t go outside | 117 (56) 50 (24) 41 (20) 0 (0) |
| Frequency of sunscreen use/sun protection: | Sometimes Only for planned exposure/tanning Usually Rarely Always Never | 69 (33) 51 (25) 32 (15) 31 (15) 19 (9) 6 (3) |
| Question | Answers and Sub-Categories | n (%) |
|---|---|---|
| Reasons for not taking supplement (n = 118; multiple answer selection possible ∧): | “I think I get enough” | 43 (36) |
| Unaware of benefits of taking them | 30 (25) | |
| “I don’t know which one I should take” | 26 (22) | |
| “I don’t think it’s important” | 10 (9) | |
| Too expensive | 5 (4) | |
| “I don’t’ know how I can get them” | 3 (3) | |
| Other (additional participant reasons) | ||
| Forgetful/lazy/busy | 12 (10) | |
| Unnatural/dislike taking tablets | 3 (3) | |
| Unwell after use | 2 (2) | |
| Lack of research on benefit | 1 (1) | |
| Other | 4 (3) | |
| Non-specified | 3 (3) | |
| Reasons for taking supplement (n = 91; multiple answer selection possible *): | Don’t get enough from sun exposure | 52 (57) |
| Good for my health | 46 (51) | |
| Don’t get enough from food | 42 (46) | |
| Healthcare professional advice | 22 (24) | |
| Updated guidelines recommendations | 18 (20) | |
| Other (additional participant reasons): | ||
| Friend/family advice | 13 (14) | |
| Mood/Seasonal Affective Disorder | 4 (4) | |
| Other | 6 (7) |
| B | SE | Wald | df | p | Odds-Ratio | 95% CI for Odds-Ratios | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | |||||||
| Nutrition-related qualifications Those with qualification compared to those without | 0.223 | 0.445 | 0.252 | 1 | 0.616 | 1.250 | 0.523 | 2.990 |
| Knowledge score Higher scores (>50%) compared to lower (≤50%) | 0.934 | 0.372 | 6.300 | 1 | 0.012 * | 2.545 | 1.227 | 5.279 |
| University degree Individuals with higher education degree compared to those without | 0.458 | 0.413 | 1.228 | 1 | 0.268 | 1.581 | 0.703 | 3.555 |
| Location (1) Wales compared to Scotland | −1.067 | 1.386 | 0.593 | 1 | 0.441 | 0.344 | 0.023 | 5.200 |
| Location (2) England compared to Scotland | −1.076 | 0.394 | 7.465 | 1 | 0.006 * | 0.341 | 0.158 | 0.738 |
| Location (3) Northern Ireland compared to Scotland | −0.886 | 0.612 | 2.094 | 1 | 0.148 | 0.412 | 0.124 | 1.369 |
| Concern re levels (1) Individuals who are “unsure if concerned” compared to those who “are not concerned” | 0.055 | 0.631 | 0.008 | 1 | 0.930 | 1.057 | 0.307 | 3.641 |
| Concern re levels (2) “Yes” compared to “no” | 0.750 | 0.359 | 4.365 | 1 | 0.037 * | 2.118 | 1.048 | 4.281 |
| Levels tested (1) “Unsure” compared to “no” | −0.646 | 0.808 | 0.640 | 1 | 0.424 | 0.524 | 0.108 | 2.553 |
| Levels tested (2) “Yes” compared to “no” | 0.757 | 0.510 | 2.204 | 1 | 0.138 | 2.131 | 0.785 | 5.785 |
| Willingness to purchase/consume fortified foods (1) “Unsure” compared to “no” | −0.654 | 0.626 | 1.091 | 1 | 0.296 | 0.520 | 0.153 | 1.773 |
| Willingness to purchase/consume fortified foods (2) “Yes” compared to “no” | 0.109 | 0.541 | 0.041 | 1 | 0.840 | 1.116 | 0.386 | 3.221 |
| Constant | −1.198 | 0.621 | 3.719 | 1 | 0.054 | 0.302 | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
O’Connor, C.; Glatt, D.; White, L.; Revuelta Iniesta, R. Knowledge, Attitudes and Perceptions towards Vitamin D in a UK Adult Population: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2018, 15, 2387. https://doi.org/10.3390/ijerph15112387
O’Connor C, Glatt D, White L, Revuelta Iniesta R. Knowledge, Attitudes and Perceptions towards Vitamin D in a UK Adult Population: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2018; 15(11):2387. https://doi.org/10.3390/ijerph15112387
Chicago/Turabian StyleO’Connor, Clodagh, Dominique Glatt, Lois White, and Raquel Revuelta Iniesta. 2018. "Knowledge, Attitudes and Perceptions towards Vitamin D in a UK Adult Population: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 15, no. 11: 2387. https://doi.org/10.3390/ijerph15112387
APA StyleO’Connor, C., Glatt, D., White, L., & Revuelta Iniesta, R. (2018). Knowledge, Attitudes and Perceptions towards Vitamin D in a UK Adult Population: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 15(11), 2387. https://doi.org/10.3390/ijerph15112387




