Disparities in Non-Fatal Health Outcomes in Pediatric General Trauma Studies
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
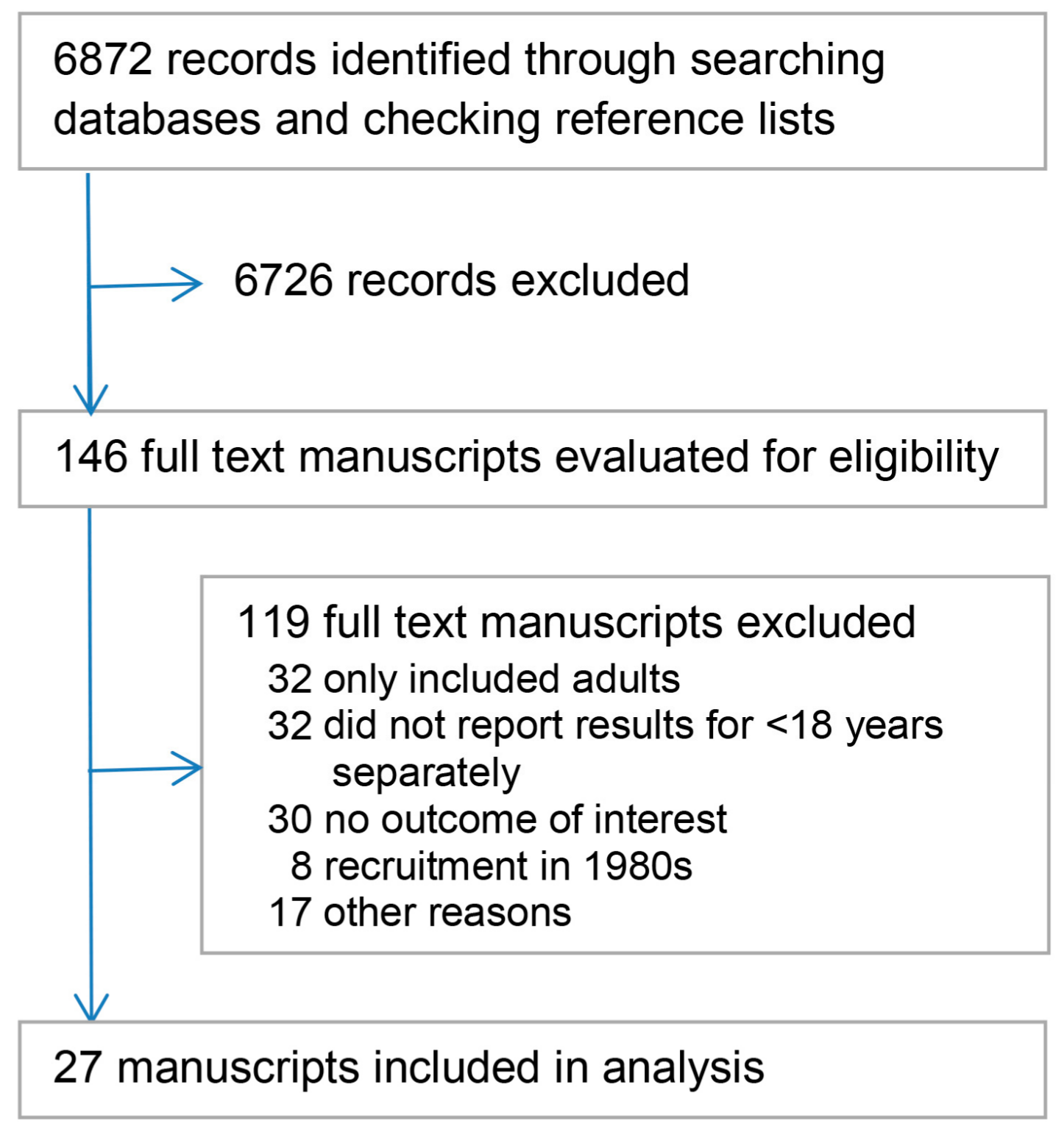
2.2. Study Selection
2.3. Data Extraction and Synthesis
3. Results
3.1. Summary of Included Studies
3.2. PROGRESS Dimensions in Eligibility and Participation
3.3. Reporting of Outcomes
4. Discussion
5. Conclusions
Supplementary Materials:
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Peden, M.M.; Oyegbite, K.; Ozanne-Smith, J.; Hyder, A.A.; Branche, C.; Rahman, A.K.M.F.; Rivara, F.P.; Bartolomeos, K. World Report on Child Injury Prevention; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Sethi, D.; Arlidge, E.; Rakovac, I.; Makhija, A. Worsening Inequalities in Child Injury Deaths in the WHO European Region. Int. J. Environ. Res. Public Health 2017, 14, 26. [Google Scholar] [CrossRef] [PubMed]
- Aitken, M.; Tilford, J.M.; Barrett, K.W.; Parker, J.G.; Simpson, P.; Landgraf, J.; Robbins, J.M. Health status of children after admission for injury. Pediatrics 2002, 110, 337–342. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, M.L. Measuring children’s health-related quality of life after trauma. J. Trauma Acute Care Surg. 2007, 63, S121–S129. [Google Scholar] [CrossRef] [PubMed]
- Gofin, R.; Avitzour, M. Outcome of head and other injuries among Israeli children: Physical limitations and stress symptoms. Isr. Med. Assoc. J. 2007, 9, 531–536. [Google Scholar] [PubMed]
- Batailler, P.; Hours, M.; Maza, M.; Charnay, P.; Tardy, H.; Tournier, C.; Javouhey, E. Health status recovery at one year in children injured in a road accident: A cohort study. Accid. Anal. Prev. 2014, 71, 267–272. [Google Scholar] [CrossRef] [PubMed]
- Davey, T.; Aitken, L.M.; Kassulke, D.; Bellamy, N.; Ambrose, J.; Gee, T.; Clark, M. Long-term outcomes of seriously injured children: A study using the Child Health Questionnaire. J. Paediatr. Child Health 2005, 41, 278–283. [Google Scholar] [CrossRef] [PubMed]
- Watson, W. Cost of Death and Hospital-Treated Injury, 2001. Available online: https://www.monash.edu/__data/assets/pdf_file/0003/218469/haz54.pdf (accessed on 2 October 2017).
- Landolt, M.A.; Vollrath, M.E.; Gnehm, H.E.; Sennhauser, F.H. Post-traumatic stress impacts on quality of life in children after road traffic accidents: Prospective study. Aust. N. Z. J. Psychiatry 2009, 43, 746–753. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Efron, D.T.; Haut, E.R.; DiRusso, S.M.; Sullivan, T.; Cornwell, E.E. Black children experience worse clinical and functional outcomes after traumatic brain injury: An analysis of the National Pediatric Trauma Registry. J. Trauma Acute Care Surg. 2007, 62, 1259–1263. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Health Assembly Adopts Resolution Targeted at Saving the Lives of Children from Injury; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Institute of Medicine: Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care; Institute of Medicine: Washington, DC, USA, 2003. [Google Scholar]
- Sharma, M.; Schoenfeld, A.J.; Jiang, W.; Chaudhary, M.A.; Ranjit, A.; Zogg, C.K.; Learn, P.; Koehlmoos, T.; Haider, A.H. Universal Health Insurance and its association with long term outcomes in Pediatric Trauma Patients. Injury 2017, 23, 23. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, M.A.; Shah, A.A.; Zogg, C.K.; Changoor, N.; Chao, G.; Nitzschke, S.; Havens, J.M.; Haider, A.H. Differences in rural and urban outcomes: A national inspection of emergency general surgery patients. J. Surg. Res. 2017, 218, 277–284. [Google Scholar] [CrossRef] [PubMed]
- Britton, B.V.; Nagarajan, N.; Zogg, C.K.; Selvarajah, S.; Schupper, A.J.; Kironji, A.G.; Lwin, A.T.; Cerullo, M.; Salim, A.; Haider, A.H. Awareness of racial/ethnic disparities in surgical outcomes and care: Factors affecting acknowledgment and action. Am. J. Surg. 2016, 212, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Schneider, E.B.; Sriram, N.; Scott, V.K.; Swoboda, S.M.; Zogg, C.K.; Dhiman, N.; Haut, E.R.; Efron, D.T.; Pronovost, P.J.; et al. Unconscious Race and Class Biases among Registered Nurses: Vignette-Based Study Using Implicit Association Testing. J. Am. Coll. Surg. 2015, 220, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Schneider, E.B.; Sriram, N.; Dossick, D.S.; Scott, V.K.; Swoboda, S.M.; Losonczy, L.; Haut, E.R.; Efron, D.T.; Pronovost, P.J.; et al. Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015, 150, 457–464. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Schneider, E.B.; Sriram, N.; Dossick, D.S.; Scott, V.K.; Swoboda, S.M.; Losonczy, L.; Haut, E.R.; Efron, D.T.; Pronovost, P.J.; et al. Unconscious race and class bias: Its association with decision making by trauma and acute care surgeons. J. Trauma Acute Care Surg. 2014, 77, 409–416. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Wevgandt, P.L.; Bentley, J.M.; Monn, M.F.; Rehman, K.A.; Zarzaur, B.L.; Crandall, M.L.; Cornwell, E.E.; Cooper, L.A. Disparities in trauma care and outcomes in the United States: A systematic review and meta-analysis. J. Trauma Acute Care Surg. 2013, 74, 1195–1205. [Google Scholar] [CrossRef] [PubMed]
- Hosking, J.E.; Ameratunga, S.N.; Bramley, D.M.; Crengle, S.M. Reducing ethnic disparities in the quality of trauma care: An important research gap. Ann. Surg. 2011, 253, 233–237. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, J.; Tabish, H.; Welch, V.; Petticrew, M.; Pottie, K.; Clarke, M.; Evans, T.; Pardo Pardo, J.; Waters, E.; White, H. Applying an equity lens to interventions: Using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. J. Clin. Epidemiol. 2014, 67, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Welch, V.A.; Petticrew, M.; O’Neill, J.; Waters, E.; Armstrong, R.; Bhutta, Z.; Francis, D.; Koehlmoos, T.P.; Kristiansson, E.; Pantoja, T. Health equity: Evidence synthesis and knowledge translation methods. Syst. Rev. 2013, 2, 43. [Google Scholar] [CrossRef] [PubMed]
- Tugwell, P.; Petticrew, M.; Kristiansson, E.; Welch, V.; Ueffing, E.; Waters, E.; Bonnefoy, J.; Morgan, A.; Doohan, E.; Kelly, M.P. Assessing equity in systematic reviews: Realising the recommendations of the Commission on Social Determinants of Health. Br. Med. J. 2010, 341, c4739. [Google Scholar] [CrossRef] [PubMed]
- Welch, V.; Petticrew, M.; Tugwell, P.; Moher, D.; O’Neill, J.; Waters, E.; White, H. PRISMA-Equity 2012 extension: Reporting guidelines for systematic reviews with a focus on health equity. Rev. Panam. Salud Pública 2013, 34, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Janssens, L.; Gorter, J.W.; Ketelaar, M.; Kramer, W.L.M.; Holtslag, H.R. Health-related quality-of-life measures for long-term follow-up in children after major trauma. Qual. Life Res. 2008, 17, 701–713. [Google Scholar] [CrossRef] [PubMed]
- Martin-Herz, S.P.; Zatzick, D.F.; McMahon, R.J. Health-related quality of life in children and adolescents following traumatic injury: A review. Clin. Child Fam. Psychol. Rev. 2012, 15, 192–214. [Google Scholar] [CrossRef] [PubMed]
- Polinder, S.; Haagsma, J.A.; Belt, F.; Lyons, R.A.; Erasmus, V.; Lund, J.; van Beeck, E.F. A systematic review of studies measuring health-related quality of life of general injury populations. BMC Public Health 2010, 10, 783. [Google Scholar] [CrossRef] [PubMed]
- Willis, C.D.; Gabbe, B.J.; Butt, W.; Cameron, P. Assessing outcomes in paediatric trauma populations. Injury 2006, 37, 1185–1196. [Google Scholar] [CrossRef] [PubMed]
- Winthrop, A.L. Health-related quality of life after pediatric trauma. Curr. Opin. Pediatr. 2010, 22, 346–351. [Google Scholar] [CrossRef] [PubMed]
- National Institute of Health. Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies. 2014. Available online: https://www.nhlbi.nih.gov/health-pro/guidelines/in-develop/cardiovascular-risk-reduction/tools/cohort (accessed on 1 October 2017).
- Dekker, R.; Van der Sluis, C.K.; Kootstra, J.; Groothoff, J.W.; Eisma, W.H.; Ten Duis, H.J. Long-term outcome of equestrian injuries in children. Disabil. Rehabil. 2004, 26, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Gabbe, B.; Simpson, P.M.; Palmer, C.S.; Williamson, O.D.; Butt, W.; Bevan, C.; Cameron, P. Functional and health-related quality of life outcomes after pediatric trauma. J. Trauma 2011, 70, 1532–1538. [Google Scholar] [CrossRef] [PubMed]
- Gofin, R.; Adler, B.; Hass, T. Incidence and impact of childhood and adolescent injuries: A population-based study. J. Trauma 1999, 47, 15–21. [Google Scholar] [CrossRef] [PubMed]
- Holbrook, T.; Hoyt, D.B.; Coimbra, R.; Potenza, B.; Sise, M.J.; Sack, D.I.; Anderson, J.P. Trauma in adolescents causes long-term marked deficits in quality of life: Adolescent children do not recover preinjury quality of life or function up to two years postinjury compared to national norms. J. Trauma 2007, 62, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Janssens, L.; Gorter, J.W.; Ketelaar, M.; Kramer, W.L.M.; Holtslag, H.R. Long-term health-related quality of life in major pediatric trauma: A pilot study. Eur. J. Trauma Emerg. Surg. 2009, 4, 371–377. [Google Scholar] [CrossRef] [PubMed]
- Kendrick, D.; Vinogradova, Y.; Coupland, C.; Mulvaney, C.A.; Christie, N.; Lyons, R.; Towner, E.L. On behalf of the UK Burden of Injuries Study Group. Recovery from injury: The UK Burden of Injury Multicentre Longitudinal Study. Injury Prev. 2013, 19, 370–381. [Google Scholar] [CrossRef] [PubMed]
- Macpherson, A.K.; Rothman, L.; McKeag, A.M.; Howard, A. Mechanism of injury affects 6-onth functional outcome in children hospitalized because of severe injuries. J. Trauma 2003, 55, 454–458. [Google Scholar] [CrossRef] [PubMed]
- Meštrović, J.; Meštrović, M.; Polić, B.; Markić, J.; Kardum, G.; Gunjaca, G.; Matas, A.; Catipović, T.; Radonić, M. Clinical scoring systems in predicting health-related quality of life of children with injuries. Coll. Antropol. 2013, 37, 373–377. [Google Scholar] [PubMed]
- Olofsson, E.; Bunketorp, O.; Andersson, A.-L. Children at risk of residual physical problems after public road traffic injuries—A 1-year follow-up study. Injury 2012, 43, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Polinder, S.; Meerding, W.J.; Toet, H.; Mulder, S.; Essink-Bot, M.-L.; van Beeck, E.F. Prevalence and prognostic factors of disability after childhood injury. Pediatrics 2005, 116, e810–e817. [Google Scholar] [CrossRef] [PubMed]
- Pumar, P.M.R.; Nunez, A.R.; Fernandez, B.-O.; Santos, L.S.; Collazo, L.R.; Torres, F.M.; Sanchez, M. Consecuencias a largo plazo de los traumatismos pediatricos que precisaron cuidados intensivos. An. Pediatr. 2007, 66, 4–10. [Google Scholar] [CrossRef]
- Schalamon, J.; Bismark, S.V.; Schober, P.H.; Hollwarth, M.E. Multiple trauma in pediatric patients. Pediatr. Surg. Int. 2003, 19, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Schneeberg, A.; Ishikawa, T.; Kruse, S.; Zallen, E.; Mitton, C.; Bettinger, J.A.; Brussoni, M. A longitudinal study on quality of life after injury in children. Health Qual. Life Outcomes 2016, 14, 120. [Google Scholar] [CrossRef] [PubMed]
- Schweer, L.H.; Cook, B.S.; Bivens, K.; Van Kuiken, D.; Garcia, V.F.; Falcone, R.A., Jr. Family perception: Quality of life following a child’s traumatic injury. J. Trauma Nurs. 2006, 13, 6–16. [Google Scholar] [CrossRef] [PubMed]
- Sturms, L.M.; van der Sluis, C.K.; Snippe, H.; Groothoff, J.W.; ten Duis, H.J.; Eisma, W.H. Bicycle-spoke injuries among children: Accident details and consequences. Pediatr. Traffic Inj. 2002, 146, 1691–1696. [Google Scholar]
- Sturms, L.M.; van der Sluis, C.K.; Groothoff, J.W.; Eisma, W.H.; ten Duis, H.J. The health-related quality of life of pediatric traffic victims. J. Trauma 2002, 52, 88–94. [Google Scholar] [CrossRef] [PubMed]
- Sturms, L.M.; van der Sluis, C.K.; Stewart, R.E.; ten Duis, H.J. A prospective study on paediatric traffic injuries: Health-related quality of life of life and post-traumatic stress. Clin. Rehabil. 2005, 19, 312–322. [Google Scholar] [PubMed]
- Valadka, S.; Poenaru, D.; Dueck, A. Long-term disability after trauma in children. J. Pediatr. Surg. 2000, 35, 684–687. [Google Scholar] [CrossRef] [PubMed]
- Van de Voorde, P.; Sabbe, M.; Tsonka, R.; Rizopoulos, D.; Calle, P.; de Jaeger, A.; Lesaffre, E.; Matthys, D. The long-term outcome after severe trauma of children in Flanders (Belgium): A population-based cohort study using the International Classification of Functioning-related outcome score. Eur. J. Pediatr. 2011, 170, 65–73. [Google Scholar] [CrossRef] [PubMed]
- Vollrath, M.; Landolt, M. Personality predicts quality of life in pediatric patients with unintentional injuries: A 1-year follow-up study. J. Pediatr. Psychol. 2005, 30, 481–491. [Google Scholar] [CrossRef] [PubMed]
- Winthrop, A.L.; Brasel, K.J.; Stahovic, L.; Paulson, J.; Schneeberger, B.; Kuhn, E.M. Quality of life and functional outcome after pediatric trauma. J. Trauma 2005, 58, 468–474. [Google Scholar] [CrossRef] [PubMed]
- Yacoubovitch, J.; Lelong, N.; Conquer, M.; Tursz, A. Étude épidémiologique des séquelles d’accidents à l’adolescence. Arch. Pediatr. 1995, 2, 532–538. [Google Scholar] [CrossRef]
- Krieger, N. The making of public health data: Paradigms, politics, and policy. J. Public Health Policy 1992, 13, 412–427. [Google Scholar] [CrossRef] [PubMed]
- Shafi, S.; de la Plata, C.M.; Diaz-Arrastia, R.; Bransky, A.; Frankel, H.; Elliott, A.C.; Parks, J.; Gentilello, L.M. Ethnic disparities exist in trauma care. J. Trauma Acute Care Surg. 2007, 63, 1138–1142. [Google Scholar] [CrossRef] [PubMed]
- Aaland, M.O.; Marose, K.; Zhu, T.H. The lost to trauma patient follow-up: A system or patient problem. J. Trauma Acute Care Surg. 2012, 73, 1507–1511. [Google Scholar] [CrossRef] [PubMed]
- Leukhardt, W.H.; Golob, J.F.; McCoy, A.M.; Fadlalla, A.M.; Malangoni, M.A.; Claridge, J.A. Follow-up disparities after trauma: A real problem for outcomes research. Am. J. Surg. 2010, 199, 348–352. [Google Scholar] [CrossRef] [PubMed]
- Ameratunga, S.; Officer, A.; Temple, B.; Tin, S.T. Rehabilitation of the injured child. Bull. World Health Organ. 2009, 87, 327–328. [Google Scholar] [CrossRef] [PubMed]
- Arlidge, B.; Asiasiga, L.; Milne, S.L.; Crengle, S.; Ameratunga, S. Experiences of whanau/families when injured children are admitted to hospital: A multi-ethnic qualitative study from Aotearoa/New Zealand. Ethn. Health 2009, 14, 169–183. [Google Scholar] [CrossRef] [PubMed]
- Haider, A.H.; Scott, V.K.; Rehman, K.A.; Velopulos, C.; Bentley, J.M.; Cornwell, E.E.; Al-Refaie, W. Racial disparities in surgical care and outcomes in the United States: A comprehensive review of patient, provider, and systemic factors. J. Am. Coll. Surg. 2013, 216, 482–492. [Google Scholar] [CrossRef] [PubMed]
- Tin, S.T.; Elwood, J.M.; Lawrenson, R.; Campbell, I.; Harvey, V.; Seneviratne, S. Differences in Breast Cancer Survival between Public and Private Care in New Zealand: Which Factors Contribute? PLoS ONE 2016, 11, e0153206. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.; Foster, K.; Mitchell, R.; Van, C. How is care provided for patients with paediatric trauma and their families in Australia? A mixed-method study. J. Paediatr. Child Health 2016, 52, 832–836. [Google Scholar] [CrossRef] [PubMed]
| Study Characteristics | Details |
|---|---|
| Country | Number of studies |
| The Netherlands | 6 |
| USA | 4 |
| Canada | 3 |
| Australia, France, Israel, Switzerland | 2 each |
| Austria, Belgium, Croatia, Spain, Sweden, UK | 1 each |
| Number of participants at final follow-up * | Number of participants |
| Median (inter-quartile range) | 146 (107–241) |
| Range | 28–700 |
| Proportion of eligible children in final follow-up * | % |
| Median (inter-quartile range) | 64 (57–73) |
| Range | 20–90 |
| Period of final follow-up (years since injury) | Number of studies |
| ≤0.5 | 7 |
| >0.5 ≤ 1 | 10 |
| >1 ≤ 3 | 4 |
| >3 | 6 |
| Tool used to measure outcome ** | Number of studies |
| A study-specific question/questionnaire | 8 |
| TACQOL | 5 |
| Child Health Questionnaire (CHQ)-PF50/PF28/CF87 | 5 |
| FIM/WeeFIM | 4 |
| Glasgow Outcome Scale/GOS-Extended | 3 |
| PEDSQL | 2 |
| EQ-5D, FS-II, IROS, KOSCHI, QWB, RAHC MOF, Rand Health Insurance, VABS, CBCL, SDQ, POPC | 1 each |
| Study (Alphabetical Order) | Country | Number of Children at Final Follow-Up | Proportion of Eligible Children Included at Final Follow-Up (%) | Period of Final Follow-Up (Years Since Injury) | Tool Used to Measure Outcome ** |
|---|---|---|---|---|---|
| Aitken 2002 [3] | USA | 141 | 45.5 | 0.5 | CHQ-PF50, FIM/WeeFIM |
| Batailler 2014 [6] | France | 127 | * | 1 | Study-specific question(s) |
| Davey 2005 [7] | Australia | 241 | 57.4 | 1–2 | CHQ-PF50 |
| Dekker 2004 [31] | The Netherlands | 100 | 71.9 | 2–7 | CHQ-CF87 |
| Gabbe 2011 [32] | Australia | 144 | * | 1 | FIM, GOS, KOSCHI, CHQ-PF28, PEDSQL |
| Gofin 1999 [33] | Israel | not reported | * | 0.5 | for 4–17 years 25 items questionnaire developed from International Classification of Impairments, Disabilities and Handicaps; study-specific questions for 0–3 years age group |
| Gofin 2007 [5] | Israel | 549 | 59.4 | 0.42 | Study-specific question(s) |
| Holbrook 2007 [34] | USA | 356 | 88.8 | 2 | Quality of wellbeing scale (QWB) |
| Janssens 2009 [35] | The Netherlands | 28 | 70.0 | 6–8 | GOS, GOSE, VABS, CBCL, SDQ |
| Kendrick 2013 [36] | UK | 164 | * | 1 | Study-specific question(s) |
| Landolt 2009 [9] | Switzerland | 68 | 58.6 | 1 | TACQOL + study-specific question(s) |
| Macpherson 2003 [37] | Canada | 357 | 73.0 | 0.5 | WeeFIM |
| Mestrovic 2013 [38] | Croatia | not reported | * | 1 | RAHC MOF to assess HRQOL |
| Oloffson 2012 [39] | Sweden | 341 | 81.2 | 1–1.67 | Study-specific question(s) |
| Polinder 2005 [40] | The Netherlands | 365 | 29.9 | 0.75 | EuroQol (EQ-5D) |
| Pumar 2007 [41] | Spain | 209 | * | 2–5 | POPC |
| Schalamon 2003 [42] | Austria | 58 | 82.9 | 2–9 | GOS |
| Schneeberg 2017 [43] | Canada | 161 | 19.5 | 1 | PEDSQL |
| Schweer 2006 [44] | USA | 128 | 22.2 | 0.5 | CHQ-PF50 |
| Sturms 2002a [45] | The Netherlands | 59 | 67.8 | 0.5–2.1 | FS-II, TACQOL |
| Sturms 2002b [46] | The Netherlands | 211 | 64.5 | 1.5–3.4 | TACQOL |
| Sturms 2005 [47] | The Netherlands | 51 | 35.7 | 0.5 | TACQOL |
| Valadka 2000 [48] | Canada | 116 | 58.3 | not reported | Rand Health Insurance Study physical health scales + study question(s) |
| van de Voorde 2011 [49] | Belgium | 146 | 63.8 | 1 | IROS |
| Vollrath 2005 [50] | Switzerland | 107 | 60.1 | 1 | TACQOL |
| Winthrop 2005 [51] | USA | 156 | 86.7 | 0.5 | FIM/WeeFIM |
| Yacoubovitch 1995 [52] | France | 700 | * | 1 | Study-specific question(s) |
| Social Dimension | Baseline Participant Characteristics | Loss to Follow-Up | Disaggregated/Unadjusted Outcomes | Adjusted Outcomes | |||
|---|---|---|---|---|---|---|---|
| Reported n (%) | Reported n (%) | Difference Found * | Reported n (%) | Difference Found * | Reported n (%) | Difference Found * | |
| P Place of residence | 1 (4) | - | - | 2 (7) | 1 | 1 (4) | 1 |
| R Race/ethnicity/culture/language | 7 (26) | 1 (4) | - | 2 (7) | - | 2 (7) | - |
| O Occupation | 2 (7) | 1 (4) | 1 | 1 (4) | - | - | - |
| G Gender/sex | 24 (89) | 9 (33) | 1 | 8 (30) | 2 | 11 (41) | 3 |
| R Religion | - | - | - | - | - | - | - |
| E Education | 1 (4) | - | - | 1 (4) | 1 | 2 (7) | 1 |
| S Socio-economic status | 4 (15) | 1 (4) | 1 | 2 (7) | - | 1 (4) | - |
| S Social capital | 2 (7) | - | - | - | - | 1 (4) | - |
| At least one | 25 (93) | 10 (37) | 10 (37) | 13 (48) | |||
| Explanatory Factor | PROGRESS Criteria | Study | Reported Difference(s) in Children | |
|---|---|---|---|---|
| Propensity of being lost to follow-up (a key factor that could influence investigations of predictors of differential health outcomes) | Occupation | Batailler 2014 [6] | Non-respondents were reported as more likely to be of lower socio-economic occupational level; no related data or statistics provided | |
| Gender | Yacoubovitch 1995 [52] | 8% of boys and 13% of girls were lost to follow-up; no statistics provided | ||
| Socio-economic status (SES) | Schneeberg 2017 [43] | Participants in low-income families less available for 12 months follow-up interview. Odds Ratio (95% CI) | ||
| 5 (highest-income quintile) | 1.0 (reference) | |||
| 4 | 0.5 (0.2–1.4) | |||
| 3 | 1.8 (0.6–4.9) | |||
| 2 | 0.7 (0.3–1.8) | |||
| 1 (lowest income quintile) | 0.3 (0.1–0.7) | |||
| Unadjusted outcomes | Place | Kendrick 2013 [36] | Variations in recovery at 12 months by study site Relative Risk (95% CI) | |
| Nottingham | 1.00 | |||
| Bristol | 1.17 (0.98–1.41) | |||
| Swansea | 1.22 (1.05–1.40) | |||
| Surrey | 1.21 (1.05–1.39) | |||
| Gender | Yacoubovitch 1995 [52] | 20% girls compared with 12% boys had not recovered at 12 months (p < 0.01) | ||
| Polinder 2005 [40] | Girls more likely than boys to have sub-optimal functioning at 12 months Odds Ratio (95% CI) | |||
| Boy | 1.0 | |||
| Girl | 2.9 (1.0–9.9) | |||
| Education | Sturms 2002b [46] | Predictors of lower health-related quality of life at a mean follow-up period of 2.4 years post-injury | ||
| Lower educational level of father (p = 0.001) | ||||
| Lower educational level of mother (p < 0.001) | ||||
| Adjusted outcomes | Place | Kendrick 2013 [36] | Recovery at 12 months: Relative Risk (95% CI) | |
| Nottingham | 1.00 | |||
| Bristol | 1.01 (0.88–1.16) | |||
| Swansea | 1.12 (0.99–1.27) | |||
| Surrey | 1.15 (1.02–1.30) | |||
| Gender | Kendrick 2013 [36] | Recovery at 12 months: Relative Risk (95% CI) | ||
| Girls | 1.0 | |||
| Boys | 1.15 (1.03–1.27) | |||
| Polinder 2005 [40] | Sub-optimal functioning at 12 months Odds Ratio (95% CI) | |||
| Boy | 1.0 | |||
| Girl | 3.0 (1.0–11.0) | |||
| Holbrook 2007 [34] | Results section notes the Quality of Well Being scores at 18-month follow-up were lower in adolescent girls than in boys; no data provided | |||
| Education | Sturms 2002b [46] | Lower education of fathers and mothers (highly correlated) were significant explanatory variables of lower health-related quality of life of children. Estimate for mothers’ educational level provided (p < 0.001) | ||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ameratunga, S.; Ramke, J.; Jackson, N.; Tin Tin, S.; Gabbe, B. Disparities in Non-Fatal Health Outcomes in Pediatric General Trauma Studies. Int. J. Environ. Res. Public Health 2018, 15, 43. https://doi.org/10.3390/ijerph15010043
Ameratunga S, Ramke J, Jackson N, Tin Tin S, Gabbe B. Disparities in Non-Fatal Health Outcomes in Pediatric General Trauma Studies. International Journal of Environmental Research and Public Health. 2018; 15(1):43. https://doi.org/10.3390/ijerph15010043
Chicago/Turabian StyleAmeratunga, Shanthi, Jacqueline Ramke, Nicki Jackson, Sandar Tin Tin, and Belinda Gabbe. 2018. "Disparities in Non-Fatal Health Outcomes in Pediatric General Trauma Studies" International Journal of Environmental Research and Public Health 15, no. 1: 43. https://doi.org/10.3390/ijerph15010043
APA StyleAmeratunga, S., Ramke, J., Jackson, N., Tin Tin, S., & Gabbe, B. (2018). Disparities in Non-Fatal Health Outcomes in Pediatric General Trauma Studies. International Journal of Environmental Research and Public Health, 15(1), 43. https://doi.org/10.3390/ijerph15010043






