Dental Environmental Noise Evaluation and Health Risk Model Construction to Dental Professionals
Abstract
:1. Introduction
2. Materials and Methods
2.1. Noise Exposure Assessment
2.2. Health Risk Assessment
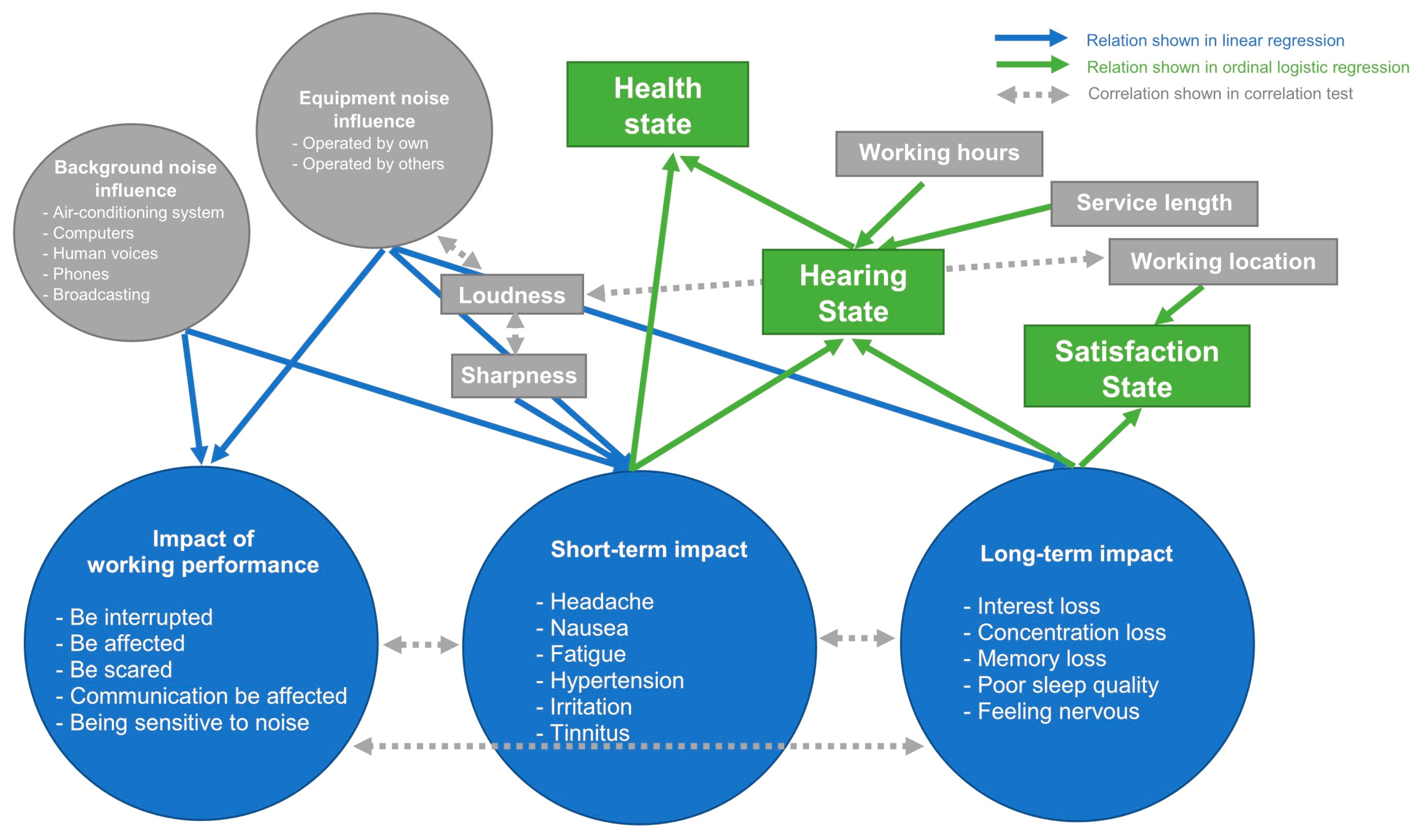
2.3. Health Risk Model from Statistical Analyses
3. Results
3.1. Results of Noise Exposure Assessment
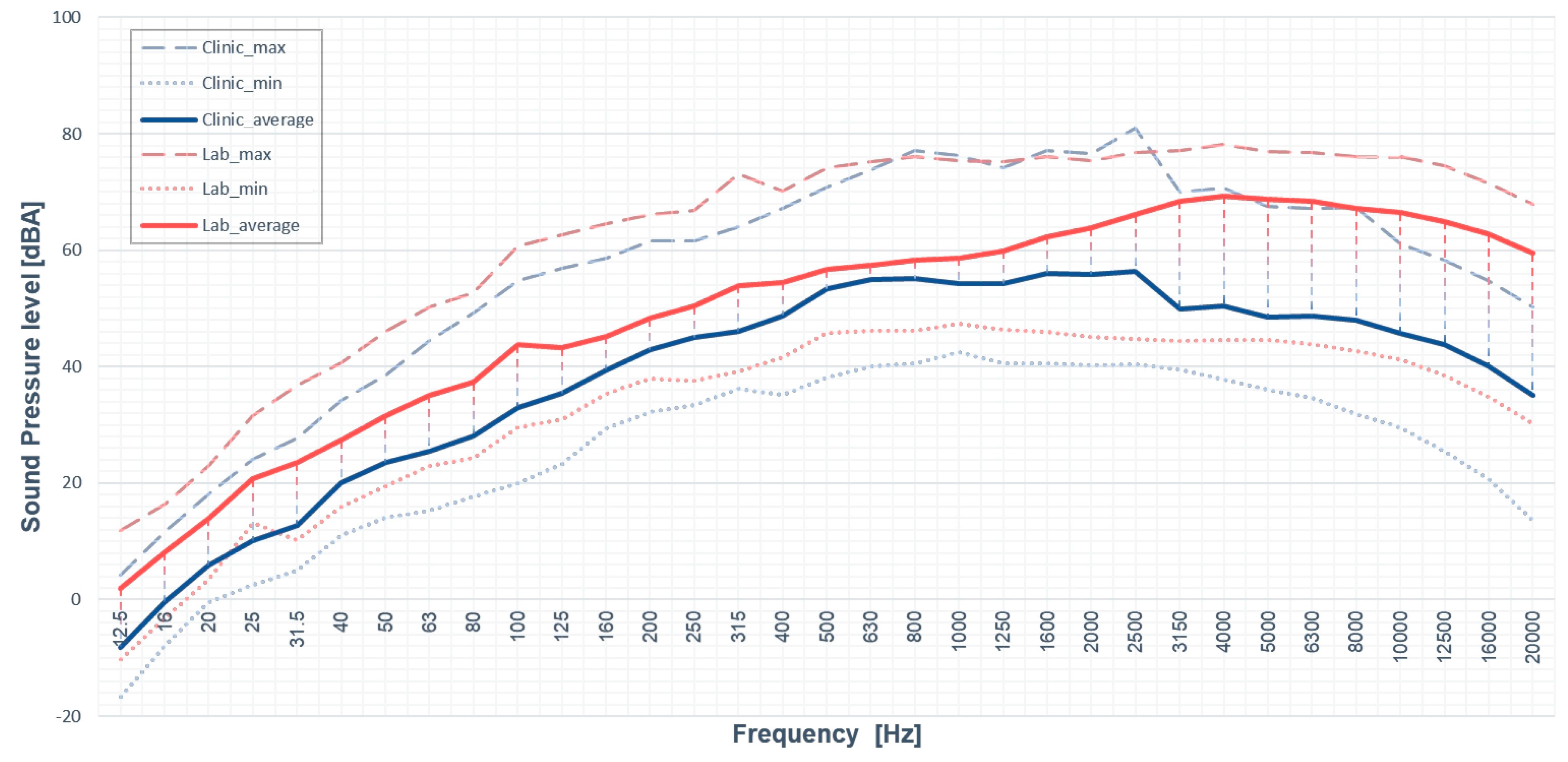
3.1.1. A-Weight SPL Measurement
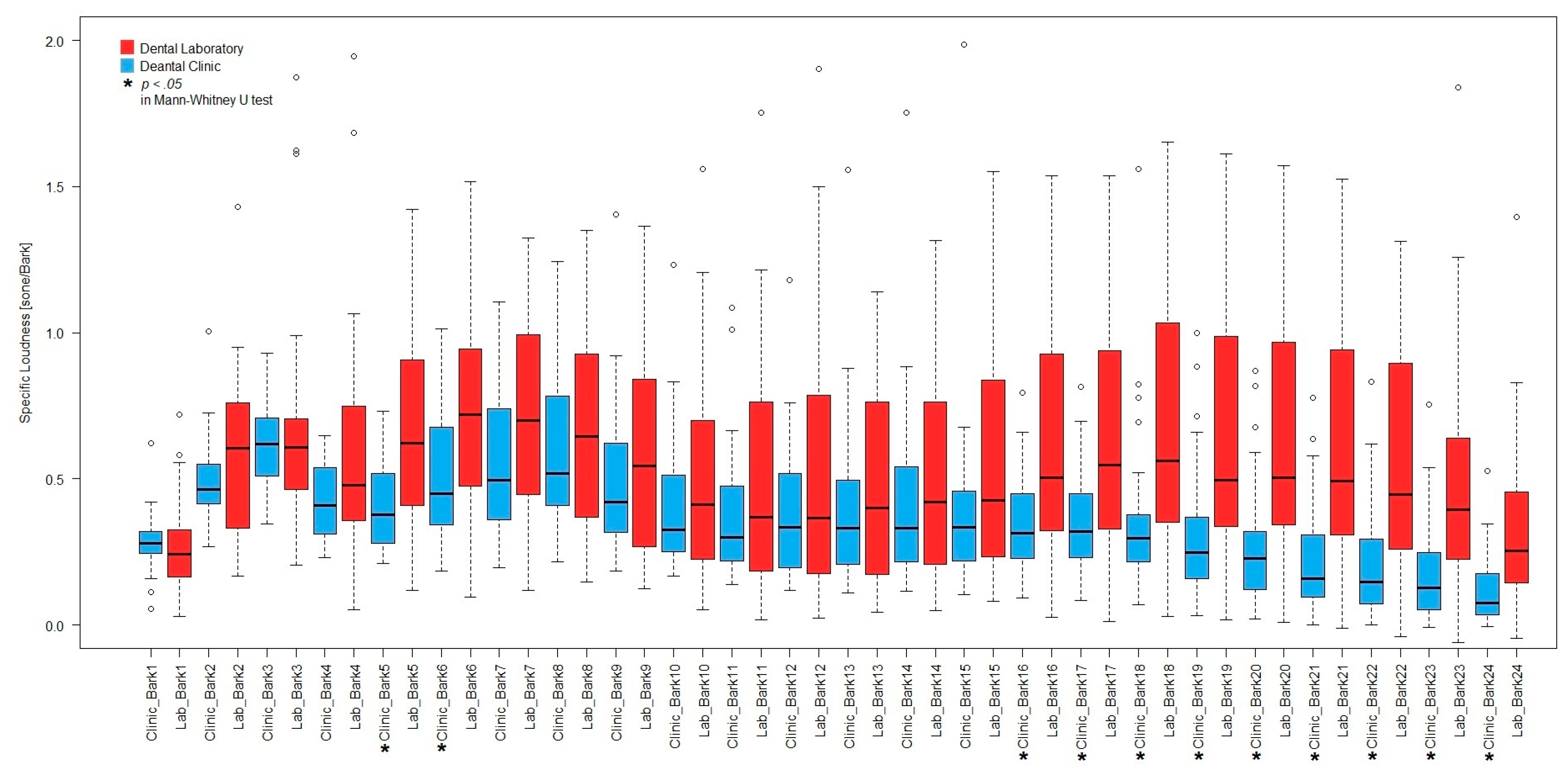
3.1.2. Psychoacoustics Metrics Calculation
3.2. Health Risk Model Construction
3.2.1. Demography Information
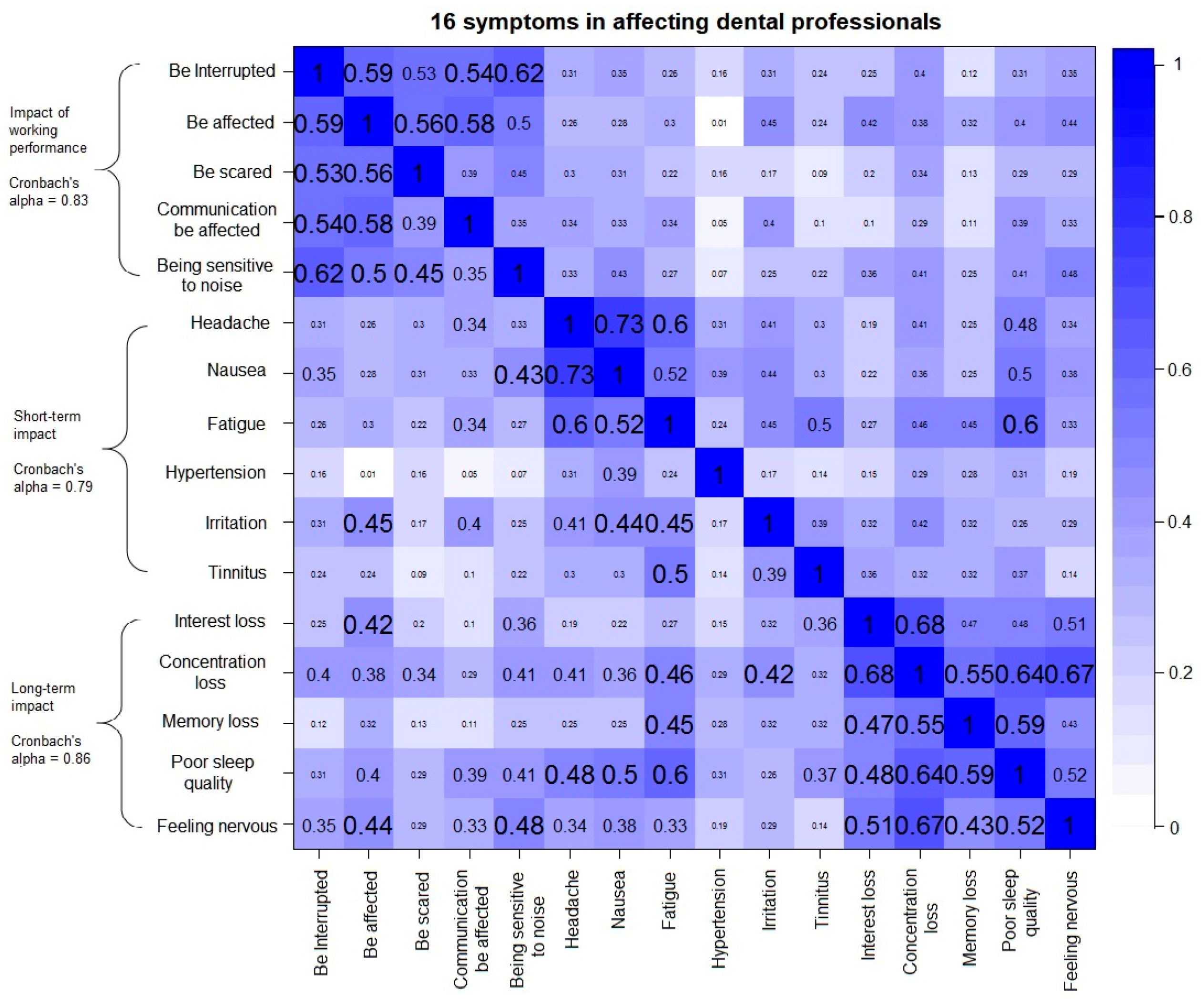
3.2.2. Reliability of the Latent Variables
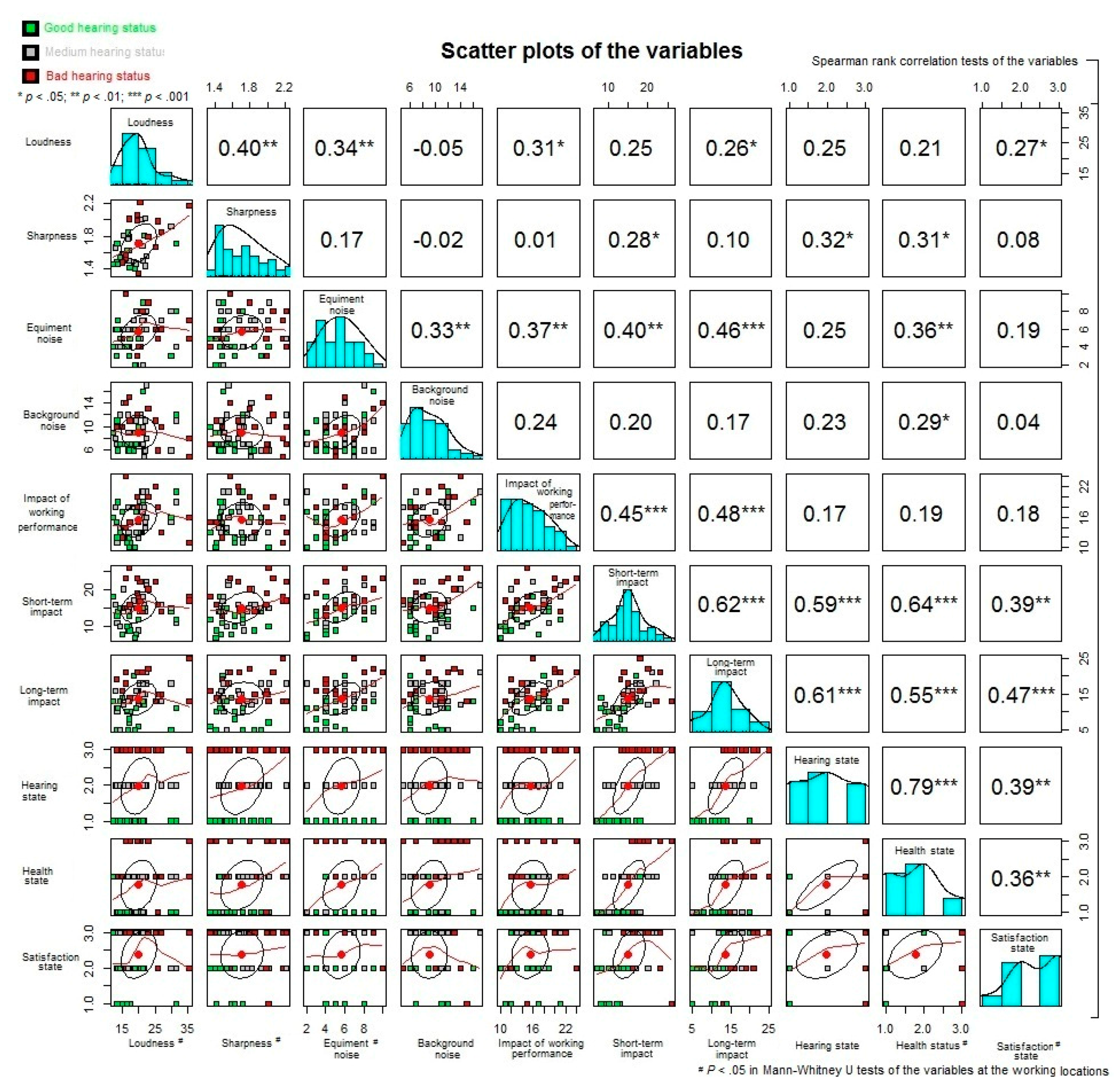
3.2.3. Bivariate Correlation Tests
3.2.4. The Effects of the Environmental Changes to the Negative Impacts
3.2.5. The Effect of the Negative Impacts to the States of Satisfaction, Hearing, and Health
4. Discussion
5. Insights and Limitations
6. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A. Equations of the Psychoacoustics Metrics
References
- World Health Organization. Environmental Burden of Disease Series, No. 9. In Occupational Noise: Assessing the Burden of Disease from Work-Related Hearing Impairment at National and Local Levels; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- Goelzer, B.; Hansen, C.H.; Sehrndt, G. Occupational Exposure to Noise: Evaluation, Prevention and Control; World Health Organisation: Geneva, Switzerland, 2001. [Google Scholar]
- World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Life; 9241562072; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- Mak, C.M.; Lui, Y.P. The effect of sound on office productivity. Build. Serv. Eng. Res. Technol. 2012, 33, 339–345. [Google Scholar] [CrossRef]
- Tzivian, L.; Winkler, A.; Dlugaj, M.; Schikowski, T.; Vossoughi, M.; Fuks, K.; Weinmayr, G.; Hoffmann, B. Effect of long-term outdoor air pollution and noise on cognitive and psychological functions in adults. Int. J. Hyg. Environ. Health 2015, 218, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Franssen, E.; Van Wiechen, C.; Nagelkerke, N.; Lebret, E. Aircraft noise around a large international airport and its impact on general health and medication use. Occup. Environ. Med. 2004, 61, 405–413. [Google Scholar] [CrossRef] [PubMed]
- Huss, A.; Küchenhoff, J.; Bircher, A.; Heller, P.; Kuster, H.; Niederer, M.; Scartazzini, G.; Schwarzenbach, S.; Waeber, R.; Wegmann, L. Symptoms attributed to the environment–a systematic, interdisciplinary assessment. Int. J. Hyg. Environ. Health 2004, 207, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, T.; Osada, Y.; Kawaguchi, T.; Hoshiyama, Y.; Yoshida, K.; Yamamoto, K. Effects of road traffic noise on inhabitants of Tokyo. J. Sound Vib. 1997, 205, 517–522. [Google Scholar] [CrossRef]
- Seidler, A.; Wagner, M.; Schubert, M.; Dröge, P.; Römer, K.; Pons-Kühnemann, J.; Swart, E.; Zeeb, H.; Hegewald, J. Aircraft, road and railway traffic noise as risk factors for heart failure and hypertensive heart disease—A case-control study based on secondary data. Int. J. Hyg. Environ. Health 2016, 219, 749–758. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, A.; Prasher, D. Tinnitus induced by occupational and leisure noise. Noise Health 2000, 2, 47. [Google Scholar] [PubMed]
- Setcos, J.C.; Mahyuddin, A. Noise levels encountered in dental clinical and laboratory practice. Int. J. Prosthodont. 1998, 11, 150–157. [Google Scholar] [PubMed]
- Messano, G.A.; Petti, S. General dental practitioners and hearing impairment. J. Dent. 2012, 40, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Choosong, T.; Kaimook, W.; Tantisarasart, R.; Sooksamear, P.; Chayaphum, S.; Kongkamol, C.; Srisintorn, W.; Phakthongsuk, P. Noise exposure assessment in a dental school. Saf. Health Work 2011, 2, 348–354. [Google Scholar] [CrossRef] [PubMed]
- Willett, K.M. Noise-induced hearing loss in orthopaedic staff. Bone Joint J. 1991, 73, 113–115. [Google Scholar]
- Jadid, K.; Klein, U.; Meinke, D. Assessment of noise exposures in a pediatric dentistry residency clinic. Pediat. Dent. 2011, 33, 342–347. [Google Scholar]
- Dutta, A.; Mala, K.; Acharya, S.R. Sound levels in conservative dentistry and endodontics clinic. J. Conserv. Dent. JCD 2013, 16, 121. [Google Scholar] [CrossRef] [PubMed]
- Aletta, F.; Botteldooren, D.; Thomas, P.; Vander Mynsbrugge, T.; De Vriendt, P.; Van de Velde, D.; Devos, P. Monitoring sound levels and soundscape quality in the living rooms of nursing homes: A case study in Flanders (Belgium). Appl. Sci. 2017, 7, 874. [Google Scholar] [CrossRef]
- Van den Bosch, K.A. Safe and Sound: Soundscape Research in Special Needs Care; University of Groningen: Groningen, The Netherlands, 2015. [Google Scholar]
- Elmehdi, H.M. Assessing acoustic noise levels in dental clinics and its link to dental anxiety and fear among uae population. Compress. Air 2010, 87, 14. [Google Scholar]
- Wong, H.M.; Mak, C.M.; Xu, Y.F. A four-part setting on examining the anxiety-provoking capacity of the sound of dental equipment. Noise Health 2011, 13, 385. [Google Scholar] [PubMed]
- Wong, H.M.; Mak, C.M.; To, W.M. Development of a dental anxiety provoking scale: A pilot study in hong kong. J. Dent. Sci. 2015, 10, 240–247. [Google Scholar] [CrossRef]
- Ahmed, H.O.; Ali, W.J. Noise levels, noise annoyance, and hearing-related problems in a dental college. Arch. Environ. Occup. Health 2017, 72, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Ai, Z.T.; Mak, C.M.; Wong, H.M. Noise level and its influences on dental professionals in a dental hospital in hong kong. Build. Serv. Eng. Res. Technol. 2017. [Google Scholar] [CrossRef]
- International Organization for Standardization. ISO 226: Acoustics—Normal Equal-Loudness-Level Contours; International Standardization: Geneva, Switzerland, 2003. [Google Scholar]
- Zwicker, E.; Fastl, H. Psychoacoustics: Facts and Models; Springer: Berlin, Germany, 1990; Volume 22. [Google Scholar]
- International Organization for Standardization. ISO 532: Acoustics—Method for Calculating Loudnesslevel; International Standardization: Geneva, Switzerland, 1975. [Google Scholar]
- Aures, W. A model for calculating the sensory euphony of various sounds. Acustica 1985, 59, 130–141. [Google Scholar]
- Brink, M. Parameters of well-being and subjective health and their relationship with residential traffic noise exposure—A representative evaluation in Switzerland. Environ. Int. 2011, 37, 723–733. [Google Scholar] [CrossRef] [PubMed]
- Gliem, J.A.; Gliem, R.R. Calculating, interpreting, and reporting cronbach’s alpha reliability coefficient for likert-type scales, 2003. In Proceedings of the Midwest Research-to-Practice Conference in Adult, Continuing, and Community Education, DeKalb, IL, USA, 9–11 October 2002. [Google Scholar]
- Neuner, R.; Seidel, H.-J. Adaptation of office workers to a new building–impaired well-being as part of the sick-building-syndrome. Int. J. Hyg. Environ. Health 2006, 209, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Willershausen, B.; Callaway, A.; Wolf, T.G.; Ehlers, V.; Scholz, L.; Wolf, D.; Letzel, S. Hearing assessment in dental practitioners and other academic professionals from an urban setting. Head Face Med. 2014, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Mak, C.M.; Wong, H.M. Pollutant dispersion in a natural ventilated dental clinic. Build. Serv. Eng. Res. Technol. 2013, 34, 245–258. [Google Scholar] [CrossRef]
- Mak, C.M.; Wang, Z. Recent advances in building acoustics: An overview of prediction methods and their applications. Build. Environ. 2015, 91, 118–126. [Google Scholar] [CrossRef]
- Mak, C.M.; Au, W.M. A turbulence-based prediction technique for flow-generated noise produced by in-duct elements in a ventilation system. Appl. Acoust. 2009, 70, 11–20. [Google Scholar] [CrossRef]
- To, W.M.; Mak, C.M.; Chung, W.L. Are the noise levels acceptable in a built environment like Hong Kong? Noise Health 2015, 17, 429. [Google Scholar] [CrossRef] [PubMed]
- Mak, C.M. Development of a prediction method for flow-generated noise produced by duct elements in ventilation systems. Appl. Acoust. 2002, 63, 81–93. [Google Scholar] [CrossRef]
- Mak, C.M.; Yang, J. A prediction method for aerodynamic sound produced by closely spaced elements in air ducts. J. Sound Vib. 2000, 229, 743–753. [Google Scholar] [CrossRef]
| Parts | Questions (Latent Variable) | Number of Questions | Scales |
|---|---|---|---|
| Part I: Demographic information | Gender; Working location; Age range; Service length; Daily Working hours | 5 | Nominal and Ordinal |
| Part II: Degree of dental noise influences | Operated by own; Operated by others (Equipment noise influence) | 2 | Five-point Likert scale |
| Air-conditioning system; Computers; Human voices; Phones; Broadcasting (Background noise influence) | 5 | Five-point Likert scale | |
| Part III: Degree of the negative impacts | Work be interrupted; Work be affected; Be scared by noise, Communication be affected, Being sensitive to noise (Impact of working performance) | 5 | Five-point Likert scale |
| Headache; Nausea; Fatigue; Hypertension; Irritation; Tinnitus (Short-term impact) | 6 | Five-point Likert scale | |
| Interest loss; Concentration loss; Memory loss; Poor sleep quality; Feeling nervous (Long-term impact) | 5 | Five-point Likert scale | |
| Part IV: Health condition | Satisfaction state; hearing state; health state | 3 | Three-point Likert scale |
| Subject Characteristics | Number (n = 60) | Percentage |
|---|---|---|
| Gender | ||
| Male | 19 | 31.7% |
| Female | 41 | 68.3% |
| Working location | ||
| Dental Clinic | 30 | 50.0% |
| Dental laboratory | 30 | 50.0% |
| Age range | ||
| 20–30 years old | 12 | 20.0% |
| 30–40 years old | 6 | 10.0% |
| 40–50 years old | 20 | 33.3% |
| 50–60 years old | 22 | 36.7% |
| Service length | ||
| <10 years | 18 | 30.0% |
| ≥10 years | 42 | 70.0% |
| Daily working hours | ||
| <8 h | 17 | 28.3% |
| ≥8 h | 43 | 71.7% |
| Outcome Variables | Remained Variables | Estimate | Standard Error | p |
|---|---|---|---|---|
| Impact of working performance 1 | Total score of noise influences | 0.34 | 0.10 | 0.002 |
| Short-term impact 2 | Total score of noise influences | 0.43 | 0.12 | <0.001 |
| Sharpness | 4.92 | 1.91 | 0.013 | |
| Long-term impact 3 | Score of equipment noise influence | 1.15 | 0.27 | <0.001 |
| Outcome Variables | Remained Variables | β # (SE) | Odds Ratio (95% CI) | p |
|---|---|---|---|---|
| Satisfaction state | Long-term impact score | 0.20 (0.067) | 1.22 (1.07–1.39) | 0.004 |
| Working location | ||||
| Dental clinic | −1.48 (0.57) | 0.23 (0.075–0.69) | 0.009 | |
| Dental laboratory ^ | ||||
| Hearing state | Short-term impact score | 0.23 (0.099) | 1.26 (1.04–1.53) | 0.006 |
| Long-term impact score | 0.27 (0.096) | 1.31 (1.08–1.58) | 0.021 | |
| Service length (Daily working hour) | ||||
| <10 years (<8 h) | −2.34 (0.94) | 0.10 (0.015–0.61) | 0.013 | |
| <10 years (≥8 h) | −2.80 (0.97) | 0.061 (0.009–0.41) | 0.010 | |
| ≥10 years (<8 h) | −2.47 (0.96) | 0.084 (0.013–0.55) | 0.004 | |
| ≥10 years (≥8 h) ^ | ||||
| Health State | Short-term impact score | 0.30 (0.12) | 1.34 (1.07–1.69) | 0.010 |
| Hearing state | ||||
| Good | −6.59 (1.59) | 0.001 (<0.001–0.031) | <0.001 | |
| Medium | −2.68 (1.15) | 0.068 (0.007–0.65) | 0.019 | |
| Bad ^ |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ma, K.W.; Wong, H.M.; Mak, C.M. Dental Environmental Noise Evaluation and Health Risk Model Construction to Dental Professionals. Int. J. Environ. Res. Public Health 2017, 14, 1084. https://doi.org/10.3390/ijerph14091084
Ma KW, Wong HM, Mak CM. Dental Environmental Noise Evaluation and Health Risk Model Construction to Dental Professionals. International Journal of Environmental Research and Public Health. 2017; 14(9):1084. https://doi.org/10.3390/ijerph14091084
Chicago/Turabian StyleMa, Kuen Wai, Hai Ming Wong, and Cheuk Ming Mak. 2017. "Dental Environmental Noise Evaluation and Health Risk Model Construction to Dental Professionals" International Journal of Environmental Research and Public Health 14, no. 9: 1084. https://doi.org/10.3390/ijerph14091084
APA StyleMa, K. W., Wong, H. M., & Mak, C. M. (2017). Dental Environmental Noise Evaluation and Health Risk Model Construction to Dental Professionals. International Journal of Environmental Research and Public Health, 14(9), 1084. https://doi.org/10.3390/ijerph14091084







