Stress Exposure and Physical, Mental, and Behavioral Health among American Indian Adults with Type 2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Procedure
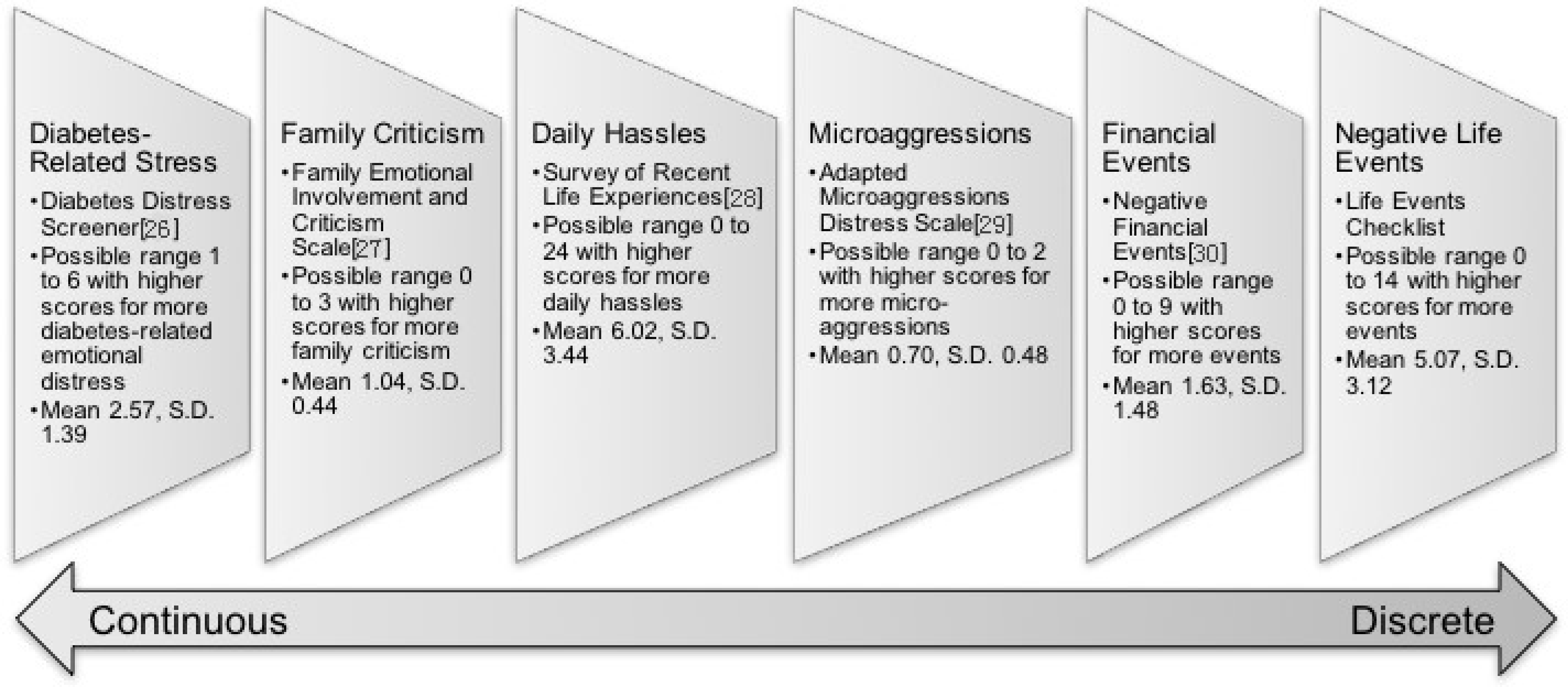
2.3. Measures
2.4. Analytic Approach
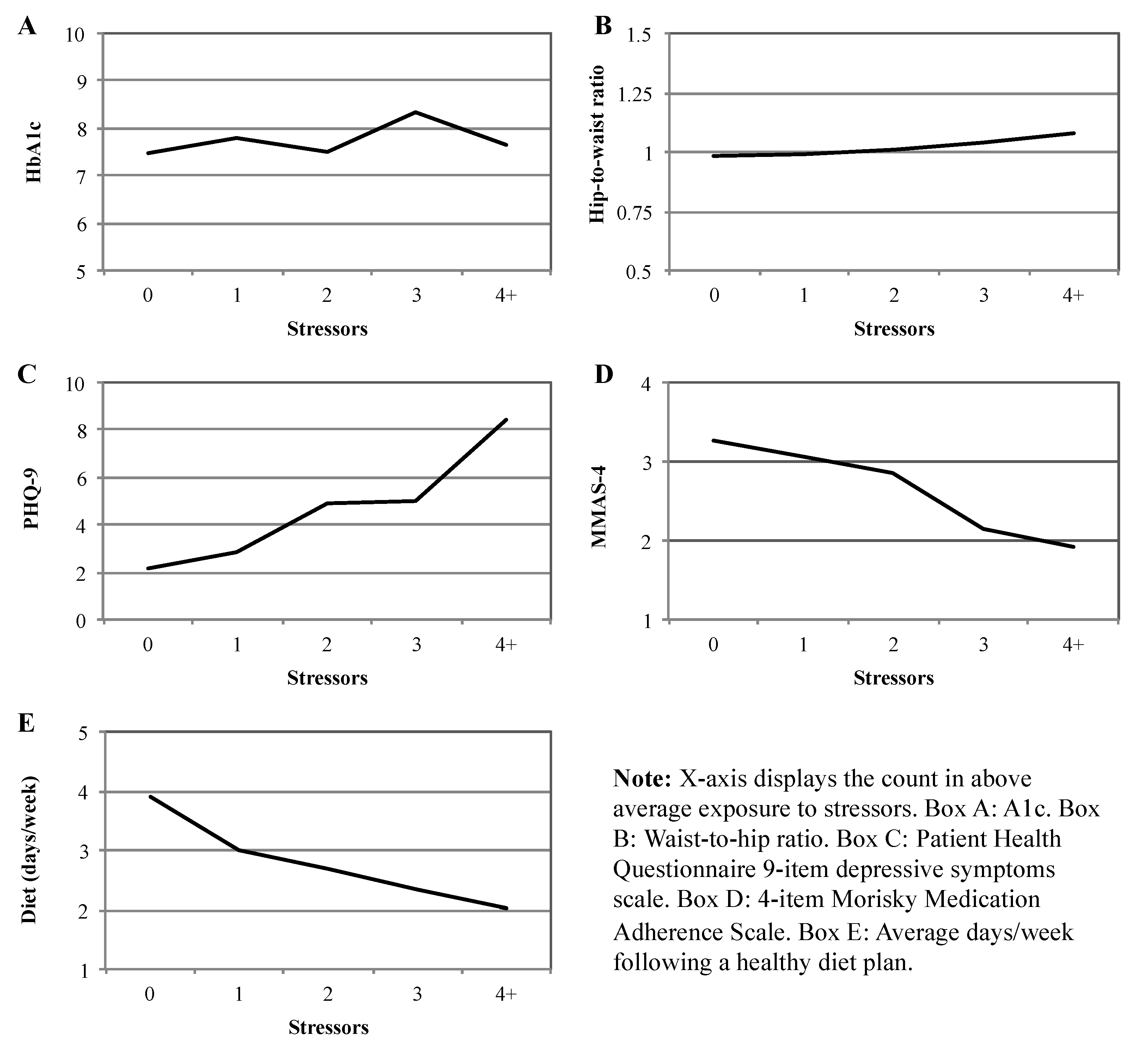
3. Results
4. Discussion
5. Conclusions
Acknowledgements
Author Contributions
Conflicts of Interest
References
- Pearlin, L.I.; Menaghan, E.G.; Lieberman, M.A.; Mullan, J.T. The stress process. J. Health Soc. Behav. 1981, 22, 337–356. [Google Scholar] [CrossRef] [PubMed]
- Walters, K.L.; Simoni, J.M. Reconceptualizing Native women’s health: An “indigenist” stress-coping model. Am. J. Public Health 2002, 92, 520–524. [Google Scholar] [CrossRef] [PubMed]
- Surwit, R.S.; Schneider, M.S.; Feinglos, M.N. Stress and diabetes mellitus. Diabetes Care 1992, 15, 1413–1422. [Google Scholar] [CrossRef] [PubMed]
- Walders, A.N.; Venditti, E.M.; levers-Landis, C.E.; Anderson, B.; Geffner, M.; Kaplan, J.; Koontz, M.B.; Saletsky, R.; Payan, M.; et al. Relationships among stressful life events and physiological markers, treatment adherence, and psychosocial functioning among youth with type 2 diabetes. J. Pediatr. 2014, 165, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Beals, J.; Whitesell, N.R.; Roubideaux, Y.; Manson, S.; The AI-SUPERPFP Team. Stress burden and diabetes in two American Indian reservation communitie. Diabetes Care 2008, 31, 427–429. [Google Scholar]
- Turner, R.J.; Wheaton, B.; Lloyd, D.A. The epidemiology of social stress. Am. Sociol. Rev. 1995, 60, 104–125. [Google Scholar] [CrossRef]
- Tiedt, J.A.; Brown, L.A. Allostatic load: The relationship between chronic stress and diabetes in Native Americans. J. Theory Constr. Test 2014, 18, 22–27. [Google Scholar]
- Xu, J.Q.; Murphy, S.L.; Kochanek, K.D.; Bastian, B.A. Deaths: Final data for 2013. In National Vital Statistics Reports; National Center for Health Statistics: Hyattsville, MD, USA, 2016; Volume 64, p. 2. [Google Scholar]
- O’Connell, J.; Yi, R.; Wilson, C.; Manson, S.M.; Acton, K.J. Racial disparities in health status. Diabetes Care 2010, 33, 1463–1470. [Google Scholar] [CrossRef] [PubMed]
- Lee, E.T.; Lee, V.S.; Kingsley, R.M.; Lu, M.; Russell, D.; Asal, N.R.; Wilkinson, C.P. Bradford, R.H.J. Diabetic retinopathy in Oklahoma Indians with NIDDM: Incidence and risk factors. Diabetes Care 1992, 15, 1620–1627. [Google Scholar] [CrossRef] [PubMed]
- Stahn, R.M.; Gohdes, D.; Valway, S.E. Diabetes and its complications among selected tribes in North Dakota, South Dakota, and Nebraska. Diabetes Care 1993, 16, 244–247. [Google Scholar] [CrossRef] [PubMed]
- Acton, K.J.; Burrows, N.R.; Geiss, L.S.; Thompson, T. Diabetes prevalence among American Indians and Alaska Natives and the overall population—United States, 1994–2002. J. Am. Med. Assoc. 2003, 290, 1571–1573. [Google Scholar]
- Benyshek, D.C.; Martin, J.F.; Johnson, C.S. Reconsideration of the origins of the type 2 diabetes epidemic among Native Americans and the implications for intervention policy. Med. Anthropol. 2001, 20, 25–64. [Google Scholar] [CrossRef] [PubMed]
- Scarton, L.J.; De Groot, M. Emotional and behavioral aspects of diabetes in American Indians/Alaska Natives: A systematic literature review. Health Educ. Behav. 2016, 44, 70–82. [Google Scholar] [CrossRef] [PubMed]
- Holmes, T.H.; Rahe, R.H. The social readjustment rating scale. J. Psychosom. Res. 1967, 11, 213–218. [Google Scholar] [CrossRef]
- Wheaton, B. Sampling the stress universe. In Stress and Mental Health; Springer: Berlin, Germany, 1994; pp. 77–114. [Google Scholar]
- Wheaton, B. Social Stress. In A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems; Cambridge University Press: Cambridge, UK, 1999; pp. 171–199. [Google Scholar]
- Turner, R.J.; Avison, W. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. J. Health Soc. Behav. 2003, 488–505. [Google Scholar] [CrossRef]
- Turner, J. Advances in the conceptualization of the stress process. In Understanding Health Disparities: The Promise of the Stress Process Model; Springer Science Business Media: Berlin, Germany, 2009; pp. 3–21. [Google Scholar]
- Elm, J.; Walls, M.; Aronson, B. Sources of stress among Midwest American Indians adults with type two diabetes. 2017. under review. [Google Scholar]
- De Koning, L.; Merchant, A.T.; Pogue, J.; Anand, S.S. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: Meta-regression analysis of prospective studies. Eur. Heart J. 2007, 28, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Patient health questionnaire primary care study group validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. J. Am. Med. Assoc. 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and predictive validity of a self-reported measure of medication adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Toobert, D.J.; Glasgow, R.E. Assessing diabetes self-management: The summary of diabetes self-care activities questionnaire. In Handbook of Psychology and Diabetes; Harwood Academic: Chur, Switzerland, 1994; pp. 351–371. [Google Scholar]
- Toobert, D.J.; Hampson, S.E.; Glasgow, R.E. The summary of diabetes self-care activities measure: Results from 7 studies and a revised scale. Diabetes Care 2000, 23, 943–950. [Google Scholar] [CrossRef] [PubMed]
- Fisher, L.; Glasgow, R.E.; Mullan, J.T.; Skaff, M.M.; Polonsky, W.H. Development of a brief diabetes distress screening instrument. Ann. Fam. Med. 2008, 6, 246–252. [Google Scholar] [CrossRef] [PubMed]
- Shields, C.G.; Franks, P.; Harp, J.J.; Campbell, T.L.; McDaniel, S.H. Family emotional involvement and criticism scale (FEICS): II reliability and validity studies. Fam. Syst. Med. 1994, 12, 361–377. [Google Scholar] [CrossRef]
- Kohn, P.M.; Macdonald, J.E. The survey of recent life experiences: A decontaminated hassles scale for adults. J. Behav. Med. 1992, 15, 221–236. [Google Scholar] [CrossRef] [PubMed]
- Chae, D.H.; Walters, K.L. Racial discrimination and racial identity attitudes in relation to self-rated health and physical pain and impairment among two-spirit American Indians/Alaska Natives. Am. J. Public Health 2009, 99, S144–S151. [Google Scholar] [CrossRef] [PubMed]
- Dohrenwend, B.S.; Askenasy, A.R.; Krasnoff, L.; Dohrenwend, B.P. Exemplification of a method for scaling life events: The PERI life events scale. J. Health Soc. Behav. 1978, 19, 205–229. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, J.S.; Peyrot, M.; McCarl, L.A.; Collins, E.M.; Serpa, L.; Mimiaga, M.J.; Safren, S.A. Depression and diabetes treatment nonadherence: A meta-analysis. Diabetes Care 2008, 31, 2398–2403. [Google Scholar] [CrossRef] [PubMed]
- Egede, L.E.; Gebregziabher, M.; Echols, C.; Lynch, C.P. Longitudinal effects of medication nonadherence on glycemic control. Ann. Pharmacother. 2014, 48, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Aikens, J.E. Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care 2012, 35, 2472–2478. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Berglund, P.; Demler, O.; Jin, R.; Merikangas, K.R.; Walters, E.E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 593–602. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Chiu, W.T.; Demler, O.; Walters, E.E. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch. Gen. Psychiatry 2005, 62, 617–627. [Google Scholar] [CrossRef] [PubMed]
- Sue, D.W.; Capodilupo, C.M.; Torino, G.C.; Bucceri, J.M.; Holder, A.; Nadal, K.L.; Esquilin, M. Racial microaggressions in everyday life: Implications for clinical practice. Am. Psychol. 2007, 62, 271–286. [Google Scholar] [CrossRef] [PubMed]
- Hill, D. Sense of belonging as connectedness, American Indian worldview, and mental health. Arch Psychiatr. Nurs. 2006, 20, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Fisher, L.; Gonzalez, J.S.; Polonsky, W.H. The confusing tale of depression and distress in patients with diabetes: A call for greater clarity and precision. Diabet. Med. 2014, 31, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Fisher, L.; Mullan, J.T.; Arean, P.; Glasgow, R.E.; Hessler, D.; Masharani, U. Diabetes distress but not clinical depression or depressive symptoms is associated with glycemic control in both cross-sectional and longitudinal analyses. Diabetes Care 2010, 33, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Kahn, J.R.; Pearlin, L.I. Financial strain over the life course and health among older adults. J. Health Soc. Behav. 2006, 47, 17–31. [Google Scholar] [CrossRef] [PubMed]
- Pearlin, L.I.; Aneshensel, C.S.; Lablanc, A.J. The forms and mechanisms of stress proliferation: The case of AIDS caregivers. J. Health Soc. Behav. 1997, 38, 223–236. [Google Scholar] [CrossRef] [PubMed]
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Diabetes Distress | 1 | ||||||||||
| 2. Family Criticism | 0.11 | ||||||||||
| 3. Daily Hassles | 0.44 *** | 0.23 ** | 1 | ||||||||
| 4. Microaggressions | 0.22 ** | 0.01 | 0.14 * | 1 | |||||||
| 5. Financial Events | 0.15 * | 0.12 | 0.17 * | 0.21 ** | 1 | ||||||
| 6. Negative Life Events | 0.16 * | 0.06 | 0.13 | 0.43 *** | 0.38 *** | 1 | |||||
| 7. HbA1c | 0.18 * | 0.12 | 0.04 | −0.04 | −0.04 | −0.03 | 1 | ||||
| 8. Waist-to-Hip Ratio | 0.12 | 0.08 | 0.07 | 0.09 | 0.21 ** | 0.15 * | −0.04 | 1 | |||
| 9. Depressive Symptoms | 0.20 ** | 0.28 *** | 0.26 *** | 0.27 *** | 0.20 ** | 0.22 ** | 0.03 | −0.01 | 1 | ||
| 10. Medication Adherence | −0.31 *** | −0.16 * | −0.30 *** | −0.14 | −0.22 ** | −0.18 * | −0.04 | −0.01 | −0.29 *** | 1 | |
| 11. Adherence to Diet Plan | −0.25 *** | −0.20 ** | −0.23 *** | −0.03 | −0.27 *** | −0.13 | −0.08 | −0.12 | −0.24 *** | 0.34 *** | 1 |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HbA1c | Waist-to-Hip Ratio | Depressive Symptoms | Medication Adherence | Adherence to Diet Plan | |||||||||||
| B | β | p Value | B | β | p value | B | β | p Value | B | β | p Value | B | β | p Value | |
| (SD) | (SD) | (SD) | (SD) | (SD) | |||||||||||
| (Constant) | 9.23 | 0.00 | 0.96 | 0.00 | −0.71 | 0.73 | 2.73 | 0.00 | 2.88 | 0.00 | |||||
| Age (years) | −0.04 | −0.21 | 0.01 | −0.00 | −0.05 | 0.50 | −0.03 | −0.07 | 0.29 | 0.02 | 0.24 | 0.00 | 0.02 | 0.18 | 0.01 |
| (0.01) | (0.00) | (0.03) | (0.01) | (0.01) | |||||||||||
| Gender (Female = 1) | −0.52 | −0.12 | 0.12 | −0.08 | −0.14 | 0.07 | 2.26 | 0.20 | 0.00 | −0.31 | −0.12 | 0.10 | 0.32 | 0.10 | 0.16 |
| (0.33) | (0.04) | (0.77) | (0.18) | (0.22) | |||||||||||
| Household Income | −0.02 | −0.06 | 0.40 | 0.00 | 0.04 | 0.65 | −0.06 | −0.09 | 0.18 | 0.01 | 0.04 | 0.62 | 0.02 | 0.12 | 0.10 |
| (0.02) | (0.00) | (0.04) | (0.01) | (0.01) | |||||||||||
| Diabetes Distress | 0.36 | 0.22 | 0.01 | 0.02 | 0.11 | 0.21 | 0.00 | 0.00 | 1.00 | −0.14 | −0.15 | 0.08 | −0.19 | −0.16 | 0.03 |
| (0.13) | (0.02) | (0.03) | (0.08) | (0.09) | |||||||||||
| Family Criticism | 0.45 | 0.09 | 0.23 | 0.02 | 0.03 | 0.68 | 3.07 | 0.24 | 0.00 | −0.22 | −0.08 | 0.28 | −0.40 | −0.11 | 0.11 |
| (0.37) | (0.05) | (0.86) | (0.20) | (0.25) | |||||||||||
| Daily Hassles | −0.02 | −0.04 | 0.65 | 0.00 | 0.02 | 0.85 | 0.17 | 0.10 | 0.17 | −0.05 | −0.14 | 0.09 | −0.06 | −0.12 | 0.12 |
| (0.05) | (0.01) | (0.12) | (0.03) | (0.04) | |||||||||||
| Microaggressions | −0.22 | −0.05 | 0.55 | 0.00 | 0.00 | 1.00 | 2.62 | 0.23 | 0.00 | −0.09 | −0.04 | 0.65 | 0.20 | 0.06 | 0.42 |
| (0.37) | (0.05) | (0.87) | (0.21) | (0.25) | |||||||||||
| Financial Events | −0.16 | −0.11 | 0.18 | 0.03 | 0.15 | 0.07 | 0.20 | 0.05 | 0.48 | −0.06 | −0.07 | 0.36 | −0.18 | −0.17 | 0.03 |
| (0.12) | (0.02) | (0.28) | (0.07) | (0.08) | |||||||||||
| Negative Life Events | −0.01 | −0.02 | 0.83 | 0.01 | 0.06 | 0.46 | 0.12 | 0.07 | 0.39 | −0.03 | −0.07 | 0.38 | 0.00 | −0.01 | 0.92 |
| (0.06) | (0.01) | (0.14) | (0.03) | (0.04) | |||||||||||
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walls, M.L.; Sittner, K.J.; Aronson, B.D.; Forsberg, A.K.; Whitbeck, L.B.; Al’Absi, M. Stress Exposure and Physical, Mental, and Behavioral Health among American Indian Adults with Type 2 Diabetes. Int. J. Environ. Res. Public Health 2017, 14, 1074. https://doi.org/10.3390/ijerph14091074
Walls ML, Sittner KJ, Aronson BD, Forsberg AK, Whitbeck LB, Al’Absi M. Stress Exposure and Physical, Mental, and Behavioral Health among American Indian Adults with Type 2 Diabetes. International Journal of Environmental Research and Public Health. 2017; 14(9):1074. https://doi.org/10.3390/ijerph14091074
Chicago/Turabian StyleWalls, Melissa L., Kelley J. Sittner, Benjamin D. Aronson, Angie K. Forsberg, Les B. Whitbeck, and Mustafa Al’Absi. 2017. "Stress Exposure and Physical, Mental, and Behavioral Health among American Indian Adults with Type 2 Diabetes" International Journal of Environmental Research and Public Health 14, no. 9: 1074. https://doi.org/10.3390/ijerph14091074
APA StyleWalls, M. L., Sittner, K. J., Aronson, B. D., Forsberg, A. K., Whitbeck, L. B., & Al’Absi, M. (2017). Stress Exposure and Physical, Mental, and Behavioral Health among American Indian Adults with Type 2 Diabetes. International Journal of Environmental Research and Public Health, 14(9), 1074. https://doi.org/10.3390/ijerph14091074





