Maternal Mental Health Disorders and Reports to Child Protective Services: A Birth Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data Sources
2.2. Variables
2.2.1. Dependent Variable
2.2.2. Independent Variables
2.2.3. Covariates
2.3. Analysis
3. Results
3.1. Characteristics of Births with a Maternal Mental Health Disorder
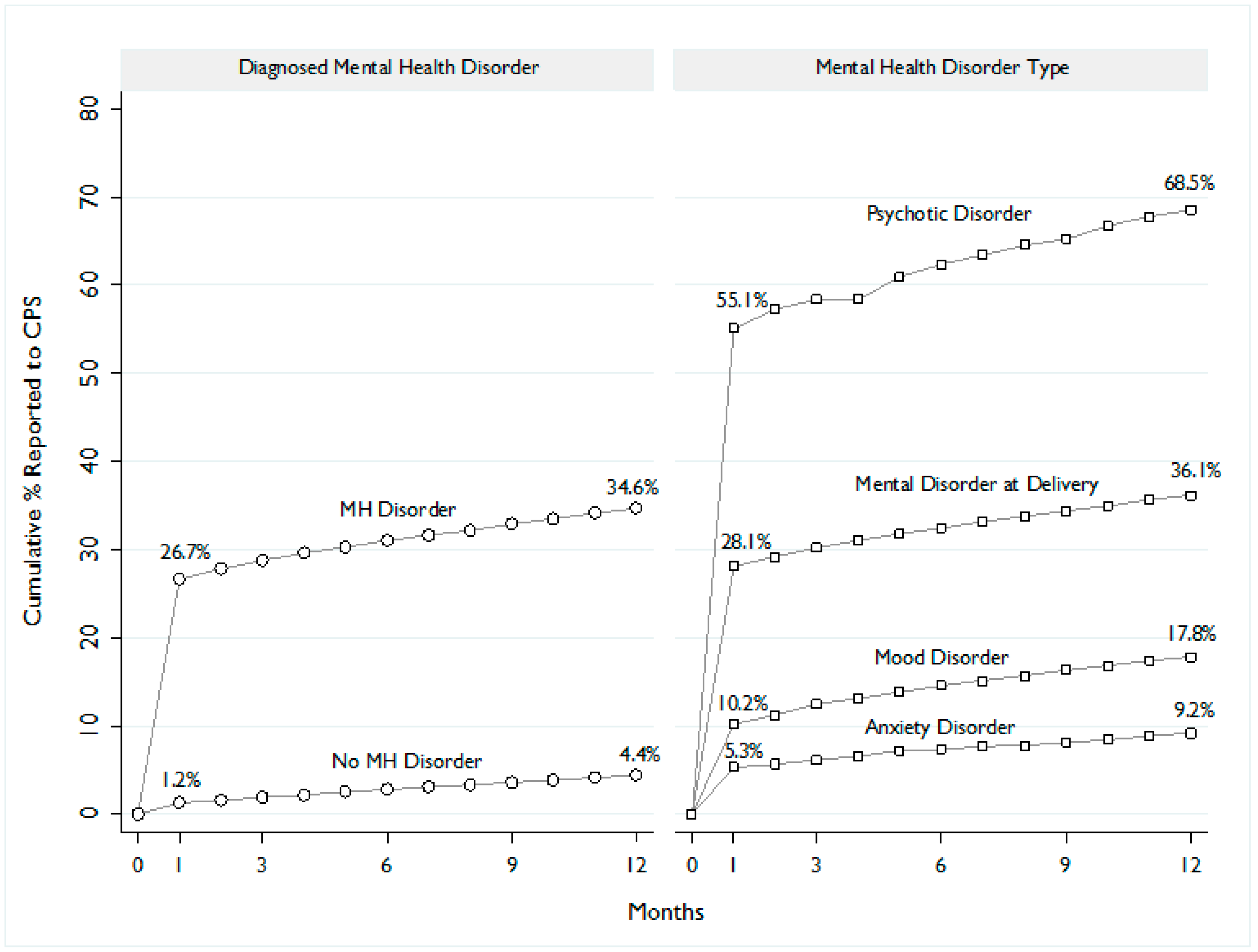
3.2. Maltreatment Reports to Child Protective Services
3.3. Association between Maternal Mental Health Disorders and Maltreatment Reporting
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
Appendix A
| Mental Health Disorders | Clinical Classification Software # | ICD-9-CM Codes |
|---|---|---|
| Psychotic Disorders | 659 | 29381 29382 29500 29501 29502 29503 29504 29505 29510 29511 29512 29513 29514 29515 29520 29521 29522 29523 29524 29525 29530 29531 29532 29533 29534 29535 29540 29541 29542 29543 29544 29545 29550 29551 29552 29553 29554 29555 29560 29561 29562 29563 29564 29565 29570 29571 29572 29573 29574 29575 29580 29581 29582 29583 29584 29585 29590 29591 29592 29593 29594 29595 2970 2971 2972 2973 2978 2979 2980 2981 2982 2983 2984 2988 2989 |
| Mood Disorders | 657 | 29383 29600 29601 29602 29603 29604 29605 29606 29610 29611 29612 29613 29614 29615 29616 29620 29621 29622 29623 29624 29625 29626 29630 29631 29632 29633 29634 29635 29636 29640 29641 29642 29643 29644 29645 29646 29650 29651 29652 29653 29654 29655 29656 29660 29661 29662 29663 29664 29665 29666 2967 29680 29681 29682 29689 29690 29699 3004 |
| Anxiety Disorders | 651 | 29384 30000 30001 30002 30009 30010 30020 30021 30022 30023 30029 3003 3005 30089 3009 3080 3081 3082 3083 3084 3089 30981 3130 3131 31321 31322 |
| Mental Disorders at Delivery | 648 | 64841 64842 |
| Other Mental Health Disorders | ||
| Adjustment Disorders | 650 | 3090 3091 30922 30923 30924 30928 30929 3093 3094 30982 30983 30989 3099 |
| Attention Deficit, Conduct, and Disruptive Behavior Disorders | 652 | 31200 31201 31202 31203 31210 31211 31212 31213 31220 31221 31222 31223 3124 31281 31282 31289 3129 31381 31400 31401 3141 3142 3148 3149 |
| Delirium, Dementia, and other Cognitive Disorders | 653 | 2900 29010 29011 29012 29013 29020 29021 2903 29040 29041 29042 29043 2908 2909 2930 2931 2940 2941 29410 29411 29420 29421 2948 2949 3100 |
| Developmental Disorders | 654 | 3070 3079 31500 31501 31502 31509 3151 3152 31531 31532 31534 31535 31539 3154 3155 3158 3159 317 3180 3181 3182 319 V400 V401 |
| Impulse Control Disorders | 656 | 31230 31231 31232 31233 31234 31235 31239 |
| Personality Disorders | 658 | 3010 30110 30111 30112 30113 30120 30121 30122 3013 3014 30150 30151 30159 3016 3017 30181 30182 30183 30184 30189 3019 |
| Miscellaneous Disorders | 670 | 29389 2939 30011 30012 30013 30014 30015 30016 30019 3006 3007 30081 30082 3021 3022 3023 3024 30250 30251 30252 30253 3026 30270 30271 30272 30273 30274 30275 30276 30279 30281 30282 30283 30284 30285 30289 3029 3060 3061 3062 3063 3064 30650 30651 30652 30653 30659 3066 3067 3068 3069 3071 30740 30741 30742 30743 30744 30745 30746 30747 30748 30749 30750 30751 30752 30753 30754 30759 30780 30781 30789 3101 316 64840 64841 64842 64843 64844 V402 V4031 V4039 V409 V673 |
| Alcohol-related Substance Use Disorders | 660 | 2910 2911 2912 2913 2914 2915 29181 29182 29189 2919 30300 30301 30302 30303 30390 30391 30392 30393 30500 76071 9800 |
| Drug-related Substance Use Disorders | 661 | 2920 29211 29212 2922 29281 29282 29283 29284 29285 29289 2929 30400 30401 30402 30403 30410 30411 30412 30413 30420 30421 30422 30423 30430 30431 30432 30433 30440 30441 30442 30443 30450 30451 30452 30453 30460 30461 30462 30463 30470 30471 30472 30473 30480 30481 30482 30483 30490 30491 30492 30493 30520 30521 30522 30523 30530 30531 30532 30533 30540 30541 30542 30543 30550 30551 30552 30553 30560 30561 30562 30563 30570 30571 30572 30573 30580 30581 30582 30583 30590 30591 30592 30593 64830 64831 64832 64833 64834 65550 65551 65553 76072 76073 76075 7795 7795 96500 96501 96502 96509 V6542 |
References
- Foster, K.; O’Brien, L.; Korhonen, T. Developing resilient children and families when parents have mental illness: A family focused approach. Int. J. Ment. Health Nurs. 2012, 21, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Jablensky, A.V.; Morgan, V.; Zubrick, S.R.; Bower, C.; Yellachich, L.A. Pregnancy, delivery, and neonatal complications in a population cohort of women with schizophrenia and major affective disorders. Am. J. Psychiatry 2005, 162, 79–91. [Google Scholar] [CrossRef] [PubMed]
- Hoirisch-Clapauch, S.; Brenner, B.; Nardi, A.E. Adverse obstetric and neonatal outcomes in women with mental disorders. Thromb. Res. 2015, 135, S60–S63. [Google Scholar] [CrossRef]
- Accortt, E.E.; Cheadle, A.C.; Schetter, C.D. Prenatal depression and adverse birth outcomes: An updated systematic review. Matern. Child Health J. 2015, 19, 1306–1337. [Google Scholar] [CrossRef] [PubMed]
- Bodén, R.; Lundgren, M.; Brandt, L.; Reutfors, J.; Andersen, M.; Kieler, H. Risks of adverse pregnancy and birth outcomes in women treated or not treated with mood stabilisers for bipolar disorder: Population based cohort study. BMJ 2012, 345, e7085. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.C.; Lin, H.C. Maternal bipolar disorder increased low birthweight and preterm births: A nationwide population-based study. J. Affect. Disord. 2010, 121, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Dietz, P.M.; Williams, S.B.; Callaghan, W.M.; Bachman, D.J.; Whitlock, E.P.; Hornbrook, M.C. Clinically identified maternal depression before, during, and after pregnancies ending in live births. Am. J. Psychiatry 2007, 164, 1515–1520. [Google Scholar] [CrossRef] [PubMed]
- Brockington, I.A.; Chandra, P.; Dubowitz, H.; Jones, D.; Moussa, S.; Nakku, J.; Ferre, I.Q. WPA guidance on the protection and promotion of mental health in children of persons with severe mental disorders. World Psychiatry 2011, 10, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Lewin, L.; Abdrbo, A. Mothers with self-reported Axis I diagnoses and child protection. Arch. Psychiatr. Nurs. 2009, 23, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Mullick, M.; Miller, L.J.; Jacobsen, T. Insight into mental illness and child maltreatment risk among mothers with major psychiatric disorders. Psychiatr. Serv. 2001, 52, 488–492. [Google Scholar] [CrossRef] [PubMed]
- Brady, K.T.; Sinha, R. Co-occurring mental and substance use disorders: The neurobiological effects of chronic stress. Am. J. Psychiatry 2005, 162, 1483–1493. [Google Scholar] [CrossRef] [PubMed]
- Kohl, P.L.; Jonson-Reid, M.; Drake, B. Maternal mental illness and the safety and stability of maltreated children. Child Abuse Negl. 2011, 35, 309–318. [Google Scholar] [CrossRef] [PubMed]
- Ackerson, B.J. Parents with serious and persistent mental illness: Issues in assessment and services. Soc. Work 2003, 48, 187–194. [Google Scholar] [CrossRef] [PubMed]
- Conroy, S.; Marks, M.N.; Schacht, R.; Davies, H.A.; Moran, P. The impact of maternal depression and personality disorder on early infant care. Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Park, J.M.; Solomon, P.; Mandell, D.S. Involvement in the child welfare system among mothers with serious mental illness. Psychiatr. Serv. 2006, 57, 493–497. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.H.; Zatzick, D.F.; Anders, T.F. The detection and treatment of psychiatric disorders and substance use among pregnant women cared for in obstetrics. Am. J. Psychiatry 2001, 158, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Kelly, R.H.; Danielsen, B.H.; Golding, J.M.; Anders, T.F.; Gilbert, W.M.; Zatzick, D.F. Adequacy of prenatal care among women with psychiatric diagnoses giving birth in California in 1994 and 1995. Psychiatr. Serv. 1999, 50, 1584–1590. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, M.; Maclean, M.J.; Sims, S.; Morgan, V.A.; Leonard, H.; Stanley, F.J. Maternal mental health and risk of child protection involvement: Mental health diagnoses associated with increased risk. J. Epidemiol. Community Health 2015, 69, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Herrchen, B.; Gould, J.B.; Nesbitt, T.S. Vital statistics linked birth/infant death and hospital discharge record linkage for epidemiological studies. Comput. Biomed. Res. 1997, 30, 290–305. [Google Scholar] [CrossRef] [PubMed]
- Prindle, J.J.; Hammond, I.; Putnam-Hornstein, E. Prenatal Substance Exposure Diagnosed at Birth and Infant Involvement with Child Protective Services. Child Abuse Negl. 2017, in press. [Google Scholar] [CrossRef] [PubMed]
- Kohl, P.L.; Jonson-Reid, M.; Drake, B. Time to leave substantiation behind: Findings from a national probability study. Child Maltreat. 2009, 14, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Hussey, J.M.; Marshall, J.M.; English, D.J.; Knight, E.D.; Lau, A.S.; Dubowitz, H.; Kotch, J.B. Defining maltreatment according to substantiation: Distinction without a difference? Child Abuse Negl. 2005, 29, 479–492. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Diseases: Manual of the International Classification of Diseases, Injuries, and Causes of Death; 9th rev.; World Health Organization: Geneva, Switzerland, 1977; Volumes I and II. [Google Scholar]
- Da Silva, A.A.; Simões, V.M.; Barbieri, M.A.; Bettiol, H.; Lamy-Filho, F.; Coimbra, L.C.; Alves, M.T. Young maternal age and preterm birth. Paediatr. Perinat. Epidemiol. 2003, 17, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Fall, C.H.; Sachdev, H.S.; Osmond, C.; Restrepo-Mendez, M.C.; Victora, C.; Martorell, R.; Stein, A.D.; Sinha, S.; Tandon, N.; Adair, L.; et al. Association between maternal age at childbirth and child and adult outcomes in the offspring: A prospective study in five low-income and middle-income countries (COHORTS collaboration). Lancet Glob. Health 2015, 3, e366–e377. [Google Scholar] [CrossRef]
- McCullagh, P.; Nelder, J.A. Generalized Linear Models, 2nd ed.; Chapman & Hall/CRC: London, UK, 1989. [Google Scholar]
- UCLA. Academic Technology Services: Statistical Consulting Group. Stata FAQ: How Can I Estimate Relative Risk Using GLM for Common Outcomes in Cohort Studies? Available online: http://www.ats.ucla.edu/stat/ stata/ado/analysis/ (accessed on 4 April 2010).
- Johnson, W. Effectiveness of California’s Child Welfare Structured Decision Making (SDM) Model: A Prospective Study of the Validity of the California Family Risk Assessment; Children’s Research Center: Madison, WI, USA, 2004. [Google Scholar]
- Walsh, C.; MacMillan, H.; Jamieson, E. The relationship between parental psychiatric disorder and child physical and sexual abuse: Findings from the Ontario Health Supplement. Child Abuse Negl. 2002, 26, 11–22. [Google Scholar] [CrossRef]
- O’Donnell, M.; Nassar, N.; Leonard, H.; Hagan, R.; Mathews, R.; Patterson, Y.; Stanley, F. Increasing prevalence of neonatal withdrawal syndrome: Population study of maternal factors and child protection involvement. Pediatrics 2009, 123, e614–e621. [Google Scholar] [CrossRef] [PubMed]
- Drake, B.; Jonson-Reid, M. Some thoughts on the increasing use of administrative data in child maltreatment research. Child Maltreat. 1999, 4, 308–315. [Google Scholar] [CrossRef]
| Variable | No Mental Health Disorder | Any Mental Health Disorder | χ2 | Psychotic Disorders | Mood Disorders | Anxiety Disorders | MH Disorder at Delivery | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (N = 535,716) | (N = 15,516) | (N = 276) | (N = 5290) | (N = 1623) | (N = 14,508) | ||||||||
| n | % | n | % | p-Value | n | % | n | % | n | % | n | ||
| Age at First Ever Birth | <0.001 | ||||||||||||
| ≤19 years | 106,650 | 19.9 | 3417 | 22 | 43 | 15.6 | 897 | 17.0 | 186 | 11.5 | 3263 | 22.5 | |
| 20–24 years | 125,594 | 23.4 | 3913 | 25.2 | 59 | 21.5 | 1111 | 21.0 | 329 | 20.3 | 3701 | 25.5 | |
| 25–29 years | 130,333 | 24.3 | 3541 | 22.8 | 64 | 23.3 | 1213 | 22.9 | 427 | 26.3 | 3283 | 22.6 | |
| 30+ years | 173,106 | 32.3 | 4633 | 29.9 | 109 | 39.6 | 2068 | 39.1 | 681 | 42.0 | 4249 | 29.3 | |
| Race/Ethnicity | <0.001 | ||||||||||||
| White | 144,609 | 27.0 | 7630 | 49.2 | 107 | 38.8 | 2869 | 54.2 | 878 | 54.1 | 7160 | 49.4 | |
| Black | 29,104 | 5.4 | 1781 | 11.5 | 66 | 23.9 | 383 | 7.2 | 81 | 5.0 | 1715 | 11.8 | |
| Hispanic | 286,036 | 53.4 | 4911 | 31.7 | 69 | 25.0 | 1656 | 31.3 | 522 | 32.2 | 4526 | 31.2 | |
| Other/Missing | 75,967 | 14.2 | 1194 | 7.7 | 34 | 12.3 | 382 | 7.2 | 142 | 8.7 | 1107 | 7.6 | |
| Insurance Type | <0.001 | ||||||||||||
| Private | 276,853 | 51.8 | 6730 | 43.7 | 53 | 19.3 | 3140 | 59.5 | 1137 | 70.1 | 6094 | 42.4 | |
| Public | 257,953 | 48.2 | 8665 | 56.3 | 221 | 80.7 | 2138 | 40.5 | 484 | 29.9 | 8294 | 57.6 | |
| Paternity | <0.001 | ||||||||||||
| Established | 488,910 | 91.3 | 11,251 | 72.5 | 144 | 52.2 | 4393 | 83.0 | 1445 | 89.0 | 10,396 | 71.7 | |
| Missing | 46,806 | 8.7 | 4265 | 27.5 | 132 | 47.8 | 897 | 17.0 | 178 | 11.0 | 4112 | 28.3 | |
| Prenatal Care | <0.001 | ||||||||||||
| 1st Trimester | 459,200 | 85.7 | 10,974 | 70.7 | 185 | 67.0 | 4564 | 86.3 | 1447 | 89.2 | 10,095 | 69.6 | |
| 2nd Trimester | 58,806 | 11.0 | 2722 | 17.5 | 52 | 18.8 | 524 | 9.9 | 134 | 8.3 | 2633 | 18.1 | |
| 3rd Trimester/No Care | 17,710 | 3.3 | 1820 | 11.7 | 39 | 14.1 | 202 | 3.8 | 42 | 2.6 | 1780 | 12.3 | |
| Parity | <0.001 | ||||||||||||
| First Birth | 209,026 | 39.0 | 5474 | 35.3 | 102 | 37.0 | 2037 | 38.5 | 676 | 41.7 | 5029 | 34.7 | |
| Non-First Birth | 326,690 | 61.0 | 10,042 | 64.7 | 174 | 63.0 | 3253 | 61.5 | 947 | 58.3 | 9479 | 65.3 | |
| Substance Abuse | <0.001 | ||||||||||||
| No | 534,132 | 99.7 | 9106 | 58.7 | 209 | 75.7 | 4730 | 89.4 | 1535 | 94.6 | 8128 | 56.0 | |
| Yes | 1584 | 0.3 | 6410 | 41.3 | 67 | 24.3 | 560 | 10.6 | 88 | 5.4 | 6380 | 44.0 | |
| Variable | Model 1 | Model 2 | Model 3 | |||
|---|---|---|---|---|---|---|
| Risk Ratio | (95% CI) | Risk Ratio | (95% CI) | Risk Ratio | (95% CI) | |
| Any Mental Health Disorder | 7.82 | 7.63, 8.02 | 3.53 | 3.37, 3.71 | 2.60 | 2.47, 2.73 |
| Any Mental Health Disorder + Substance | -- | -- | 13.91 | 13.59, 14.23 | 5.69 | 5.51, 5.87 |
| Psychotic Disorder | 13.10 | 12.09, 14.19 | 12.11 | 10.92, 13.42 | 4.60 | 3.96, 5.34 |
| Psychotic Disorder + Substance | -- | -- | 20.97 | 18.10, 24.29 | 5.67 | 4.50, 7.14 |
| Mood Disorder | 3.47 | 3.27, 3.68 | 2.56 | 2.38, 2.76 | 2.22 | 2.07, 2.39 |
| Mood Disorder + Substance | -- | -- | 13.22 | 10.88, 16.07 | 4.61 | 4.18, 5.09 |
| Anxiety Disorder | 1.74 | 1.49, 2.03 | 1.28 | 1.07, 1.55 | 1.43 | 1.20, 1.70 |
| Anxiety Disorder + Substance | -- | -- | 12.24 | 7.14, 21.02 | 3.87 | 3.01, 5.00 |
| Mental Disorder at Delivery | 8.13 | 7.93, 8.34 | 3.65 | 3.46, 3.84 | 2.60 | 2.47, 2.74 |
| Mental Disorder at Delivery + Substance | -- | -- | 16.36 | 15.54, 17.22 | 5.65 | 5.47, 5.83 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hammond, I.; Eastman, A.L.; Leventhal, J.M.; Putnam-Hornstein, E. Maternal Mental Health Disorders and Reports to Child Protective Services: A Birth Cohort Study. Int. J. Environ. Res. Public Health 2017, 14, 1320. https://doi.org/10.3390/ijerph14111320
Hammond I, Eastman AL, Leventhal JM, Putnam-Hornstein E. Maternal Mental Health Disorders and Reports to Child Protective Services: A Birth Cohort Study. International Journal of Environmental Research and Public Health. 2017; 14(11):1320. https://doi.org/10.3390/ijerph14111320
Chicago/Turabian StyleHammond, Ivy, Andrea Lane Eastman, John M. Leventhal, and Emily Putnam-Hornstein. 2017. "Maternal Mental Health Disorders and Reports to Child Protective Services: A Birth Cohort Study" International Journal of Environmental Research and Public Health 14, no. 11: 1320. https://doi.org/10.3390/ijerph14111320
APA StyleHammond, I., Eastman, A. L., Leventhal, J. M., & Putnam-Hornstein, E. (2017). Maternal Mental Health Disorders and Reports to Child Protective Services: A Birth Cohort Study. International Journal of Environmental Research and Public Health, 14(11), 1320. https://doi.org/10.3390/ijerph14111320




