Adding Natural Areas to Social Indicators of Intra-Urban Health Inequalities among Children: A Case Study from Berlin, Germany
Abstract
:1. Introduction
1.1. Health Inequality Indicators
1.2. Environmental Health Determinants
1.3. Objectives
2. Materials and Methods
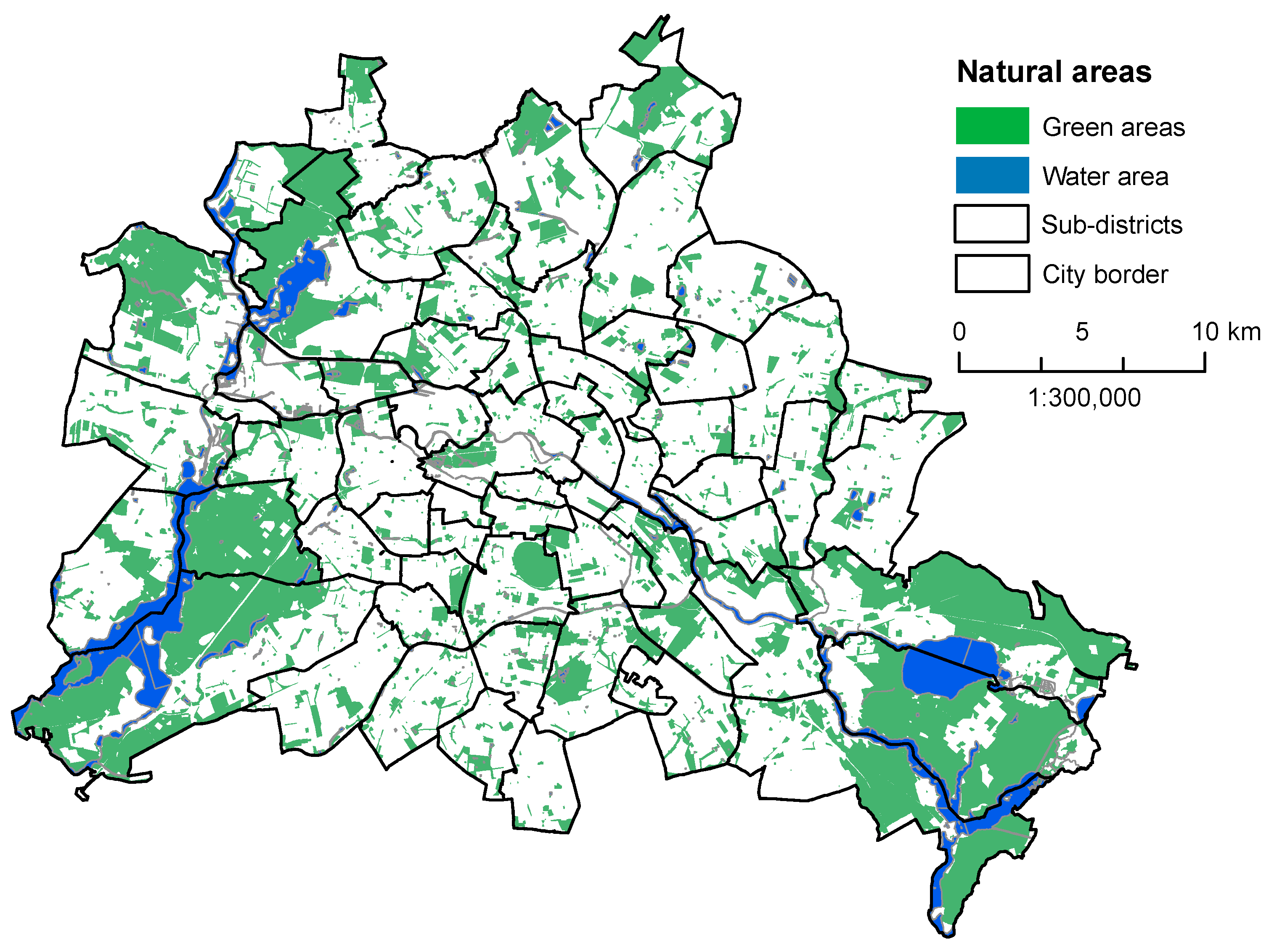
2.1. Study Area
2.2. Data
2.3. Statistical Analysis
3. Results
3.1. Correlation Analysis
3.2. Factor Analysis
3.3. Cluster Analysis and Characterization of the Sub-Districts
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Marmot, M. Social determinants of health inequalities. Lancet 2005, 365, 1099–1104. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef]
- Martuzzi, M.; Mitis, F.; Forastiere, F. Inequalities, inequities, environmental justice in waste management and health. Eur. J. Public Health 2010, 20, 21–26. [Google Scholar] [CrossRef] [PubMed]
- McMichael, A.J. The urban environment and health in a world of increasing globalization: Issues for developing countries. Bull. World Health Organ. 2000, 78, 1117–1126. [Google Scholar] [PubMed]
- Sivertsen, B. Global ambient air pollution concentrations, trends. In WHO Air Quality Guidelines, Global Update 2005; WHO Regional Office for Europe: Copenhagen, Denmark, 2006; pp. 31–59. [Google Scholar]
- Clark, L.P.; Millet, D.B.; Marshall, J.D. National patterns in environmental injustice and inequality: Outdoor NO2 air pollution in the United States. PLoS ONE 2014, 9, e9443. [Google Scholar] [CrossRef] [PubMed]
- Richardson, E.A.; Pearce, J.; Tunstall, H.; Mitchell, R.; Shortt, N.K. Particulate air pollution and health inequalities: A Europe-wide ecological analysis. Int. J. Health Geogr. 2013. [Google Scholar] [CrossRef] [PubMed]
- Sun, Q.; Yue, P.; Deiuliis, J.; Lumeng, C.; Kampfrath, T.; Mikolaj, M.; Cai, Y.M.; Ostrowski, M.C.; Lu, B.; Parthasarathy, S.; et al. Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 2009, 119, 538–546. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Kan, H. Air pollution and population health: A global challenge. Environ. Health Prev. Med. 2008, 13, 94–101. [Google Scholar] [CrossRef] [PubMed]
- King, K.E.; Morenoff, J.D.; House, J.S. Neighborhood context and social disparities in cumulative biological risk factors. Psychosom. Med. 2011, 73, 572–579. [Google Scholar] [CrossRef] [PubMed]
- Lindström, M.; Fridh, M.; Rosvall, M. Economic stress in childhood and adulthood, and poor psychological health: Three life course hypotheses. Psychiatry Res. 2014, 215, 386–393. [Google Scholar] [CrossRef] [PubMed]
- CSDH. Closing the Gap in a Generation: Health Equity through Action on the Social Determinants of Health; Final Report of the Commission on Social Determinants of Health; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- WHO Regional Office for Europe. Available online: http://data.euro.who.int/equity/IA/AllIndicators/doubleMap/atlas.html (accessed on 27 July 2015).
- WHO. Urban HEART Urban Health Equity Assessment and Response Tool; World Health Organization: Kobe, Japan, 2010. [Google Scholar]
- Koller, D.; Mielck, A. Regional and social differences concerning overweight, participation in health check-ups and vaccination. Analysis of data from a whole birth cohort of 6-year old children in a prosperous German city. BMC Public Health 2009, 9, 43. [Google Scholar] [CrossRef] [PubMed]
- Østergren, M.M.; Barnekow, V. Child and adolescent health and development in a European perspective—A new WHO strategy. Dan. Med. Bull. 2007, 54, 150–152. [Google Scholar] [PubMed]
- Barton, H.; Grant, M. A health map for the local human habitat. J. R. Soc. Promot. Health 2006, 126, 252–253. [Google Scholar] [CrossRef]
- Richardson, E.A.; Pearce, J.; Mitchell, R.; Shortt, N.K. A regional measure of neighborhood multiple environmental deprivation: Relationships with health and health inequalities. Prof. Geogr. 2013, 65, 153–170. [Google Scholar] [CrossRef]
- Schwarz, K.; Fragkias, M.; Boone, C.G.; Zhou, W.; McHale, M.; Grove, J.M.; O’Neil-Dunne, J.; McFadden, J.P.; Buckley, G.L.; Childers, D.; et al. Trees grow on money: Urban tree canopy cover and environmental justice. PLoS ONE 2015, 10, e0122051. [Google Scholar] [CrossRef] [PubMed]
- Kabisch, N.; Haase, D. Green justice or just green? Provision of urban green spaces in Berlin, Germany. Landsc. Urban Plan. 2014, 122, 129–139. [Google Scholar] [CrossRef]
- WHO. Healthy Cities. Promoting Health and Equity—Evidence for Local Policy and Practice; De Leeuw, E., Tsouros, A., Dyakova, M., Green, G., Eds.; WHO: Copenhagen, Denmark, 2014. [Google Scholar]
- WHO. Parma Declaration on Environment and Health, Fifth Ministerial Conference on Environment and Health “Protecting Children’s Health in a Changing Environment”; WHO Regional Office for Europe: Copenhagen, Denmark, 2010. [Google Scholar]
- van den Bosch, M.A.; Mudu, P.; Uscila, V.; Barrdahl, M.; Kulinkina, A.; Staatsen, B.; Swart, W.; Kruize, H.; Zurlyte, I.; Egorov, E. Development of an urban green space indicator and the public health rationale. Scand. J. Public Health 2015. [Google Scholar] [CrossRef]
- Kabisch, N.; Strohbach, M.; Haase, D.; Kronenberg, J. Urban green space availability in European cities. Ecol. Indic. 2016. [Google Scholar] [CrossRef]
- Hartig, T.; Mitchell, R.; de Vries, S.; Frumkin, H. Nature and Health. Annu. Rev. Public Health 2014, 35, 207–228. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.C.K.; Maheswaran, R. The health benefits of urban green spaces: A review of the evidence. J. Public Health (Oxf.) 2011, 33, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Bowler, D.E.; Buyung-Ali, L.; Knight, T.M.; Pullin, A.S. Urban greening to cool towns and cities: A systematic review of the empirical evidence. Landsc. Urban Plan. 2010, 97, 147–155. [Google Scholar] [CrossRef]
- Escobedo, F.J.; Kroeger, T.; Wagner, J.E. Urban forests and pollution mitigation: Analyzing ecosystem services and disservices. Environ. Pollut. 2011, 159, 2078–2087. [Google Scholar] [CrossRef] [PubMed]
- Maas, J.; Verheij, R.A.; Groenewegen, P.P.; de Vries, S.; Spreeuwenberg, P. Green space, urbanity, and health: How strong is the relation? J. Epidemiol. Community Health 2006, 60, 587–592. [Google Scholar] [CrossRef] [PubMed]
- De Vries, S.; Verheij, R.A.; Groenewegen, P.P.; Spreeuwenberg, P. Natural environments—Healthy environments? An exploratory analysis of the relationship between greenspace and health. Environ. Plan. A 2003, 35, 1717–1731. [Google Scholar] [CrossRef]
- Gascon, M.; Triguero-Mas, M.; Martínez, D.; Dadvand, P.; Rojas-Rueda, D.; Plasència, A.; Nieuwenhuijsen, M. Residential green spaces and mortality: A systematic review. Environ. Int. 2016, 86, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Sunyer, J.; Basagana, X.; Ballester, F.; Lertxundi, A.; Fernandez-Somoano, A.; Estarlich, M.; Garcia-Esteban, R.; Medndez, M.A.; Nieuwenhuijsen, M. Surrounding greenness and pregnancy outcomes in four Spanish birth cohorts. Environ. Health Perspect. 2012, 120, 1481–1487. [Google Scholar] [CrossRef] [PubMed]
- Tamosiunas, A.; Grazuleviciene, R.; Luksiene, D.; Dedele, A.; Reklaitiene, R.; Baceviciene, M.; Vencloviene, J.; Bernotiene, G.; Radisauskas, R.; Malinauskiene, V.; et al. Accessibility and use of urban green spaces, and cardiovascular health: Findings from a Kaunas cohort study. Environ. Health 2014, 13, 20. [Google Scholar] [CrossRef] [PubMed]
- Annerstedt, M.; Ostergren, P.-O.; Bjork, J.; Grahn, P.; Skarback, E.; Wahrborg, P. Green qualities in the neighbourhood and mental health—Results from a longitudinal cohort study in Southern Sweden. BMC Public Health 2012, 12, 337. [Google Scholar] [CrossRef] [PubMed]
- van den Bosch, M.A.; Östergren, P.-O.; Grahn, P.; Skärbäck, E.; Währborg, P. Moving to serene nature may prevent poor mental health—Results from a Swedish longitudinal cohort study. Int. J. Environ. Res. Public Health 2015, 12, 7974. [Google Scholar] [CrossRef] [PubMed]
- Reklaitiene, R.; Grazuleviciene, R.; Dedele, A.; Virviciute, D.; Vensloviene, J.; Tamosiunas, A.; Baceviciene, M.; Luksiene, D.; Sapranaviciute-Zabazlajeva, L.; Radisauskas, R.; et al. The relationship of green space, depressive symptoms and perceived general health in urban population. Scand. J. Public Health 2014, 42, 669–676. [Google Scholar] [CrossRef] [PubMed]
- Bratman, G.N.; Hamilton, J.P.; Hahn, K.S.; Daily, G.C.; Gross, J.J. Nature experience reduces rumination and subgenual prefrontal cortex activation. Proc. Natl. Acad. Sci. USA 2015, 112, 8567–8572. [Google Scholar] [CrossRef] [PubMed]
- Amoly, E.; Dadvand, P.; Forns, J.; López-Vicente, M.; Basagaña, X.; Julvez, J.; Alvarez-Pedrerol, M.; Nieuwenhuijsen, M.; Sunyer, J. Green and blue spaces and behavioral development in Barcelona schoolchildren: The BREATHE project. Environ. Health Perspect. 2014, 122, 1351–1358. [Google Scholar] [CrossRef] [PubMed]
- Balseviciene, B.; Sinkariova, L.; Grazuleviciene, R.; Andrusaityte, S.; Uzdanaviciute, I.; Dedele, A.; Nieuwenhuijsen, M. Impact of residential greenness on preschool children’s emotional and behavioral problems. Int. J. Environ. Res. Public Health 2014, 11, 6757–6770. [Google Scholar] [CrossRef] [PubMed]
- Dadvand, P.; Nieuwenhuijsen, M.J.; Esnaola, M.; Forns, J.; Basagaña, X.; Alvarez-Pedrerol, M.; Rivas, I.; Lopez-Vicente, M.; De Castro Pascual, M.; Su, J.; et al. Green spaces and cognitive development in primary schoolchildren. Proc. Natl. Acad. Sci. USA 2015, 112, 7937–7942. [Google Scholar] [CrossRef] [PubMed]
- Markevych, I.; Tiesler, C.M.T.; Fuertes, E.; Romanos, M.; Dadvand, P.; Nieuwenhuijsen, M.J.; Berdel, D.; Koletzko, S.; Heinrich, J. Access to urban green spaces and behavioural problems in children: Results from the GINIplus and LISAplus studies. Environ. Int. 2014, 71, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Bush, C.L.; Pittman, S.; McKay, S.; Ortiz, T.; Wong, W.W.; Klish, W.J. Park-based obesity intervention program for inner-city minority children. J. Pediatr. 2007, 151, 513–517. [Google Scholar] [CrossRef] [PubMed]
- Lovasi, G.S.; Schwartz-Soicher, O.; Quinn, J.W.; Berger, D.K.; Neckerman, K.M.; Jaslow, R.; Lee, K.K.; Rundle, A. Neighborhood safety and green space as predictors of obesity among preschool children from low-income families in New York city. Prev. Med. 2013, 57, 189–193. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Lee, C.; Olvera, N.E.; Ellis, C.D. The role of landscape spatial patterns on obesity in Hispanic children residing in inner-city neighborhoods. J. Phys. Act. Health 2014, 11, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- Sanders, T.; Feng, X.; Fahey, P.P.; Lonsdale, C.; Astell-Burt, T. Greener neighbourhoods, slimmer children? Evidence from 4423 participants aged 6 to 13 years in the longitudinal study of Australian children. Int. J. Obes. 2015, 39, 1224–1229. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, R.; Popham, F. Effect of exposure to natural environment on health inequalities: An observational population study. Lancet 2008, 372, 1655–1660. [Google Scholar] [CrossRef]
- Mitchell, R.J.; Richardson, E.A.; Shortt, N.K.; Pearce, J.R. Neighborhood environments and socioeconomic inequalities in mental well-being. Am. J. Prev. Med. 2015, 49, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Roe, J.; Thompson, C.; Aspinall, P.; Brewer, M.; Duff, E.; Miller, D.; Mitchell, R.; Clow, A. Green space and stress: Evidence from cortisol measures in deprived urban communities. Int. J. Environ. Res. Public Health 2013, 10, 4086–4103. [Google Scholar] [CrossRef] [PubMed]
- Thompson, C.W.; Roe, J.; Aspinall, P.; Mitchell, R.; Clow, A.; Miller, D. More green space is linked to less stress in deprived communities: Evidence from salivary cortisol patterns. Landsc. Urban Plan. 2012, 105, 221–229. [Google Scholar] [CrossRef]
- Annerstedt, M.; Jönsson, P.; Wallergård, M.; Johansson, G.; Karlson, B.; Grahn, P.; Hansen, A.M.; Währborg, P. Inducing physiological stress recovery with sounds of nature in a virtual reality forest—Results from a pilot study. Physiol. Behav. 2013, 118, 240–250. [Google Scholar] [CrossRef] [PubMed]
- Andersson, E.; McPhearson, T.; Kremer, P.; Gomez-Baggethun, E.; Haase, D.; Tuvendal, M.; Wurster, D. Scale and context dependence of ecosystem service providing units. Ecosyst. Serv. 2015, 12, 157–164. [Google Scholar] [CrossRef]
- Byrne, J.; Wolch, J. Nature, race, and parks: Past research and future directions for geographic research. Prog. Hum. Geogr. 2009, 33, 743–765. [Google Scholar] [CrossRef]
- Gobster, P.H. Urban parks as green walls or green magnets? Interracial relations in neighborhood boundary parks. Landsc. Urban Plan. 1998, 41, 43–55. [Google Scholar] [CrossRef]
- Jenkins, G.; Yuen, H.; Rose, E.; Maher, A.; Gregory, K.; Cotton, M. Disparities in quality of park play spaces between two cities with diverse income and race/ethnicity composition: A pilot study. Int. J. Environ. Res. Public Health 2015, 12, 8009. [Google Scholar] [CrossRef] [PubMed]
- Vaughan, K.B.; Kaczynski, A.T.; Stanis, S.A.W.; Besenyi, G.M.; Bergstrom, R.; Heinrich, K.M. Exploring the distribution of park availability, features, and quality across Kansas City, Missouri by income and race/ethnicity: An environmental justice investigation. Ann. Behav. Med. 2013, 45 (Suppl. 1), S28–S38. [Google Scholar] [CrossRef] [PubMed]
- Richardson, E.A.; Shortt, N.K.; Mitchell, R.J. The mechanism behind environmental inequality in Scotland: Which came first, the deprivation or the landfill? Environ. Plan. A 2010, 42, 223–240. [Google Scholar] [CrossRef]
- Dai, D. Racial/ethnic and socioeconomic disparities in urban green space accessibility: Where to intervene? Landsc. Urban Plan. 2011, 102, 234–244. [Google Scholar] [CrossRef]
- IPCC. Climate Change 2014: Synthesis Report; Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change; IPCC: Geneva, Switzerland, 2014. [Google Scholar]
- Shishegar, N. The impact of green areas on mitigating urban heat island effect: A review. Int. J. Environ. Sustain. 2014, 9, 119–130. [Google Scholar] [CrossRef]
- Senatsver_altung_für_Stadtentwicklung_und_Umwelt_Berlin. Anteil öffentlicher Grünflächen in Berlin. Available online: http://www.stadtentwicklung.berlin.de/planen/bevoelkerungsprognose/download/bevprog_2011_2030_kurzfassung.pdf (accessed on 29 July 2015).
- Senatsverwaltung_für_Stadtentwicklung_und_Umwelt_Berlin. Bevölkerungsprognose für Berlin und die Bezirke 2011–2030. Available online: http://www.stadtentwicklung.berlin.de/planen/bevoelkerungsprognose/download/bevprog_2011_2030_kurzfassung.pdf (accessed on 29 July 2015).
- Senatsverwaltung_für_Gesundheit_und_Soziales. Grundauswertung der Einschulungsdaten in Berlin 2013. Available online: http://www.berlin.de/sen/gessoz/gesundheits-und-sozialberichterstattung/ (accessed on 29 July 2015).
- Cromley, E.K.; McLafferty, S.L. GIS and Public Health, 2nd ed.; The Guilford Press: New York, NY, USA, 2012. [Google Scholar]
- Schwarz, N. Urban form revisited—Selecting indicators for characterizing European cities. Landsc. Urban Plan. 2010, 96, 29–47. [Google Scholar] [CrossRef]
- Kabisch, N.; Haase, D.; Haase, A. Evolving reurbanisation? Spatio-temporal dynamics as exemplified by the East German city of Leipzig. Urban Stud. 2010, 47, 967–990. [Google Scholar] [CrossRef]
- Wolch, J.R.; Byrne, J.; Newell, J.P. Urban green space, public health, and environmental justice: The challenge of making cities “just green enough”. Landsc. Urban Plan. 2014, 125, 234–244. [Google Scholar] [CrossRef]
- Dooling, S. Ecological Gentrification: A research agenda exploring justice in the city. Int. J. Urban Reg. Res. 2009, 33, 621–639. [Google Scholar] [CrossRef]
- Voigt, A.; Kabisch, N.; Wurster, D.; Haase, D.; Breuste, J. Structural diversity: A multi-dimensional approach to assess recreational services in urban parks. Ambio 2014, 43, 480–491. [Google Scholar] [CrossRef] [PubMed]
- Hughey, S.M.; Walsemann, K.M.; Child, S.; Powers, A.; Reed, J.A.; Kaczynski, A.T. Using an environmental justice approach to examine the relationships between park availability and quality indicators, neighborhood disadvantage, and racial/ethnic composition. Landsc. Urban Plan. 2016, 148, 159–169. [Google Scholar] [CrossRef]
- Mitchell, R.; Astell-Burt, T.; Richardson, E.A. A comparison of green space indicators for epidemiological research. J. Epidemiol. Community Health 2011, 65, 853–858. [Google Scholar] [CrossRef] [PubMed]
- Nordic Council of Ministers. Friluftsliv Trenger mer Enn Arealer—En Studie av Kriterier og Normer for Friarealer I Kommunalplanlegging (Outdoor Recreation Demands More Than Areas—A Study of criteria and Norms for Recreational Areas in Municipal Planning); Nordisk Ministerråd: Copenhagen, Denmark, 1996. [Google Scholar]
- Burgess, D.C.; Burgess, M.A.; Leask, J. The MMR vaccination and autism controversy in United Kingdom 1998–2005: Inevitable community outrage or a failure of risk communication? Vaccine 2006, 24, 3921–3928. [Google Scholar] [CrossRef] [PubMed]
- Blume, S. Anti-vaccination movements and their interpretations. Soc. Sci. Med. 2006, 62, 628–642. [Google Scholar] [CrossRef] [PubMed]
- Lewandowsky, S.; Ecker, U.K.H.; Seifert, C.M.; Schwarz, N.; Cook, J. Misinformation and its correction: Continued influence and successful debiasing. Psychol. Sci. Public Interest Suppl. 2012, 13, 106–131. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W.; Melgaard, B.; Clements, C.J.; Kane, M.; Mulholland, E.K.; Olivé, J.M. Autism, inflammatory bowel disease, and MMR vaccine. Lancet 1998, 351, 905. [Google Scholar] [CrossRef]
- Godlee, F.; Smith, J.; Marcovitch, H. Wakefield’s article linking MMR vaccine and autism was fraudulent. BMJ 2011, 342, 64–66. [Google Scholar] [CrossRef] [PubMed]
- Demicheli, V.; Rivetti, A.; Debalini, M.G.; Di Pietrantonj, C. Vaccines for measles, mumps and rubella in children. Evid.-Based Child Health Cochrane Rev. J. 2013, 8, 2076–2238. [Google Scholar] [CrossRef]
- Mäkelä, A.; Nuorti, J.P.; Peltola, H. Neurologic disorders after measles-mumps-rubella vaccination. Pediatrics 2002, 110, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Madsen, K.M.; Hviid, A.; Vestergaard, M.; Schendel, D.; Wohlfahrt, J.; Thorsen, P.; Olsen, J.; Melbye, M. A population-based study of measles, mumps, and rubella vaccination and autism. N. Engl. J. Med. 2002, 347, 1477–1482. [Google Scholar] [CrossRef] [PubMed]
- Bender, A.M.; Kawachi, I.; Jørgensen, T.; Pisinger, C. Neighborhood deprivation is strongly associated with participation in a population-based health check. PLoS ONE 2015, 10, e0129819. [Google Scholar] [CrossRef] [PubMed]
- White, M.P.; Alcock, I.; Wheeler, B.W.; Depledge, M.H. Coastal proximity, health and well-being: Results from a longitudinal panel survey. Health Place 2013, 23, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Völker, S.; Kistemann, T. “I’m always entirely happy when I’m here!” Urban blue enhancing human health and well-being in Cologne and Düsseldorf, Germany. Soc. Sci. Med. 2013, 78, 113–124. [Google Scholar] [CrossRef] [PubMed]
- Byrne, J.; Sipe, N. Green and Open Space Planning for Urban Consolidation—A Review of the Literature and Best Practice; Urban Research Program, Issues Paper 11; Griffith University: Brisbane, Australia, 2010. [Google Scholar]

| Variables | Description | Year | Data Source |
|---|---|---|---|
| Health-outcome variables | |||
| Overweight (%) | Percentage of children overweight as defined by the Body-Mass-Index, BMI (thresholds are defined monthly by Kromeyer-Hausschild) | 2013 | SDHS |
| Dental problems (%) | Percentage of children with dental problems | 2013 | SDHS |
| Deficits in viso-motoric development (%) | Percentage of children with impaired fine motor ability | 2013 | SDHS |
| Deficits in language development (%) | Percentage of children with deficits in language development | 2013 | SDHS |
| Social variables | |||
| Social status index | Median index (0–18) representing the status of parents based on school education, employment education and employment status: 0–8 low social status, 9–15 medium social status, 16–18 high social status | 2013 | SDHS |
| Single parent household (%) | Percentage of children living in single parent households | 2013 | SDHS |
| Non-German (%) | Percentage of children with background other than German | 2013 | SDHS |
| Complete measles immunization (%) | Percentage of children with at least two doses (considered complete) of measles vaccination | 2013 | SDHS |
| Participating in U8 (%) | Percentage of children that participated in a preventive health check-up at the age of 4, i.e., U8 | 2013 | SDHS |
| Variables of social-environmental conditions of child care | |||
| Kindergarten attendance (%) | Percentage of children enrolled in kindergarten for at least 2 years | 2013 | SDHS |
| Smokers (%) | Percentage of children with at least one smoking person in household | 2013 | SDHS |
| Own TV (%) | Percentage of children with their own TV | 2013 | SDHS |
| Land use variables | |||
| Simple residential area (%) | Percentage of addresses situated in an area classified as a “simple residential area.” These areas are very dense, highly contained and have low to no green space. The streets and building facades are mostly not well maintained. | 2010 | SDUDE |
| Natural area (%) | Percentage of green and water areas in the sub-districts in relation to the total sub-district area. Green areas include forest areas, urban green and parks, cemeteries and allotment gardens. Water areas include all the water bodies such as lakes, rivers and canals. | 2011 | |
| Per capita natural area (m2/inhabitant) | Natural area (m2)/total number of inhabitants in the sub-district | 2011 | SDUDE |
| Availability of natural area (%) | Percentage of inhabitants living a maximum of 300 m distance away from a natural area (green area of min. 2 ha) | 2011 | SDUDE |
| Population density (inhabitants/km2) | Total number of inhabitants in 2014/total area of the sub-districts (km2) | 2014 | SDUDE, Dep. for Statistics BBR |
| Health Outcome | Overweight (%) | Dental Problems (%) | Deficits in Viso-Motoric Development (%) | Deficits in Language Development (%) | |
|---|---|---|---|---|---|
| Health Determinants | |||||
| Social variables | |||||
| Social status index | −0.780 ** | −0.786 ** | −0.660 ** | −0.822 ** | |
| Non-German (%) | 0.809 ** | 0.754 ** | 0.334 ** | 0.779 ** | |
| Single parent household (%) | 0.333 ** | 0.475 ** | 0.415 ** | 0.365 ** | |
| Complete measles immunization (%) | 0.354 ** | 0.394 ** | 0.467 ** | 0.470 ** | |
| Participating in U8 (%) | −0.525 ** | −0.507 ** | −0.356 ** | −0.506 ** | |
| Socio-environmental variables | |||||
| Kindergarten attendance (%) | −0.780 ** | −0.821 ** | −0.585 ** | −0.873 ** | |
| Smokers in family (%) | 0.658 ** | 0.686 ** | 0.630 ** | 0.685 ** | |
| Own TV (%) | 0.689 ** | 0.728 ** | 0.747 ** | 0.754 ** | |
| Land use variables | |||||
| Simple residential area (%) | 0.520 ** | 0.525 ** | 0.444 ** | 0.538 ** | |
| Natural area (%) | −0.149 | −0.172 | −0.260 * | −0.248 | |
| Per capita natural area (m²/inhabitants) | −0.322 ** | −0.334 ** | −0.209 | −0.332 ** | |
| Inhabitants with availability of natural area (%) | 0.105 | 0.102 | 0.116 | 0.106 | |
| Population density (inhabitants/km²) | 0.369 ** | 0.393 ** | 0.168 | 0.342 ** | |
| Social & Socio-Environ | Social Status Index | Non-German (%) | Single Parent Household (%) | Complete Measles Immunezation (%) | Participating in U8 (%) | Kindergarten Attendance (%) | Smokers (%) | Own TV (%) | |
|---|---|---|---|---|---|---|---|---|---|
| Land-Use Variables | |||||||||
| Simple residential area (%) | −0.594 ** | 0.478 ** | 0.258 * | 0.250 | −0.566 ** | −0.358 ** | 0.582 ** | 0.489 ** | |
| Natural area (%) | −0.02 | −0.189 | 0.073 | −0.095 | 0.002 | 0.128 | 0.019 | −0.017 | |
| Per capita natural area (m²/inh.) | 0.034 | −0.462 ** | 0.013 | 0.139 | 0.209 | 0.232 | −0.030 | 0.004 | |
| Availability of natural areas (%) | −0.316 * | 0.006 | 0.181 | −0.036 | −0.175 | −0.181 | 0.427 ** | 0.270 * | |
| Population density (inh./km²) | −0.076 | 0.555 ** | 0.049 | −0.228 | −0.314 * | −0.267 * | 0.089 | 0.013 | |
| Social & Socio-Environ. Variables | Social Status Index | Non-German (%) | Single Parent Household (%) | Complete Measles Immunization (%) | Participating in U8 (%) | Kindergarten Attendance (%) | Smokers (%) |
|---|---|---|---|---|---|---|---|
| Non-German (%) | −0.551 ** | ||||||
| Single parent household (%) | −0.576 ** | 0.132 | |||||
| Complete measles immunization (%) | −0.551 ** | 0.123 | 0.342 ** | ||||
| Participation in U8 (%) | 0.542 ** | −0.441 ** | −0.354 ** | 0.010 | |||
| Kindergarten attendance (%) | 0.742 ** | −0.743 ** | −0.372 ** | −0.400 ** | 0.357 ** | ||
| Smokers (%) | −0.883 ** | 0.395 ** | 0.748 ** | 0.422 ** | −0.550 ** | −0.593 ** | |
| Own TV (%) | −0.898 ** | 0.381 ** | 0.714 ** | 0.578 ** | −0.526 ** | −0.695 ** | 0.886 ** |
| Variables | Factor (% of Variance) | Communalities | |||
|---|---|---|---|---|---|
| I (48.97) | II (16.84) | III (9.67) | IV (6.57) | ||
| Overweight (%) | 0.919 | 0.891 | |||
| Non-German (%) | 0.915 | 0.898 | |||
| Deficit in language (%) | 0.907 | 0.954 | |||
| Dental problems (%) | 0.854 | 0.860 | |||
| Kindergarten attendance (%) | −0.847 | 0.825 | |||
| Social status index | −0.829 | 0.910 | |||
| U8 participation (%) | −0.628 | 0.731 | |||
| Simple residential area (%) | 0.616 | 0.620 | |||
| Single parent household (%) | 0.907 | 0.829 | |||
| Smoker in family (%) | 0.820 | 0.904 | |||
| Own TV (%) | 0.776 | 0.947 | |||
| Deficits in viso-motoric development (%) | 0.648 | 0.667 | |||
| Natural area (%) | 0.924 | 0.876 | |||
| Per capita natural area (m²/inhabitant) | 0.866 | 0.813 | |||
| Availability of natural area (%) | 0.633 | 0.543 | |||
| Complete measles immunization (%) | 0.821 | 0.862 | |||
| Population density (inhabitants/km²) | −0.609 | 0.822 | |||
| Cluster Indicators | Cluster | Total City | ||||
|---|---|---|---|---|---|---|
| ANOVA F (df, p-values) | 1 | 2 | 3 | 4 | ||
| M (SD) Cluster 1 | M (SD) Cluster 2 | M (SD) Cluster 3 | M (SD) Cluster 4 | |||
| Overweight (%) | 12.69 (3; 0.000) | 5.79 (2.41) | 11.48 (3.72) | 8.41 (2.22) | 7.58 (2.92) | 8.76 (3.92) |
| Single parent household (%) | 20.13 (3; 0.000) | 19.48 (6.01) | 23.48 (4.07) | 39.89 (5.55) | 23.68 (10.18) | 24.17 (8.44) |
| Natural area (%) | 51.84 (3; 0.000) | 20.21 (7.29) | 15.16 (7.16) | 15.30 (9.39) | 55.54 (12.03) | 22.28 (15.68) |
| Complete measles immunization (%) | 7.17 (3; 0.000) | 88.59 (4.49) | 92.89 (2.13) | 93.26 (1.56) | 90.19 (4.14) | 91.18 (3.83) |
| N (districts) | 19 | 25 | 7 | 8 | 59 | |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kabisch, N.; Haase, D.; Annerstedt van den Bosch, M. Adding Natural Areas to Social Indicators of Intra-Urban Health Inequalities among Children: A Case Study from Berlin, Germany. Int. J. Environ. Res. Public Health 2016, 13, 783. https://doi.org/10.3390/ijerph13080783
Kabisch N, Haase D, Annerstedt van den Bosch M. Adding Natural Areas to Social Indicators of Intra-Urban Health Inequalities among Children: A Case Study from Berlin, Germany. International Journal of Environmental Research and Public Health. 2016; 13(8):783. https://doi.org/10.3390/ijerph13080783
Chicago/Turabian StyleKabisch, Nadja, Dagmar Haase, and Matilda Annerstedt van den Bosch. 2016. "Adding Natural Areas to Social Indicators of Intra-Urban Health Inequalities among Children: A Case Study from Berlin, Germany" International Journal of Environmental Research and Public Health 13, no. 8: 783. https://doi.org/10.3390/ijerph13080783
APA StyleKabisch, N., Haase, D., & Annerstedt van den Bosch, M. (2016). Adding Natural Areas to Social Indicators of Intra-Urban Health Inequalities among Children: A Case Study from Berlin, Germany. International Journal of Environmental Research and Public Health, 13(8), 783. https://doi.org/10.3390/ijerph13080783





