Effects of Meteorological Parameters and PM10 on the Incidence of Hand, Foot, and Mouth Disease in Children in China
Abstract
:1. Introduction
2. Methods
2.1. Data Collection
2.2. Data Analysis
| Yt~poisson (μt) |
| log(μt) = α + ns(Tt,1,df) + ns(NO2,df) + φ atmospheric pressure + ns(PM10 t,1,df) + wind |
| velocity + γSO2 + ns(RHt,1,df) + jDOWt, + кStratat |
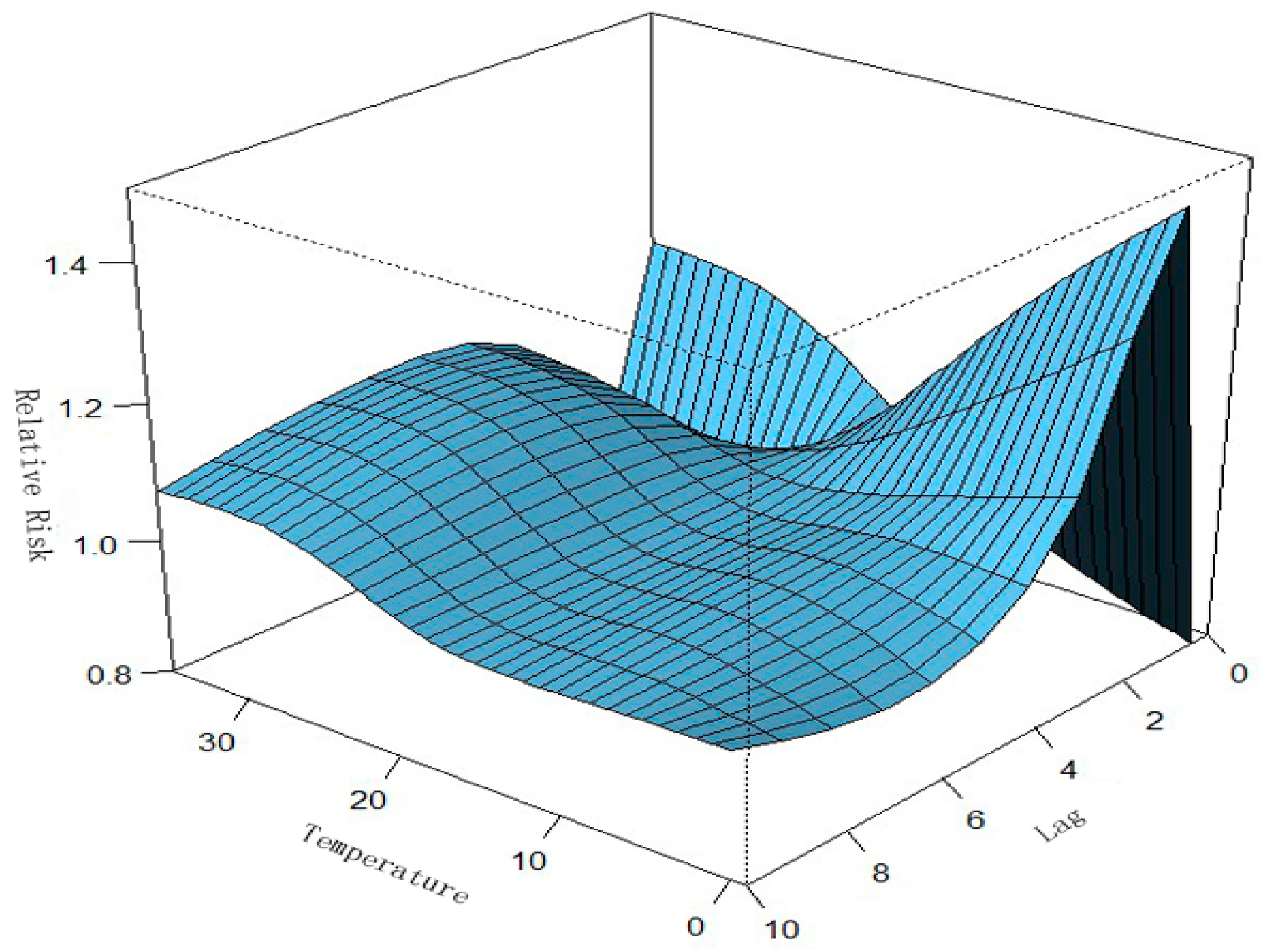
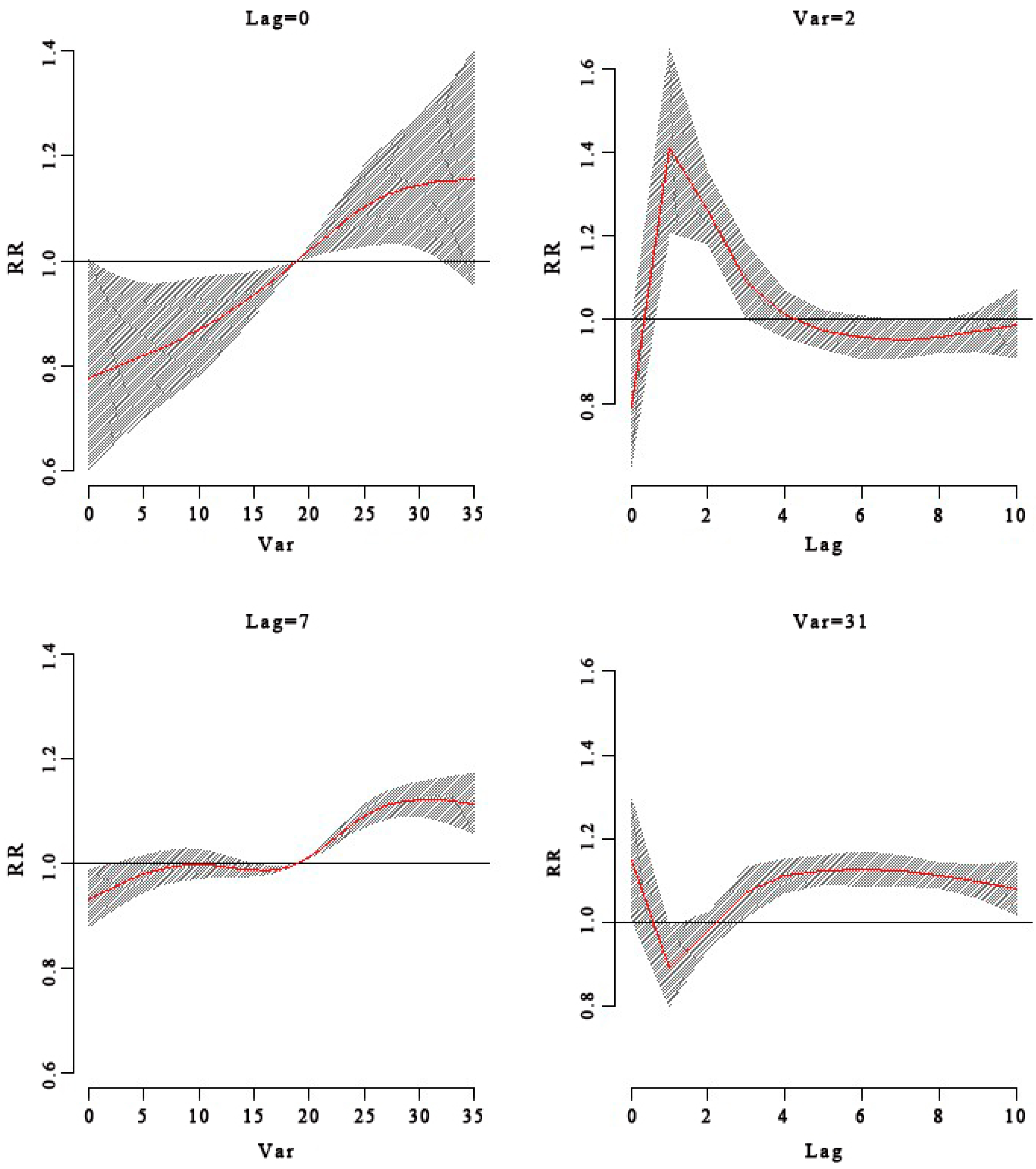
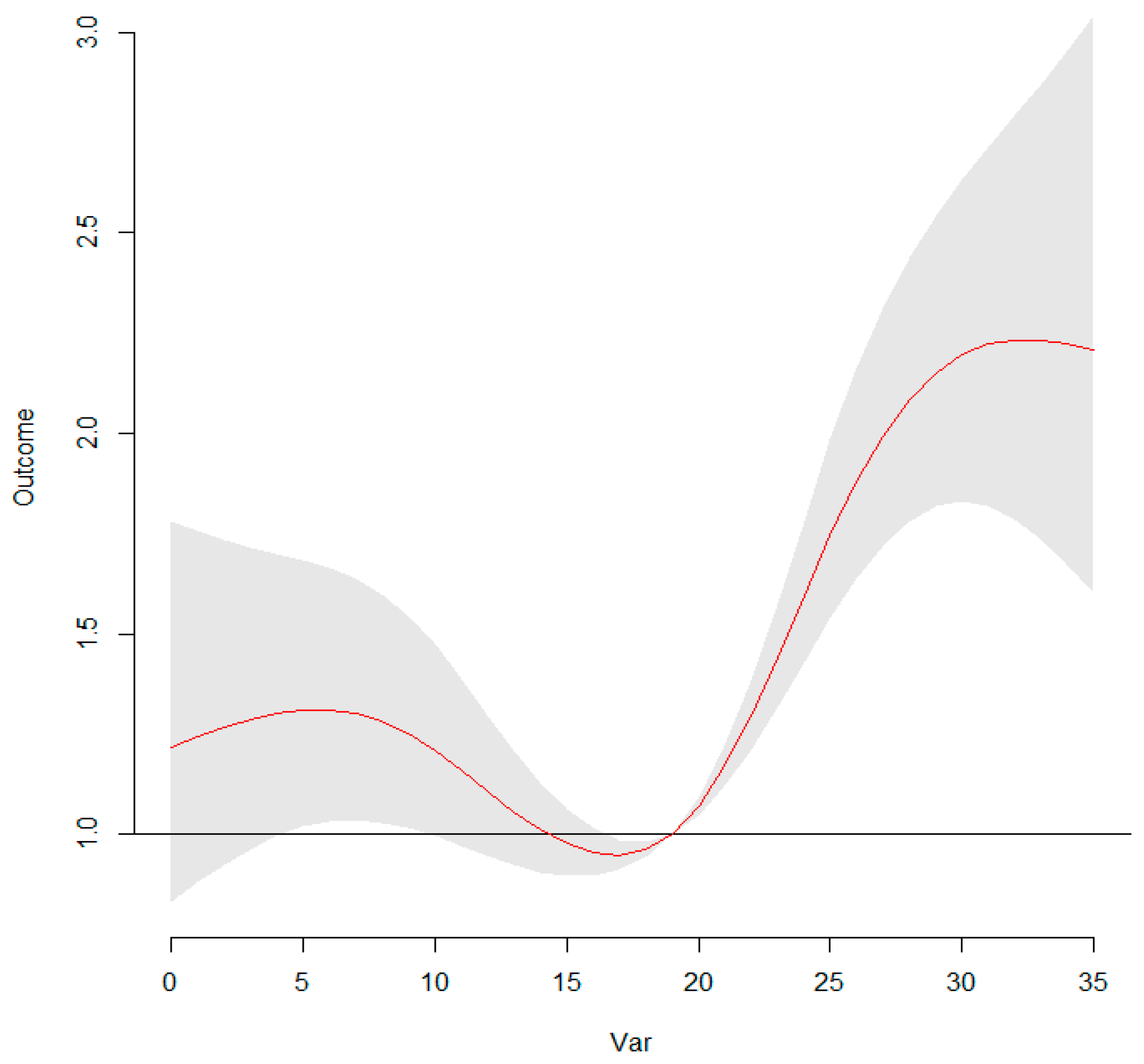
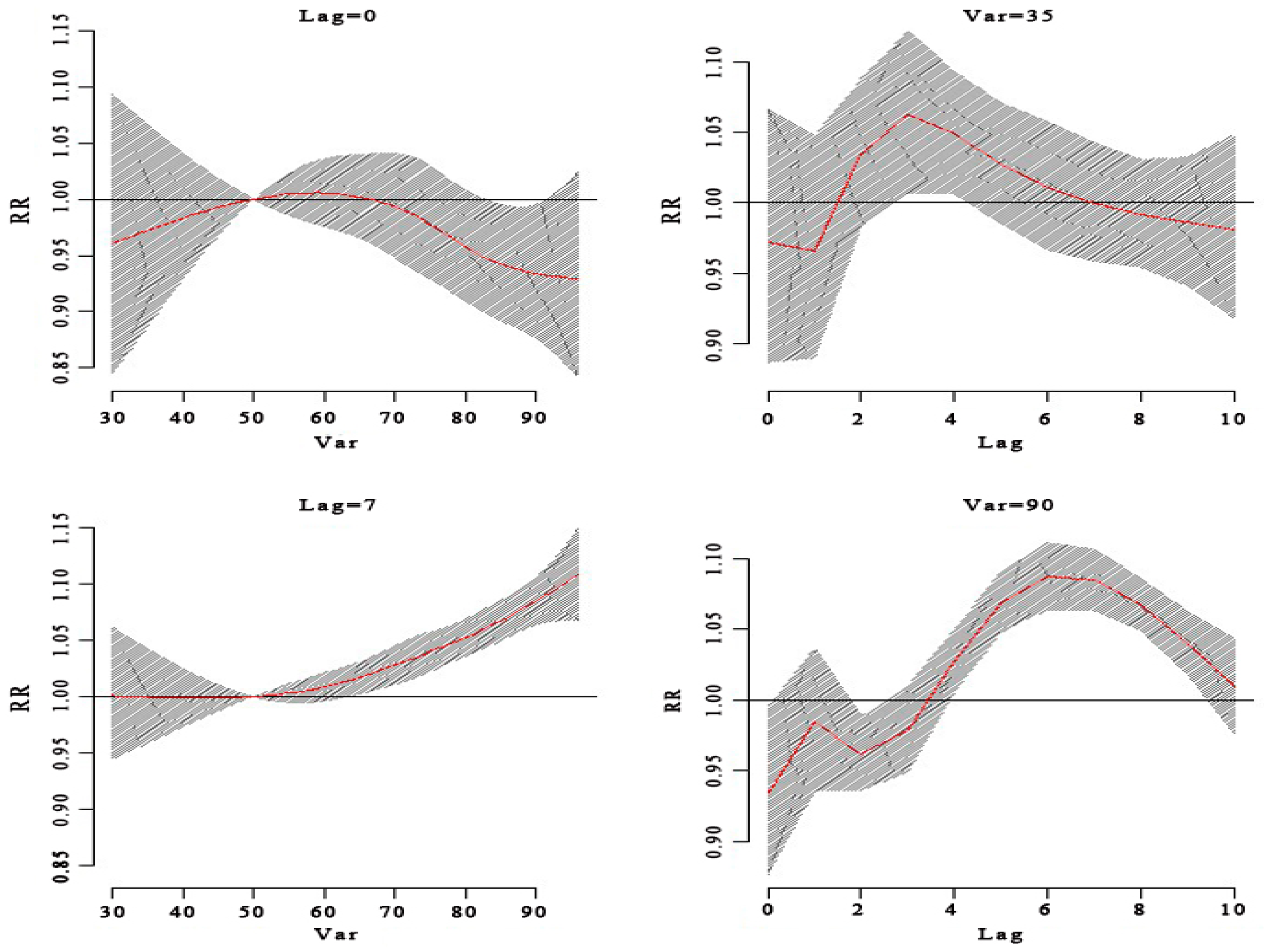
3. Results
Study Characteristics
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Nassef, C.; Ziemer, C.; Morrell, D.S. Hand-foot-and-mouth disease: A new look at a classic viral rash. Curr. Opin. Pediatr. 2015, 27, 486–491. [Google Scholar] [CrossRef] [PubMed]
- Lai, F.F.; Yan, Q.; Ge, S.X.; Tang, X.; Chen, R.J.; Xu, H.M. Epidemiologic and etiologic characteristics of hand, foot, and mouth disease in Chongqing, China between 2010 and 2013. J. Med. Virol. 2016, 88, 408–416. [Google Scholar] [CrossRef] [PubMed]
- Ooi, M.H.; Wong, S.C.; Lewthwaite, P.; Cardosa, M.J.; Solomon, T. Clinical features, diagnosis, and management of enterovirus 71. Lancet Neurol. 2010, 9, 1097–1105. [Google Scholar] [CrossRef]
- Zhu, F.C.; Liang, Z.-L.; Meng, F.-Y.; Zeng, Y.; Mao, Q.-Y.; Chu, K.; Song, X.-F.; Yao, X.; Li, J.-X.; Ji, H.; et al. Retrospective study of the incidence of HFMD and seroepidemiology of antibodies against EV71 and CoxA16 in prenatal women and their infants. PLoS ONE 2012, 7, e37206. [Google Scholar]
- AbuBakar, S.; Chee, H.-Y.; Al-Kobaisi, M.F.; Xiao, J.; Chua, K.B.; Lam, S.K. Identification of enterovirus 71 isolates from an outbreak of hand, foot and mouth disease (HFMD) with fatal cases of encephalomyelitis in Malaysia. Virus Res. 1999, 61, 1–9. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhu, Z.; Yang, W.; Ren, J.; Tan, X.; Wang, Y.; Mao, N.; Xu, S.; Zhu, S.; Cui, A.; et al. An emerging recombinant human enterovirus 71 responsible for the 2008 outbreak of hand foot and mouth disease in Fuyang city of China. Virol. J. 2010, 7, 94. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Yuan, Z.; Wang, X.; Li, J.; Wang, L.; Liu, Y.; Xue, F.; Liu, Y. The Impact of Ambient Temperature on Childhood HFMD Incidence in Inland and Coastal Area: A Two-City Study in Shandong Province, China. Int. J. Environ. Res. Public Health 2015, 12, 8691–8704. [Google Scholar] [CrossRef] [PubMed]
- Goldizen, F.C.; Sly, P.D.; Knibbs, L.D. Respiratory effects of air pollution on children. Pediatr. Pulmonol. 2016, 51, 94–108. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Fang, L.; Cao, W.; Zhang, Y.; Cao, K.; Xu, Q.; Guo, X. Analysis on impact of meteorological factors on incidence of hand, foot and mouth disease based on Bayes spatial-temporal theory. Zhonghua Liu Xing Bing Xue Za Zhi 2015, 36, 476–480. [Google Scholar] [PubMed]
- Yang, H.; Wu, J.; Cheng, J.; Wang, X.; Wen, L.; Li, K.; Su, H. Is high relative humidity associated with childhood hand, foot, and mouth disease in rural and urban areas? Public Health 2015. [Google Scholar] [CrossRef] [PubMed]
- Ma, E.; Lam, T.; Wong, C.; Chuang, S. Is hand, foot and mouth disease associated with meteorological parameters? Epidemiol. Infet. 2014, 138, 1779–1788. [Google Scholar] [CrossRef] [PubMed]
- Hii, Y.L.; Rocklov, J.; Ng, N. Short term effects of weather on hand, foot and mouth disease. PLoS ONE 2011, 6, e16796. [Google Scholar] [CrossRef] [PubMed]
- Xu, M.; Yu, W.; Tong, S.; Jia, L.; Liang, F.; Pan, X. Non-Linear Association between Exposure to Ambient Temperature and Children’s Hand-Foot-and-Mouth Disease in Beijing, China. PLoS ONE 2015, 10, e0126171. [Google Scholar]
- Zheng, X.Y.; Ding, H.; Jiang, L.; Chen, S.; Zheng, J.; Qiu, M.; Zhou, Y.; Chen, Q.; Guan, W. Association between Air Pollutants and Asthma Emergency Room Visits and Hospital Admissions in Time Series Studies: A Systematic Review and Meta-Analysis. PLoS ONE 2015, 10, e0138146. [Google Scholar]
- Sunyer, J.; Spix, C.; Quénel, P.; Ponce-de-León, A.; Pönka, A.; Barumandzadeh, T.; Touloumi, G.; Bacharova, L.; Wojtyniak, B.; Vonk, J.; et al. Urban air pollution and emergency admissions for asthma in four European cities: The APHEA Project. Thorax 1997, 52, 760–765. [Google Scholar] [CrossRef] [PubMed]
- Barnett, A.G.; Williams, G.M.; Schwartz, J.; Neller, A.H.; Best, T.L.; Petroeschevsky, A.L.; Simpson, R.W. Air pollution and child respiratory health: A case-crossover study in Australia and New Zealand. Am. J. Respir. Crit. Care Med. 2005, 171, 1272–1278. [Google Scholar] [CrossRef] [PubMed]
- Worldmap. Available online: http://worldmap.harvard.edu/maps/new (accessed on 30 September 2015).
- Guide for Hand, Foot and Mouth Disease Control. Available online: http://www.chinacdc.cn/jkzt/crb/szkb/jszl_2275/200906/t20090612_24707.htm (accessed on 12 June 2009).
- Guo, Y.; Barnett, A.G.; Pan, X.; Yu, W.; Tong, S. The impact of temperature on mortality in Tianjin, China: A case-crossover design with a distributed lag nonlinear model. Environ. Health Perspect. 2011, 119, 1719–1725. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.S.; Yip, C.C.; Lau, S.K.; Yuen, K.Y. Human enterovirus 71 and hand, foot and mouth disease. Epidemiol. Infect. 2010, 138, 1071–1089. [Google Scholar] [CrossRef] [PubMed]
- Braga, A.; Zanobetti, A.; Schwartz, J. The time course of weather-related deaths. Epidemiology 2001, 12, 662–667. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B. Distributed Lag Non-Linear Models in R: The Package DLNM. Available online: http://cran.r-project.org/web/packages/dlnm/vignettes/dlnmOver-view.pdf (accessed on 13 June 2012).
- Gasparrini, A. Modeling exposure-lag-response associations with distributed lag non-linear models. Stat. Med. 2014, 33, 881–899. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Liu, Y.; Ma, Z.; Toloo, G.; Hu, W.; Tong, S. Assessment of the temperature effect on childhood diarrhea using satellite imagery. Sci. Rep. 2014, 4, 5389. [Google Scholar] [PubMed]
- Zhang, Y.; Li, S.; Pan, X.; Tong, S.; Jaakkola, J.J.; Gasparrini, A.; Guo, Y.; Wang, S. The effects of ambient temperature on cerebrovascular mortality: An epidemiologic study in four climatic zones in China. Environ. Health 2014, 13, 24. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Wu, J.; Xu, Z.; Zhu, R.; Wang, X.; Li, K.; Wen, K.; Yang, H.; Su, H. Associations between extreme precipitation and childhood hand, foot and mouth disease in urban and rural areas in Hefei, China. Sci. Total Environ. 2014, 497–498, 484–490. [Google Scholar] [CrossRef] [PubMed]
- Wu, S.X.; Wu, J.F.; Yang, J.; Wei, H.Y.; Xu, Y.L.; Huang, X.Y. Hand-foot-mouth disease pathogen separation and EV71 VP1 gene analysis in Sanmenxia City, Henan Province, China. Bing Du Xue Bao 2014, 30, 630–635. [Google Scholar] [PubMed]
- Deng, Q.; Lu, C.; Norbäck, D.; Bornehag, C.-G.; Zhang, Y.; Liu, W.; Yuan, H.; Sundell, J. Early life exposure to ambient air pollution and childhood asthma in China. Environ. Res. 2015, 143, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Su, C.; Breitner, S.; Schneider, A.; Liu, L.; Franck, U.; Peters, A.; Pan, X. Short-term effects of fine particulate air pollution on cardiovascular hospital emergency room visits: A time-series study in Beijing, China. Int. Arch. Occup. Environ. Health 2016, 89, 641–657. [Google Scholar] [CrossRef] [PubMed]
- Clifford, H.D.; Perks, K.L.; Zosky, G.R. Geogenic PM10 exposure exacerbates responses to influenza infection. Sci. Total Environ. 2015, 533, 275–282. [Google Scholar] [CrossRef] [PubMed]
- Reedijk, M.; van Leuken, J.P.; van der Hoekm, W. Particulate matter strongly associated with human Q fever in The Netherlands: An ecological study. Epidemiol. Infect. 2013, 141, 2623–2633. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.R.; Veranth, J.M.; Kodavanti, U.P.; Aust, A.E.; Pinkerton, K.E. Acute pulmonary and systemic effects of inhaled coal fly ash in rats: Comparison to ambient environmental particles. Toxicol. Sci. 2006, 93, 390–399. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Sioutas, C.; Cho, A.; Schmitz, D.; Misra, C.; Sempf, J.; Wang, M.; Oberley, T.; Froines, J.; Nel, A. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ. Health Perspect. 2003, 111, 455–460. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.N.; Sun, Y.; Lin, C.Y.; Jia, L.; Wu, Q.R.; Li, X.Y.; Wang, Q.Y. A Case-control study to identify environmental risk factors for hand, foot, and mouth disease outbreaks in Beijing. Jpn. J. Infect. Dis. 2014, 67, 95–99. [Google Scholar] [PubMed]






| Basic Demographic Characteristics | Ningbo |
|---|---|
| Total Cases | 86,695 |
| Age | |
| 0–1 years | 7103 (8.19%) |
| 1–3 years | 44,270 (51.06%) |
| 3–6 years | 30,492 (35.17%) |
| 6–15 years | 4525 (5.21%) |
| 15–50 years | 298 (0.34%) |
| >50 years | 7 (0.03%) |
| Sex | |
| Male | 51,989 (59.97%) |
| Female | 34,706 (40.03%) |
| Index | Mean ± SD | Min. | Median | Max. |
|---|---|---|---|---|
| Temp (°C) | 17.64 ± 8.82 | −0.8 | 18.95 | 34.4 |
| Humidity | 73.17 ± 12.34 | 28 | 74 | 95 |
| Atmospheric pressure | 1015.51 ± 8.67 | 986.61 | 1015.59 | 1037.55 |
| Wind velocity | 11.88 ± 8.02 | 3 | 10 | 60 |
| PM10 | 90.69 ± 56.91 | 13 | 74 | 605 |
| NO2 | 46.19 ± 20.73 | 7 | 44 | 132 |
| SO2 | 19.45 ± 13.23 | 4 | 16 | 108 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, R.; Bian, G.; He, T.; Chen, L.; Xu, G. Effects of Meteorological Parameters and PM10 on the Incidence of Hand, Foot, and Mouth Disease in Children in China. Int. J. Environ. Res. Public Health 2016, 13, 481. https://doi.org/10.3390/ijerph13050481
Huang R, Bian G, He T, Chen L, Xu G. Effects of Meteorological Parameters and PM10 on the Incidence of Hand, Foot, and Mouth Disease in Children in China. International Journal of Environmental Research and Public Health. 2016; 13(5):481. https://doi.org/10.3390/ijerph13050481
Chicago/Turabian StyleHuang, Ruixue, Guolin Bian, Tianfeng He, Lv Chen, and Guozhang Xu. 2016. "Effects of Meteorological Parameters and PM10 on the Incidence of Hand, Foot, and Mouth Disease in Children in China" International Journal of Environmental Research and Public Health 13, no. 5: 481. https://doi.org/10.3390/ijerph13050481
APA StyleHuang, R., Bian, G., He, T., Chen, L., & Xu, G. (2016). Effects of Meteorological Parameters and PM10 on the Incidence of Hand, Foot, and Mouth Disease in Children in China. International Journal of Environmental Research and Public Health, 13(5), 481. https://doi.org/10.3390/ijerph13050481





