Knowledge, Attitudes and Behaviours of Healthcare Workers in the Kingdom of Saudi Arabia to MERS Coronavirus and Other Emerging Infectious Diseases
Abstract
:1. Introduction
1.1. Background
1.2. Aim
2. Methods
3. Results
3.1. MERS Coronavirus Knowledge and Sources of Information
3.2. Personal Experiences with MERS-CoV
3.3. Location of Management of Patients with Emerging Infectious Diseases
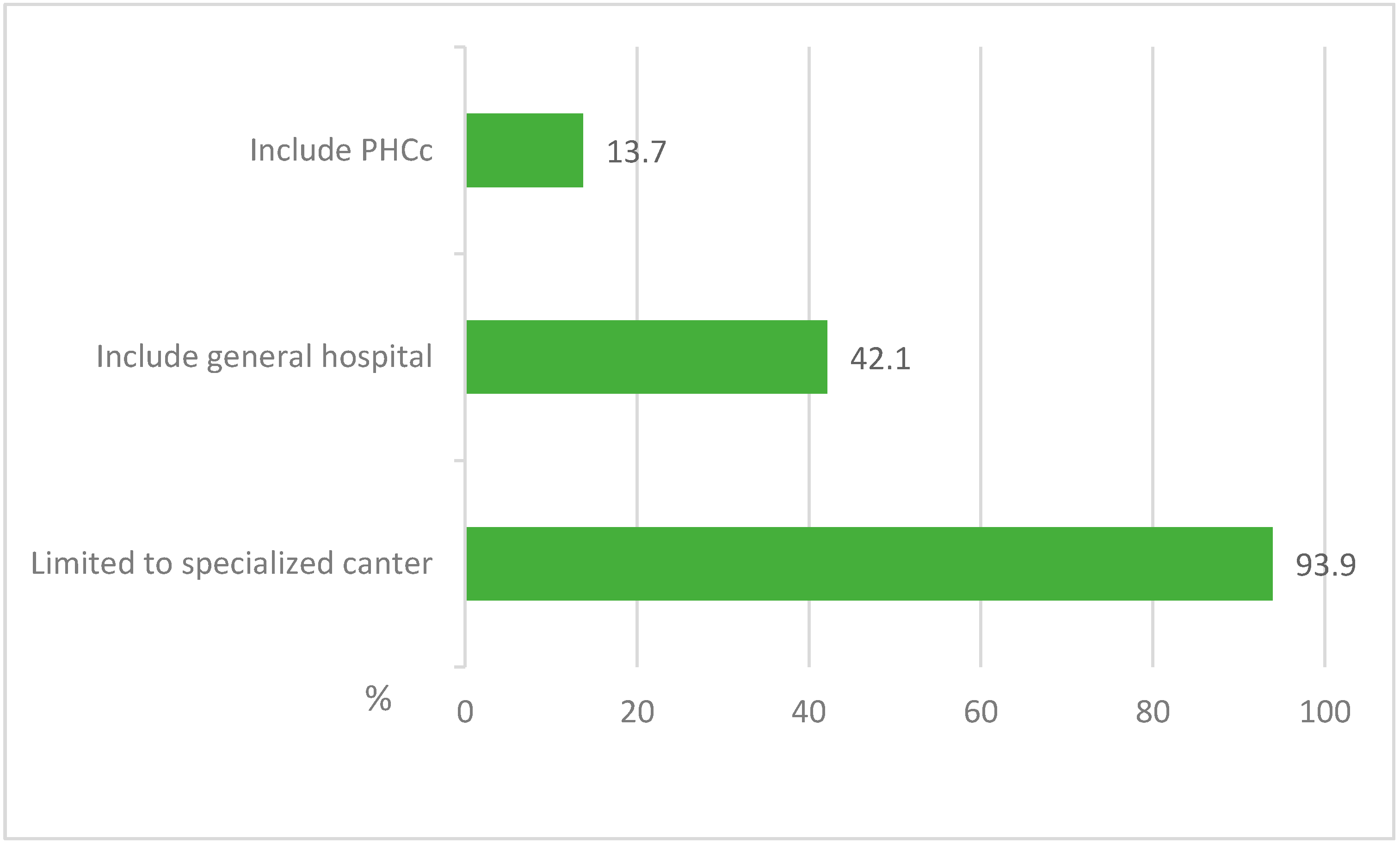
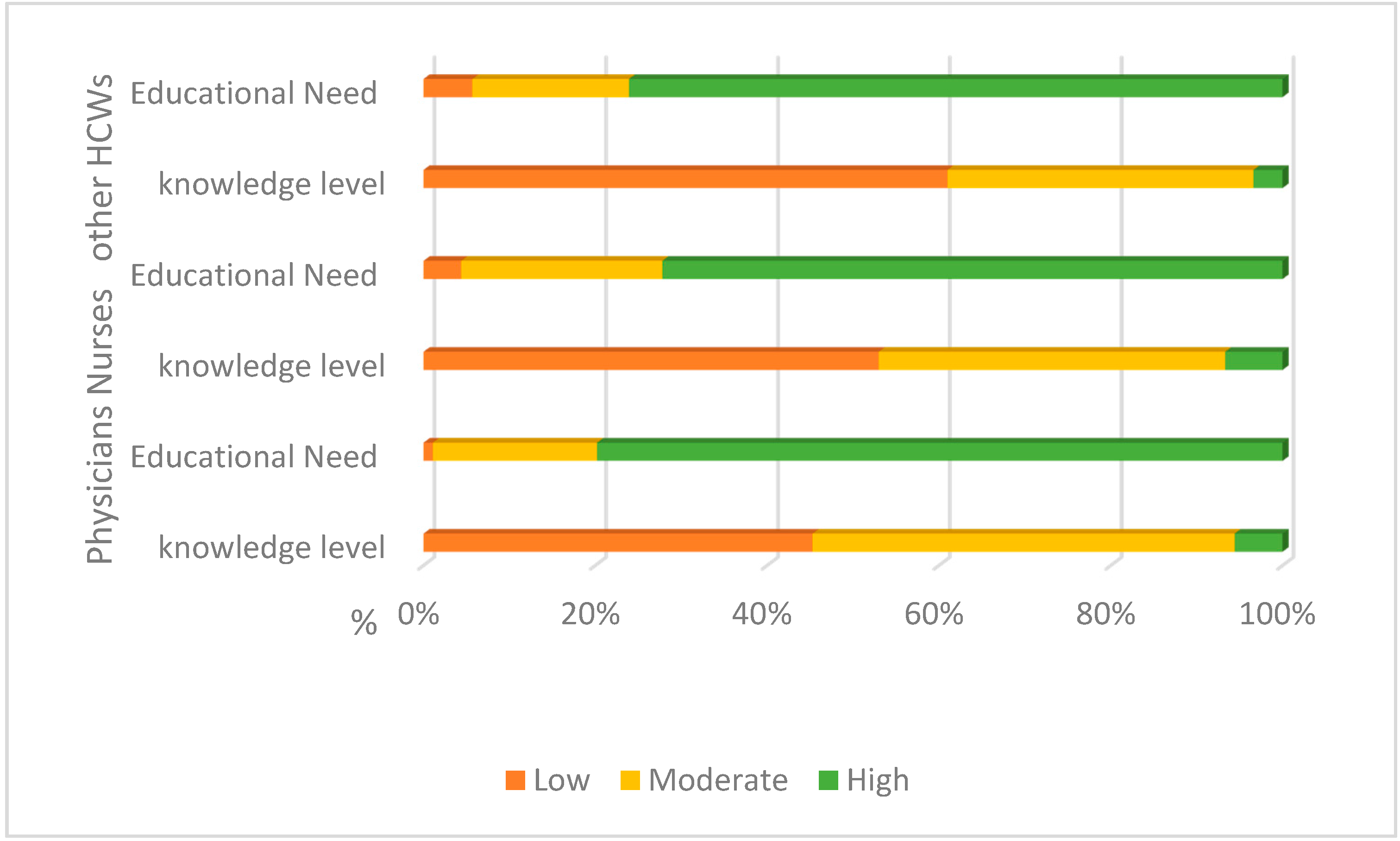
3.4. Educational Needs about Emerging Infectious Diseases
3.5. Attitudes to Infection Control Practices
3.6. Self-Reported Infection Control Practices
4. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Zaki, A.M.; van Boheemen, S.; Bestebroer, T.M.; Osterhaus, A.D.M.E.; Fouchier, R.A.M. Isolation of a Novel Coronavirus from a Man with Pneumonia in Saudi Arabia. N. Engl. J. Med. 2012, 367, 1814–1820. [Google Scholar] [CrossRef] [PubMed]
- Mailles, A.; Blanckaert, K.; Chaud, P.; van der Werf, S.; Lina, B.; Caro, V.; Campese, C.; Guéry, B.; Prouvost, H.; Lemaire, X.; et al. First Cases of Middle East Respiratory Syndrome Coronavirus (MERS-CoV) Infections in France, Investigations and Implications for the Prevention of Human-to-Human Transmission, France, May 2013. Available online: http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=20502 (accessed on 21 September 2016).
- Annicka, R.; Annette, L.; Christian, D.; Seilmaier, M.; Böhmer, M.; Graf, P.; Gold, H.; Wendtner, C.; Zanuzdana, A.; Schaade, L.; et al. Contact Investigation for Imported Case of Middle East Respiratory Syndrome, Germany. Emerg. Infect. Dis. 2014, 20. [Google Scholar] [CrossRef]
- Assiri, A.; McGeer, A.; Perl, T.M.; Price, C.S.; Al Rabeeah, A.A.; Cummings, D.A.; Alabdullatif, Z.N.; Assad, M.; Almulhim, A.; Makhdoom, H.; et al. Hospital outbreak of middle east respiratory syndrome coronavirus. N. Engl. J. Med. 2013, 369, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Memish, Z.A.; Zumla, A.I.; Assiri, A. Middle East respiratory syndrome coronavirus infections in health care workers. N. Engl. J. Med. 2013, 369, 884–886. [Google Scholar] [CrossRef] [PubMed]
- Hall, A.J.; Tokars, J.I.; Badreddine, S.A.; Saad, Z.B.; Furukawa, E.; Al Masri, M.; Haynes, L.M.; Gerber, S.I.; Kuhar, D.T.; Miao, C.; et al. Health care worker contact with MERS patient, Saudi Arabia. Emerg. Infect. Dis. 2014, 20, 2148–2151. [Google Scholar] [CrossRef] [PubMed]
- Bialek, S.R.; Allen, D.; Alvarado-Ramy, F.; Arthur, R.; Balajee, A.; Bell, D.; Best, S.; Blackmore, C.; Breakwell, L.; Cannons, A.; et al. First confirmed cases of Middle East respiratory syndrome coronavirus (MERS-CoV) infection in the United States, updated information on the epidemiology of MERS-CoV infection, and guidance for the public, clinicians, and public health authorities—May 2014. Am. J. Transplant. 2014, 14, 1693–1699. [Google Scholar]
- Alsahafi, A.J.; Cheng, A.C. The epidemiology of Middle East respiratory syndrome coronavirus in the Kingdom of Saudi Arabia, 2012–2015. Int. J. Infect. Dis. 2016, 45, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H. Institutional preparedness for infectious diseases and improving care. J. Korean Med. Assoc. 2015, 58, 606–610. [Google Scholar] [CrossRef]
- Kim, S.G. Healthcare workers infected with Middle East respiratory syndrome coronavirus and infection control. J. Korean Med. Assoc. 2015, 58, 647–654. [Google Scholar] [CrossRef]
- Khan, A.; Farooqui, A.; Guan, Y.; Kelvin, D.J. Emerging problems in infectious diseases lessons to learn from mers-cov outbreak in South Korea. J. Infect. Dev. Ctries. 2015, 9, 543–546. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y. Healthcare policy and healthcare utilization behavior to improve hospital infection control after the Middle East respiratory syndrome outbreak. J. Korean Med. Assoc. 2015, 58, 598–605. [Google Scholar] [CrossRef]

| Socio-Demographic Fetchers | Physicians | Nurses | Other HCWs * | Total | |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | |||
| Number | 267 (22) | 685 (56.3) | 264 (21.7) | 1216 (100) | |
| Gender: | |||||
| Male | 199 (74.5) | 299 (43.6) | 201 (76.1) | 699 (57.5) | |
| Female | 68 (25.5) | 386 (56.4) | 63 (23.9) | 517 (42.5) | |
| Work place: | |||||
| Hospital | 57 (21.3) | 204 (29.8) | 31 (11.7) | 292 (24) | |
| PHC | 207 (77.5) | 472 (68.9) | 228 (86.4) | 907 (74.6) | |
| Other | 3 (1.1) | 9 (1.3) | 5 (1.9) | 17 (1.4) | |
| Have you heard about Middle East Respiratory Syndrome (MERS)? | p ** | ||||
| Yes | 263 (98.5) | 677 (98.8) | 261 (98.9) | 1201 | 0.906 |
| No | 4 (1.5) | 8 (1.2) | 3 (1.1) | 15 | |
| MERS has been diagnosed in patients in the practice of the HCW: | |||||
| Yes | 75 (28.10) | 218 (31.8) | 58 (22) | 351 | 0.02 |
| No | 192 (71.9) | 462 (67.4) | 203 (76.9) | 857 | |
| Don’t Know | 0 (0) | 5 (0.7) | 3 (1.1) | 8 | |
| Do you think that Middle East Respiratory Syndrome (MERS) a problem in this community? | |||||
| Strongly agree | 118 (44.2) | 362 (52.8) | 145 (54.9) | 625 | 0.105 |
| Agree | 104 (39) | 230 (33.6) | 88 (33.3) | 422 | |
| Neutral | 24 (9) | 65 (9.5) | 18 (6.8) | 107 | |
| Disagree | 17 (6.4) | 23 (3.4) | 10 (3.8) | 50 | |
| Strongly disagree | 4 (1.5) | 5 (0.7) | 3 (1.1) | 12 | |
| The HCWs who had been investigated for MERS-CoV and the duration from sample taking and releasing the result: | |||||
| One day | 7 (23.3) | 54 (36.7) | 18 (45) | 79 | 0.013 |
| 2 days | 10 (33.3) | 34 (23) | 8 (20) | 52 | |
| 3 days | 9 (30) | 46 (31.2) | 9 (22.5) | 64 | |
| More | 4 (13.3) | 13 (8.8) | 5 (12.5) | 22 | |
| The impact of suspicion of having MERS-CoV on the HCWs work performance, social and psychological life: | |||||
| Work performance: | 17 (17.7) | 61 (63.5) | 18 (18.8) | 96 | 0.006 |
| Social life | 18 (16.1) | 72 (64.3) | 22 (19.6) | 112 | 0.001 |
| Psychological life | 18 (13.3) | 96 (71.1) | 21 (15.6) | 135 | 0.001 |
| Clinical experience of the HCWs in the last 2 years or less regarding: | |||||
| Working in place where MERS-CoV infected patient was diagnosed or admitted. | 75 (28.1) | 218 (31.8) | 58 (22) | 351 | 0.02 |
| Cared a MERS-CoV infected patient. | 24 (9) | 106 (15.5) | 15 (5.7) | 145 | <0.001 |
| After the MERS-CoV outbreak: | |||||
| Sometimes get scared of going to work for fear of contacting MERS-CoV patient. | 123 (46.1) | 448 (65.4) | 173 (65.5) | 744 | <0.001 |
| Sometimes avoid body contact whenever HCWs are in a public area. | 116 (43.4) | 421 (61.5) | 154 (58.3) | 691 | <0.001 |
| Knowledge about MERS-CoV Infection | Correct Responses | p ** | |||
|---|---|---|---|---|---|
| Physicians | Nurses | Other HCWs * | Total | ||
| N (%) | N (%) | N (%) | |||
| Indications of testing for MERS-CoV: | |||||
| Acute respiratory illness requiring ICU | 224 (83.9) | 552 (80.6) | 188 (71.2) | 964 | <0.001 |
| Acute respiratory illness requiring hospitalisation but not ICU | 153 (57.3) | 391 (57.1) | 154 (58.3) | 698 | <0.001 |
| Mild respiratory illness not requiring hospitalisation | 170 (63.7) | 316 (46.1) | 108 (40.9) | 594 | <0.001 |
| Mild acute respiratory illness where there is a history of contact with a confirmed MERS case | 203 (76) | 409 (59.7) | 175 (66.3) | 787 | <0.001 |
| Other acute non-respiratory illness in patients with a history of contact with a confirmed MERS case | 189 (70.8) | 437 (63.9) | 153 (58.2) | 779 | <0.001 |
| MERS-CoV infection: | |||||
| About 3–4 out of every 10 people reported with MERS-CoV have died. | 149 (55.8) | 345 (50.4) | 121 (45.8) | 615 | <0.001 |
| Some infected people had mild symptoms (such as cold-like symptoms) | 212 (79.4) | 441 (64.4) | 146 (55.3) | 799 | <0.001 |
| Most of the people who died had an underling medical condition | 196 (73.4) | 407 (59.4) | 149 (56.4) | 752 | <0.001 |
| MERS-CoV has spread from ill people to others through close contact | 233 (87.3) | 530 (77.4) | 189 (71.6) | 952 | <0.001 |
| The possibility of transmission through infected camel and bats | 194 (72.7) | 340 (49.6) | 122 (46.2) | 656 | <0.001 |
| Higher risk for getting MERS-CoV or having a severe case include pre-existing conditions such as diabetes; cancer, renal failure and patients taking immunosuppressive drugs. | 235 (88) | 476 (69.5) | 165 (62.5) | 876 | <0.001 |
| The incubation period for MERS is usually about 5 or 6 days but can be more | 183 (68.5) | 333 (48.6) | 100 (37.9) | 616 | <0.001 |
| MERS is spread through mosquito bite | 159 (59.6) | 284 (41.50) | 99 (37.5) | 542 | <0.001 |
| Some infected people had no symptoms | 127 (47.6) | 208 (30.4) | 79 (29.9) | 414 | <0.001 |
| MERS-CoV infected patient need isolation | 253 (94.8) | 616 (89.9) | 228 (86.4) | 1097 | <0.001 |
| Self-Reporting Infection Control Practice | Physicians | Nurses | Other HCWs * | Total | p ** |
|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | |||
| Hand washing after patient contact: | |||||
| Always | 161 (60.3) | 444 (64.8) | 160 (60.6) | 765 | 0.040 |
| Very Often | 69 (25.8) | 130 (19) | 50 (18.9) | 249 | |
| Sometimes | 33 (12.4) | 96 (14) | 40 (15.2) | 169 | |
| Rarely | 3 (1.1) | 11 (1.6) | 12 (4.5) | 26 | |
| Never | 1 (0.4) | 4 (0.6) | 2 (0.8) | 7 | |
| Wearing of surgical mask during patient contact: | |||||
| Always | 115 (43.1) | 308 (45) | 106 (40.2) | 529 | <0.001 |
| Very Often | 75 (28.1) | 157 (23) | 58 (22) | 290 | |
| Sometimes | 60 (22.5) | 162 (23.6) | 51 (19.3) | 273 | |
| Rarely | 14 (5.2) | 44 (6.4) | 32 (12.1) | 90 | |
| Never | 3 (1.1) | 14 (2) | 17 (6.4) | 34 | |
| Wearing of N95 mask during patient contact: | |||||
| Always | 118 (44.2) | 317 (46.3) | 105 (39.8) | 540 | 0.009 |
| Very Often | 57 (21.4) | 136 (19.9) | 53 (20.1) | 246 | |
| Sometimes | 38 (14.2) | 129 (18.8) | 51 (19.3) | 218 | |
| Rarely | 35 (13.1) | 76 (11.1) | 27 (10.2) | 138 | |
| Never | 19 (7.1) | 27 (3.9) | 28 (10.6) | 74 | |
| After the MERS outbreak, are the HCWs become more eager to apply infection control measures? | |||||
| Strongly Agree | 184 (68.9) | 429 (62.6) | 162 (61.4) | 775 | 0.12 |
| Agree | 72 (27) | 202 (29.5) | 78 (29.5) | 352 | |
| Do you have a guideline or protocol for caring for patients with MERS? | |||||
| Yes | 142 (53.2) | 234 (34.2) | 65 (24.6) | 441 | <0.001 |
| No | 62 (23.2) | 238 (34.7) | 98 (37.1) | 398 | |
| Don’t Know | 63 (23.6) | 213 (31.1) | 101 (38.3) | 441 | |
| HCWs training assessment: | |||||
| How to deal with an infectious disease outbreak. | 80 (30) | 152 (22.1) | 45 (17.8) | 277 | 0.011 |
| Infection control policies and procedures. | 98 (36.7) | 285 (41.6) | 68 (25.8) | 451 | <0.001 |
| Hand washing techniques. | 158 (59.2) | 389 (56.8) | 115 (43.6) | 662 | 0.001 |
| N95 mask wearing techniques. | 145 (54.3) | 317 (46.3) | 92 (34.8) | 554 | <0.001 |
| IN the last 12 months, the HCW who got an annual influenza vaccine. | 182 (68.2) | 403 (58.8) | 138 (52.3) | 723 | 0.001 |
| IN the last 3–5 years, the HCW who got Meningitis vaccine. | 209 (78.3) | 502 (73.3) | 194 (73.5) | 905 | 0.263 |
| HCW through his work career who ever had been took viral hepatitis (B) immunisation or examined for its antibodies. | 172 (64.4) | 331 (48.3) | 110 (41.7) | 613 | <0.001 |
| The barriers to infection control practices as addressed by HCWs | |||||
| Lack of knowledge about the mode of transmission of the disease MERS-CoV: | 240 (90) | 645 (94.2) | 238 (90.2) | 1123 | 0.118 |
| Not wearing mask while examine or contact with the patient: | 262 (98) | 647 (94.5) | 252 (95.5) | 1161 | <0.001 |
| No hand washing after examine or contact with the patient: | 260 (97.3) | 652 (95.2) | 250 (94.7) | 1162 | <0.001 |
| Limitation of infection control material: | 217 (81.3) | 603 (88) | 213 (80.7) | 1033 | 0.014 |
| Lack of policy and Procedures in infection control: | 227 (85) | 598 (87.3) | 236 (89.4) | 1061 | 0.003 |
| Insufficient training in infection control measurements: | 243 (91) | 633 (92.4) | 240 (90.9) | 1116 | 0.178 |
| Less commitment of health care workers to the policies and procedures: | 250 (93.6) | 659 (96.2) | 242 (98.4) | 1151 | <0.001 |
| Overcrowding in ER: | 258 (96.6) | 666 (97.2) | 246 (93.2) | 1170 | 0.010 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alsahafi, A.J.; Cheng, A.C. Knowledge, Attitudes and Behaviours of Healthcare Workers in the Kingdom of Saudi Arabia to MERS Coronavirus and Other Emerging Infectious Diseases. Int. J. Environ. Res. Public Health 2016, 13, 1214. https://doi.org/10.3390/ijerph13121214
Alsahafi AJ, Cheng AC. Knowledge, Attitudes and Behaviours of Healthcare Workers in the Kingdom of Saudi Arabia to MERS Coronavirus and Other Emerging Infectious Diseases. International Journal of Environmental Research and Public Health. 2016; 13(12):1214. https://doi.org/10.3390/ijerph13121214
Chicago/Turabian StyleAlsahafi, Abdullah J., and Allen C. Cheng. 2016. "Knowledge, Attitudes and Behaviours of Healthcare Workers in the Kingdom of Saudi Arabia to MERS Coronavirus and Other Emerging Infectious Diseases" International Journal of Environmental Research and Public Health 13, no. 12: 1214. https://doi.org/10.3390/ijerph13121214
APA StyleAlsahafi, A. J., & Cheng, A. C. (2016). Knowledge, Attitudes and Behaviours of Healthcare Workers in the Kingdom of Saudi Arabia to MERS Coronavirus and Other Emerging Infectious Diseases. International Journal of Environmental Research and Public Health, 13(12), 1214. https://doi.org/10.3390/ijerph13121214





