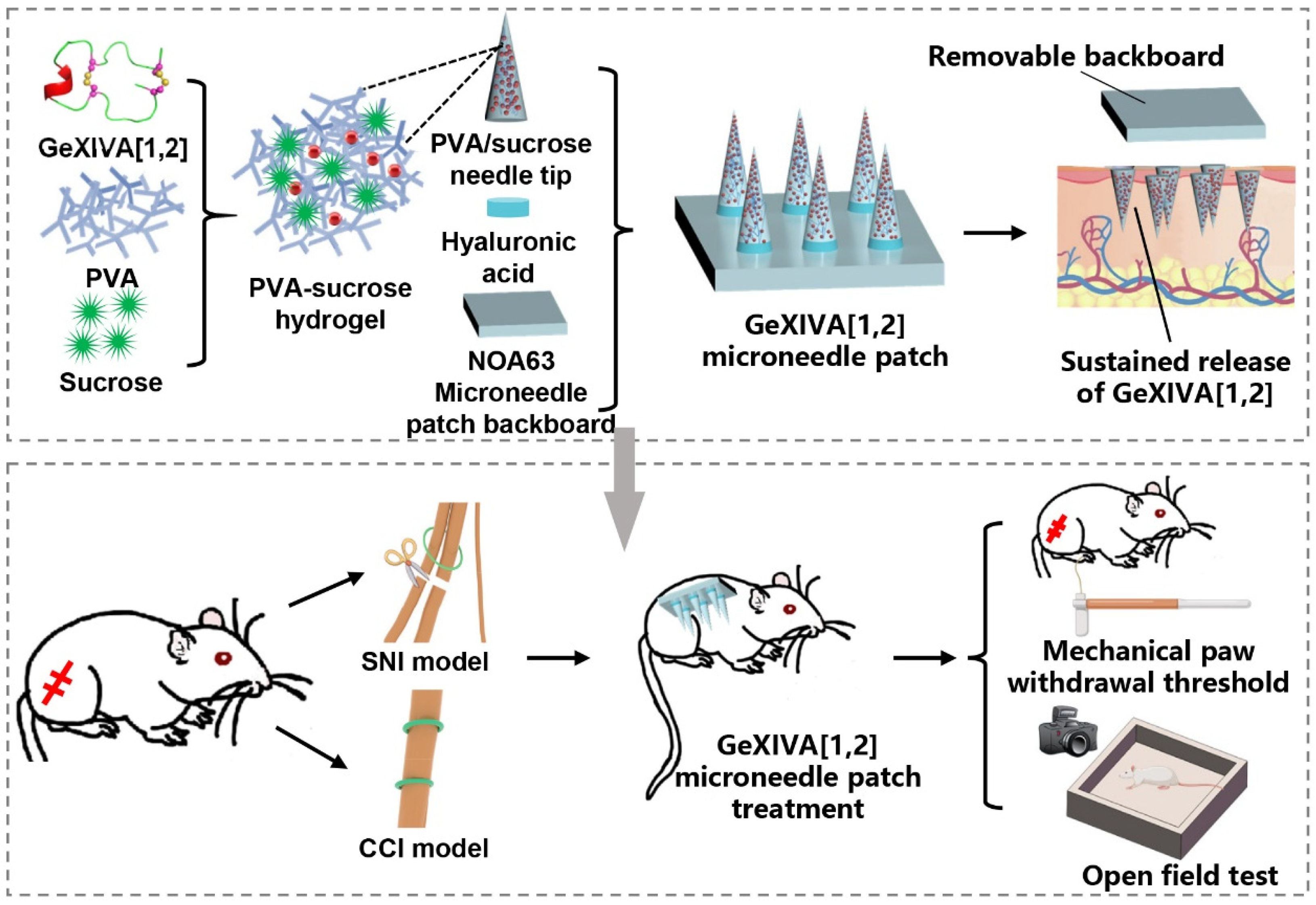
Sustained Release of αO-Conotoxin GeXIVA[1,2] via Hydrogel Microneedle Patch for Chronic Neuropathic Pain Management
Abstract
1. Introduction
2. Results
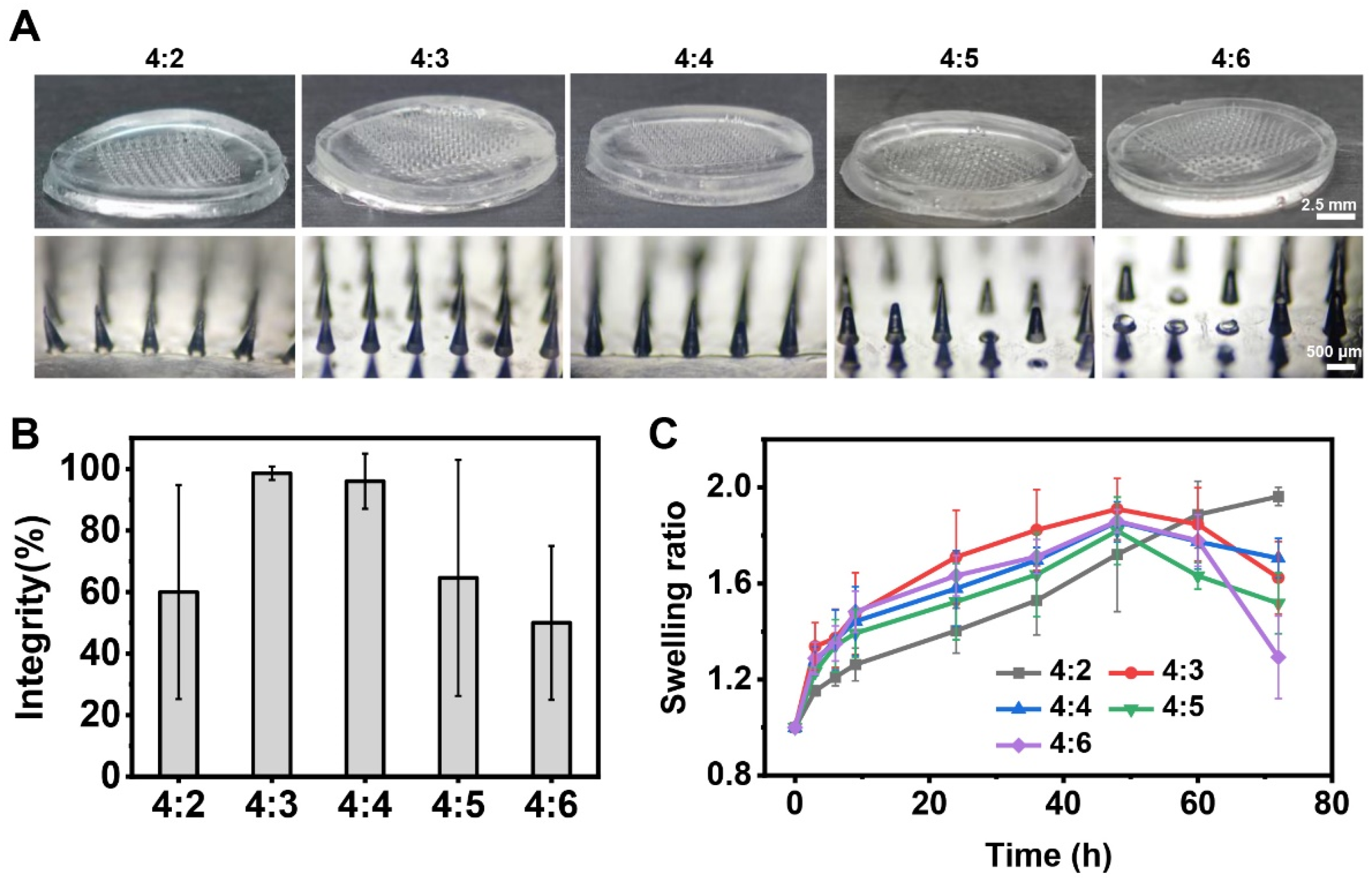
2.1. Optimization of Composition Ratios of Hydrogel Microneedle Patches
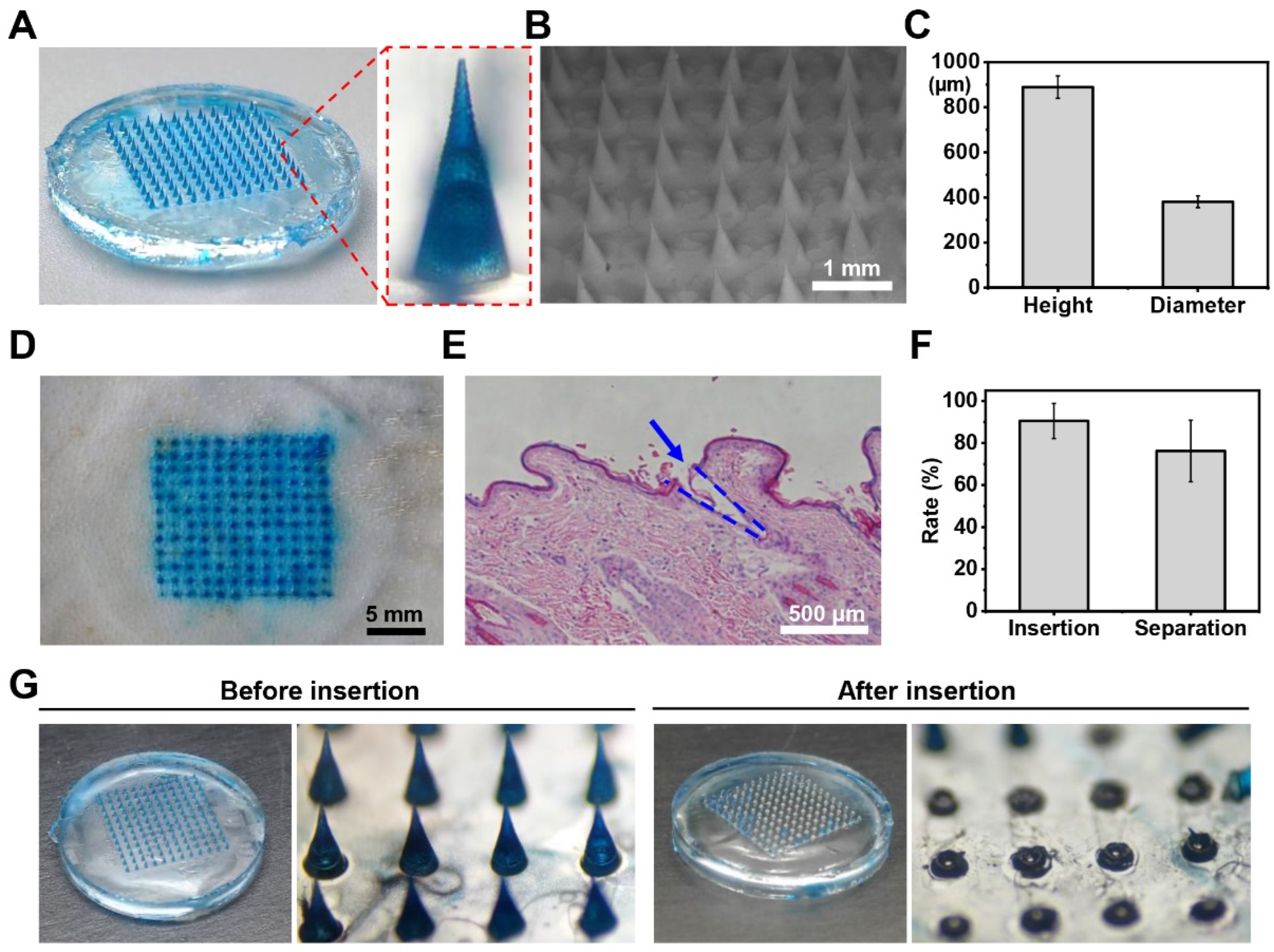
2.2. Fabrication and Characterization of Hydrogel Microneedle Patches
2.3. In Vitro Release of the GeXIVA[1,2] Microneedle Patches
2.4. Evaluation of Drug Release In Vivo
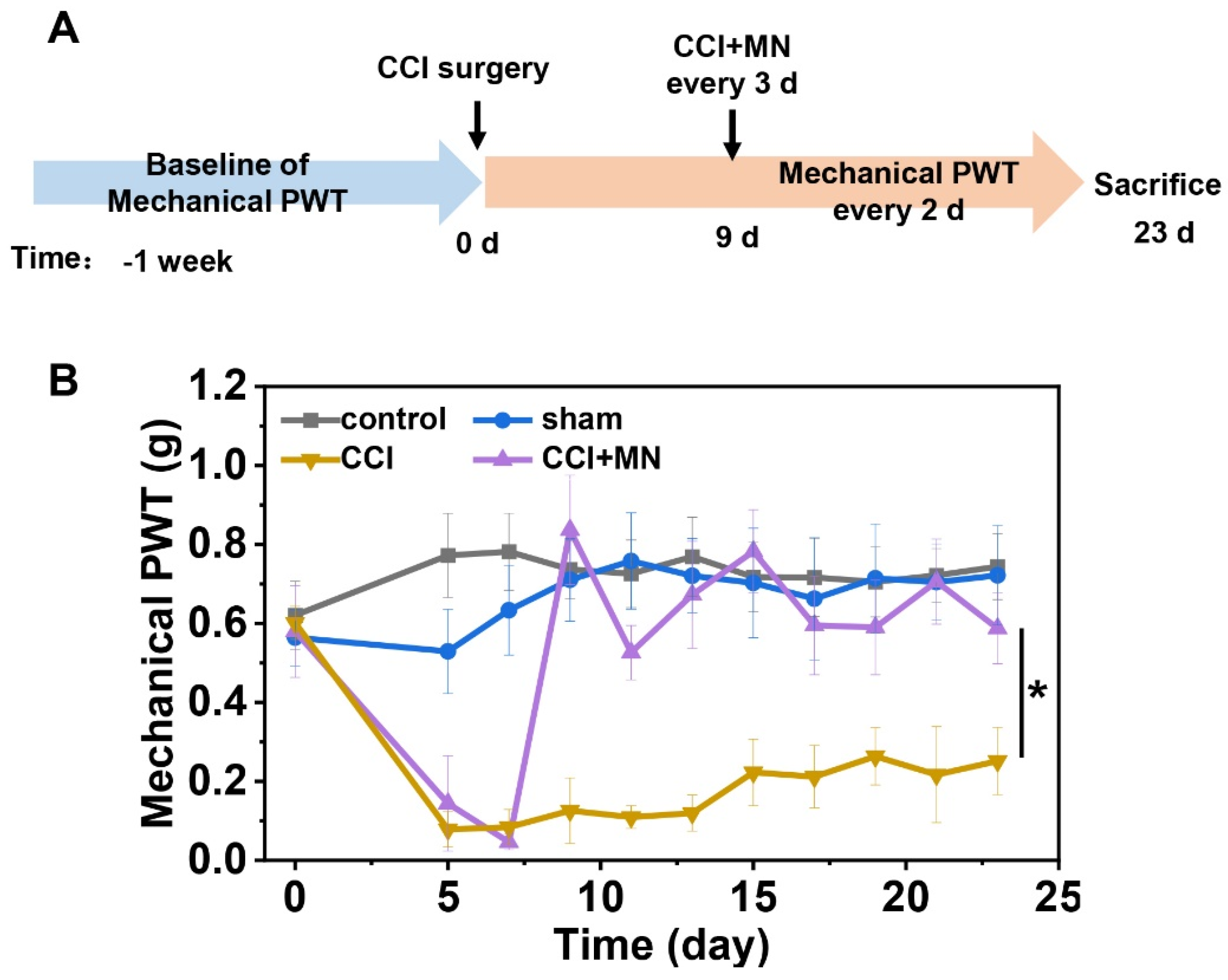
2.5. GeXIVA[1,2] Microneedle Patches for Neuropathic Pain Management
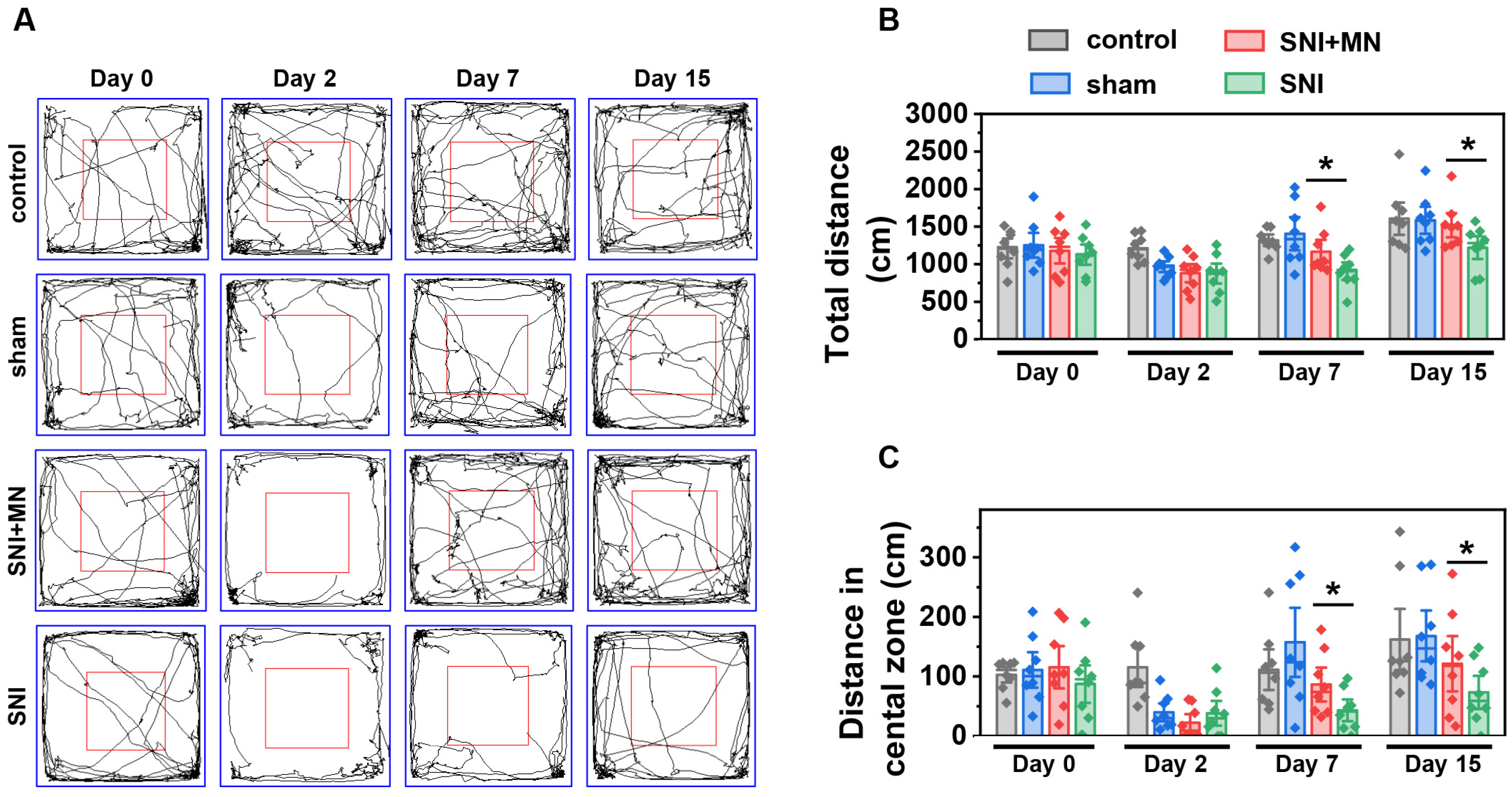
2.6. The Effect of GeXIVA[1,2] Microneedle Patch on Motor Function Recovery
3. Discussion
4. Materials and Methods
4.1. Materials
4.2. Fabrication of GeXIVA[1,2] Hydrogel Microneedle Patches
4.3. Exploration of Optimal Ratio of PVA–Sucrose Hydrogel
4.4. Characterizations of GeXIVA[1,2] Microneedle Patch
4.5. In Vitro Release Study of GeXIVA[1,2] from Hydrogel Microneedle Patches
4.6. Drug Release In Vivo
4.7. Mechanical Allodynia Testing
4.8. Animal Chronic Neuropathic Pain Models
4.9. Administration of GeXIVA[1,2] Microneedle Patches
4.10. Open Field Test
4.11. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| nAChR | nicotinic acetylcholine receptor |
| PVA | polyvinyl alcohol |
| NOA63 | Norland optical adhesive 63 |
| HA | hyaluronic acid |
| RP-HPLC | reverse-phase high-performance liquid chromatography |
| ESI-MS | electrospray-ionization mass spectroscopy |
| PBS | phosphate buffer saline |
| SNI | spared nerve injury |
| CCI | chronic constriction injury |
| PWT | paw withdrawal threshold |
| UV | ultraviolet |
| PDMS | polydimethylsiloxane |
| TFA | trifluoroacetic acid |
| SEM | scanning electron microscope |
| H&E | hematoxylin–eosin |
References
- Cohen, S.P.; Vase, L.; Hooten, W.M. Chronic pain: An update on burden, best practices, and new advances. Lancet 2021, 397, 2082–2097. [Google Scholar] [CrossRef] [PubMed]
- Glare, P.; Mahendran, M.; Weiss, A.D. Update on chronic pain management. Intern. Med. J. 2025, 55, 200–206. [Google Scholar] [CrossRef]
- Llorca-Torralba, M.; Camarena-Delgado, C.; Suárez-Pereira, I.; Bravo, L.; Mariscal, P.; Garcia-Partida, J.A.; López-Martín, C.; Wei, H.; Pertovaara, A.; Mico, J.A.; et al. Pain and depression comorbidity causes asymmetric plasticity in the locus coeruleus neurons. Brain 2022, 145, 154–167. [Google Scholar] [CrossRef]
- Sun, L.; Liu, R.; Guo, F.; Wen, M.Q.; Ma, X.L.; Li, K.Y.; Sun, H.; Xu, C.L.; Li, Y.Y.; Wu, M.Y.; et al. Parabrachial nucleus circuit governs neuropathic pain-like behavior. Nat. Commun. 2020, 11, 5974. [Google Scholar] [CrossRef]
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.B.; et al. Neuropathic pain. Nat. Rev. Dis. Primers 2017, 3, 17002. [Google Scholar] [CrossRef] [PubMed]
- Attal, N.; Bouhassira, D.; Colvin, L. Advances and challenges in neuropathic pain: A narrative review and future directions. Br. J. Anaesth. 2023, 131, 79–92. [Google Scholar] [CrossRef]
- Cohen, S.P.; Mao, J. Neuropathic pain: Mechanisms and their clinical implications. BMJ 2014, 348, f7656. [Google Scholar] [CrossRef] [PubMed]
- Varadi, G. Mechanism of Analgesia by Gabapentinoid Drugs: Involvement of Modulation of Synaptogenesis and Trafficking of Glutamate-Gated Ion Channels. J. Pharmacol. Exp. Ther. 2024, 388, 121–133. [Google Scholar] [CrossRef]
- Srivastava, A.B.; Mariani, J.J.; Levin, F.R. New directions in the treatment of opioid withdrawal. Lancet 2020, 395, 1938–1948. [Google Scholar] [CrossRef]
- Fiorotti, H.B.; Figueiredo, S.G.; Campos, F.V.; Pimenta, D.C. Cone snail species off the Brazilian coast and their venoms: A review and update. J. Venom. Anim. Toxins Incl. Trop. Dis. 2023, 29, e20220052. [Google Scholar] [CrossRef]
- Luo, S.; Zhangsun, D.; Harvey, P.J.; Kaas, Q.; Wu, Y.; Zhu, X.; Hu, Y.; Li, X.; Tsetlin, V.I.; Christensen, S.; et al. Cloning, synthesis, and characterization of αO-conotoxin GeXIVA, a potent α9α10 nicotinic acetylcholine receptor antagonist. Proc. Natl. Acad. Sci. USA 2015, 112, E4026–E4035. [Google Scholar] [PubMed]
- Li, Z.; Han, X.; Hong, X.; Li, X.; Gao, J.; Zhang, H.; Zheng, A. Lyophilization Serves as an Effective Strategy for Drug Development of the α9α10 Nicotinic Acetylcholine Receptor Antagonist α-Conotoxin GeXIVA[1,2]. Mar. Drugs 2021, 19, 121. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Li, X.; Zhangsun, D.; Yu, G.; Su, R.; Luo, S. The α9α10 Nicotinic Acetylcholine Receptor Antagonist αO-Conotoxin GeXIVA[1,2] Alleviates and Reverses Chemotherapy-Induced Neuropathic Pain. Mar. Drugs 2019, 17, 265. [Google Scholar] [CrossRef]
- Wang, H.; Li, X.; Qiao, Y.; Wang, M.; Wang, W.; McIntosh, J.M.; Zhangsun, D.; Luo, S. αO-Conotoxin GeXIVA[1,2] Reduced Neuropathic Pain and Changed Gene Expression in Chronic Oxaliplatin-Induced Neuropathy Mice Model. Mar. Drugs 2024, 22, 49. [Google Scholar] [CrossRef]
- Li, X.; Hu, Y.; Wu, Y.; Huang, Y.; Yu, S.; Ding, Q.; Zhangsun, D.; Luo, S. Anti-hypersensitive effect of intramuscular administration of αO-conotoxin GeXIVA[1,2] and GeXIVA [1,4] in rats of neuropathic pain. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2016, 66, 112–119. [Google Scholar]
- Wang, M.Z.; Li, X.D.; Wang, H.B.; Luo, S.L.; Zhangsun, D.T. Preliminaryevaluating toxicity of αO-conotoxin GeXIVA[1,2] in mice. Toxicon 2019, 158, S80. [Google Scholar]
- Imperial, J.S.; Bansal, P.S.; Alewood, P.F.; Daly, N.L.; Craik, D.J.; Sporning, A.; Terlau, H.; López-Vera, E.; Bandyopadhyay, P.K.; Olivera, B.M. A novel conotoxin inhibitor of Kv1.6 channel and nAChR subtypes defines a new superfamily of conotoxins. Biochemistry 2006, 45, 8331–8340. [Google Scholar] [CrossRef]
- Lin, J.; Chen, S.; Butt, U.D.; Yan, M.; Wu, B. A comprehensive review on ziconotide. Heliyon 2024, 10, e31105. [Google Scholar] [CrossRef]
- McLenon, J.; Rogers, M.A.M. The fear of needles: A systematic review and meta-analysis. J. Adv. Nurs. 2019, 75, 30–42. [Google Scholar]
- Vora, L.K.; Sabri, A.H.; Naser, Y.; Himawan, A.; Hutton, A.R.J.; Anjani, Q.K.; Volpe-Zanutto, F.; Mishra, D.; Li, M.; Rodgers, A.M.; et al. Long-acting microneedle formulations. Adv. Drug Deliv. Rev. 2023, 201, 115055. [Google Scholar]
- Song, K.; Hao, Y.; Tan, X.; Huang, H.; Wang, L.; Zheng, W. Microneedle-mediated delivery of Ziconotide-loaded liposomes fused with exosomes for analgesia. J. Control. Release 2023, 356, 448–462. [Google Scholar] [CrossRef] [PubMed]
- Tehrani, F.; Teymourian, H.; Wuerstle, B.; Kavner, J.; Patel, R.; Furmidge, A.; Aghavali, R.; Hosseini-Toudeshki, H.; Brown, C.; Zhang, F.; et al. An integrated wearable microneedle array for the continuous monitoring of multiple biomarkers in interstitial fluid. Nat. Biomed. Eng. 2022, 6, 1214–1224. [Google Scholar] [CrossRef]
- Wang, C.; Yang, Y.; Zhang, J.; Zhang, H.; Wang, Q.; Ma, S.; Zhao, P.; Li, Z.; Liu, Y. Microneedles at the Forefront of Next Generation Theranostics. Adv. Sci. 2025, e2412140. [Google Scholar] [CrossRef] [PubMed]
- He, R.; Liu, H.; Fang, T.; Niu, Y.; Zhang, H.; Han, F.; Gao, B.; Li, F.; Xu, F. A Colorimetric Dermal Tattoo Biosensor Fabricated by Microneedle Patch for Multiplexed Detection of Health-Related Biomarkers. Adv. Sci. 2021, 8, e2103030. [Google Scholar] [CrossRef]
- He, R.; Niu, Y.; Li, Z.; Li, A.; Yang, H.; Xu, F.; Li, F. A Hydrogel Microneedle Patch for Point-of-Care Testing Based on Skin Interstitial Fluid. Adv. Healthc. Mater. 2020, 9, e1901201. [Google Scholar] [CrossRef]
- Ghosh, S.; Kumar, N.; Chattopadhyay, S. Electrically conductive “SMART” hydrogels for on-demand drug delivery. Asian J. Pharm. Sci. 2025, 20, 101007. [Google Scholar] [CrossRef]
- Zhong, Y.; Lin, Q.; Yu, H.; Shao, L.; Cui, X.; Pang, Q.; Zhu, Y.; Hou, R. Construction methods and biomedical applications of PVA-based hydrogels. Front. Chem. 2024, 12, 1376799. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Sasaki, S. Swelling and mechanical properties of physically crosslinked poly(vinyl alcohol) hydrogels. Proc. Inst. Mech. Eng. Part H J. Eng. Med. 2015, 229, 828–844. [Google Scholar] [CrossRef]
- Zhao, J.; Li, Y.; Wang, M. Fabrication of robust transparent hydrogel with stretchable, self-healing, easily recyclable and adhesive properties and its application. Mater. Res. Bull. 2019, 112, 292–296. [Google Scholar] [CrossRef]
- Oltulu, P.; Ince, B.; Kokbudak, N.; Findik, S.; Kilinc, F. Measurement of epidermis, dermis, and total skin thicknesses from six different body regions with a new ethical histometric technique. Turk. J. Plast. Surg. 2018, 26, 56–61. [Google Scholar]
- Beebe, J.A.; Kronman, C.; Mahmud, F.; Basch, M.; Hogan, M.; Li, E.; Ploski, C.; Simons, L.E. Gait Variability and Relationships With Fear, Avoidance, and Pain in Adolescents With Chronic Pain. Phys. Ther. 2021, 101, pzab012. [Google Scholar] [PubMed]
- Ganguly, A.; McEwen, C.; Troy, E.L.; Colburn, R.W.; Caggiano, A.O.; Schallert, T.J.; Parry, T.J. Recovery of sensorimotor function following sciatic nerve injury across multiple rat strains. J. Neurosci. Methods 2017, 275, 25–32. [Google Scholar] [PubMed]
- Yu, S.; Wu, Y.; Xu, P.; Wang, S.; Zhangsun, D.; Luo, S. Effects of serum, enzyme, thiol, and forced degradation on the stabilities of αO-Conotoxin GeXIVA[1,2] and GeXIVA [1,4]. Chem. Biol. Drug Des. 2018, 91, 1030–1041. [Google Scholar]
- Pei, S.; Wang, N.; Mei, Z.; Zhangsun, D.; Craik, D.J.; McIntosh, J.M.; Zhu, X.; Luo, S. Conotoxins Targeting Voltage-Gated Sodium Ion Channels. Pharmacol. Rev. 2024, 76, 828–845. [Google Scholar] [CrossRef] [PubMed]
- Tietze, A.A.; Tietze, D.; Ohlenschläger, O.; Leipold, E.; Ullrich, F.; Kühl, T.; Mischo, A.; Buntkowsky, G.; Görlach, M.; Heinemann, S.H.; et al. Structurally diverse μ-conotoxin PIIIA isomers block sodium channel NaV 1.4. Angew. Chem.-Int. Ed. 2012, 51, 4058–4061. [Google Scholar]
- Tran, H.N.T.; McMahon, K.L.; Deuis, J.R.; Vetter, I.; Schroeder, C.I. Structural and functional insights into the inhibition of human voltage-gated sodium channels by μ-conotoxin KIIIA disulfide isomers. J. Biol. Chem. 2022, 298, 101728. [Google Scholar]
- Vetter, I.; Dekan, Z.; Knapp, O.; Adams, D.J.; Alewood, P.F.; Lewis, R.J. Isolation, characterization and total regioselective synthesis of the novel μO-conotoxin MfVIA from Conus magnificus that targets voltage-gated sodium channels. Biochem. Pharmacol. 2012, 84, 540–548. [Google Scholar]
- Wang, S.; Zhu, X.; Zhangsun, M.; Wu, Y.; Yu, J.; Harvey, P.J.; Kaas, Q.; Zhangsun, D.; Craik, D.J.; Luo, S. Engineered Conotoxin Differentially Blocks and Discriminates Rat and Human α7 Nicotinic Acetylcholine Receptors. J. Med. Chem. 2021, 64, 5620–5631. [Google Scholar]
- Li, L.; Li, Z.; Guo, Y.; Zhang, K.; Mi, W.; Liu, J. Preparation of uniform-sized GeXIVA[1,2]-loaded PLGA microspheres as long-effective release system with high encapsulation efficiency. Drug Deliv. 2022, 29, 2283–2295. [Google Scholar] [CrossRef]
- Dixon, W.J. Efficient analysis of experimental observations. Annu. Rev. Pharmacol. Toxicol. 1980, 20, 441–462. [Google Scholar]
- Richner, M.; Bjerrum, O.J.; Nykjaer, A.; Vaegter, C.B. The spared nerve injury (SNI) model of induced mechanical allodynia in mice. J. Vis. Exp. 2011, 54, 3092. [Google Scholar]
- Bennett, G.J.; Xie, Y.K. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 1988, 33, 87–107. [Google Scholar] [CrossRef] [PubMed]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
He, R.; Li, M.; Li, W.; Li, W.; Xiao, S.; Cao, Q.; Wang, H.; Zhangsun, D.; Luo, S. Sustained Release of αO-Conotoxin GeXIVA[1,2] via Hydrogel Microneedle Patch for Chronic Neuropathic Pain Management. Mar. Drugs 2025, 23, 161. https://doi.org/10.3390/md23040161
He R, Li M, Li W, Li W, Xiao S, Cao Q, Wang H, Zhangsun D, Luo S. Sustained Release of αO-Conotoxin GeXIVA[1,2] via Hydrogel Microneedle Patch for Chronic Neuropathic Pain Management. Marine Drugs. 2025; 23(4):161. https://doi.org/10.3390/md23040161
Chicago/Turabian StyleHe, Rongyan, Mingjuan Li, Weitao Li, Wenqi Li, Shuting Xiao, Qiuyu Cao, Huanbai Wang, Dongting Zhangsun, and Sulan Luo. 2025. "Sustained Release of αO-Conotoxin GeXIVA[1,2] via Hydrogel Microneedle Patch for Chronic Neuropathic Pain Management" Marine Drugs 23, no. 4: 161. https://doi.org/10.3390/md23040161
APA StyleHe, R., Li, M., Li, W., Li, W., Xiao, S., Cao, Q., Wang, H., Zhangsun, D., & Luo, S. (2025). Sustained Release of αO-Conotoxin GeXIVA[1,2] via Hydrogel Microneedle Patch for Chronic Neuropathic Pain Management. Marine Drugs, 23(4), 161. https://doi.org/10.3390/md23040161







