Natural Products Derived from Marine Sponges with Antitumor Potential against Lung Cancer: A Systematic Review
Abstract
1. Introduction
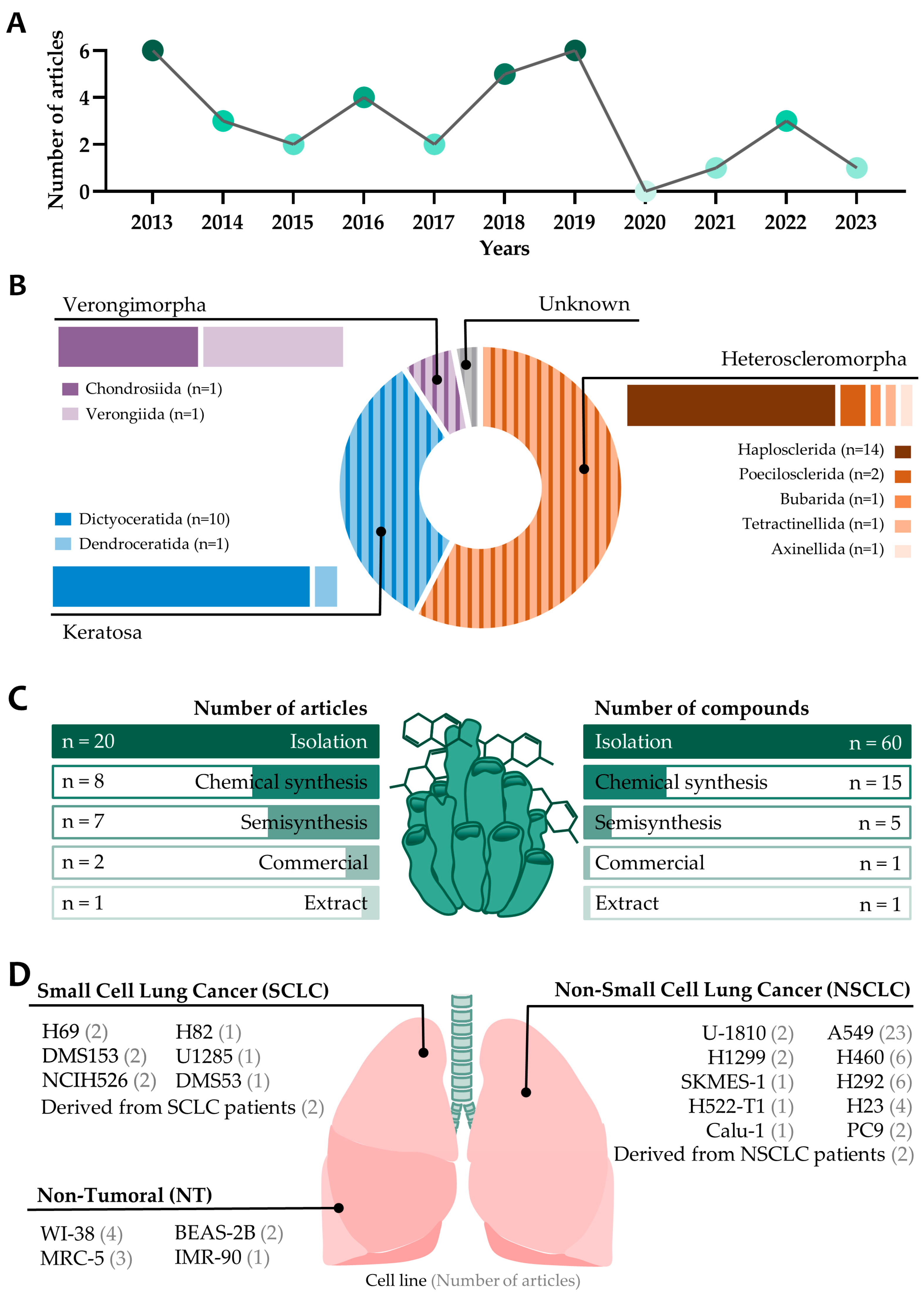
2. Results
2.1. Order Heterosclemorpha
| Sponge | Compounds | Chemical Class | Methods of Production | Cell line (NSCLC/SCLC) | IC50 | In Vivo * | Molecular Mechanism | Ref. |
|---|---|---|---|---|---|---|---|---|
| Xestospongia sp. | renieramycin M (1) and 5-O-acetylated hydroquinone derivative (2) | 1: Bistetrahydroisoquinolinequinone alkaloid 2: Hydroquinone derivative | 1: Isolation 2: Semisynthesis. Chemical modification of (1) | H23 (NSCLC) | 1 and 2: ~1 μM (24 h) | ✗ | (2) reduced the accidental necrosis-inducing effect while preserving the apoptosis-inducing effect of (1). | [11] |
| Xestospongia sp. | renieramycin M (1), jorunnamycin A (3), and 22-O-(4-pyridinecarbonyl) ester derivative of jorunnamycin A (4) | Alkaloid | 1 and 3: Isolation 4: Semisynthesis. Chemical modification of (2) | H292 and H460 (NSCLC) | 1: 23 ± 4 and 8.3 ± 0.6 3: 220 ± 20 and 160 ± 10 4: 1.1 ± 0.1 and 1.6 ± 0.3 IC50 H292 and H460 (nM), respectively (72 h) | ✗ | NR | [12] |
| Xestospongia sp. | renieramycin M (1), 5-O-acetyl ester (2), and 5-O-propanoyl ester (5) derivatives | Alkaloid | 1: Isolation 2 and 5: Semisynthesis. Chemical modification of (2) | H292 and H460 (NSCLC) | 1: 24 ± 1 and 6.5 ± 0.4 2: 3 ± 0.6 and 3.6 ± 0.6 5: 2.3 ± 0.4 and 5.1 ± 0.5 IC50 H292 and H460 (nM), respectively (72 h) | ✗ | NR | [13] |
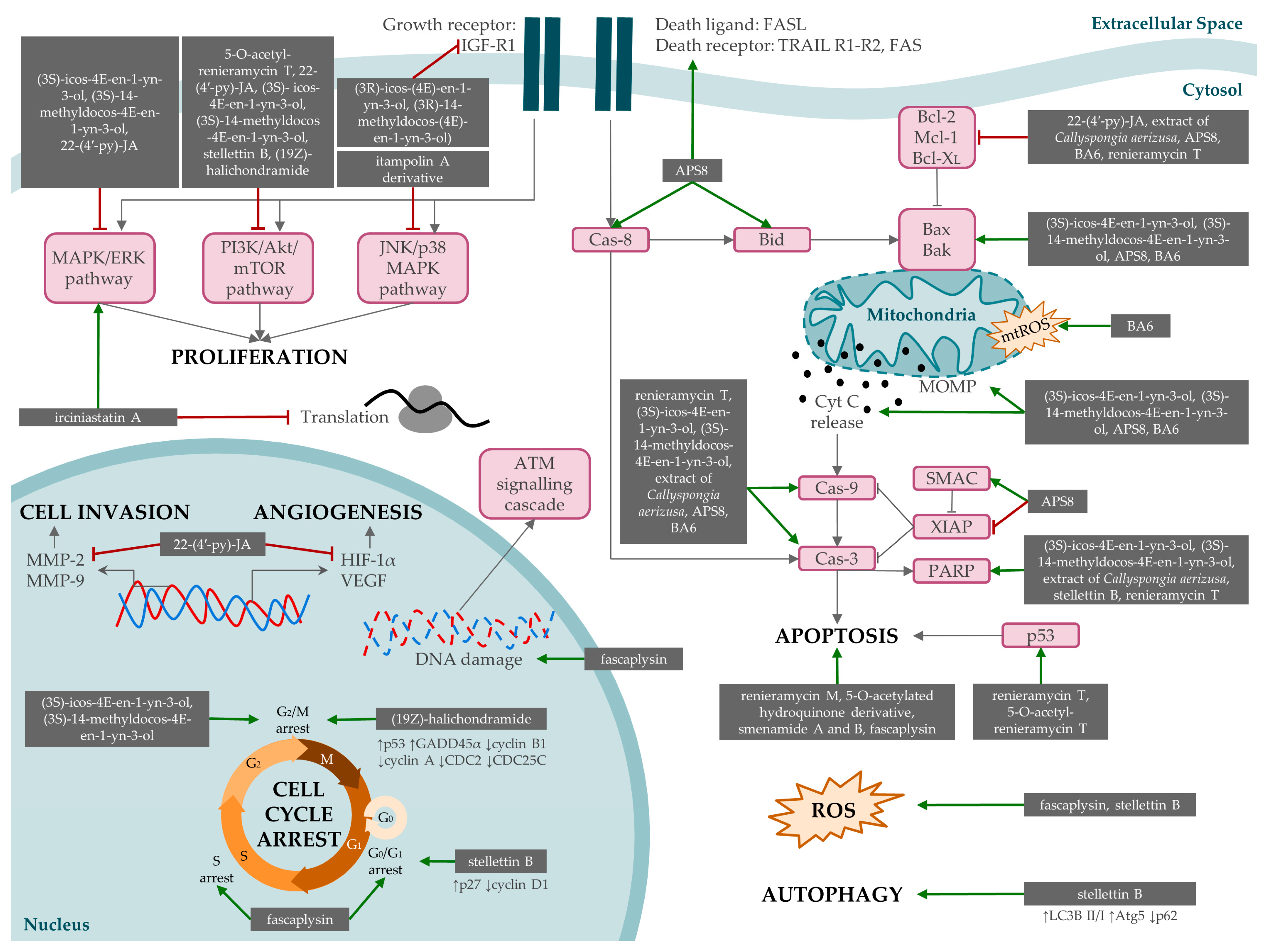
| Xestospongia sp. | renieramycin T (6) | Tetrahydroisoquinoline alkaloid | Isolated | H460, H292, H23, A549 (NSCLC), and BEAS-2B (NT) | 1.93 ± 0.4, 0.88 ± 0.06, 2.47 ± 0.14, 3.77 ± 0.38, 6.42 ± 0.65 IC50 H460, H292, H23, A549, and BEAS-2B (μM), respectively (24 h) | ✗ | Apoptosis induction through Mcl-1 (antiapoptotic protein), proteasomal degradation, and activation of p53, caspase-9 and -3, and PARP. | [14] |
| Xestospongia sp. | 5-O-acetyl-renieramycin T (7) | Alkaloid | Semisynthesis. Chemical modification of renieramycin T | H292, A549, and H23 (NSCLC) | 0.66 ± 0.26, 33.24 ± 4.75, 33.77 ± 2.22 IC50 H292, A549, and H23 (μM), respectively | ✗ | Induction of p53-dependent apoptosis, suppressing expression of CSC markers and depleting AKT signal. | [15] |
| Xestospongia sp. | 22-(4′-pyridinecarbonyl) jorunnamycin A (22-(4′-py)-JA) (4) | Tetrahydroisoquinoline derivative | Semisynthesis. Chemical modification of JA | A549, H460, and H292 (NSCLC) | 14.43 ± 0.68, 18.9 ± 0.76, 16.95 ± 0.41 IC50 A549, H460, and H292 (nM), respectively (48 h) | ✗ | Induction of apoptosis in an ERK/MEK/Bcl-2-dependent manner. | [16] |
| Xestospongia sp. | 22-(4′-pyridinecarbonyl) jorunnamycin A (22-(4′-py)-JA) (4) | Tetrahydroisoquinoline derivative | Semisynthesis. Chemical modification of JA | A549 and H460 (NSCLC) | 810 ± 33, 19 ± 1, and 11 ± 0.5 IC50 A549 (nM) at 24, 48, and 72 h, respectively 835 ± 30, 14 ± 1, and 12 ± 0.4 IC50 H460 (nM) at 24, 48, and 72 h, respectively | ✓ | Suppression of AKT/mTOR/p70S6K signaling, leading to the downregulation of MMP-2 and MMP-9, HIF-1α, and VEGF. Reduction of in vivo metastasis. | [17] |
| Xestospongia testudinaria | langcosterol A (8), xestosterol (9), and 24-hydroperoxy-24-vinyl cholesterol (10) | Sterol | Isolation | A549 (NSCLC) and WI-38 (NT) | 8: 63.1 and 68 9: >100 and >100 10: 29 and 43.4 IC50 (μM) A549 and WI-38, respectively (72 h) | ✗ | NR | [20] |
| Cribrochalina vasculum | (3S)-icos-4E-en-1-yn-3-ol (11) and (3S)-14-methyldocos-4E-en-1-yn-3-ol (12) | Acetylenic alcohol | Isolation | U-1810 (NSCLC), U-1285, H69, H82 (SCLC), WI-38, and BEAS-2B (NT) | 11: 0.5, 1.6, 2.2, 1.1, 7.3, and 12.9 12: 0.8, 1.8, 1.1, 1.1, 9.7, and N/A IC50 (μM) U-1810, U-1285, H69, H82, WI-38, and BEAS-2B, respectively (72 h) | ✗ | Induction of apoptosis involving cleavage of caspase-9, caspase3, and PARP. Conformational changes in Bak and Bax and loss of mitochondrial potential and cytochrome release. Decreased phosphorylation of Akt, mTOR, and ERK and increased phosphorylation of JNK. Cell cycle arrest in G2/M. | [21] |
| Cribrochalina vasculum | (3R)-icos-(4E)-en-1-yn-3-ol (13) and (3R)-14-methyldocos-(4E)-en-1-yn-3-ol) (14) | Acetylenic alcohol | Isolation | U-1810 (NSCLC) | 13: 1.5 μM 14: 15.1 μM (72 h) | ✗ | (13) Inhibition of IGF-1R phosphorylation, thus reducing pro-survival signaling. | [22] |
| Callyspongia aerizusa | methanol extraction | Ergosteroid (suggested to suppress cell viability) | Extract | A549 (NSCLC) | 9.38 μg/mL (24 h) | ✗ | Induction of apoptosis. Increase in PARP-1 and caspase-3 and -9 and decrease in Bcl-2. | [23] |
| Acanthostrongylophora ingens | ingenine F (15) | 1,2,3,4-tetrahydro-β-carboline (THβCs) alkaloid | Isolation | A549 (NSCLC) | 2.37 μM | ✗ | NR | [24] |
| Reniera sarai renamed to Haliclona (Rhizoneira) sarai | analog of 3-alkylpyridinium polymer (APS8) (16) | Polymeric alkylpyridinium salt | Chemical synthesis | A549 and SKMES-1 (NSCLC) and MRC-5 (NT) | 375 ± 4.89, 362 ± 9.29, and >1000 IC50 (nM) A549, SKMES-1, and MRC-5, respectively (48 h) | ✗ | Apoptosis, mitochondrial membrane depolarization, upregulation of several proapoptotic proteins, downregulation of antiapoptotic proteins, and activation of caspase-9. | [25] |
| Petrosia sp. | petrosynoic acid A (17), petrosynoic acid B (18), petrosynoic acid C (19), petrosynoic acid D (20), pellynol A (21), pellynol C (22), pellynol D (23), pellynol F (24), and pellynol I (25) | 17–20: (−)-petrosynoic acids 21–25: pellynols | Isolation | H522-T1 and H460 (NSCLC) and IMR-90 (NT) | 17: 5.5, 3.4, and 0.4 18: 8.4, 7.3, and 0.4 19: 4.6, 3.1, and 0.3 20: >10, >10, and 0.2 21: 0.8, 0.4, and 0.4 22: 0.6, 1, and 0.3 23: 1.1, 0.7, and 0.5 24: 2.7, 1.2, and 1.6 25: 1.2, 0.8, and N/A IC50 (μM) H522-T1, A549, and IMR-90 (72 h) | ✗ | NR | [26] |
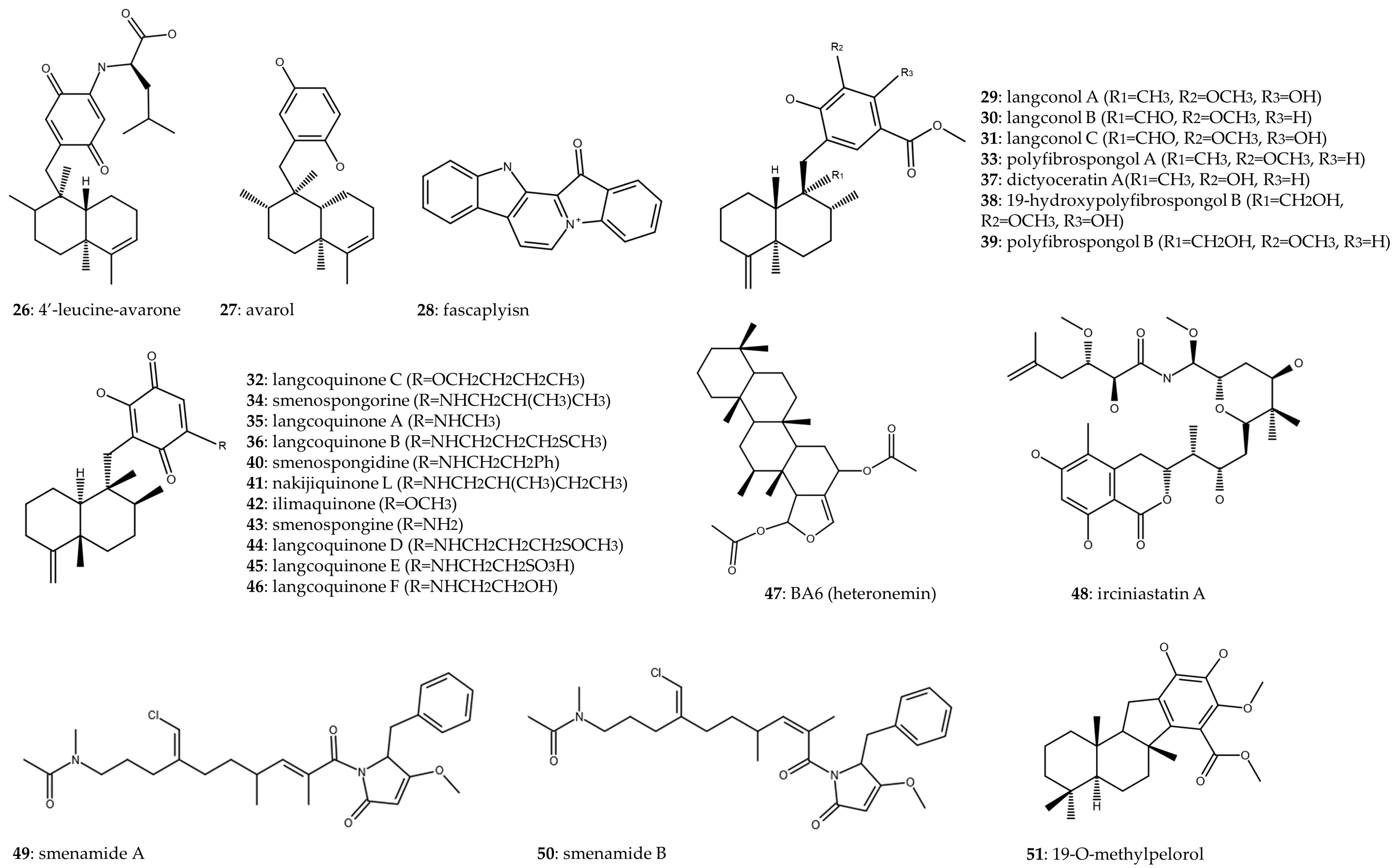
2.2. Order Dictyoceratida
| Sponge | Compounds | Chemical Class | Methods of Production | Cell Line (NSCLC/SCLC) | IC50 | In Vivo * | Molecular Mechanism | Ref. |
|---|---|---|---|---|---|---|---|---|
| Dysidea avara | 4′-leucine-avarone (26) | Amino derivative | Semisynthesis. Chemical modification of avarol | A549 (NSCLC) and MRC-5 (NT) | 7.40 ± 2.98 and >100 IC50 (μM) A549 and MRC-5, respectively (48 h) | ✗ | NR | [30] |
| Dysidea avara | avarol (27) | Sesquiterpene hydroquinone | Isolation | A549 (NSCLC) and MRC-5 (NT) | 35.27 ± 0.64 and 29.14 ± 0.41 IC50 (μg/mL) A549 and MRC-5, respectively (72 h) | ✗ | NR | [29] |
| Fascaplysinopsis Bergquist sp. | fascaplysin (28) | Red bis-indole alkaloid | Commercial | NCI-H417, DMS153, NCI-H526 (SCLC), H1299, A549, H23 (NSCLC), SCLC26A, GLC14, GLC16, and GLC19 (derived from SCLC patients) | 134–1740 nM (96 h) | ✗ | Affects topoisomerase I, integrity of DNA, generation of ROS, apoptosis, and cell cycle arrest. | [31] |
| Fascaplysinopsis Bergquist sp. | fascaplysin (28) | Red bis-indole alkaloid | Commercial | NCI-H526, DMS53, DMS153, H69 (SCLC), A549, H1299, PC9 (NSCLC), SCLC26A and S457 (derived from pleural effusions of SCLC patients), IVIC-A, BH295 (derived from pleural effusions of NSCLC patients), and SCLC CTCs | 0.53 ± 0.06, 1.17 ± 0.02, 1.35 ± 0.23, 1.05 ± 0.14, 0.63 ± 0.11, 0.69 ± 0.12, 0.99 ± 0.39, 1.48 ± 0.12, 0.2 ± 0.03, 1.41 ± 0.33, and 2.04 ± 0.05 IC50 (μM) NCI-H526, DMS53, DMS153, H69, A549, H1299, PC9, SCLC26A, S457, IVIC-A, and BH295, respectively | ✗ | ATM-triggered signaling cascade provoked by drug-induced DNA damage. Cytotoxic effect against lung cancer cell lines and spheroids of SCLC CTCs. | [37] |
| Spongia sp. | Langconol A (29); langconol B (30); langconol C (31); langcoquinone C (32); polyfibrospongol A (33); smenospongorine (34); langcoquinone A (35); langcoquinone B (36); dictyoceratin A (37); 19-hydroxypolyfibrospongol B (38); polyfibrospongol B (39); smenospongidine (40); nakijiquinone L (41); ilimaquinone (42); and smenospongine (43) | Merosesquiterpenes | Isolation | A549 (NSCLC) and WI-38 (NT) | 29, 30, 33,
37, and 39: >50 and >50 31: 7.8 and 8.7 32: 6.6 and 8.2 34: 6.7 and 3.5 35: 9.9 and 8.4 36: 6.2 and 8.8 38: >50 and 42.1 40: 4 and 3 41: 8.9 and 6.9 42: 5.9 and 9.7 43: 7.8 and 9.2 IC50 (μM) A549 and WI-38, respectively (72 h) | ✗ | NR | [38] |
| Spongia sp. | Langcoquinone D (44), langcoquinone E (45), and langcoquinone F (46) | Sesquiterpenoid quinones | Isolation | A549 (NSCLC) and WI-38 (NT) | 44: 8.9 and 5.6 45 and 46: >50 and >50 IC50 (μM) A549 and WI-38, respectively (24 h) | ✗ | NR | [39] |
| Hyrtios erecta | BA6 (heteronemin) (47) | Sesterterpen | Isolation | A549 (NSCLC) | 5.12 μM (24 h) | ✗ | Induction of apoptosis by increasing mtROS and mitochondrial dysfunction. Bax upregulation; Bcl-2 downregulation; release of cytochrome C; activation of caspase-9 and -3. | [40] |
| Ircinia ramose and Psammocinia | irciniastatin A (48), also known as psymberin | Pederin family or pederin-type natural product | Chemical synthesis | A549 (NSCLC) | NR | ✗ | Translation inhibition that induces activation of ERK pathway and promotes the ectodomain shedding of TNF receptor 1. | [43] |
| Smenospongia aurea | smenamide A (49) and smenamide B (50) | Hybrid peptide/polyketide | Isolation | Calu-1 (NSCLC) | 49: 48 nM 50: 49 nM (72 h) | ✗ | Induction of apoptosis | [44] |
| Dactylospongia sp. | 19-O-methylpelorol (51) | Sesquiterpene hydroquinone | Isolation | PC-9 (NSCLC) | 9.2 μM (72 h) | ✗ | NR | [45] |
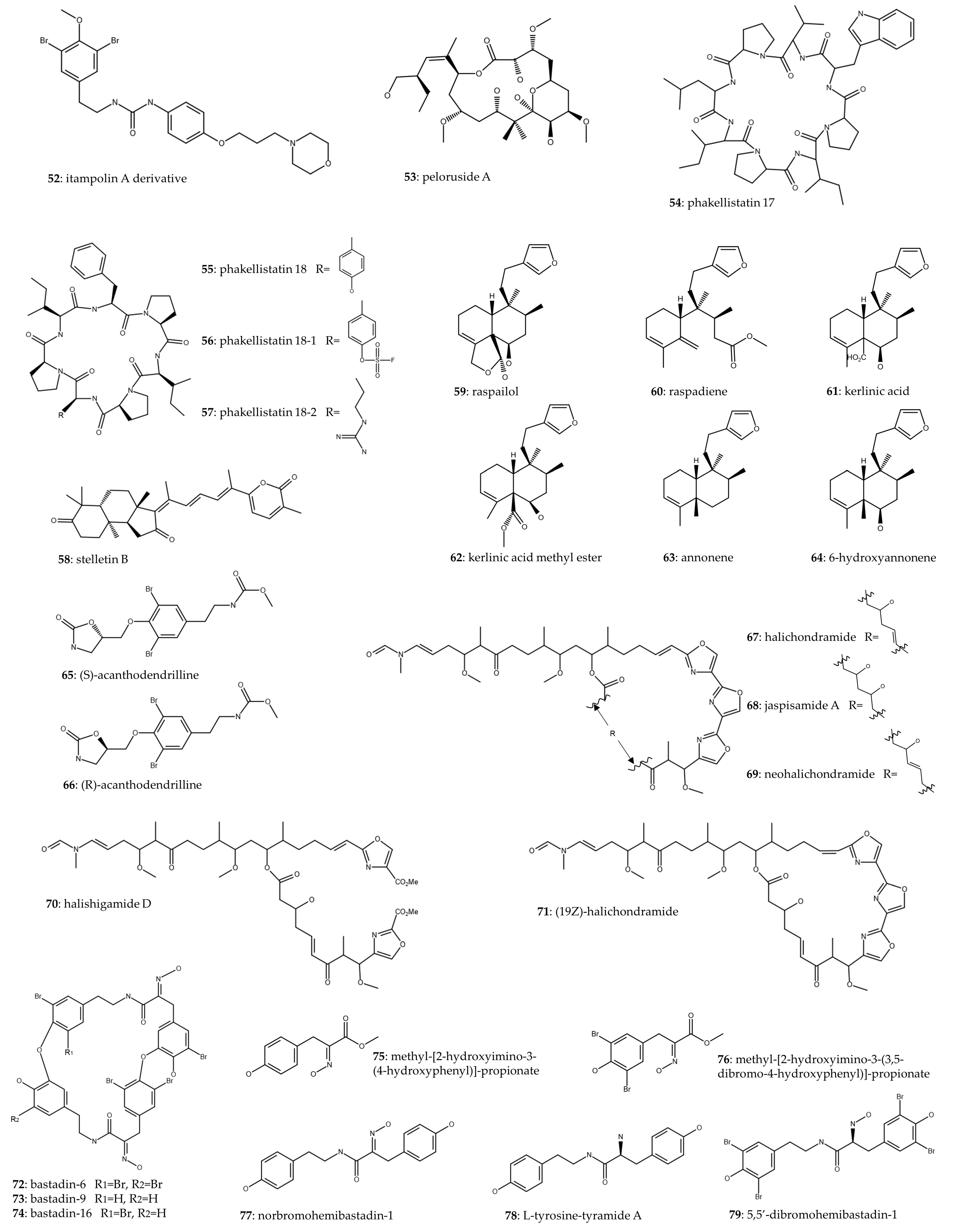
2.3. Minority Orders
| Sponge | Compounds | Chemical Class | Methods of Production | Cell Line (NSCLC/SCLC) | IC50 | In Vivo * | Molecular Mechanism | Ref. |
|---|---|---|---|---|---|---|---|---|
| Iotrochota purpurea | itampolin A derivative (52) | Brominated tyrosine alkaloid | Chemical synthesis | A549 (NSCLC) | 0.66 μM (48 h) | ✗ | Decreased expression of phospho-p38 | [48] |
| Mycale henscheli | peloruside A (53) | Polyketide | Isolation and chemical synthesis (both methods) | NR | NR | ✓ | (H460 xenografts) Dose-dependent decrease in tumor growth, with TGI values of 88% at 5 mg/kg and 99% at 10 mg/kg, with no deaths. (A549 Xenografts) TGI ranging from 51% to 74% | [49] |
| Phakellia fusca | phakellistatin 17 (54), phakellistatin 18 (55), phakellistatin 18 analog 1 (56), and phakellistatin 18 analog 2 (57) | Proline-rich cyclopeptides | Chemical synthesis | A549 (NSCLC) | 54: >100 μM 55: 72.42 μM 56: 67.53 μM 57: 79.71 μM (72 h) | ✗ | NR | [50] |
| Jaspis stellifera | stellettin B (Stel B) (58) | Isomalabaricane triterpene | Isolation | A549 (NSCLC) | 0.022 μM (48 h) | ✗ | Targeting PI3K/Akt/mTOR pathway. Induction of G1 arrest (↑p27 and ↓cyclin D1), apoptosis (↑PARP cleavage and ↑ROS generation), and autophagy (↑LC3B II/I, ↑Atg5, and ↓p62). | [51] |
| Raspailia bouryesnaultae | raspailol (59), raspadiene (60), kerlinic acid (61), kerlinic acid methyl ester (62), annonene (63), and 6-hydroxyannonene (64) | Clerodane diterpenes | Isolation | A549 (NSCLC) | 59: 24.12 μM 60: 100.3 μM 61: 66.22 μM 62: 20.63 μM 63: 143.7 μM 64: 24.52 μM (48 h) | ✗ | NR | [54] |
| Acanthodendrilla sp. | (S)- acanthodendrilline (65) and (R)- acanthodendrilline (66) | Bromotyrosine alkaloid | Chemical synthesis | H292 (NSCLC) | 65: 58.5 ± 6.7 μM 66: 173.5 ± 24.7 μM (72 h) | ✗ | NR | [55] |
| Chondrosia corticata | halichondramide (67), jaspisamide A (68), neohalichondramide (69), halishigamide D (70), and (19Z)-halichondramide (71) | Oxazole-containing macrolide | Isolation | A549 (NSCLC) | 67: 0.045 μM 68: 32.63 μM 69: 3.73 μM 70: 1.65 μM 71: 0.024 μM (72 h) | ✗ | G2/M cell cycle arrest (↑p53, ↑GADD45α, ↓cyclin B1, ↓cyclin A, ↓CDC2, and ↓CDC25C) and suppression of the Akt/mTOR signaling pathway (71). | [56] |
| Ianthella basta | bastadin-6 (72), bastadin-9 (73), bastadin-16 (74), methyl-[2-hydroxyimino-3-(4-hydroxyphenyl)]-propionate (75), methyl-[2-hydroxyimino-3-(3,5-dibromo-4-hydroxyphenyl)]-propionate (76), norbromohemibastadin-1 (77), L-tyrosine-tyramide A (78), and 5,5′-dibromohemibastadin-1 (79) | Bastadins | 72–74: Isolation 4–8: Chemical synthesis | A549 (NSCLC) | 72: 3 μM 73: 7 μM 74: 8 μM 75–78: >100 μM 79: 68 μM (72 h) | ✗ | NR | [57] |
| NR | alkaloid analogs with 2-amino-1H-imidazole core | Alkaloid | Chemical synthesis | A549 (NSCLC) | 14.15–43.72 μM (72 h) | ✓ | Inhibition of tumor growth in A549 xenograft models. | [58] |
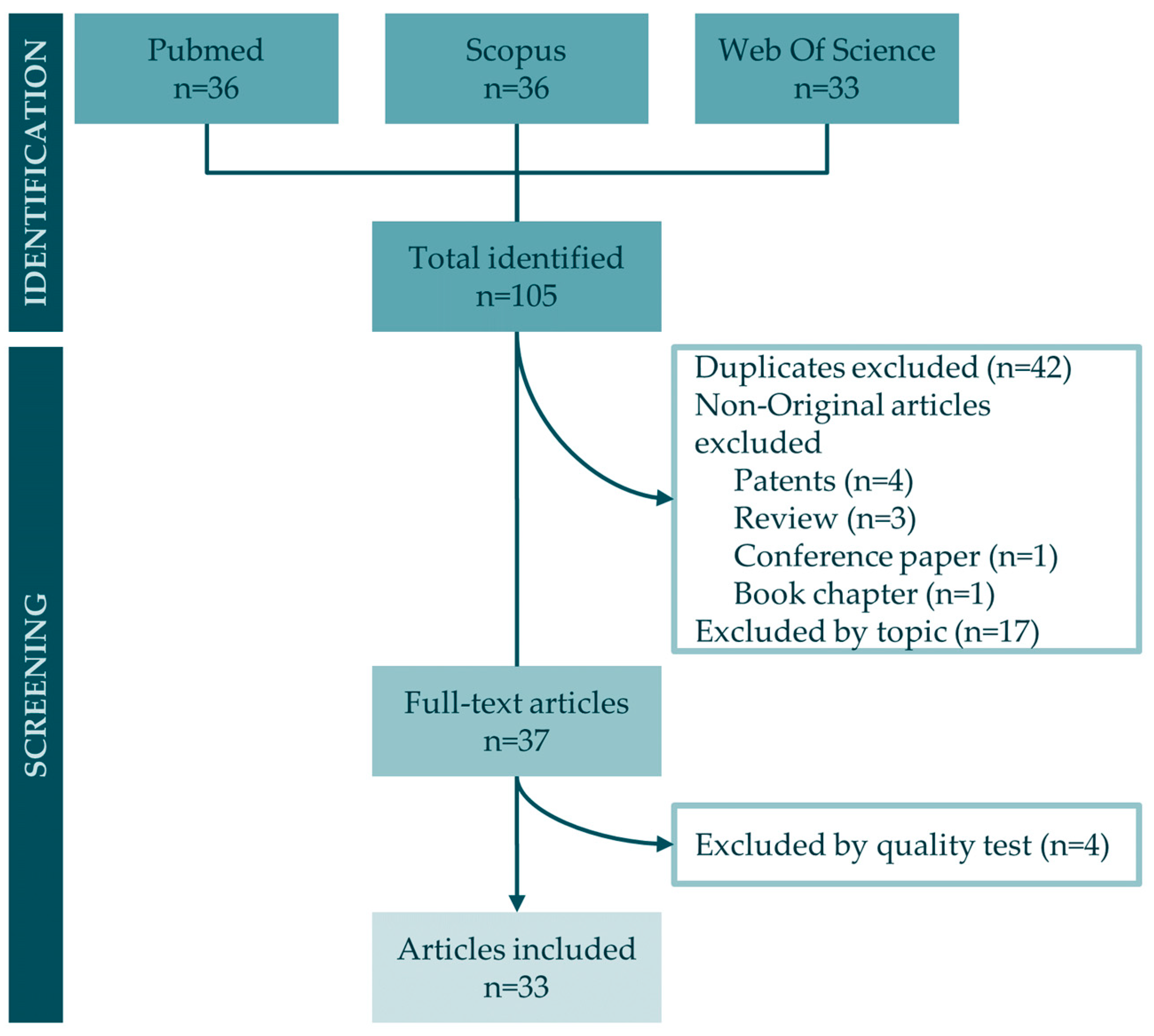
3. Materials and Methods
3.1. Study Eligibility
3.2. Inclusion and Exclusion Criteria
3.2.1. Inclusion Criteria
3.2.2. Exclusion Criteria
3.3. Data Sources and Search Strategy
3.4. Study Selection
3.5. Data Extraction
4. Limitations and Future Perspectives
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Pikor, L.A.; Ramnarine, V.R.; Lam, S.; Lam, W.L. Genetic Alterations Defining NSCLC Subtypes and Their Therapeutic Implications. Lung Cancer 2013, 82, 179–189. [Google Scholar] [CrossRef] [PubMed]
- Taghvimi, S.; Vakili, O.; Soltani Fard, E.; Khatami, S.H.; Karami, N.; Taheri-Anganeh, M.; Salehi, M.; Negahdari, B.; Ghasemi, H.; Movahedpour, A. Exosomal MicroRNAs and Long Noncoding RNAs: Novel Mediators of Drug Resistance in Lung Cancer. J. Cell Physiol. 2022, 237, 2095–2106. [Google Scholar] [CrossRef]
- Li, Y.; Yan, B.; He, S. Advances and Challenges in the Treatment of Lung Cancer. Biomed. Pharmacother. 2023, 169, 115891. [Google Scholar] [CrossRef] [PubMed]
- Pucci, C.; Martinelli, C.; Ciofani, G. Innovative Approaches for Cancer Treatment: Current Perspectives and New Challenges. Ecancermedicalscience 2019, 13, 961. [Google Scholar] [CrossRef] [PubMed]
- Khalifa, S.A.M.; Elias, N.; Farag, M.A.; Chen, L.; Saeed, A.; Hegazy, M.-E.F.; Moustafa, M.S.; Abd El-Wahed, A.; Al-Mousawi, S.M.; Musharraf, S.G.; et al. Marine Natural Products: A Source of Novel Anticancer Drugs. Mar. Drugs 2019, 17, 491. [Google Scholar] [CrossRef]
- Jimenez, P.C.; Wilke, D.V.; Branco, P.C.; Bauermeister, A.; Rezende-Teixeira, P.; Gaudêncio, S.P.; Costa-Lotufo, L.V. Enriching Cancer Pharmacology with Drugs of Marine Origin. Br. J. Pharmacol. 2020, 177, 3–27. [Google Scholar] [CrossRef]
- Ye, J.; Zhou, F.; Al-Kareef, A.M.Q.; Wang, H. Anticancer Agents from Marine Sponges. J. Asian Nat. Prod. Res. 2015, 17, 64–88. [Google Scholar] [CrossRef]
- Nigam, M.; Suleria, H.A.R.; Farzaei, M.H.; Mishra, A.P. Marine Anticancer Drugs and Their Relevant Targets: A Treasure from the Ocean. DARU J. Pharm. Sci. 2019, 27, 491–515. [Google Scholar] [CrossRef]
- Dyshlovoy, S.A.; Honecker, F. Marine Compounds and Cancer: Updates 2022. Mar. Drugs 2022, 20, 759. [Google Scholar] [CrossRef]
- Cheun-Arom, T.; Chanvorachote, P.; Sirimangkalakitti, N.; Chuanasa, T.; Saito, N.; Abe, I.; Suwanborirux, K. Replacement of a Quinone by a 5-O-Acetylhydroquinone Abolishes the Accidental Necrosis Inducing Effect While Preserving the Apoptosis-Inducing Effect of Renieramycin M on Lung Cancer Cells. J. Nat. Prod. 2013, 76, 1468–1474. [Google Scholar] [CrossRef] [PubMed]
- Sirimangkalakitti, N.; Chamni, S.; Charupant, K.; Chanvorachote, P.; Mori, N.; Saito, N.; Suwanborirux, K. Chemistry of Renieramycins. 15. Synthesis of 22-O-Ester Derivatives of Jorunnamycin A and Their Cytotoxicity against Non-Small-Cell Lung Cancer Cells. J. Nat. Prod. 2016, 79, 2089–2093. [Google Scholar] [CrossRef] [PubMed]
- Chamni, S.; Sirimangkalakitti, N.; Chanvorachote, P.; Saito, N.; Suwanborirux, K. Chemistry of Renieramycins. 17. A New Generation of Renieramycins: Hydroquinone 5-O-Monoester Analogues of Renieramycin M as Potential Cytotoxic Agents against Non-Small-Cell Lung Cancer Cells. J. Nat. Prod. 2017, 80, 1541–1547. [Google Scholar] [CrossRef]
- Petsri, K.; Chamni, S.; Suwanborirux, K.; Saito, N.; Chanvorachote, P. Renieramycin T Induces Lung Cancer Cell Apoptosis by Targeting Mcl-1 Degradation: A New Insight in the Mechanism of Action. Mar. Drugs 2019, 17, 301. [Google Scholar] [CrossRef] [PubMed]
- Chantarawong, W.; Chamni, S.; Suwanborirux, K.; Saito, N.; Chanvorachote, P. 5-O-Acetyl-Renieramycin T from Blue Sponge Xestospongia sp. Induces Lung Cancer Stem Cell Apoptosis. Mar. Drugs 2019, 17, 109. [Google Scholar] [CrossRef] [PubMed]
- Iksen, I.; Sinsook, S.; Wattanathamsan, O.; Buaban, K.; Chamni, S.; Pongrakhananon, V. Target Identification of 22-(4-Pyridinecarbonyl) Jorunnamycin A, a Tetrahydroisoquinoline Derivative from the Sponge Xestospongia sp., in Mediating Non-Small-Cell Lung Cancer Cell Apoptosis. Molecules 2022, 27, 8948. [Google Scholar] [CrossRef]
- Iksen, I.; Seephan, S.; Limprasutr, V.; Sinsook, S.; Buaban, K.; Chamni, S.; Pongrakhananon, V. Preclinical Characterization of 22-(4′-Pyridinecarbonyl) Jorunnamycin A against Lung Cancer Cell Invasion and Angiogenesis via AKT/MTOR Signaling. ACS Pharmacol. Transl. Sci. 2023, 6, 1143–1154. [Google Scholar] [CrossRef]
- Gonzalez-Avila, G.; Sommer, B.; Mendoza-Posada, D.A.; Ramos, C.; Garcia-Hernandez, A.A.; Falfan-Valencia, R. Matrix Metalloproteinases Participation in the Metastatic Process and Their Diagnostic and Therapeutic Applications in Cancer. Crit. Rev. Oncol. Hematol. 2019, 137, 57–83. [Google Scholar] [CrossRef]
- Zimna, A.; Kurpisz, M. Hypoxia-Inducible Factor-1 in Physiological and Pathophysiological Angiogenesis: Applications and Therapies. BioMed Res. Int. 2015, 2015, 549412. [Google Scholar] [CrossRef]
- Nguyen, H.M.; Ito, T.; Win, N.N.; Vo, H.Q.; Nguyen, H.T.; Morita, H. A New Sterol from the Vietnamese Marine Sponge Xestospongia testudinaria and Its Biological Activities. Nat. Prod. Res. 2019, 33, 1175–1181. [Google Scholar] [CrossRef]
- Zovko, A.; Viktorsson, K.; Hååg, P.; Kovalerchick, D.; Färnegårdh, K.; Alimonti, A.; Ilan, M.; Carmeli, S.; Lewensohn, R. Marine Sponge Cribrochalina vasculum Compounds Activate Intrinsic Apoptotic Signaling and Inhibit Growth Factor Signaling Cascades in Non-Small Cell Lung Carcinoma. Mol. Cancer Ther. 2014, 13, 2941–2954. [Google Scholar] [CrossRef]
- Zovko, A.; Novak, M.; Hååg, P.; Kovalerchick, D.; Holmlund, T.; Färnegårdh, K.; Ilan, M.; Carmeli, S.; Lewensohn, R.; Viktorsson, K. Compounds from the Marine Sponge Cribrochalina vasculum Offer a Way to Target IGF-1R Mediated Signaling in Tumor Cells. Oncotarget 2016, 7, 50258–50276. [Google Scholar] [CrossRef]
- Hadisaputri, Y.E.; Andika, R.; Sopyan, I.; Zuhrotun, A.; Maharani, R.; Rachmat, R.; Abdulah, R. Caspase Cascade Activation During Apoptotic Cell Death of Human Lung Carcinoma Cells A549 Induced by Marine Sponge Callyspongia aerizusa. Drug Des. Dev. Ther. 2021, 15, 1357–1368. [Google Scholar] [CrossRef]
- Ibrahim, S.; Mohamed, G.; Al Haidari, R.; El-Kholy, A.; Zayed, M. Ingenine F: A New Cytotoxic Tetrahydro Carboline Alkaloid from the Indonesian Marine Sponge Acanthostrongylophora ingens. Pharmacogn. Mag. 2018, 14, 231. [Google Scholar] [CrossRef] [PubMed]
- Zovko, A.; Viktorsson, K.; Lewensohn, R.; Kološa, K.; Filipič, M.; Xing, H.; Kem, W.; Paleari, L.; Turk, T. APS8, a Polymeric Alkylpyridinium Salt Blocks A7 NAChR and Induces Apoptosis in Non-Small Cell Lung Carcinoma. Mar. Drugs 2013, 11, 2574–2594. [Google Scholar] [CrossRef] [PubMed]
- Mejia, E.J.; Magranet, L.B.; De Voogd, N.J.; Tendyke, K.; Qiu, D.; Shen, Y.Y.; Zhou, Z.; Crews, P. Structures and Cytotoxic Evaluation of New and Known Acyclic Ene-Ynes from an American Samoa Petrosia sp. Sponge. J. Nat. Prod. 2013, 76, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Sindhoor, S.M.; Naveen, N.R.; Rao, G.K.; Gopan, G.; Chopra, H.; Park, M.N.; Alshahrani, M.M.; Jose, J.; Emran, T.B.; Kim, B. A Spotlight on Alkaloid Nanoformulations for the Treatment of Lung Cancer. Front. Oncol. 2022, 12, 994155. [Google Scholar] [CrossRef]
- Olofinsan, K.; Abrahamse, H.; George, B.P. Therapeutic Role of Alkaloids and Alkaloid Derivatives in Cancer Management. Molecules 2023, 28, 5578. [Google Scholar] [CrossRef] [PubMed]
- Stanojkovic, T.P.; Filimonova, M.; Grozdanic, N.; Petovic, S.; Shitova, A.; Soldatova, O.; Filimonov, A.; Vladic, J.; Shegay, P.; Kaprin, A.; et al. Evaluation of In Vitro Cytotoxic Potential of Avarol towards Human Cancer Cell Lines and In Vivo Antitumor Activity in Solid Tumor Models. Molecules 2022, 27, 9048. [Google Scholar] [CrossRef]
- Pejin, B.; Iodice, C.; Tommonaro, G.; Bogdanovic, G.; Kojic, V.; De Rosa, S. Further in Vitro Evaluation of Cytotoxicity of the Marine Natural Product Derivative 4′-Leucine-Avarone. Nat. Prod. Res. 2014, 28, 347–350. [Google Scholar] [CrossRef]
- Hamilton, G. Cytotoxic Effects of Fascaplysin against Small Cell Lung Cancer Cell Lines. Mar. Drugs 2014, 12, 1377–1389. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, H.; Takada, K. Reactive Oxygen Species in Cancer: Current Findings and Future Directions. Cancer Sci. 2021, 112, 3945–3952. [Google Scholar] [CrossRef] [PubMed]
- Zhao, H.-M.; He, J.; Chang, Y.-T.; Liu, L.-Y.; Sun, F.; Lin, H.-W.; Yang, F. Marine Sponge-Derived Alkaloid Induces Mitochondrial Dysfunction and Inhibits the PI3K/AKT/MTOR Signaling Pathway against Burkitt’s Lymphoma. J. Nat. Prod. 2023, 86, 51. [Google Scholar] [CrossRef] [PubMed]
- Lucchetti, D.; Luongo, F.; Colella, F.; Gurreri, E.; Artemi, G.; Desiderio, C.; Serra, S.; Giuliante, F.; De Maria, R.; Sgambato, A.; et al. Exploiting Bioactive Natural Products of Marine Origin: Evaluation of the Meroterpenoid Metachromin V as a Novel Potential Therapeutic Drug for Colorectal Cancer. Biomed. Pharmacother. 2023, 162, 114679. [Google Scholar] [CrossRef] [PubMed]
- Alkhilaiwi, F.; Fadil, S.; Aljoud, F.; Yonbawi, A.; Ashi, A.; Hareeri, R.; Bakhashab, S.; Alamri, A.; Albikairi, A.; Shaala, L.; et al. Evaluation of Cytotoxicity of the Methanolic Extract of Red Sea Marine Sponge Xestospongia testudinaria and Its Related Compounds Against MCF-7 Human Breast Cancer Cells. Breast Cancer Targets Ther. 2023, 15, 879–890. [Google Scholar] [CrossRef] [PubMed]
- Romano, B.; Maresca, D.C.; Somma, F.; Ahmadi, P.; Putra, M.Y.; Rahmawati, S.I.; Chianese, G.; Formisano, C.; Ianaro, A.; Ercolano, G. Ircinia ramosa Sponge Extract (ISP) Induces Apoptosis in Human Melanoma Cells and Inhibits Melanoma Cell Migration and Invasiveness. Mar. Drugs 2023, 21, 371. [Google Scholar] [CrossRef]
- Rath, B.; Hochmair, M.; Plangger, A.; Hamilton, G. Anticancer Activity of Fascaplysin against Lung Cancer Cell and Small Cell Lung Cancer Circulating Tumor Cell Lines. Mar. Drugs 2018, 16, 383. [Google Scholar] [CrossRef]
- Nguyen, H.M.; Ito, T.; Kurimoto, S.-I.; Ogawa, M.; Win, N.N.; Hung, V.Q.; Nguyen, H.T.; Kubota, T.; Kobayashi, J.; Morita, H. New Merosesquiterpenes from a Vietnamese Marine Sponge of Spongia sp. and Their Biological Activities. Bioorg. Med. Chem. Lett. 2017, 27, 3043–3047. [Google Scholar] [CrossRef]
- Ito, T.; Nguyen, H.M.; Win, N.N.; Vo, H.Q.; Nguyen, H.T.; Morita, H. Three New Sesquiterpene Aminoquinones from a Vietnamese Spongia sp. and Their Biological Activities. J. Nat. Med. 2018, 72, 298–303. [Google Scholar] [CrossRef]
- Cheng, M.-H.; Huang, H.-L.; Lin, Y.-Y.; Tsui, K.-H.; Chen, P.-C.; Cheng, S.-Y.; Chong, I.-W.; Sung, P.-J.; Tai, M.-H.; Wen, Z.-H.; et al. BA6 Induces Apoptosis via Stimulation of Reactive Oxygen Species and Inhibition of Oxidative Phosphorylation in Human Lung Cancer Cells. Oxidative Med. Cell. Longev. 2019, 2019, 6342104. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Su, C.; Zhao, F.; Tao, J.; Hu, D.; Shi, A.; Pan, J.; Zhang, Y. Paclitaxel Promotes Lung Cancer Cell Apoptosis via MEG3-P53 Pathway Activation. Biochem. Biophys. Res. Commun. 2018, 504, 123–128. [Google Scholar] [CrossRef]
- Matsumoto, M.; Nakajima, W.; Seike, M.; Gemma, A.; Tanaka, N. Cisplatin-Induced Apoptosis in Non-Small-Cell Lung Cancer Cells Is Dependent on Bax- and Bak-Induction Pathway and Synergistically Activated by BH3-Mimetic ABT-263 in P53 Wild-Type and Mutant Cells. Biochem. Biophys. Res. Commun. 2016, 473, 490–496. [Google Scholar] [CrossRef]
- Quach, H.T.; Hirano, S.; Fukuhara, S.; Watanabe, T.; Kanoh, N.; Iwabuchi, Y.; Usui, T.; Kataoka, T. Irciniastatin A Induces Potent and Sustained Activation of Extracellular Signal-Regulated Kinase and Thereby Promotes Ectodomain Shedding of Tumor Necrosis Factor Receptor 1 in Human Lung Carcinoma A549 Cells. Biol. Pharm. Bull. 2015, 38, 941–946. [Google Scholar] [CrossRef]
- Teta, R.; Irollo, E.; Della Sala, G.; Pirozzi, G.; Mangoni, A.; Costantino, V. Smenamides A and B, Chlorinated Peptide/Polyketide Hybrids Containing a Dolapyrrolidinone Unit from the Caribbean Sponge Smenospongia aurea. Evaluation of Their Role as Leads in Antitumor Drug Research. Mar. Drugs 2013, 11, 4451–4463. [Google Scholar] [CrossRef]
- Li, J.; Yang, F.; Wang, Z.; Wu, W.; Liu, L.; Wang, S.-P.; Zhao, B.-X.; Jiao, W.-H.; Xu, S.-H.; Lin, H.-W. Unusual Anti-Inflammatory Meroterpenoids from the Marine Sponge Dactylospongia sp. Org. Biomol. Chem. 2018, 16, 6773–6782. [Google Scholar] [CrossRef]
- Costantino, V.; Bourguet-Kondracki, M.L.; Ioannou, E. Editorial: Peptide/Polyketide Molecules From Marine Macro and/or Microorganisms. Front. Chem. 2020, 8, 558911. [Google Scholar] [CrossRef]
- Esposito, G.; Teta, R.; Miceli, R.; Ceccarelli, L.; Della Sala, G.; Camerlingo, R.; Irollo, E.; Mangoni, A.; Pirozzi, G.; Costantino, V. Isolation and Assessment of the in Vitro Anti-Tumor Activity of Smenothiazole A and B, Chlorinated Thiazole-Containing Peptide/Polyketides from the Caribbean Sponge, Smenospongia aurea. Mar. Drugs 2015, 13, 444–459. [Google Scholar] [CrossRef]
- Liang, J.; Wang, M.; Wang, S.; Li, X.; Meng, F. Fragment-Based Structural Optimization of a Natural Product Itampolin A as a P38α Inhibitor for Lung Cancer. Mar. Drugs 2019, 17, 53. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.J.; Krauth, M.; Wick, M.J.; Shay, J.W.; Gellert, G.; De Brabander, J.K.; Northcote, P.T.; Miller, J.H. Peloruside A Inhibits Growth of Human Lung and Breast Tumor Xenografts in an Athymic Nu/Nu Mouse Model. Mol. Cancer Ther. 2015, 14, 1816–1823. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Li, Y.; Chang, Q.; Zhao, X.; Chen, Q. Total Synthesis and Modification of Proline-Rich Cyclopeptides Phakellistatins 17 and 18 Isolated from Marine Sponge. Tetrahedron Lett. 2018, 59, 4011–4014. [Google Scholar] [CrossRef]
- Wang, R.; Zhang, Q.; Peng, X.; Zhou, C.; Zhong, Y.; Chen, X.; Qiu, Y.; Jin, M.; Gong, M.; Kong, D. Stellettin B Induces G1 Arrest, Apoptosis and Autophagy in Human Non-Small Cell Lung Cancer A549 Cells via Blocking PI3K/Akt/MTOR Pathway. Sci. Rep. 2016, 6, 27071. [Google Scholar] [CrossRef] [PubMed]
- De Santi, M.; Baldelli, G.; Diotallevi, A.; Galluzzi, L.; Schiavano, G.F.; Brandi, G. Metformin Prevents Cell Tumorigenesis through Autophagy-Related Cell Death. Sci. Rep. 2019, 9, 66. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Liu, F.; Wang, Y.; Li, D.; Guo, F.; Xu, L.; Zeng, Z.; Zhong, X.; Qian, K. Rapamycin-Induced Autophagy Sensitizes A549 Cells to Radiation Associated with DNA Damage Repair Inhibition. Thorac. Cancer 2016, 7, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Lhullier, C.; de Oliveira Tabalipa, E.; Nienkötter Sardá, F.; Sandjo, L.; Zanchett Schneider, N.; Carraro, J.; Oliveira Simões, C.; Schenkel, E. Clerodane Diterpenes from the Marine Sponge Raspailia bouryesnaultae Collected in South Brazil. Mar. Drugs 2019, 17, 57. [Google Scholar] [CrossRef] [PubMed]
- Sirimangkalakitti, N.; Yokoya, M.; Chamni, S.; Chanvorachote, P.; Plubrukrn, A.; Saito, N.; Suwanborirux, K. Synthesis and Absolute Configuration of Acanthodendrilline, a New Cytotoxic Bromotyrosine Alkaloid from the Thai Marine Sponge Acanthodendrilla sp. Chem. Pharm. Bull. 2016, 64, 258–262. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bae, S.Y.; Kim, G.D.; Jeon, J.; Shin, J.; Lee, S.K. Anti-Proliferative Effect of (19Z)-Halichondramide, a Novel Marine Macrolide Isolated from the Sponge Chondrosia corticata, Is Associated with G2/M Cell Cycle Arrest and Suppression of MTOR Signaling in Human Lung Cancer Cells. Toxicol. In Vitro 2013, 27, 694–699. [Google Scholar] [CrossRef]
- Mathieu, V.; Wauthoz, N.; Lefranc, F.; Niemann, H.; Amighi, K.; Kiss, R.; Proksch, P. Cyclic versus Hemi-Bastadins. Pleiotropic Anti-Cancer Effects: From Apoptosis to Anti-Angiogenic and Anti-Migratory Effects. Molecules 2013, 18, 3543–3561. [Google Scholar] [CrossRef]
- Gémes, N.; Makra, Z.; Neuperger, P.; Szabó, E.; Balog, J.Á.; Flink, L.B.; Kari, B.; Hackler, L., Jr.; Puskás, L.G.; Kanizsai, I.; et al. A Cytotoxic Survey on 2-Amino-1H-Imidazol Based Synthetic Marine Sponge Alkaloid Analogues. Drug Dev. Res. 2022, 83, 1906–1922. [Google Scholar] [CrossRef]
- Takeda, A.; Takano, N.; Kokuba, H.; Hino, H.; Moriya, S.; Abe, A.; Hiramoto, M.; Tsukahara, K.; Miyazawa, K. Macrolide Antibiotics Enhance the Antitumor Effect of Lansoprazole Resulting in Lysosomal Membrane Permeabilization-Associated Cell Death. Int. J. Oncol. 2020, 57, 1280. [Google Scholar] [CrossRef]
- Tang, S.A.; Zhou, Q.; Guo, W.Z.; Qiu, Y.; Wang, R.; Jin, M.; Zhang, W.; Li, K.; Yamori, T.; Dan, S.; et al. In Vitro Antitumor Activity of Stellettin B, a Triterpene from Marine Sponge Jaspis stellifera, on Human Glioblastoma Cancer SF295 Cells. Mar. Drugs 2014, 12, 4200–4213. [Google Scholar] [CrossRef]
- Li, Y.X.; Himaya, S.W.A.; Kim, S.K. Triterpenoids of Marine Origin as Anti-Cancer Agents. Molecules 2013, 18, 7886. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Dyshlovoy, S.A.; Honecker, F. Marine Compounds and Cancer: The First Two Decades of XXI Century. Mar. Drugs 2019, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Kumari, S.; Raj, S.; Babu, M.A.; Bhatti, G.K.; Bhatti, J.S. Antibody-Drug Conjugates in Cancer Therapy: Innovations, Challenges, and Future Directions. Arch. Pharm. Res. 2023, 47, 40–65. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, S.; Abrahams, C.L.; Krimm, S.; Smith, J.; Bajjuri, K.; Stephenson, H.T.; Henningsen, R.; Hanson, J.; Heibeck, T.H.; et al. Discovery of STRO-002, a Novel Homogeneous ADC Targeting Folate Receptor Alpha, for the Treatment of Ovarian and Endometrial Cancers. Mol. Cancer Ther. 2023, 22, 155–167. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Matsubara, N.; Naito, Y.; Kuboki, Y.; Harano, K.; Ono, M.; Urasaki, T.; Ohmoto, A.; Kawanai, T.; Hisai, T.; et al. First-in-Human Study of E7130 (a Tumor Microenvironment-Ameliorating Microtubule Inhibitor) in Patients with Advanced Solid Tumors: Primary Results of the Dose-Escalation Part. Cancer 2023, 129, 2348–2359. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, T.; Fujiwara, Y.; Yonemori, K.; Koyama, T.; Sato, J.; Tamura, K.; Shimomura, A.; Ikezawa, H.; Nomoto, M.; Furuuchi, K.; et al. First-in-Human Phase 1 Study of MORAb-202, an Antibody–Drug Conjugate Comprising Farletuzumab Linked to Eribulin Mesylate, in Patients with Folate Receptor-α–Positive Advanced Solid Tumors. Clin. Cancer Res. 2021, 27, 3905–3915. [Google Scholar] [CrossRef]
- Ramanjooloo, A.; Andersen, R.J.; Bhaw-Luximon, A. Marine Sponge-Derived/Inspired Drugs and Their Applications in Drug Delivery Systems. Future Med. Chem. 2021, 13, 487–504. [Google Scholar] [CrossRef]
- Hickman, J.A.; Graeser, R.; de Hoogt, R.; Vidic, S.; Brito, C.; Gutekunst, M.; van der Kuip, H. IMI PREDECT consortium Three-dimensional Models of Cancer for Pharmacology and Cancer Cell Biology: Capturing Tumor Complexity in Vitro/Ex Vivo. Biotechnol. J. 2014, 9, 1115–1128. [Google Scholar] [CrossRef]
- Nakarada, Đ.; Pejin, B.; Tommonaro, G.; Mojović, M. Liposomal Integration Method for Assessing Antioxida-tive Activity of Water Insoluble Compounds towards Biologically Relevant Free Radicals: Example of Avarol. J. Liposome Res. 2020, 30, 218–226. [Google Scholar] [CrossRef]
- Anjum, K.; Abbas, S.Q.; Shah, S.A.A.; Akhter, N.; Batool, S.; Hassan, S.S.U. Marine Sponges as a Drug Treasure. Biomol. Ther. 2016, 24, 347. [Google Scholar] [CrossRef] [PubMed]
- Sipkema, D.; Osinga, R.; Schatton, W.; Mendola, D.; Tramper, J.; Wijffels, R.H. Large-scale Production of Pharmaceuticals by Marine Sponges: Sea, Cell, or Synthesis? Biotechnol. Bioeng. 2005, 90, 201–222. [Google Scholar] [CrossRef] [PubMed]

| Database | Search Strategy |
|---|---|
| PubMed | ((Lung Neoplasms[MeSH Terms]) OR (Lung Cancer[Title/Abstract]) OR (Pulmonary Cancer[Title/Abstract]) OR (Pulmonary Neoplasms[Title/Abstract])) AND ((porifera[MeSH Terms]) OR (Demospongiae[Title/Abstract]) OR (marine sponge[Title/Abstract])) AND ((Antineoplastic Agents[MeSH Terms]) OR (Bioactive*[Title/Abstract]) OR (Antitumor*[Title/Abstract]) OR (Anticancer*[Title/Abstract])) |
| Scopus | (TITLE-ABS (lung AND neoplasms) OR TITLE-ABS (lung AND cancer) OR TITLE-ABS (lung AND adenocarcinoma) OR TITLE-ABS (pulmonary AND cancer) OR TITLE-ABS (pulmonary AND neoplasms)) AND (TITLE-ABS (porifera) OR TITLE-ABS (demospongiae) OR TITLE-ABS (marine AND sponge)) AND (TITLE-ABS (bioactive) OR TITLE-ABS (antitumor) OR TITLE-ABS (anticancer) OR TITLE-ABS (antineoplastic)) |
| Web of Science | ((TI = (Lung Neoplasms OR Lung Cancer OR Pulmonary Cancer OR Pulmonary Neoplasms)) OR (AB = (Lung Neoplasms OR Lung Cancer OR Pulmonary Cancer OR Pulmonary Neoplasms))) AND ((TI = (porifera OR demospongiae OR marine sponge)) OR (AB = (porifera OR demospongiae OR marine sponge))) AND ((TI = (bioactive OR antitumor OR anticancer OR antineoplastic)) OR (AB = (bioactive OR antitumor OR anticancer OR antineoplastic))) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ortigosa-Palomo, A.; Quiñonero, F.; Ortiz, R.; Sarabia, F.; Prados, J.; Melguizo, C. Natural Products Derived from Marine Sponges with Antitumor Potential against Lung Cancer: A Systematic Review. Mar. Drugs 2024, 22, 101. https://doi.org/10.3390/md22030101
Ortigosa-Palomo A, Quiñonero F, Ortiz R, Sarabia F, Prados J, Melguizo C. Natural Products Derived from Marine Sponges with Antitumor Potential against Lung Cancer: A Systematic Review. Marine Drugs. 2024; 22(3):101. https://doi.org/10.3390/md22030101
Chicago/Turabian StyleOrtigosa-Palomo, Alba, Francisco Quiñonero, Raul Ortiz, Francisco Sarabia, Jose Prados, and Consolación Melguizo. 2024. "Natural Products Derived from Marine Sponges with Antitumor Potential against Lung Cancer: A Systematic Review" Marine Drugs 22, no. 3: 101. https://doi.org/10.3390/md22030101
APA StyleOrtigosa-Palomo, A., Quiñonero, F., Ortiz, R., Sarabia, F., Prados, J., & Melguizo, C. (2024). Natural Products Derived from Marine Sponges with Antitumor Potential against Lung Cancer: A Systematic Review. Marine Drugs, 22(3), 101. https://doi.org/10.3390/md22030101







