Sodium Alginate as a Potential Therapeutic Filler: An In Vivo Study in Rats
Abstract
1. Introduction
2. Results
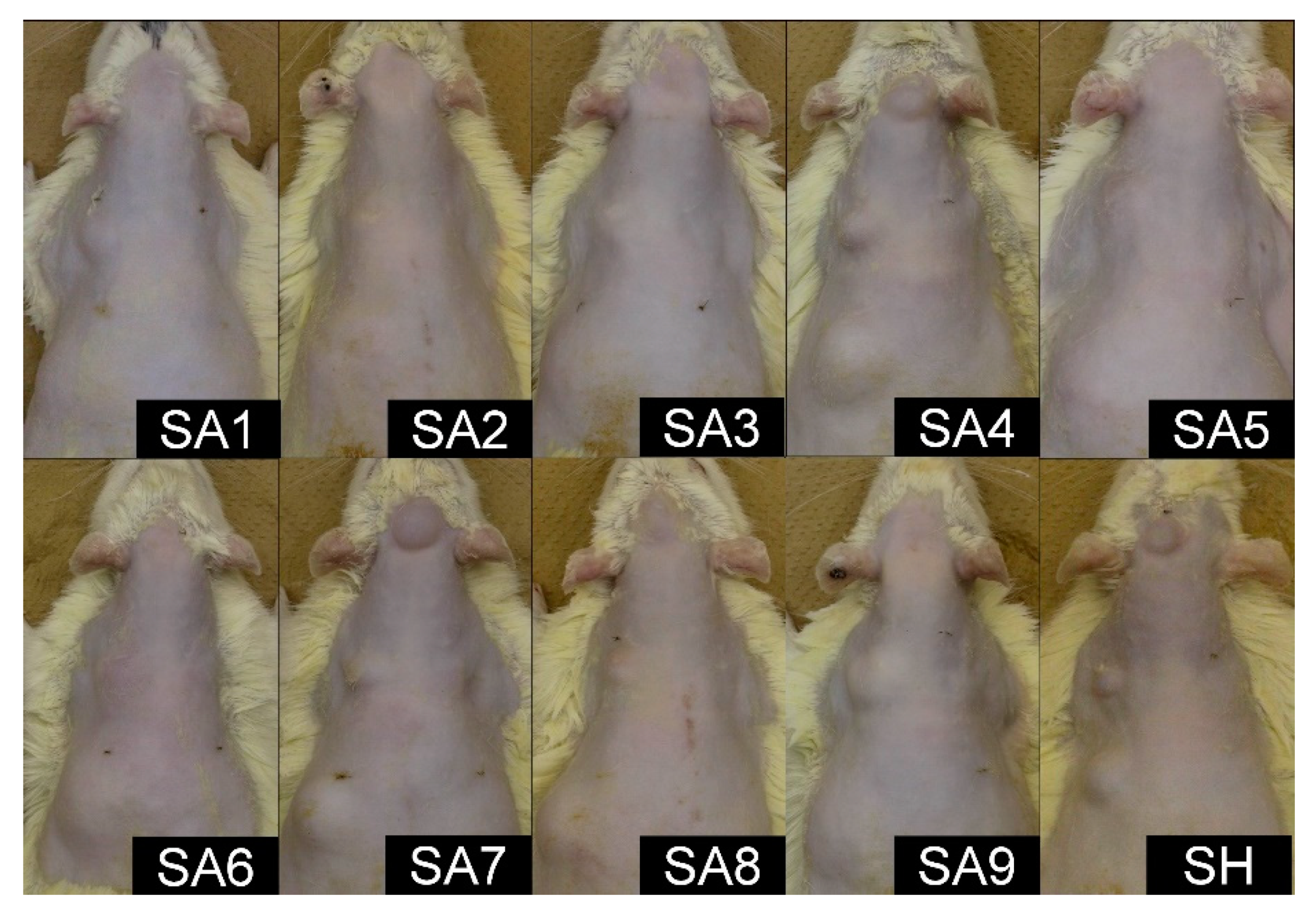
2.1. Macroscopic Findings
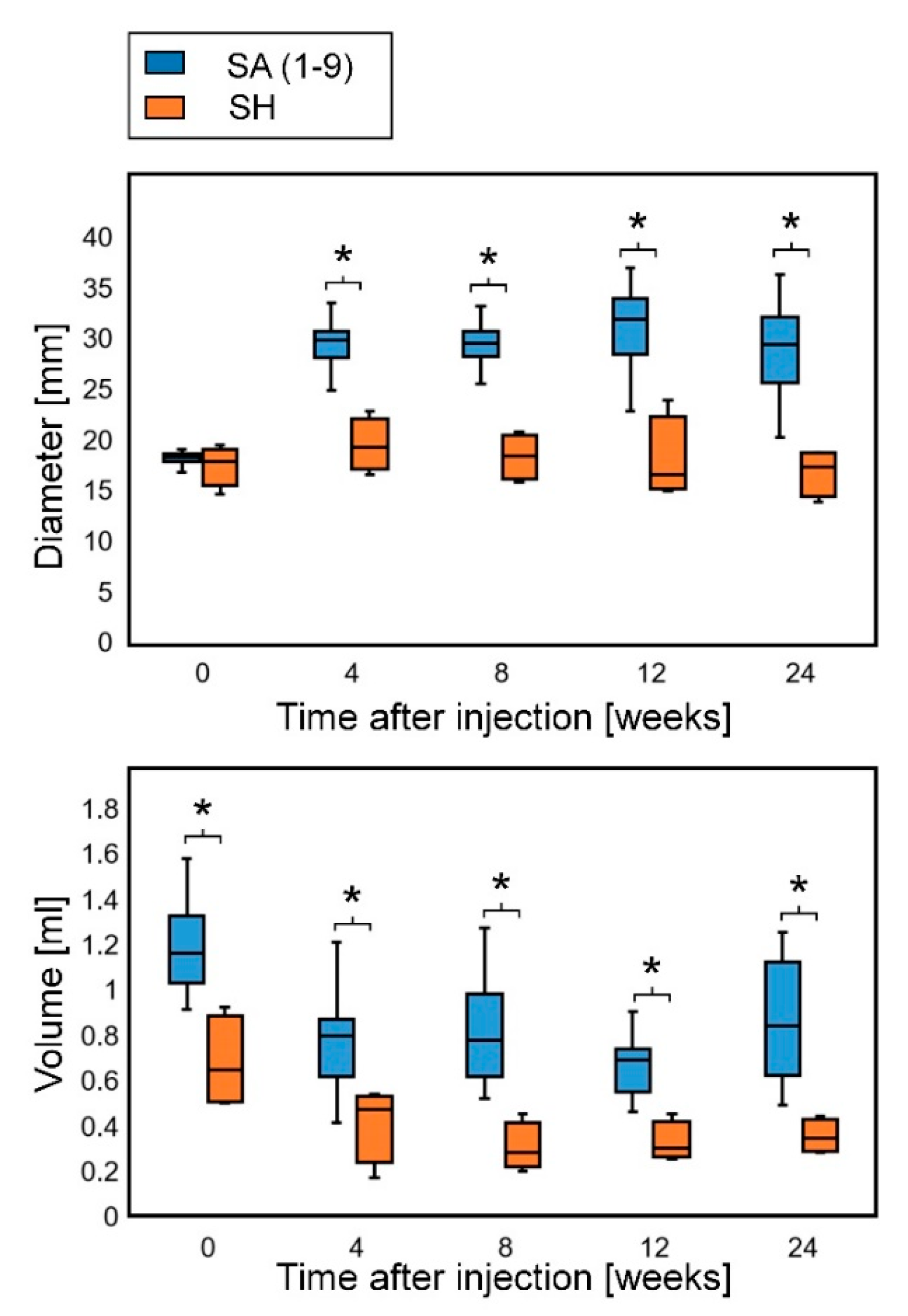
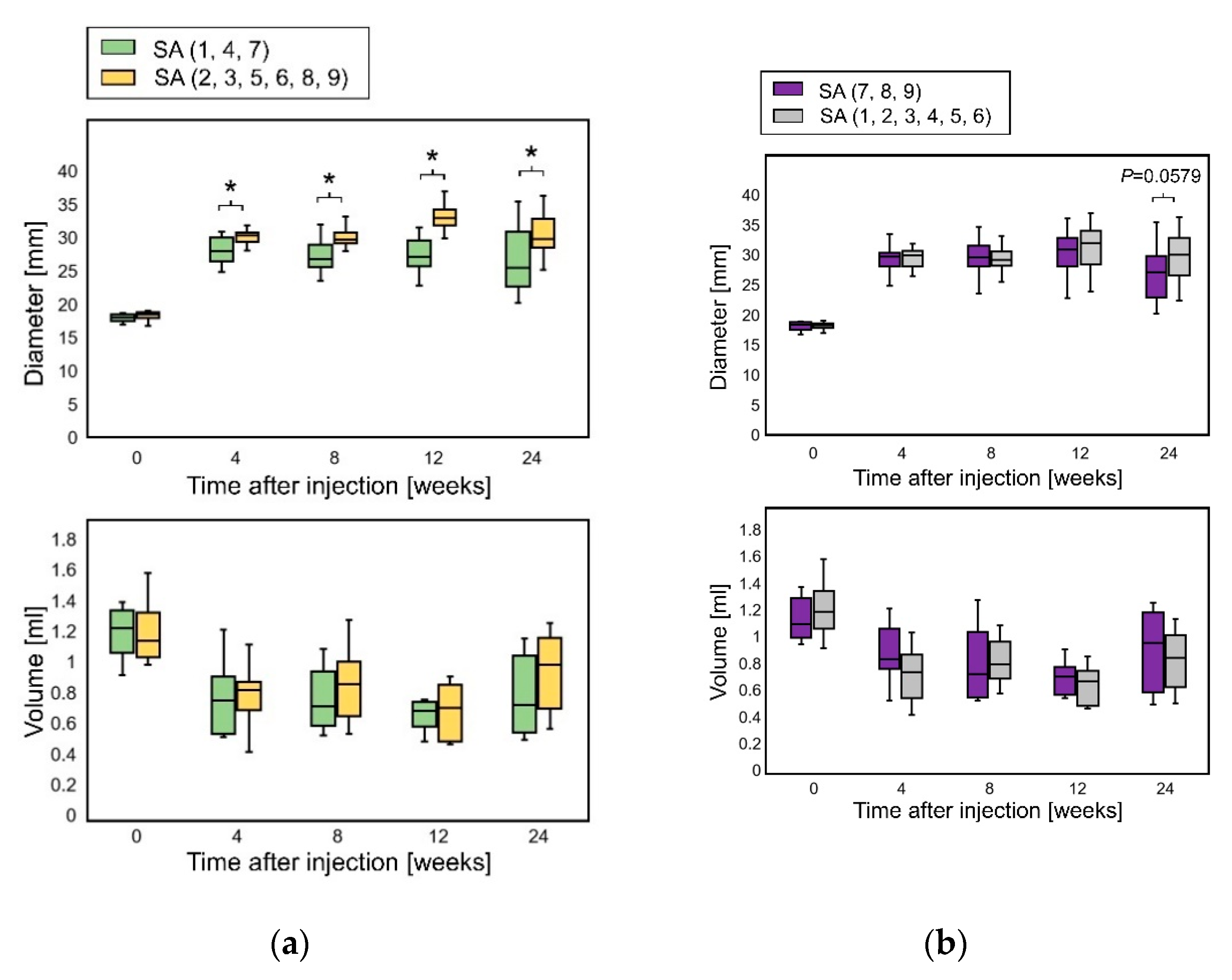
2.2. Sequential Changes in the Diameter and Volume
2.3. Elastica van Gieson Staining
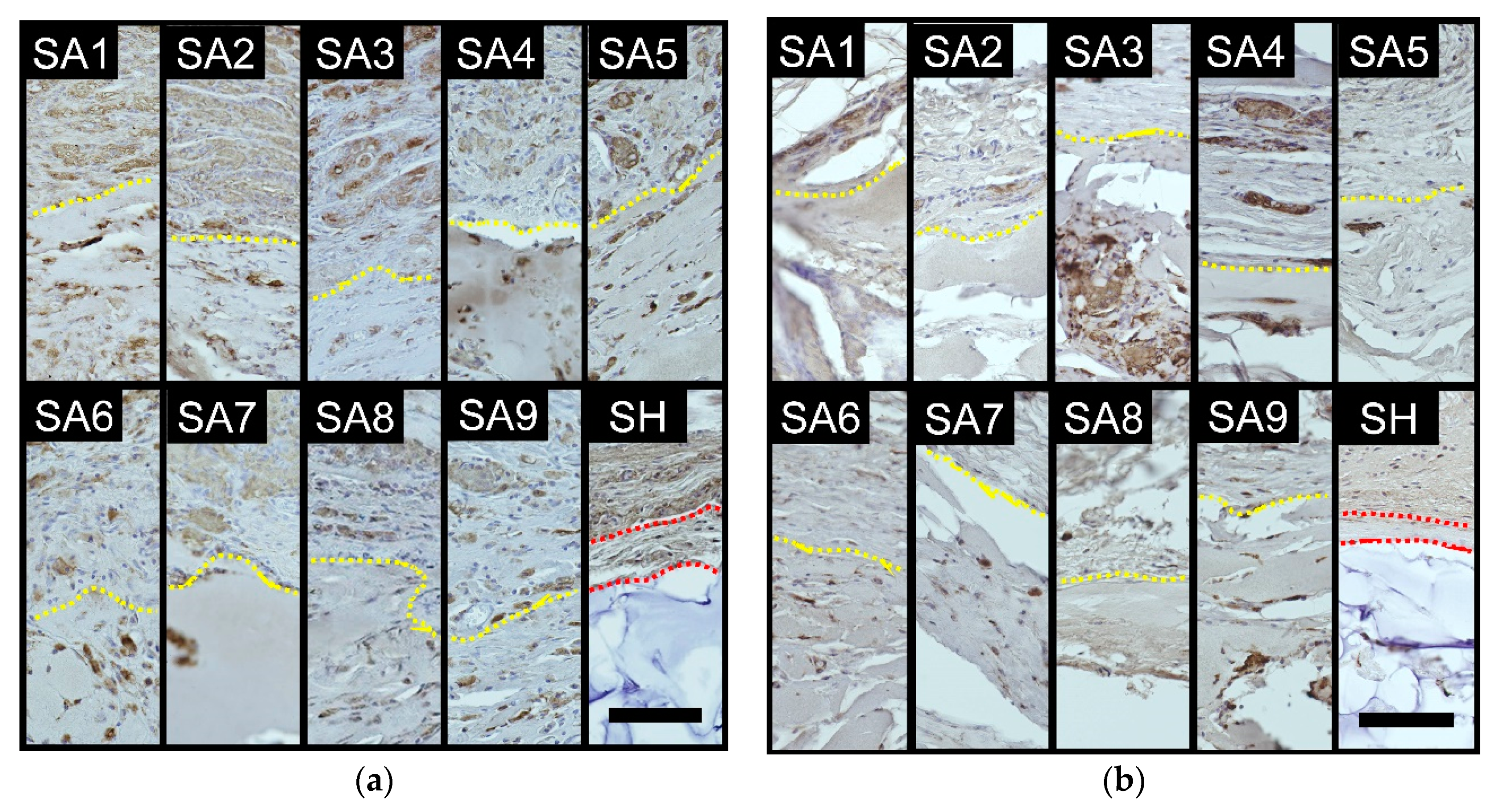
2.4. Immunohistochemical Staining of Macrophages
3. Discussion
4. Materials and Methods
4.1. Test Substances
4.2. Animals
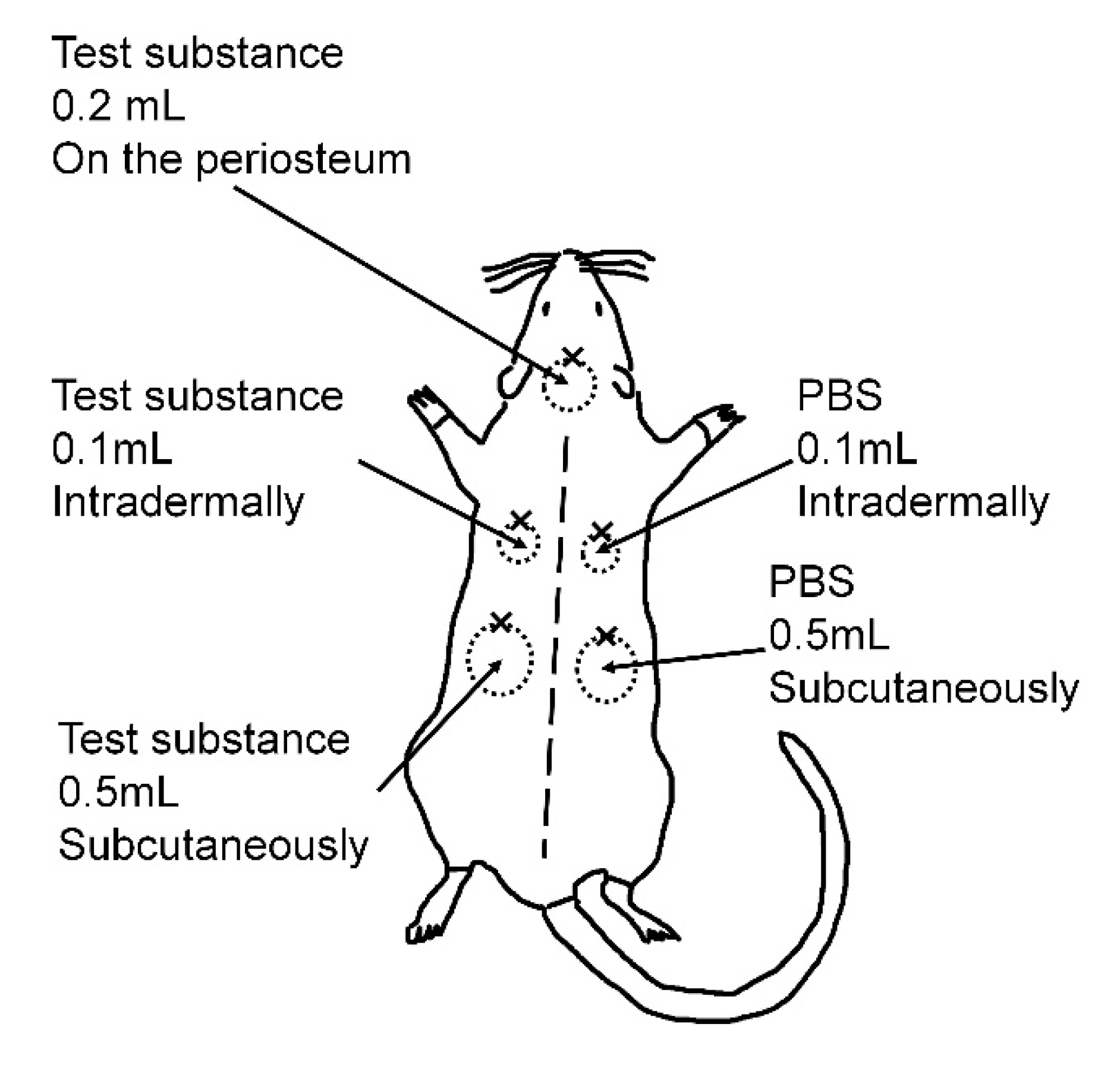
4.3. Injection Procedure
4.4. Diameter and Volume Measurements
4.5. Histopathological Analysis
4.6. Elastica van Gieson Staining
4.7. Immunohistochemical Staining of Macrophages
4.8. Statistical Analysis
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Mitura, S.; Sionkowska, A.; Jaiswal, A. Biopolymers for hydrogels in cosmetics: Review. J. Mater. Sci. Mater. Med. 2020, 31, 50. [Google Scholar] [CrossRef]
- Bacos, J.T.; Sayan, S.H. Superficial Dermal Fillers with Hyaluronic Acid. Facial Plast. Surg. 2019, 3, 219–223. [Google Scholar] [CrossRef]
- Carruthers, J.D.; Glogau, R.G.; Blitzer, A. Facial Aesthetics Consensus Group Faculty. Advances in facial rejuvenation: Botulinum toxin type a, hyaluronic acid dermal fillers, and combination therapies. Consensus recommendatuions. Plast. Reconst. Surg. 2008, 121, 5S–30S. [Google Scholar] [CrossRef] [PubMed]
- Xi, G.; Yan, W.; Yimin, Q.; Peili, S.; Qiang, P. Structures, propertied and application of alginic acid: A review. Int. J. Biol. Macromol. 2020, 11, 618–628. [Google Scholar]
- Scieszka, S.; Klewicka, E. Algae in food: A general review. Crit. Rev. Food Sci. Nutr. 2019, 21, 3538–3547. [Google Scholar] [CrossRef] [PubMed]
- Jain, D.; Shalom, B.D. Alginic drug delivery systems: Application in context of pharmaceutical and biomedical research. Drug Dev. Ind. Pharm. 2014, 12, 1576–1584. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Mooney, D.J. Alginate: Properties and biomedical applications. Progress in polymer. Science 2012, 1, 106–126. [Google Scholar]
- Filardo, G.; Perdisa, F.; Gelinsky, M.; Despang, F.; Fini, M.; Marcacci, M.; Parrilli, A.P.; Roffi, A.; Salamanna, F.; Sartori, M.; et al. Novel alginate biphasic scaffold for osteochondral regeneration: An in vivo evaluation in rabbit and sheep models. J. Mater. Sci. Mater. Med. 2018, 29, 74. [Google Scholar] [CrossRef]
- Daigo, K.; Wada, Y.; Yamada, C.; Yamaji, M.; Okuda, S.; Okada, M.; Miyazato, T. Pharmacological studies of sodium alginate. I. Protective effect of sodium alginate on mucous membranes of upper-gastrointestinal tract. Yakugaku Zasshi 1981, 101, 452–457. [Google Scholar] [CrossRef]
- Daigo, K.; Yamada, C.; Wada, Y.; Yamaji, M.; Okuda, S.; Okada, M.; Miyazato, T. Pharmacological studies of sodium alginate. II. Hemostatic effect of sodium alginate on gastrointestinal bleeding. Yakugaku Zasshi 1981, 101, 458–463. [Google Scholar] [CrossRef]
- Akagi, T.; Yasuda, K.; Tajima, M.; Suzuki, K.; Inomata, M.; Shiraishi, N.; Sato, Y.; Kitano, S. Sodium alginate as an ideal submucosal injection material for endoscopic submucosal resection: Preliminary experimental and clinical study. Gastrointest. Endosc. 2011, 5, 1026–1032. [Google Scholar] [CrossRef] [PubMed]
- Haug, A.; Larsen, B.; Smidsrød, O.; Hagen, G. Alkaline Degradation of Alginate. Acta Chemica Scandinavica 1967, 21, 2859–2870. [Google Scholar] [CrossRef]
- Voisin, M.; Engel, C.R.; Viard, F. Differential shuffling of native genetic diversity across introduced regions in a brown alga: Aquaculture vs. maritime traffic effects. Proc. Natl. Acad. Sci. USA 2005, 15, 5432–5437. [Google Scholar] [CrossRef]
- Ertesvåg, H. Alginate-modifying enzymes: Biological roles and biotechnological uses. Front. Microbiol. 2015, 6, 523. [Google Scholar] [PubMed]
- Ueno, M.; Oda, T. Biological activities of alginate. Adv. Food Nutr. Res. 2014, 72, 95–112. [Google Scholar]
- Andre, P.; Moulonguet, I. Alginate (Novabel): A new class of injectable filler. Facial Plast. Surg. 2014, 6, 644–646. [Google Scholar]
- Halberstadt, C.; Austin, C.; Rowley, J.; Culberson, C.; Loebsack, A.; Wyatt, S.; Coleman, S.; Blacksten, L.; Burg, K.; Mooney, D.; et al. A hydrogel material for plastic and reconstructive applications injected into the subcutaneous space of a sheep. Tissue Eng. 2002, 2, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Menard, M.; Dusseault, J.; Langlois, G.; Menard, M.; Dusseault, J.; Langlois, G.; Baille, W.E.; Tam, S.K.; Yahia, L.; Zhu, X.X.; et al. Role of protein contaminants in the immunogenicity of alginates. J. Biomed. Mater. Res. B Appl. Biomater. 2010, 2, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Moulonguet, I.; de Goursac, C.; Plantier, F. Granulomatous reaction after injection of a new resorbable filler Novabel. Am. J. Dermatopathol. 2011, 7, 710–711. [Google Scholar] [CrossRef]
- Schuller-Petrovic, S.; Pavlovic, M.D.; Schukker, S.S.; Sculler-Lukic, B.; Neuhold, N. Early granulomatous foreign body reactions to a novel alginate dermal filler: The system’s failure? J. Eur. Acad. Dermatol. Venereol. 2013, 1, 121–123. [Google Scholar] [CrossRef]
- Santos, J.M.; Pereira, S.; Sequeira, D.B.; Messias, A.L.; Martins, J.B.; Cunha, H.; Palma, P.J.; Santos, A.C. Biocompatibility of a bioceramic silicone-based sealer in subcutaneous tissue. J. Oral Sci. 2019, 1, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 3, 452–458. [Google Scholar] [CrossRef] [PubMed]

| The Capsule Thickness (µm) | |
|---|---|
| SA1 | 0.0 ± 0.0 |
| SA2 | 0.0 ± 0.0 |
| SA3 | 0.0 ± 0.0 |
| SA4 | 0.0 ± 0.0 |
| SA5 | 0.0 ± 0.0 |
| SA6 | 0.0 ± 0.0 |
| SA7 | 0.0 ± 0.0 |
| SA8 | 0.0 ± 0.0 |
| SA9 | 0.0 ± 0.0 |
| SH | 52.9 ± 7.2 |
| Macrophages/Granulomatous Reaction | ||
|---|---|---|
| 4 Weeks | 24 Weeks | |
| SA1 | ++/++ | +/++ |
| SA2 | ++/++ | +/+ |
| SA3 | ++/+ | +/± |
| SA4 | ++/++ | +/++ |
| SA5 | ++/++ | +/+ |
| SA6 | ++/+ | +/+ |
| SA7 | ++/+ | +/± |
| SA8 | ++/+ | +/– |
| SA9 | ++/+ | +/± |
| SH | +/– | ±/– |
| Type | M/G Ratio † | Viscosity (Pa·s) | Extrusion Force (N) |
|---|---|---|---|
| SA1 | 0.3 | 1.0 ± 0.0 | 10.9 ± 0.0 |
| SA2 | 1.4 | 1.3 ± 0.0 | 14.7 ± 0.0 |
| SA3 | 1.7 | 1.5 ± 0.0 | 15.0 ± 0.0 |
| SA4 | 0.3 | 10.1 ± 0.1 | 15.8 ± 0.1 |
| SA5 | 1.1 | 8.4 ± 0.0 | 14.9 ± 0.0 |
| SA6 | 1.6 | 8.5 ± 0.4 | 16.4 ± 0.4 |
| SA7 | 0.4 | 18.2 ± 0.2 | 16.0 ± 0.2 |
| SA8 | 1.4 | 19.9 ± 0.1 | 16.8 ± 0.1 |
| SA9 | 1.6 | 15.8 ± 0.1 | 17.1 ± 0.1 |
| SH | N/A | 23.2 ± 0.1 | 11.1 ± 0.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mori, M.; Asahi, R.; Yamamoto, Y.; Mashiko, T.; Yoshizumi, K.; Saito, N.; Shirado, T.; Wu, Y.; Yoshimura, K. Sodium Alginate as a Potential Therapeutic Filler: An In Vivo Study in Rats. Mar. Drugs 2020, 18, 520. https://doi.org/10.3390/md18100520
Mori M, Asahi R, Yamamoto Y, Mashiko T, Yoshizumi K, Saito N, Shirado T, Wu Y, Yoshimura K. Sodium Alginate as a Potential Therapeutic Filler: An In Vivo Study in Rats. Marine Drugs. 2020; 18(10):520. https://doi.org/10.3390/md18100520
Chicago/Turabian StyleMori, Masanori, Rintaro Asahi, Yoshihiro Yamamoto, Takanobu Mashiko, Kayo Yoshizumi, Natsumi Saito, Takako Shirado, Yunyan Wu, and Kotaro Yoshimura. 2020. "Sodium Alginate as a Potential Therapeutic Filler: An In Vivo Study in Rats" Marine Drugs 18, no. 10: 520. https://doi.org/10.3390/md18100520
APA StyleMori, M., Asahi, R., Yamamoto, Y., Mashiko, T., Yoshizumi, K., Saito, N., Shirado, T., Wu, Y., & Yoshimura, K. (2020). Sodium Alginate as a Potential Therapeutic Filler: An In Vivo Study in Rats. Marine Drugs, 18(10), 520. https://doi.org/10.3390/md18100520




