DSPE-PEG Modification of α-Conotoxin TxID
Abstract
1. Introduction
2. Results
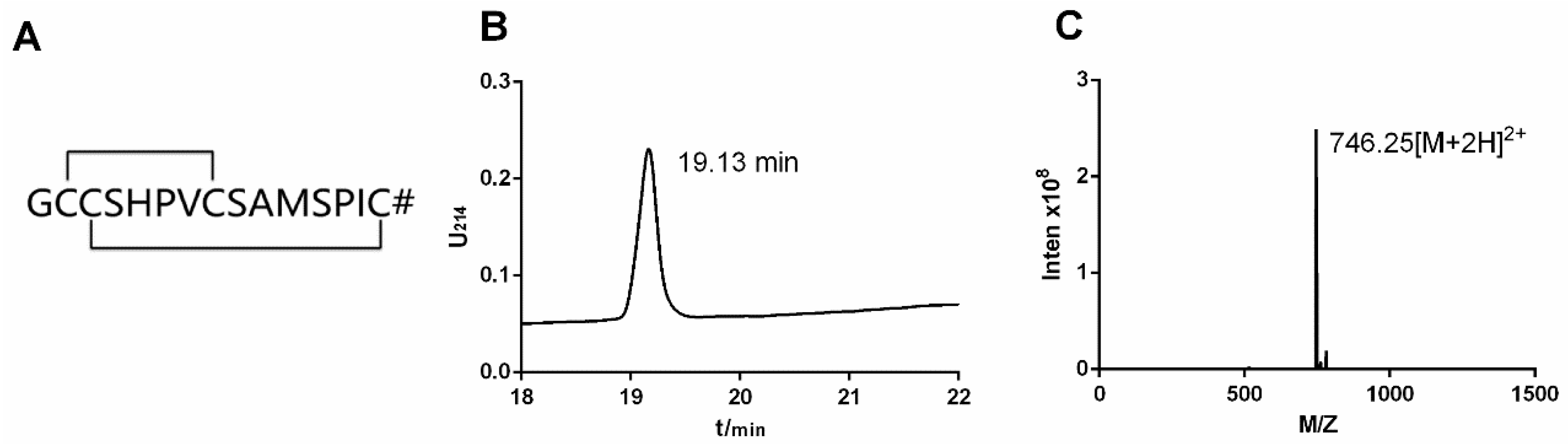
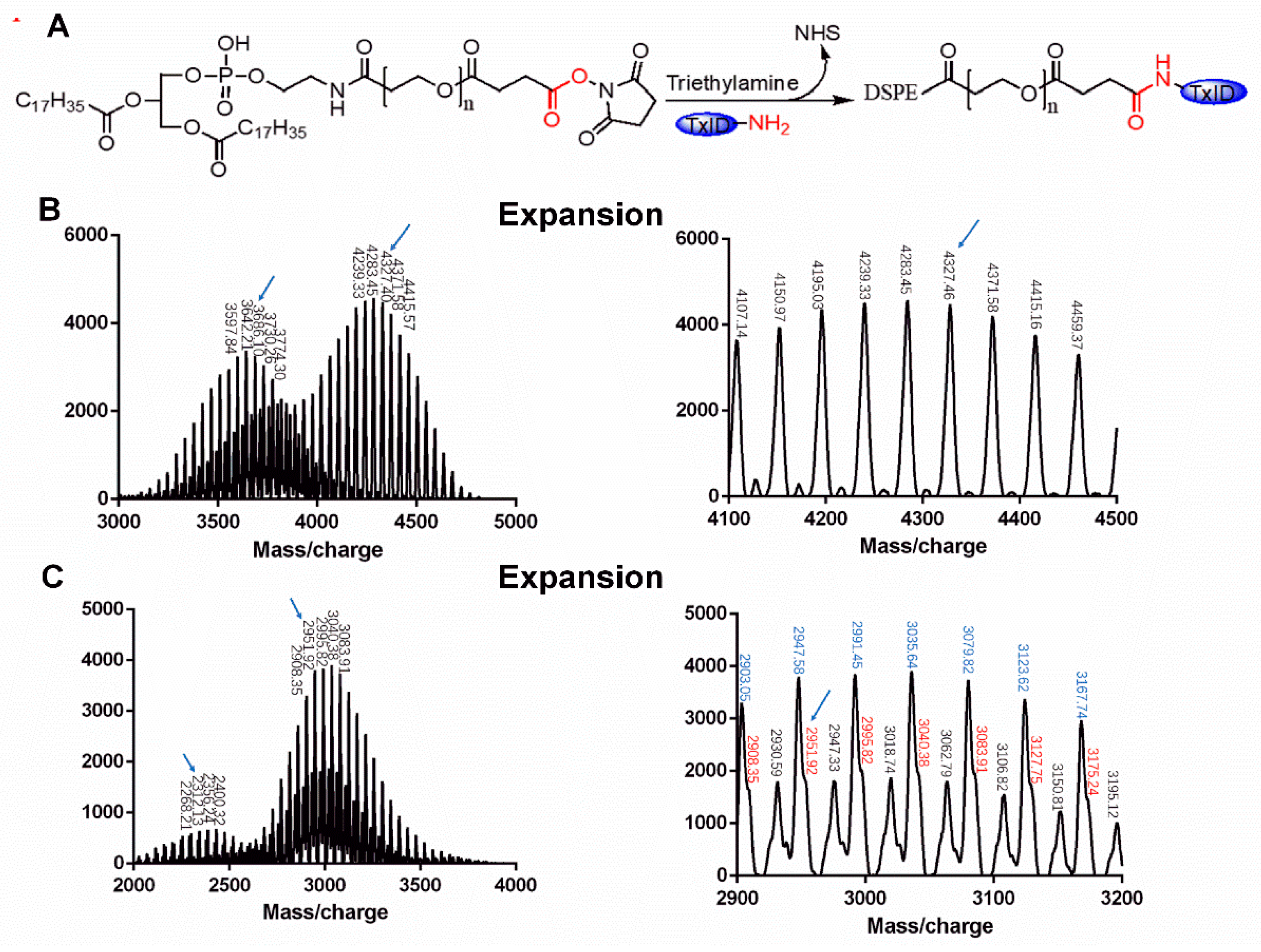
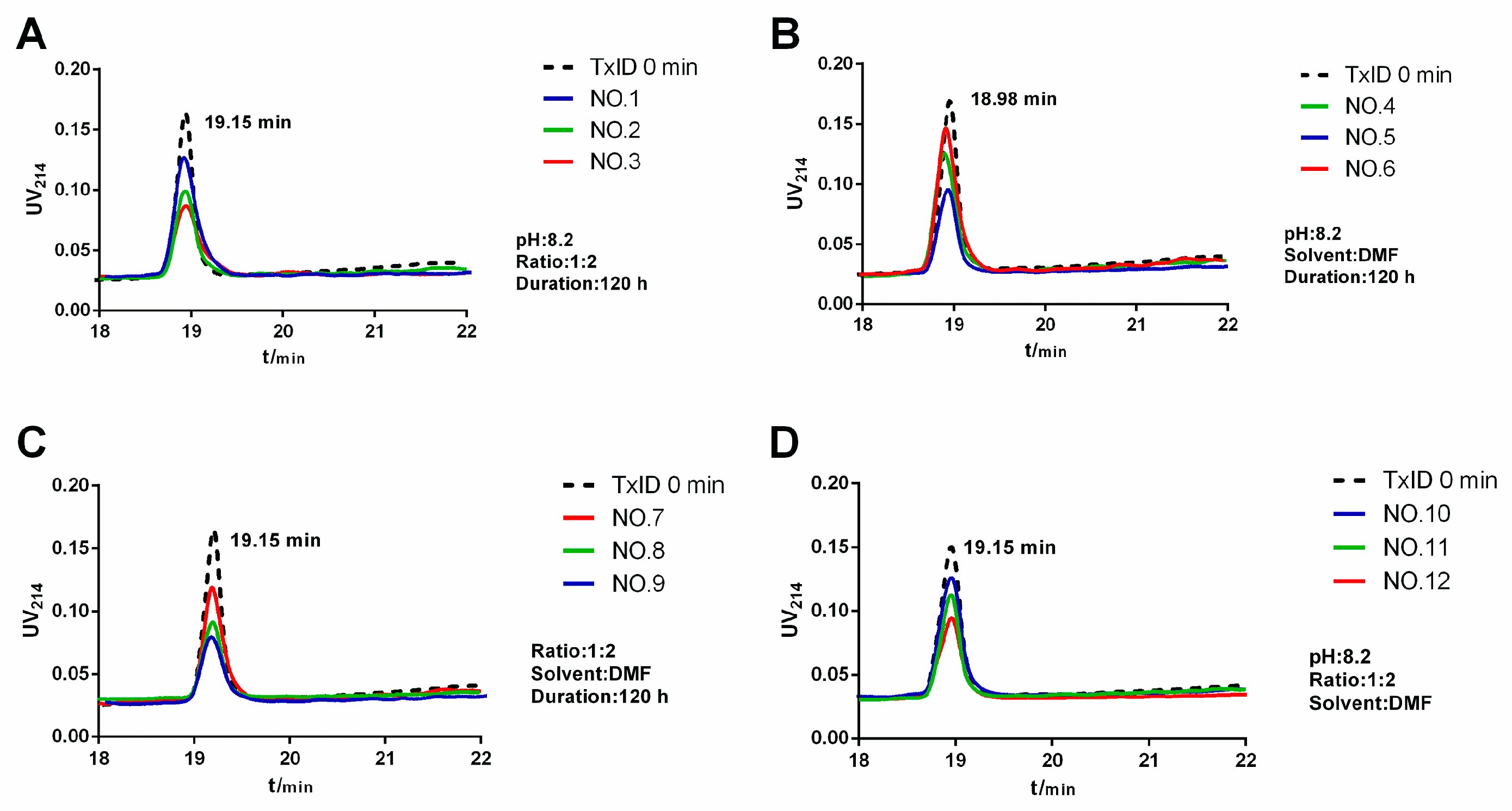
2.1. Synthesis and Identification of DSPE-PEG-TxID
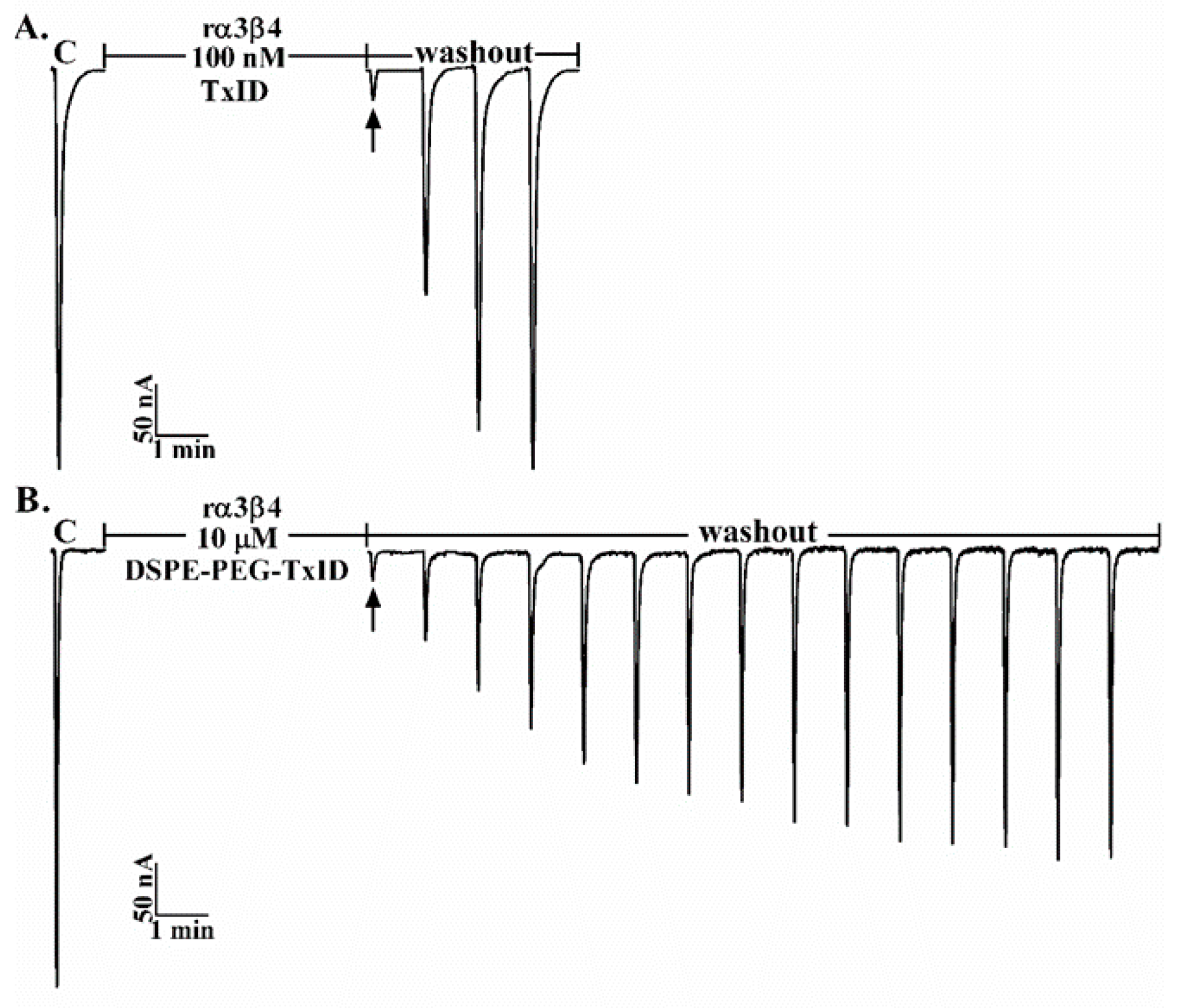
2.2. Potency of TxID and DSPE-PEG-TxID on α3β4 nAChR
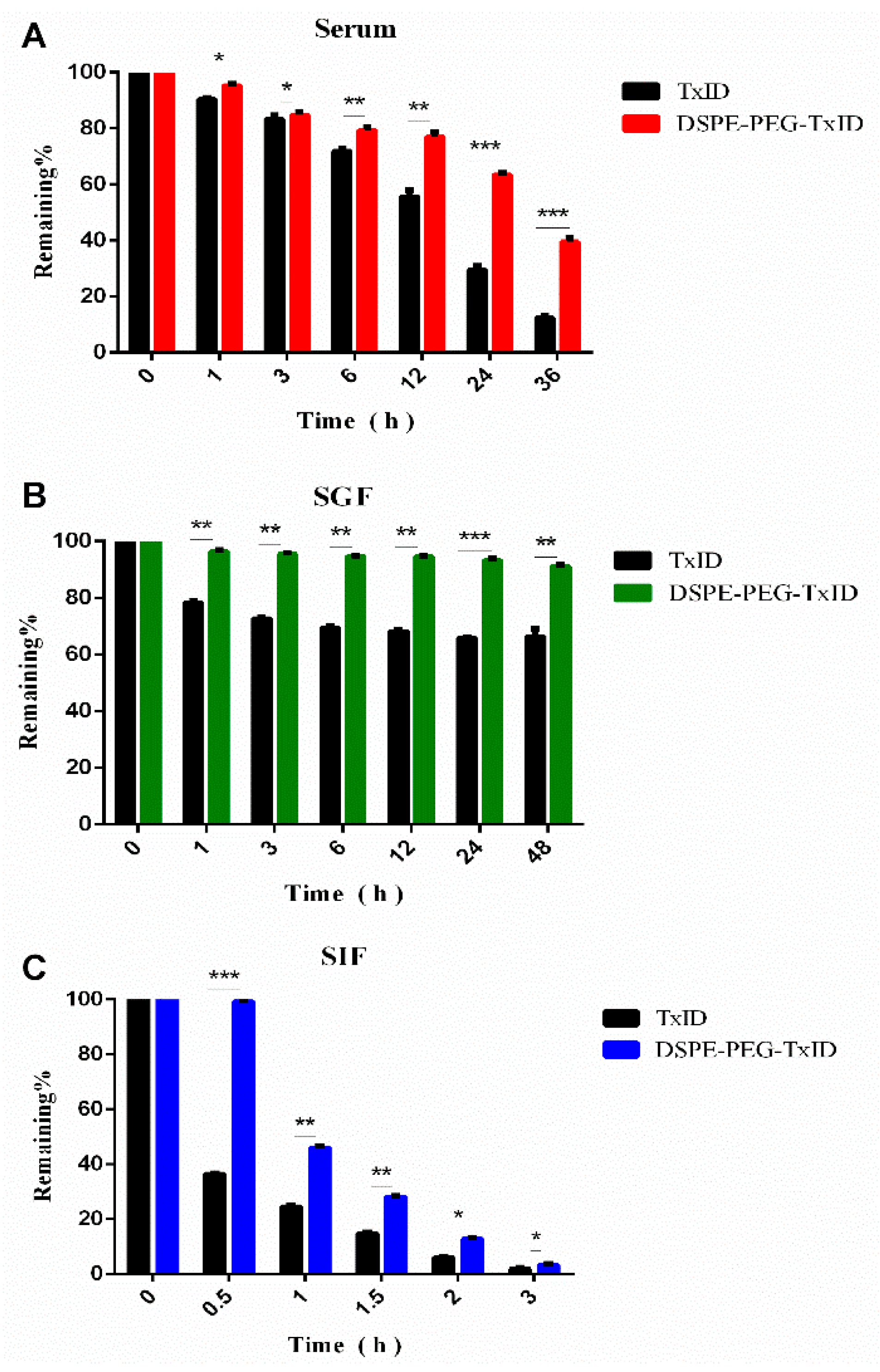
2.3. Stability of TxID and DSPE-PEG-TxID
3. Discussion
4. Materials and Methods
4.1. Synthesis of DSPE-PEG-TxID
4.2. Activity of DSPE-PEG-TxID on α3β4 nAChR
4.3. Stability Assessment of DSPE-PEG-TxID
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| Abbreviation | Full name in English |
| CTx | Conotoxin |
| nAChR | Nicotinic Acetylcholine Receptor |
| TFA | Trifluoroacetic Acid |
| RP-HPLC | Reversed-Phase High-Performance Liquid Chromatography |
| DSPE-PEG-NHS | 1,2-distearoyl-sn-glycero-3-phosphoeth-anolamine-N-[hydroxyl succinimidyl (polyethylene glycol)-2000] |
| DMF | N,N-Dimethylformamide |
| LC-MS | Liquid Chromatograph Mass Spectrometer |
| MADLI-TOF-MS | Matrix-Assisted Laser Desorption/ Ionization Time of Flight Mass Spectrometry |
| DMSO | Dimethyl Sulfoxide |
| PBS | Phosphate Buffer Saline |
| SGF | Simulated Gastric Fluid |
| SIF | Simulated Intestinal Fluid |
References
- Hurst, R.; Rollema, H.; Bertrand, D. Nicotinic acetylcholine receptors: From basic science to therapeutics. Pharmacol. Ther. 2013, 137, 22–54. [Google Scholar] [CrossRef] [PubMed]
- Albuquerque, E.X.; Pereira, E.F.R.; Manickavasagom, A.; Rogers, S.W. Mammalian nicotinic acetylcholine receptors: from structure to function. Physiol. Rev. 2009, 89, 73–120. [Google Scholar] [CrossRef] [PubMed]
- Gotti, C.; Clementi, F. Neuronal nicotinic receptors: from structure to pathology. Prog. Neurobiol. 2004, 74, 363–396. [Google Scholar] [CrossRef] [PubMed]
- Dong-Ting, Z.; Yong, W.U.; Zhu, X.P.; Luo, S.L. Sensitivity of α-Conotoxin TxID on Stoichiometry of α3β4 Nicotinic Acetylcholine Receptors. Chin. Pharm. J. 2016, 51, 802–808. [Google Scholar]
- Luo, S.; Christensen, S.; Zhangsun, D.; Wu, Y.; Hu, Y.; Zhu, X.; Chhabra, S.; Norton, R.S.; McIntosh, J.M. A novel inhibitor of α9α10 nicotinic acetylcholine receptors from Conus vexillum delineates a new conotoxin superfamily. PLoS ONE 2013, 8, 546–548. [Google Scholar] [CrossRef] [PubMed]
- Luo, S.; Zhangsun, D.; Harvey, P.J.; Kaas, Q.; Wu, Y.; Zhu, X.; Hu, Y.; Li, X.; Tsetlin, V.I.; Christensen, S.; et al. Cloning, synthesis, and characterization of αO-conotoxin GeXIVA, a potent α9α10 nicotinic acetylcholine receptor antagonist. Proc. Natl. Acad. Sci. USA 2015, 112, 4026–4035. [Google Scholar] [CrossRef] [PubMed]
- Mannelli, L.D.C.; Cinci, L.; Micheli, L.; Zanardelli, M.; Pacini, A.; Mcintosh, J.M.; Ghelardini, C. α-Conotoxin RgIA protects against the development of nerve injury-induced chronic pain and prevents both neuronal and glial derangement. Pain 2014, 155, 1986–1995. [Google Scholar] [CrossRef] [PubMed]
- Layla, A.J.; Michael, M. α-Conotoxins as pharmacological probes of nicotinic acetylcholine receptors. Acta Pharmacol. Sin. 2009, 30, 771–783. [Google Scholar]
- Olivera, B.M.; Quik, M.; Vincler, M.; Mcintosh, J.M. Subtype-selective conopeptides targeted to nicotinic receptors: Concerted discovery and biomedical applications. Channels 2008, 2, 143–152. [Google Scholar] [CrossRef]
- Tang, L.; Persky, A.M.; Hochhaus, G.; Meibohm, B. Pharmacokinetic aspects of biotechnology products. J. Pharm. Sci. 2004, 93, 2184–2204. [Google Scholar] [CrossRef]
- Sanchez-Ruiz, J.M. Protein kinetic stability. J. Biophys. Chem. 2010, 148, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Pascal, B.; Chee-Youb, W. PEG-modified biopharmaceuticals. Exp. Opin. Drug Deliv. 2009, 6, 1–16. [Google Scholar]
- Fishburn, C.S. The pharmacology of PEGylation: Balancing PD with PK to generate novel therapeutics. J. Pharm. Sci. 2010, 97, 4167–4183. [Google Scholar] [CrossRef] [PubMed]
- Tong, S.W.; Xiang, B.; Dong, D.W.; Qi, X.R. Enhanced antitumor efficacy and decreased toxicity by self-associated docetaxel in phospholipid-based micelles. Int. J. Pharm. 2012, 434, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Wu, H.; Zhu, L.; Torchilin, V.P. pH-sensitive poly(histidine)-PEG/DSPE-PEG co-polymer micelles for cytosolic drug delivery. Biomaterials 2013, 34, 1213–1222. [Google Scholar] [CrossRef]
- Pasut, G.; Veronese, F.M. State of the art in PEGylation: The great versatility achieved after forty years of research. J. Control. Release 2012, 161, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Zündorf, I.; Dingermann, T. PEGylation―A well-proven strategy for the improvement of recombinant drugs. Pharmazie 2014, 69, 323–326. [Google Scholar]
- Li-Qiang, P.; Hai-Bin, W.; Jun, L.; Ying-Chun, X.; Chen, Z.; Shu-Qing, C. Site-specific PEGylation of a mutated-cysteine residue and its effect on tumor necrosis factor (TNF)-related apoptosis-inducing ligand (TRAIL). Biomaterials 2013, 34, 9115–9123. [Google Scholar]
- Kompella, S.N.; Andrew, H.; Clark, R.J.; Frank, M.; Adams, D.J. Alanine scan of α-conotoxin RegIIA reveals a selective α3β4 nicotinic acetylcholine receptor antagonist. J. Biol. Chem. 2015, 290, 1039–1048. [Google Scholar] [CrossRef]
- Luo, S.; Zhangsun, D.; Zhu, X.; Wu, Y.; Hu, Y.; Christensen, S.; Harvey, P.J.; Akcan, M.; Craik, D.J.; Mcintosh, J.M. Characterization of a Novel α-Conotoxin TxID from Conus textile that Potently Blocks rat α3β4 Nicotinic Acetylcholine Receptors. J. Med. Chem. 2013, 288, 894–902. [Google Scholar] [CrossRef]
- Napier, I.A.; Klimis, H.; Rycroft, B.K.; Jin, A.H.; Alewood, P.F.; Motin, L.; Adams, D.J.; Christie, M.J. Intrathecal α-conotoxins Vc1.1, AuIB and MII acting on distinct nicotinic receptor subtypes reverse signs of neuropathic pain. Neuropharmacology 2012, 62, 2201–2206. [Google Scholar] [CrossRef] [PubMed]
- Improgo, M.R.; Soll, L.G.; Tapper, A.R.; Gardner, P.D. Nicotinic acetylcholine receptors mediate lung cancer growth. Front. Physiol. 2013, 4, 251. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.D.; Norton, R.S. Conotoxin gene superfamilies. Mar. Drugs 2014, 12, 6058–6101. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Yadav, V.; Smart, A.L.; Tajiri, S.; Basit, A.W. Toward oral delivery of biopharmaceuticals: An assessment of the gastrointestinal stability of 17 peptide drugs. Mol. Pharm. 2015, 12, 966–973. [Google Scholar] [CrossRef]
- Maddux, N.R.; Joshi, S.B.; Volkin, D.B.; Ralston, J.P.; Middaugh, C.R. Multidimensional methods for the formulation of biopharmaceuticals and vaccines. J. Pharm. Sci. 2011, 100, 4171–4197. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dai, Q.Y.; Liu, F.Y.; Zhou, Y.R. The synthesis of SO-3, a conopeptide with high analgesic activity derived from Conus striatus. J. Nat. Prod. 2003, 66, 1276–1279. [Google Scholar] [CrossRef]
- Clark, R.J.; Jensen, J.; Nevin, S.T.; Callaghan, B.P.; Adams, D.J.; Craik, D.J. The Engineering of an Orally Active Conotoxin for the Treatment of Neuropathic Pain. Angew. Chem. Int. Ed. Engl. 2010, 49, 6545–6548. [Google Scholar] [CrossRef]
- Mross, K.; Richly, H.; Fischer, R.; Scharr, D.; Büchert, M.; Stern, A.; Gille, H.; Audoly, L.P.; Scheulen, M.E. First-in-human phase I study of PRS-050 (Angiocal), an Anticalin targeting and antagonizing VEGF-A, in patients with advanced solid tumors. PLoS ONE 2013, 8, e83232. [Google Scholar] [CrossRef][Green Version]
- Tamizi, E.; Jouyban, A. Forced degradation studies of biopharmaceuticals: Selection of stress conditions. Eur. J. Pharm. Biopharm. 2016, 98, 26–46. [Google Scholar] [CrossRef]
- Luo, S.; Zhangsun, D.; Schroeder, C.I.; Zhu, X.; Hu, Y.; Wu, Y.; Weltzin, M.M.; Eberhard, S.; Kaas, Q.; Craik, D.J.; et al. A novel α4/7-conotoxin LvIA from Conus lividus that selectively blocks α3β2 vs. α6/α3β2β3 nicotinic acetylcholine receptors. FASEB J. 2014, 28, 1842–1853. [Google Scholar] [CrossRef]
- Zhangsun, D.; Zhu, X.; Wu, Y.; Hu, Y.; Kaas, Q.; Craik, D.J.; Mclntosh, J.M.; Luo, S. Key residues in the nicotinic acetylcholine receptor β2 subunit contribute to α-conotoxin LvIA binding. J. Biol. Chem. 2015, 290, 9855–9862. [Google Scholar] [CrossRef] [PubMed]
- Mei, D.; Lin, Z.; Fu, J.; He, B.; Gao, W.; Ma, L.; Dai, W.; Zhang, H.; Wang, X.; Wang, J.; et al. The use of α-conotoxin ImI to actualize the targeted delivery of paclitaxel micelles to α7 nAChR-overexpressing breast cancer. Biomaterials 2015, 42, 52–65. [Google Scholar] [CrossRef] [PubMed]
- Defu, C.; Wei, G.; Bing, H.; Wenbing, D.; Hua, Z.; Xueqing, W.; Jiancheng, W.; Xuan, Z.; Qiang, Z. Hydrophobic penetrating peptide PFVYLI-modified stealth liposomes for doxorubicin delivery in breast cancer therapy. Biomaterials 2014, 35, 2283–2294. [Google Scholar]
- Oba, T.; Matsunaka, R.; Dai, N.; Yamane, K. The United States Pharmacopeia, 19th ed.; The United States Pharmacopeial Convention, Inc., Mack Publishing Co.: Easton, PA, USA, 1974. [Google Scholar]
| Product | Company | Modifier | Indication | Time to Market |
|---|---|---|---|---|
| Rurioctocog Alfa Pegol | Schering-Plough | Growth Factor VIII | Hemophilia | 2016 |
| Pegloticase | Horizon Pharma plc | Recombinant Uricase | Gout | 2016 |
| Naloxegol | AstraZeneca | Opioid Receptor Agonist | Constipation | 2015 |
| Omontys | Affymax | PEG-Erythrocyte Stimulating Agent | Anemia | 2012 |
| Krystexxa | Savient | PEG-Porcine Uricase | Gout | 2010 |
| Cimzia | UCB | PEG-TNF Antibody Fab Segment | Rheumatoid Arthritis | 2008 |
| Mircera | Roche | PEG-EPO | Anemia | 2007 |
| Pegaptanib | NeXstar | VEGF Receptor Agonist | Senile Macular | 2005 |
| Macugen | OSI/Pfizer | PEG-Nucleic Acid Ligand | Senile Macular | 2004 |
| Pegvisomant | Pfizer | EG-Growth Hormone Antagonist | Limb Hypertrophy | 2003 |
| Number | Solvent | Peptide: PEG | pH | Duration (h) | % Remaining Amount |
|---|---|---|---|---|---|
| 1 | PBS | 63.28 | |||
| 2 | DMSO | 1:2 | 8.2 | 120 | 34.16 |
| 3 | DMF | 36.02 | |||
| 4 | 1:1 | 66.84 | |||
| 5 | DMF | 1:2 | 8.2 | 120 | 31.55 |
| 6 | 2:1 | 85.88 | |||
| 7 | 6.2 | 47.46 | |||
| 8 | DMF | 1:2 | 7.2 | 120 | 31.64 |
| 9 | 8.2 | 29.94 | |||
| 10 | 54 | 68.25 | |||
| 11 | DMF | 1:2 | 8.2 | 78 | 48.65 |
| 12 | 120 | 34.61 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, W.; Xiong, Y.; Zhangsun, D.; Luo, S. DSPE-PEG Modification of α-Conotoxin TxID. Mar. Drugs 2019, 17, 342. https://doi.org/10.3390/md17060342
Zhao W, Xiong Y, Zhangsun D, Luo S. DSPE-PEG Modification of α-Conotoxin TxID. Marine Drugs. 2019; 17(6):342. https://doi.org/10.3390/md17060342
Chicago/Turabian StyleZhao, Weinan, Yang Xiong, Dongting Zhangsun, and Sulan Luo. 2019. "DSPE-PEG Modification of α-Conotoxin TxID" Marine Drugs 17, no. 6: 342. https://doi.org/10.3390/md17060342
APA StyleZhao, W., Xiong, Y., Zhangsun, D., & Luo, S. (2019). DSPE-PEG Modification of α-Conotoxin TxID. Marine Drugs, 17(6), 342. https://doi.org/10.3390/md17060342






