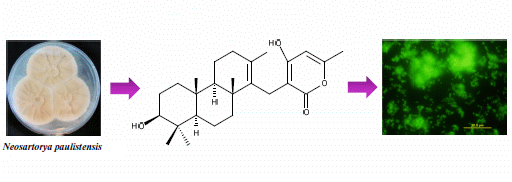
Antibacterial and Antibiofilm Activities of Tryptoquivalines and Meroditerpenes Isolated from the Marine-Derived Fungi Neosartorya paulistensis, N. laciniosa, N. tsunodae, and the Soil Fungi N. fischeri and N. siamensis
Abstract
:1. Introduction

| Position | δC, Type | δH, (J in Hz) | COSY | HMBC |
|---|---|---|---|---|
| 1 | --- | --- | ||
| 2 | 81.0, CH | 6.10, s | H-29 | C-3, 13, 14 |
| 3 | 84.2, C | --- | ||
| 4 | 133.5,C | --- | ||
| 5 | 126.8, CH | 8.04, dd (8.0, 1.0) | H-6 | C-3, 7, 9 |
| 6 | 126.7, CH | 7.46, ddd (8.0, 8.0, 1.0) | H-5 | C-4, 8 |
| 7 | 131.8, CH | 7.61, ddd (8.0, 8.0, 1.0) | H-6, 8 | C-5, 9 |
| 8 | 116.4, CH | 7.56, ddd (8.0, 1.0) | H-7 | C-4, 6 |
| 9 | 138.4, C | --- | ||
| 11 | 171.1, CO | --- | ||
| 12 | 57.7, CH | 5.47, dd (10.7, 8.6) | H-13 | C-11, 18 |
| 13a | 33.8, CH2 | 3.30, dd (14.0, 8.6) | H-12, 13b | C-2, 3, 4 |
| b | 3.40, dd (14.0, 10.7) | H-12, 13a | C-2, 3, 4 | |
| 14 | 172.5, CO | --- | ||
| 15 | 64.1, C | --- | ||
| 18 | 160.0, CO | --- | ||
| 19 | 121.4, C | --- | ||
| 20 | 126.2, CH | 8.26, d (8.0, 1.0) | H-21 | C-18, 22, 24 |
| 21 | 127.6, CH | 7.63, ddd (8.0, 8.0, 1.0) | H-20, 22 | C-19, 23 |
| 22 | 135.1, CH | 7.93, ddd (8.0, 8.0, 1.0) | H-21, 23 | C-20, 24 |
| 23 | 127.4, CH | 7.76, d (8.0) | H-22 | C-19, 21 |
| 24 | 147.8, C | --- | ||
| 26 | 148.1, CH | 8.62, s | C-12, 18, 24 | |
| 27 | 26.6, CH3 | 1.72, s | C-14, 15, 28 | |
| 28 | 25.5, CH3 | 1.55, s | C-14, 15, 27 | |
| 29 | 162.3, CHO | 8.73, d (0.9) | H-2 | C-2 |
2. Results and Discussion
| Position | δC, Type | δH, (J in Hz) | COSY | HMBC |
|---|---|---|---|---|
| 1 | 37.9, CH2 | 1.65, m | H-2 | |
| 2 | 27.1, CH2 | 1.46, m | H-1, 3 | |
| 3 | 76.9, CH | 2.97, m | H-2 | |
| 4 | 38.4, C | --- | --- | |
| 5 | 54.8, CH | 0.67, brd (9.6) | H-6 | |
| 6 | 17.7, CH2 | 1.35, m | H-5, 7 | |
| 7 | 38.0, CH2 | 1.96, m | H-6 | |
| 8 | 38.8, C | -- | ||
| 9 | 56.0, CH | 0.97, brd (11.4) | H-11 | CH3-24 |
| 10 | 36.8, C | --- | ||
| 11 | 18.2, CH2 | 1.46, m | H-9, 12 | |
| 12 | 34.2, CH2 | 1.94, m | H-11 | |
| 13 | 126.2, C | --- | --- | |
| 14 | 136.6, C | --- | --- | |
| 15 | 22.1, CH2 | 3.02, brs | --- | C-8, 13, 14, 16, 17, 21 |
| 16 | 101.4, C | --- | --- | |
| 17 | 164.3, C | --- | --- | |
| 18 | 99.9, CH | 5.90, s | CH3-20, C-1617, 19, 20 | |
| 19 | 159.3, C | --- | --- | |
| 20 | 19.2, CH3 | 2.12, s | H-18 | C-18, 19 |
| 21 | 164.6, C | --- | --- | C-3, 4, 5, 23 |
| 22 | 28.1, CH3 | 0.86, s | --- | C-3, 4, 5, 22 |
| 23 | 15.7, CH3 | 0.66, s | --- | |
| 24 | 16.3, CH3 | 0.77, s | --- | C-1, 5, 9, 10 |
| 25 | 21.2, CH3 | 0.89, s | --- | C-8, 9, 14 |
| 26 | 20.3, CH3 | 1.55, s | --- | C-12, 13, 14 |
| (A) | ||||||||
| Compounds | S. aureus ATCC 25923 | P. aeruginosa ATCC 27853 | B. subtilis ATCC 6633 | E. coli ATCC 25922 | ||||
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| 1a | 128 | − | 128 | 256 | 128 | − | 128 | − |
| 1b | 128 | − | 128 | 256 | 128 | − | 128 | − |
| 1c | 128 | − | 128 | 128 | 128 | − | 128 | − |
| 1d | − | − | 128 | − | 128 | − | 128 | − |
| 2 | 256 | − | 128 | 256 | 128 | − | 128 | − |
| 3 | 128 | − | 128 | 256 | 128 | − | 128 | − |
| 4a | 8 | 64 | 128 | 256 | 8 | 16 | 128 | − |
| 4b | 256 | − | 128 | 256 | 128 | − | 128 | − |
| 5 | 128 | − | 128 | 256 | 128 | − | 128 | − |
| 6 | − | − | − | − | − | − | − | − |
| 7a | − | − | − | − | − | − | − | − |
| 7b | − | − | − | − | − | − | − | − |
| 8 | 32 | − | − | − | 64 | − | − | − |
| (B) | ||||||||
| Compounds | S. aureus B1 | S. aureus B1 | E. faecalis W1 | E. faecium W5 | ||||
| MIC | MBC | MIC | MBC | MIC | MBC | MIC | MBC | |
| 4a | 8 | − | 8 | − | 16 | − | 16 | − |
| 8 | 32 | − | 32 | − | − | − | − | − |
| E. coli G1 | S. aureus B1 | E. faecium W5 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Antibiotics | ||||||||||
| Compounds | CIP | AMP | CTX | S | OX | AMP | CTX | VA | AMP | E |
| 1a | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 1b | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 1c | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 1d | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 2 | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 3 | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 4a | 8 | 8 | = | 8 | 12.5 | 13 | 13 | 11 | 12 | 13.5 |
| 4b | 7 | 7 | = | 7.5 | 11 | 10 | 10.5 | 11 | 12 | 13.5 |
| 5 | 7 | 7 | = | 7.5 | = | = | = | = | = | = |
| 6 | 7 | 7 | = | 7.5 | = | 9 | = | = | = | = |
| 7a | 8 | 8 | = | 8 | 9.5 | 10 | 9.5 | 8.5 | 9 | 8 |
| 7b | 7 | 7.5 | = | 7.5 | 8.5 | 9.5 | 8.5 | = | = | = |
| 8 | 7.5 | 7.5 | = | 7.5 | 10 | 10 | 10 | 8.5 | 7 | 7 |
| Control | 0 | 0 | 14 | 0 | 0 | 7 | 0 | 8 | 0 | 0 |
| Bacterial Isolate | 4a-OX | 8-OX | 4a-VA | 8-Va | 4a-AMP | 8-AMP | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ΣFIC | Activity a | ΣFIC | Activity | ΣFIC | Activity | ΣFIC | Activity | ΣFIC | Activity | ΣFIC | Activity | |
| S. aureus B1 | 0.562 | I | 0.516 | I | − | − | − | − | 2 | I | 0.516 | I |
| S. aureus B2 | 2 | I | 0.625 | I | − | − | − | − | 2 | I | 0.625 | I |
| E. faecalis W1 | − | − | − | − | 0.312 | S | − | − | 0.75 | I | − | − |
| E. faecium W5 | − | − | − | − | 0.312 | S | − | − | 0.75 | S | − | − |


3. Experimental Section
3.1. General Experimentation Procedures
3.2. Extraction and Isolation
3.2.1. Sartorypyrone C (5)
3.2.2. Isolation of Tryptoquivaline T (1d) from the Culture of Neosartorya laciniosa (KUFC 7896)
Tryptoquivaline T (1d)
3.2.3. Isolation of Chevalone B (6) and Chevalone C (7a) from the Culture of Neosartorya siamensis (KUFC 6349)
3.3. Antibacterial Activity Bioassays
3.3.1. Bacterial Strains
3.3.2. Determination of Minimum Inhibitory and Bactericidal Concentrations
3.3.3. Synergistic Studies
3.3.4. Antibiofilm Activity Assay
4. Conclusions
Supplementary Files
Acknowledgements
Conflicts of Interest
References
- Johnson, A.P.; Livermore, D.M.; Tillotson, G.S. Antimicrobial susceptibility of Gram-positive bacteria: What’s current, what’s anticipated? J. Hosp. Infect. 2001, 49, S3–S11. [Google Scholar] [CrossRef]
- Aksoy, D.Y.; Unal, S. New antimicrobial agents for treatment of Gram-positive bacterial infections. Clin. Microbiol. Infect. 2008, 14, 411–420. [Google Scholar] [CrossRef]
- Aziz, A.M. The role of healthcare strategies in controlling antibiotic resistance. Br. J. Nurs. 2013, 22, 1066–1074. [Google Scholar]
- Bassetti, M.; Merelli, M.; Temperoni, C.; Astilean, A. New antibiotics for bad bugs: Where are we? Ann. Clin. Microbiol. Antimicrob. 2013, 12. [Google Scholar] [CrossRef]
- Kijjoa, A.; Sawangwong, P. Drugs and Cosmetics from the Sea. Mar. Drugs 2004, 2, 73–82. [Google Scholar] [CrossRef]
- Newman, D.J.; Cragg, G.M. Natural Products as Sources of New Drugs over the 30 Years from 1981 to 2010. J. Nat. Prod. 2012, 75, 311–335. [Google Scholar] [CrossRef]
- Blunt, J.W.; Copp, B.R.; Keyzers, R.A.; Munro, M.H.G.; Prinsep, M.R. Marine natural products. Nat. Prod. Rep. 2013, 30, 237–323. [Google Scholar] [CrossRef]
- Rowley, D.C.; Kelly, S.; Kauffman, C.A.; Jensen, P.R.; Fenical, W. Halovirs A–E, new antiviral agents from a marine-derived fungus of the genus Scytalidium. Bioorg. Med. Chem. 2003, 11, 4263–4274. [Google Scholar] [CrossRef]
- Shen, S.; Li, W.; Ouyang, M.A.; Wu, Z.J.; Lin, Q.Y.; Xie, L.H. Identification of two marine fungi and evaluation of their antivirus and antitumor activities. Acta Microbiol. Sin. 2009, 49, 1240–1246. [Google Scholar]
- Bugni, T.S.; Ireland, C.M. Marine-derived fungi: A chemically and biologically diverse group of microorganisms. Nat. Prod. Rep. 2004, 21, 143–163. [Google Scholar] [CrossRef]
- Pejin, B.; Jovanović, K.K.; Mojović, M.; Savić, A.G. New and highly potent antitumor natural products from marine-derived fungi: Covering the period from 2003 to 2012. Curr. Top. Med. Chem. 2013, 13, 2745–2766. [Google Scholar] [CrossRef]
- Christophersen, C.; Crescente, C.; Frisvad, J.C.; Gram, L.; Nielsen, J.; Nielsen, P.H.; Rahbæk, L. Antibacterial activity of marine-derived fungi. Mycopathologia 1999, 143, 135–138. [Google Scholar]
- Arasu, M.V.; Duraipandiyan, V.; Ignacimuthu, S. Antibacterial and antifungal activities of polyketide metabolite from marine Streptomyces sp. AP-123 and its cytotoxic effect. Chemosphere 2013, 90, 479–487. [Google Scholar] [CrossRef]
- Manimegalai, K.; Devi, N.K.A.; Padmavathy, S. Marine fungi as a source of secondary metabolites of antibiotics. Int. J. Biotechnol. Bioeng. Res. 2013, 4, 275–282. [Google Scholar]
- Eamvijarn, A.; Gomes, N.M.; Dethoup, T.; Buaruang, J.; Manoch, L.; Silva, A.; Pedro, M.; Marini, I.; Roussis, V.; Kijjoa, A. Bioactive meroditerpenes and indole alkaloids from the soil fungus Neosartorya fischeri (KUFC 6344), and the marine-derived fungi Neosartorya laciniosa (KUFC 7896) and Neosartorya tsunodae (KUFC 9213). Tetrahedron 2013, 69, 8583–8591. [Google Scholar]
- Buttachon, S.; Chandrapatya, A.; Manoch, L.; Silva, A.; Gales, L.; Bruyére, C.; Kiss, R.; Kijjoa, A. Sartorymensin, a new indole alkaloid, and new analogues of tryptoquivaline and fiscalins produced by Neosartorya siamensis (KUFC 6349). Tetrahedron 2012, 68, 3253–3262. [Google Scholar] [CrossRef]
- Mahato, S.B.; Kundu, A.P. 13C NMR spectra of pentacyclic triterpenoids—a compilation and some salient feature. Phytochemistry 1994, 37, 1517–1575. [Google Scholar] [CrossRef]
- Hoffman, L.R.; D’Argenio, D.A.; MacCoss, M.J.; Zhang, Z.; Jones, R.A.; Miller, S.I. Aminoglycoside antibiotics induce bacterial biofilm formation. Nature 2005, 436, 1171–1175. [Google Scholar] [CrossRef]
- Kaplan, J.B.; Jabbouri, S.; Sadovskaya, I. Extracellular DNA-dependent biofilm formation by Staphylococcus epidermidis RP62A in response to subminimal inhibitory concentrations of antibiotics. Res. Microbiol. 2011, 162, 535–541. [Google Scholar] [CrossRef]
- Bessa, L.J.; Grande, R.; Di Iorio, D.; Di Giulio, M.; Di Campli, E.; Cellini, L. Helicobacter pylori free-living and biofilm modes of growth: Behavior in response to different culture media. APMIS 2013, 121, 549–560. [Google Scholar] [CrossRef]
- Glass, N.L.; Donaldson, G.C. Development of primer sets designed for use with the PCR to amplify conserved genes from filamentous ascomycetes. Appl. Environ. Microbiol. 1995, 61, 1323–1330. [Google Scholar]
- Kulkarni, S.S.; Singh, S.; Shah, J.R.; Low, W. K.; Talele, T.T. Synthesis and SAR optimization of quinazolin-4(3H)-ones as poly(ADP-ribose)polymerase-1 inhibitors. Eur. J. Med. Chem. 2012, 50, 264–273. [Google Scholar]
- Franklin, R.; Cockerill, M.D., III. Performance Standards for Antimicrobial Susceptibility Testing, Twenty-First Informational Supplement M100-S21; Clinical and Laboratory Standards Institute (CLSI): Wayne, PA, USA, 2011. [Google Scholar]
- Odds, F.C. Synergy, antagonism, and what the chequerboard puts between them. J. Antimicrob. Chemother. 2003, 52. [Google Scholar] [CrossRef]
- Johnson, S.A.; Goddard, P.A.; Iliffe, C.; Timmins, B.; Rickard, A.H.; Robson, G.; Handley, P.S. Comparative susceptibility of resident and transient hand bacteria to para-chloro-meta-xylenol and triclosan. J. Appl. Microbiol. 2002, 93, 336–344. [Google Scholar] [CrossRef]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Gomes, N.M.; Bessa, L.J.; Buttachon, S.; Costa, P.M.; Buaruang, J.; Dethoup, T.; Silva, A.M.S.; Kijjoa, A. Antibacterial and Antibiofilm Activities of Tryptoquivalines and Meroditerpenes Isolated from the Marine-Derived Fungi Neosartorya paulistensis, N. laciniosa, N. tsunodae, and the Soil Fungi N. fischeri and N. siamensis. Mar. Drugs 2014, 12, 822-839. https://doi.org/10.3390/md12020822
Gomes NM, Bessa LJ, Buttachon S, Costa PM, Buaruang J, Dethoup T, Silva AMS, Kijjoa A. Antibacterial and Antibiofilm Activities of Tryptoquivalines and Meroditerpenes Isolated from the Marine-Derived Fungi Neosartorya paulistensis, N. laciniosa, N. tsunodae, and the Soil Fungi N. fischeri and N. siamensis. Marine Drugs. 2014; 12(2):822-839. https://doi.org/10.3390/md12020822
Chicago/Turabian StyleGomes, Nelson M., Lucinda J. Bessa, Suradet Buttachon, Paulo M. Costa, Jamrearn Buaruang, Tida Dethoup, Artur M. S. Silva, and Anake Kijjoa. 2014. "Antibacterial and Antibiofilm Activities of Tryptoquivalines and Meroditerpenes Isolated from the Marine-Derived Fungi Neosartorya paulistensis, N. laciniosa, N. tsunodae, and the Soil Fungi N. fischeri and N. siamensis" Marine Drugs 12, no. 2: 822-839. https://doi.org/10.3390/md12020822
APA StyleGomes, N. M., Bessa, L. J., Buttachon, S., Costa, P. M., Buaruang, J., Dethoup, T., Silva, A. M. S., & Kijjoa, A. (2014). Antibacterial and Antibiofilm Activities of Tryptoquivalines and Meroditerpenes Isolated from the Marine-Derived Fungi Neosartorya paulistensis, N. laciniosa, N. tsunodae, and the Soil Fungi N. fischeri and N. siamensis. Marine Drugs, 12(2), 822-839. https://doi.org/10.3390/md12020822