Aeroallergen IgE-Reactivity Patterns and Respiratory Allergy in Children and Adults: A Retrospective Study in 1711 Patients from the Central Poland Urban Area
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Location
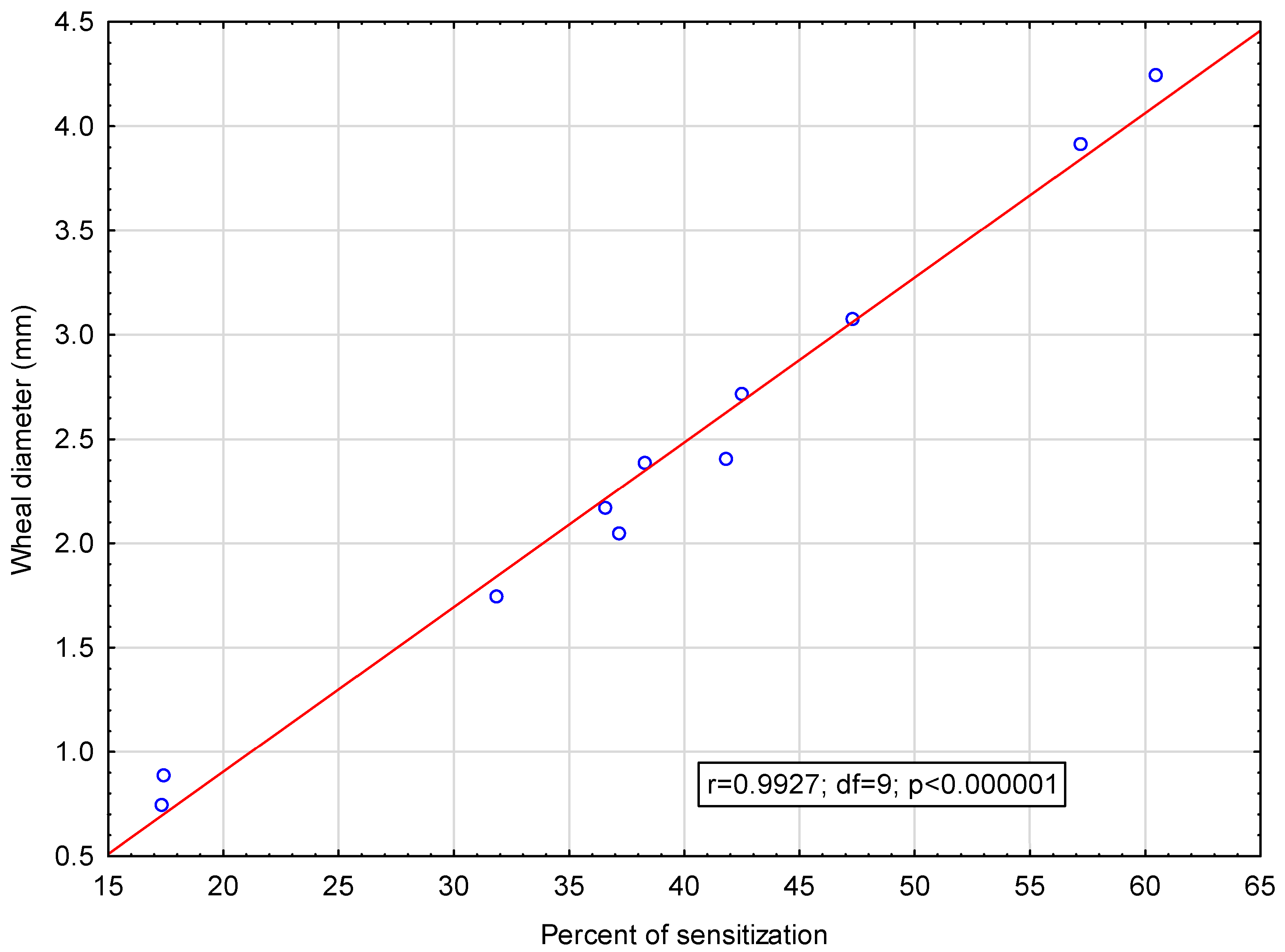
2.2. Skin Prick Tests
2.3. Statistical Methods
3. Results
3.1. Distribution of Sex and Age Groups
3.2. Reactivity Profiles in the Entire Study Group
3.3. Monovalent and Polyvalent Reactivity
3.3.1. Monovalent Reactivity Profiles
3.3.2. Polyvalent Reactivity Profiles
3.4. Factor Analysis
- Factor I was associated with positive SPT results to tree pollen extracts (alder, hazel, birch).
- Factor II characterized allergy to mites (Dermatophagoides pteronyssinus and Dermatophagoides farinae).
- Factor III was associated with allergies to grass pollen extracts: mix and rye.
- Factor IV determined allergies to animal allergens: dog and cat.
3.4.1. Testing of the Four Extracted Factors in Relation to Age, Sex and the Extracted Age Categories
Factor I—Allergy to Tree Pollen
Factor II—Allergy to House Dust Mites
Factor III—Allergy to Grass and Rye Pollen
Factor IV—Allergy to Pet Allergens
3.5. Frequency of Clinical Diagnoses According to the ICD-10 Classification
3.6. Clinical Diagnoses in Relation to SPT Results
3.6.1. Allergic Rhinitis (AR)
3.6.2. Asthma
3.6.3. Other Atopic Conditions
4. Discussion
4.1. Monovalent Reactivity
4.2. Reactivity and Age
4.3. Atopy and Sex
4.4. SPT Results and Allergic Diseases
5. Conclusions
- According to the results of SPTs, the most important sensitizing allergens in allergic subjects in central Poland were the pollen from grass (60.5%), rye (57.22%) and birch (47.34%).
- The most common monovalent reactivity found was that to mugwort pollen.
- The frequency of one or more positive SPT results was higher among males.
- The age distribution shows the highest reactivity of allergies in the age group 10–50 years, with male predominance
- In patients with clinically diagnosed AR, the probability of developing symptoms was higher in those sensitized to grass pollen, rye, alder, hazel, Alternaria, birch, cat, D. pteronyssinus and D. farinae allergens.
- Higher odds of developing asthma were associated with positive SPT results with dog, cat and dust mite allergens.
- Higher odds of developing atopic dermatitis were associated with positive SPT results with birch and alder pollen allergens.
- Higher odds of developing allergic conjunctivitis were associated with positive SPT results with alder, hazel and birch pollen allergens.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SPT | Skin prick test |
| AR | Allergic rhinitis |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems, Tenth Revision |
| NADPH | Nicotinamide Adenine Dinucleotide Phosphate |
| OR | Odds ratio |
| CI | Confidence interval |
| IL | Interleukin |
| HDM | House dust mite(s) |
| FeNO | Fractional exhaled nitric oxide |
| FEV1 | Forced expiratory volume in one second |
| FVC | Forced vital capacity |
References
- Rezwan, T.; Perez, M.; Jacobs, S.; Shafik, J.; Mitchell, W.B.; Conrad, L.A.; Soshnick, S.H. Correlation between Total IgE Level and Asthma Symptom Severity in Hospitalized Children. J. Allergy Clin. Immunol. Glob. 2025, 4, 100452. [Google Scholar] [CrossRef]
- Scelo, G.; Torres-Duque, C.A.; Maspero, J.; Tran, T.N.; Murray, R.; Martin, N.; Menzies-Gow, A.N.; Hew, M.; Peters, M.J.; Gibson, P.G.; et al. Analysis of Comorbidities and Multimorbidity in Adult Patients in the International Severe Asthma Registry. Ann. Allergy Asthma Immunol. 2024, 132, 42–53. [Google Scholar] [CrossRef]
- Wang, H.; Li, X.-B.; Chu, X.-J.; Cao, N.-W.; Wu, H.; Huang, R.-G.; Li, B.-Z.; Ye, D.-Q. Ambient Air Pollutants Increase the Risk of Immunoglobulin E–Mediated Allergic Diseases: A Systematic Review and Meta-Analysis. Environ. Sci. Pollut. Res. 2022, 29, 49534–49552. [Google Scholar] [CrossRef]
- Guo, Y.; Cai, S.; Deng, J.; Li, J.; Qiu, L.; Sun, Q.; Cui, Y.; Li, L.; Yu, L.; Yin, H.; et al. Trends and Hotspots of Acupuncture for Allergic Rhinitis: A Bibliometric Analysis from 2002 to 2022. Complement. Ther. Med. 2023, 78, 102984. [Google Scholar] [CrossRef]
- Cingi, C.; Gevaert, P.; Mösges, R.; Rondon, C.; Hox, V.; Rudenko, M.; Muluk, N.B.; Scadding, G.; Manole, F.; Hupin, C.; et al. Multi-Morbidities of Allergic Rhinitis in Adults: European Academy of Allergy and Clinical Immunology Task Force Report. Clin. Transl. Allergy 2017, 7, 17. [Google Scholar] [CrossRef]
- Seys, S.F.; Quirce, S.; Agache, I.; Akdis, C.A.; Alvaro-Lozano, M.; Antolín-Amérigo, D.; Bjermer, L.; Bobolea, I.; Bonini, M.; Bossios, A.; et al. Severe Asthma: Entering an Era of New Concepts and Emerging Therapies: Highlights of the 4th International Severe Asthma Forum, Madrid, 2018. Allergy 2019, 74, 2244–2248. [Google Scholar] [CrossRef] [PubMed]
- Mortada, M.M.; Kurowski, M. Challenges in Local Allergic Rhinitis Diagnosis, Management, and Research: Current Concepts and Future Perspectives. Medicina 2023, 59, 929. [Google Scholar] [CrossRef]
- Krzych-Fałta, E.; Wojas, O. Local Allergic Rhinitis or Local Allergic Conjunctivitis? Alergol. Pol. Pol. J. Allergol. 2023, 10, 310–314. [Google Scholar] [CrossRef]
- Berghi, O.; Dumitru, M.; Cergan, R.; Musat, G.; Serboiu, C.; Vrinceanu, D. Local Allergic Rhinitis—A Challenge for Allergology and Otorhinolaryngology Cooperation (Scoping Review). Life 2024, 14, 965. [Google Scholar] [CrossRef] [PubMed]
- Testera-Montes, A.; Jurado, R.; Salas, M.; Eguiluz-Gracia, I.; Mayorga, C. Diagnostic Tools in Allergic Rhinitis. Front. Allergy 2021, 2, 721851. [Google Scholar] [CrossRef]
- Riggioni, C.; Ricci, C.; Moya, B.; Wong, D.; Van Goor, E.; Bartha, I.; Buyuktiryaki, B.; Giovannini, M.; Jayasinghe, S.; Jaumdally, H.; et al. Systematic Review and Meta-analyses on the Accuracy of Diagnostic Tests for IgE-mediated Food Allergy. Allergy 2024, 79, 324–352. [Google Scholar] [CrossRef]
- García-Marcos, L.; Asher, M.I.; Pearce, N.; Ellwood, E.; Bissell, K.; Chiang, C.-Y.; El Sony, A.; Ellwood, P.; Marks, G.B.; Mortimer, K.; et al. The Burden of Asthma, Hay Fever and Eczema in Children in 25 Countries: GAN Phase I Study. Eur. Respir. J. 2022, 60, 2102866. [Google Scholar] [CrossRef] [PubMed]
- Romano, M.R.; James, S.; Farrington, E.; Perry, R.; Elliott, L. The Impact of Perennial Allergic Rhinitis with/without Allergic Asthma on Sleep, Work and Activity Level. Allergy Asthma Clin. Immunol. 2019, 15, 81. [Google Scholar] [CrossRef]
- Krzych-Fałta, E.; Wojas, O.; Raciborski, F.; Furmańczyk, K.; Chrzanowska, M.; Samoliński, B.; Lipiec, A.; Piekarska, B.; Gujski, M. Specificity and Sensitivity of Questionnaires in the Diagnosis of Allergic Diseases. Adv. Dermatol. Allergol. 2024, 41, 594–603. [Google Scholar] [CrossRef]
- Majkowska-Wojciechowska, B.; Pełka, J.; Korzon, L.; Kozłowska, A.; Kaczała, M.; Jarzebska, M.; Gwardys, T.; Kowalski, M.L. Prevalence of Allergy, Patterns of Allergic Sensitization and Allergy Risk Factors in Rural and Urban Children. Allergy 2007, 62, 1044–1050. [Google Scholar] [CrossRef] [PubMed]
- Pereira, R.N.; Rodrigues, R.M.; Madalena, D.A.; Vicente, A. Tackling Food Allergens—The Role of Food Processing on Proteins’ Allergenicity. In Advances in Food and Nutrition Research; Elsevier: Amsterdam, The Netherlands, 2023; Volume 106, pp. 317–351. ISBN 978-0-443-19304-0. [Google Scholar]
- Aldakheel, F.M. Allergic Diseases: A Comprehensive Review on Risk Factors, Immunological Mechanisms, Link with COVID-19, Potential Treatments, and Role of Allergen Bioinformatics. Int. J. Environ. Res. Public Health 2021, 18, 12105. [Google Scholar] [CrossRef] [PubMed]
- Finn, P.W.; Perkins, D.L. Born to Wheeze or Learned When We Were Young: Maternal and Environmental Factors Influence Atopic Risk. Trans. Am. Clin. Climatol. Assoc. 2023, 133, 181–192. [Google Scholar]
- Fujimura, K.E.; Sitarik, A.R.; Havstad, S.; Lin, D.L.; Levan, S.; Fadrosh, D.; Panzer, A.R.; LaMere, B.; Rackaityte, E.; Lukacs, N.W.; et al. Neonatal Gut Microbiota Associates with Childhood Multisensitized Atopy and T Cell Differentiation. Nat. Med. 2016, 22, 1187–1191. [Google Scholar] [CrossRef]
- Wang, H.; Jiang, X.; Zhang, P.; Li, Y.; Wang, Y.; Li, X. Allergen-Specific IgE in the Tear Fluid of Chinese Patients with Common Allergic Conjunctivitis in Autumn and Winter. Int. Ophthalmol. 2023, 43, 4541–4549. [Google Scholar] [CrossRef]
- Satnarine, T.; Makkoukdji, N.; Pundit, V.; Vignau, A.; Sharma, P.; Warren, D.; Kleiner, G.; Gans, M. Peanut Allergy Diagnosis: Current Practices, Emerging Technologies, and Future Directions. Allergies 2025, 5, 4. [Google Scholar] [CrossRef]
- Haidar, L.; Bănărescu, C.F.; Uța, C.; Moldovan, S.I.; Zimbru, E.-L.; Zimbru, R.-I.; Ciurariu, E.; Georgescu, M.; Panaitescu, C. Pollen–Food Allergy Syndrome: Allergens, Clinical Insights, Diagnostic and Therapeutic Challenges. Appl. Sci. 2024, 15, 66. [Google Scholar] [CrossRef]
- Gawryjołek, J.; Krogulska, A. Diagnostics of Peanut Allergy—Part I. Alergol. Pol. Pol. J. Allergol. 2022, 9, 160–169. [Google Scholar] [CrossRef]
- Krupka Olek, M.; Bożek, A.; Foks Ciekalska, A.; Grzanka, A.; Kawczyk-Krupka, A. Assessment of Hypersensitivity to House Dust Mites in Selected Skin Diseases Using the Basophil Activation Test: A Preliminary Study. Medicina 2024, 60, 1608. [Google Scholar] [CrossRef] [PubMed]
- Izmailovich, M.; Semenova, Y.; Abdushukurova, G.; Mukhamejanova, A.; Dyussupova, A.; Faizova, R.; Gazaliyeva, M.; Akhvlediani, L.; Glushkova, N.; Kalmakhanov, S.; et al. Molecular Aspects of Allergen-Specific Immunotherapy in Patients with Seasonal Allergic Rhinitis. Cells 2023, 12, 383. [Google Scholar] [CrossRef] [PubMed]
- Połomska, J.; Dydak, P.; Sozańska, B.; Sikorska-Szaflik, H. Peanut Allergy and Component-Resolved Diagnostics Possibilities—What Are the Benefits? Nutrients 2023, 15, 5132. [Google Scholar] [CrossRef] [PubMed]
- Wąsik, J.; Likońska, A.; Kurowski, M. IgE-Mediated Allergy and Asymptomatic Sensitization to Cannabis Allergens—Review of Current Knowledge and Presentation of Six Cases. Medicina 2024, 60, 954. [Google Scholar] [CrossRef]
- Jankowski, W.; Przychodniak, D.; Kurowski, M. LTP Syndrome and Edible Insect Allergy in a Patient with Recurrent Anaphylaxis Incidents. Alergol. Pol. Pol. J. Allergol. 2024, 12, 138–139. [Google Scholar] [CrossRef]
- Zhang, J.; Tang, Y.; Yang, D.; Yu, J. Investigating Allergen-Specific IgE Distribution and Correlations in Chronic Urticaria: A Retrospective Study in Shanghai, China. Eur. J. Med. Res. 2025, 30, 182. [Google Scholar] [CrossRef]
- Liu, M.; Liu, L.; Qi, W.; Zheng, X.; Chen, J.; Yao, J.; Li, Y.; Lin, J.; Li, X.; Hu, X.; et al. Interpreting Epidemiologic Distribution of Total and Specific IgE Levels for Food Allergy in Southern China from 2004 to 2023: Understanding the Mechanisms and Focusing on Prevention. BMC Public Health 2024, 24, 3022. [Google Scholar] [CrossRef]
- Wang, J.; Xu, B.; Jia, X.; He, Y.; Jia, B.; Li, J.; Xu, M. Predictive Value of Der p 2-Specific IgE for Subcutaneous Immunotherapy in Children with Allergic Rhinitis. Sci. Rep. 2024, 14, 25467. [Google Scholar] [CrossRef]
- Łódź Raport o Stanie Miasta. BS_p25_120_20250530. PDF. Available online: https://bip.uml.lodz.pl/ (accessed on 7 September 2025).
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems 10th Revision 2019. World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- Bousquet, J.; Heinzerling, L.; Bachert, C.; Papadopoulos, N.G.; Bousquet, P.J.; Burney, P.G.; Canonica, G.W.; Carlsen, K.H.; Cox, L.; Haahtela, T.; et al. Practical Guide to Skin Prick Tests in Allergy to Aeroallergens. Allergy 2012, 67, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Wallace, D.V.; Bahna, S.L.; Goldstein, S.; Hamilton, R.G.; Cohn, J.R. American Academy of Allergy, Asthma & Immunology Work Group Report: Allergy Diagnosis in Clinical Practice. J. Allergy Clin. Immunol. 2007, 120, 967–969. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kowalski, M.L.; Ansotegui, I.; Aberer, W.; Al-Ahmad, M.; Akdis, M.; Ballmer-Weber, B.K.; Beyer, K.; Blanca, M.; Brown, S.; Bunnag, C.; et al. Risk and Safety Requirements for Diagnostic and Therapeutic Procedures in Allergology: World Allergy Organization Statement. World Allergy Organ. J. 2016, 9, 33. [Google Scholar] [CrossRef] [PubMed]
- Szmyd, B.; Biedrzycka, M.; Rogut, M.; Daszkiewicz, G.; Hałucha, J.; Kaszkowiak, M.; Kowalski, M.L.; Kurowski, M. Assessment of Skin Prick Tests and sIgE Measurement Performance in the Diagnosis of Food and Inhalat Allergy. Alerg. Astma Immunol. 2020, 25, 104–110. (In Polish) [Google Scholar]
- Ansotegui, I.J.; Melioli, G.; Canonica, G.W.; Caraballo, L.; Villa, E.; Ebisawa, M.; Passalacqua, G.; Savi, E.; Ebo, D.; Gómez, R.M.; et al. IgE Allergy Diagnostics and Other Relevant Tests in Allergy, a World Allergy Organization Position Paper. World Allergy Organ. J. 2020, 13, 100080. [Google Scholar] [CrossRef]
- Czarnobilska, E.; Klimaszewska-Rembiasz, M.; Gaweł, B.; Obtułowicz, A. Prevalence of Allergic Diseases in Primary School Children in Cracow and Surroundings—An Attempt to Define Main Risk Factors. Przegląd Lekarski 2002, 59, 422–426. (In Polish) [Google Scholar]
- Wojciechowska, M.; Hnatyszyn-Dzikowska, A.; Bartuzi, Z. Sensitization to Haptens, Inhalant and Food Allergensamong Patients Diagnosed for Contact Allergy. Alerg. Astma Immunol. 2016, 21, 110–120. (In Polish) [Google Scholar]
- Sybilski, A.J.; Raciborski, F.; Lipiec, A.; Tomaszewska, A.; Lusawa, A.; Samel-Kowalik, P.; Walkiewicz, A.; Krzych-Fałta, E.; Samoliński, B. Epidemiology of Atopic Dermatitis in Poland According to the Epidemiology of Allergic Disorders in Poland (ECAP) Study. J. Dermatol. 2015, 42, 140–147. [Google Scholar] [CrossRef]
- Antico, A.; Lima, G.; Arisi, M.; Ostan, A.; Morrica, B. Assay of Prick Test Inoculum Volume. II. Average Values and Individual Variability. Ann. Allergy Asthma Immunol. 2000, 85, 145–149. [Google Scholar] [CrossRef]
- Samoliński, B.; Raciborski, F.; Lipiec, A.; Tomaszewska, A.; Krzych-Fałta, E.; Samel-Kowalik, P.; Walkiewicz, A.; Lusawa, A.; Borowicz, J.; Komorowski, J.; et al. Epidemiology of allergic diseases in Poland. Alergol. Pol. Pol. J. Allergol. 2014, 1, 10–18. (In Polish) [Google Scholar] [CrossRef]
- Worm, M.; Lee, H.; Kostev, K. Prevalence and Treatment Profile of Patients with Grass Pollen and House Dust Mite Allergy. JDDG J. Dtsch. Dermatol. Ges. 2013, 11, 653–661. [Google Scholar] [CrossRef] [PubMed]
- García-Mozo, H. Poaceae Pollen as the Leading Aeroallergen Worldwide: A Review. Allergy 2017, 72, 1849–1858. [Google Scholar] [CrossRef]
- Dramburg, S.; Hilger, C.; Santos, A.F.; de Las Vecillas, L.; Aalberse, R.C.; Acevedo, N.; Aglas, L.; Altmann, F.; Arruda, K.L.; Asero, R.; et al. EAACI Molecular Allergology User’s Guide 2.0. Pediatr. Allergy Immunol. 2023, 34 (Suppl. 28), e13854. [Google Scholar] [CrossRef] [PubMed]
- Abou Chakra, O.R.; Sutra, J.-P.; Poncet, P.; Lacroix, G.; Sénéchal, H. Key Role of Water-Insoluble Allergens of Pollen Cytoplasmic Granules in Biased Allergic Response in a Rat Model. World Allergy Organ. J. 2011, 4, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Dharajiya, N.; Boldogh, I.; Cardenas, V.; Sur, S. Role of Pollen NAD(P)H Oxidase in Allergic Inflammation. Curr. Opin. Allergy Clin. Immunol. 2008, 8, 57–62. [Google Scholar] [CrossRef]
- Wang, X.-L.; Takai, T.; Kamijo, S.; Gunawan, H.; Ogawa, H.; Okumura, K. NADPH Oxidase Activity in Allergenic Pollen Grains of Different Plant Species. Biochem. Biophys. Res. Commun. 2009, 387, 430–434. [Google Scholar] [CrossRef]
- Visez, N.; De Nadaï, P.; Choël, M.; Farah, J.; Hamzé, M.; Sénéchal, H.; Pauwels, M.; Frérot, H.; Thibaudon, M.; Poncet, P. Biochemical Composition of Phleum Pratense Pollen Grains: A Review. Mol. Immunol. 2021, 136, 98–109. [Google Scholar] [CrossRef]
- Raith, M.; Swoboda, I. Birch Pollen—The Unpleasant Herald of Spring. Front. Allergy 2023, 4, 1181675. [Google Scholar] [CrossRef]
- Darnhofer, B.; Tomin, T.; Liesinger, L.; Schittmayer, M.; Tomazic, P.V.; Birner-Gruenberger, R. Comparative Proteomics of Common Allergenic Tree Pollens of Birch, Alder, and Hazel. Allergy 2021, 76, 1743–1753. [Google Scholar] [CrossRef]
- Rapiejko, J.; Puc, M.; Piotrowska-Weryszko, K.; Myszkowska, D.; Chodkowski, J.; Malkiewicz, M.; Jurkiewicz, D.; Siergiejko, G.; Chłopek, K.; Lipiec, A. Analysis of Artemisia Pollen Season in Selected Cities of Poland in 2022. Alergoprofil 2023, 19, 13–19. [Google Scholar] [CrossRef]
- Majkowska–Wojciechowska, B.; Balwierz, Z.; Kowalski, M. Pollen Counts Analysis in the Atmosphere of Lodz (Poland) during Vegetation in 2008. Alerg. Astma Immunol. 2008, 13, 250–263. [Google Scholar]
- Majkowska-Wojciechowska, B.; Balwierz, Z.; Kowalski, M.L. Changes in the Concentration of Pollen over an 11-Year Period in a Polish Urban Environment. Acta Agrobot. 2016, 69, 1–11. [Google Scholar] [CrossRef][Green Version]
- Majkowska-Wojciechowska, B.; Balwierz, Z.; Kowalski, M. Pollen and Spores of Microscopic Fungi in Atmospheric Air Lodz in 2013. Alerg. Astma Immunol. 2015, 20, 192–198. (In Polish) [Google Scholar][Green Version]
- Ma, T.; Wang, H.; Chen, Y.; Zhuang, Y.; Shi, H.; Yu, R.; Guo, M.; Yin, J.; Wang, X. Sensitization Spectrum of Inhaled Allergens in Outpatients in Beijing Area. Chin. J. Allergy Clin Immunol. 2021, 15, 136–143. (In Chinese) [Google Scholar][Green Version]
- Yu, Y.; Yan, X.; Wang, L.; Dong, L.; Song, D.; Liu, J.; Gao, X. Investigation and Analysis of Inhalant Allergens in Patients with Allergic Rhinitis in Yinchuan, China. Int. Arch. Allergy Immunol. 2024, 186, 445–453. [Google Scholar] [CrossRef]
- Wang, M.; Ma, J.; Yang, Z.; Wang, W.; Sa, Y.; Ma, F.; Zhang, W.; He, X.; Chen, G.; Ma, X. Immunoproteomic Analysis and Identification of Possible Allergenic Proteins in Artemisia Annua Pollen. Int. Immunopharmacol. 2025, 146, 113837. [Google Scholar] [CrossRef]
- Asero, R. Is the Strange Case of Mugwort Sensitivity in Ragweed-Allergic Subjects Coming Eventually to a Solution? Eur. Ann. Allergy Clin. Immunol. 2011, 43, 67–68. [Google Scholar]
- Pablos, I.; Eichhorn, S.; Machado, Y.; Briza, P.; Neunkirchner, A.; Jahn-Schmid, B.; Wildner, S.; Soh, W.T.; Ebner, C.; Park, J.-W.; et al. Distinct Epitope Structures of Defensin-like Proteins Linked to Proline-rich Regions Give Rise to Differences in Their Allergenic Activity. Allergy 2018, 73, 431–441. [Google Scholar] [CrossRef]
- Stępalska, D.; Myszkowska, D.; Piotrowicz, K.; Kluska, K.; Chłopek, K.; Grewling, Ł.; Lafférsová, J.; Majkowska-Wojciechowska, B.; Malkiewicz, M.; Piotrowska-Weryszko, K.; et al. High Ambrosia Pollen Concentrations in Poland Respecting the Long Distance Transport (LDT). Sci. Total Environ. 2020, 736, 139615. [Google Scholar] [CrossRef]
- Bergmann, K.-C. Biology of House Dust Mites and Storage Mites. Allergo J. Int. 2022, 31, 272–278. [Google Scholar] [CrossRef]
- Solarz, K. Risk of Exposure to House Dust Pyroglyphid Mites in Poland. Ann. Agric. Environ. Med. AAEM 2001, 8, 11–24. [Google Scholar]
- Lee, K.-A.; Flores, R.R.; Jang, I.H.; Saathoff, A.; Robbins, P.D. Immune Senescence, Immunosenescence and Aging. Front. Aging 2022, 3, 900028. [Google Scholar] [CrossRef]
- Ventura, M.T.; Scichilone, N.; Paganelli, R.; Minciullo, P.L.; Patella, V.; Bonini, M.; Passalacqua, G.; Lombardi, C.; Simioni, L.; Ridolo, E.; et al. Allergic Diseases in the Elderly: Biological Characteristics and Main Immunological and Non-Immunological Mechanisms. Clin. Mol. Allergy 2017, 15, 2. [Google Scholar] [CrossRef] [PubMed]
- Warren, K.J.; Deering-Rice, C.; Huecksteadt, T.; Trivedi, S.; Venosa, A.; Reilly, C.; Sanders, K.; Clayton, F.; Wyatt, T.A.; Poole, J.A.; et al. Steady-State Estradiol Triggers a Unique Innate Immune Response to Allergen Resulting in Increased Airway Resistance. Biol. Sex Differ. 2023, 14, 2. [Google Scholar] [CrossRef] [PubMed]
- Harvey, B.J.; McElvaney, N.G. Sex Differences in Airway Disease: Estrogen and Airway Surface Liquid Dynamics. Biol. Sex Differ. 2024, 15, 56. [Google Scholar] [CrossRef] [PubMed]
- Cephus, J.-Y.; Stier, M.T.; Fuseini, H.; Yung, J.A.; Toki, S.; Bloodworth, M.H.; Zhou, W.; Goleniewska, K.; Zhang, J.; Garon, S.L.; et al. Testosterone Attenuates Group 2 Innate Lymphoid Cell-Mediated Airway Inflammation. Cell Rep. 2017, 21, 2487–2499. [Google Scholar] [CrossRef]
- Han, Y.-Y.; Yan, Q.; Yang, G.; Chen, W.; Forno, E.; Celedon, J.C. Serum Free Testosterone and Asthma, Asthma Hospitalisations and Lung Function in British Adults. Thorax 2020, 75, 849–854. [Google Scholar] [CrossRef]
- Trivedi, S.; Deering-Rice, C.E.; Aamodt, S.E.; Huecksteadt, T.P.; Myers, E.J.; Sanders, K.A.; Paine, R.; Warren, K.J. Progesterone Amplifies Allergic Inflammation and Airway Pathology in Association with Higher Lung ILC2 Responses. Am. J. Physiol.-Lung Cell. Mol. Physiol. 2024, 327, L65–L78. [Google Scholar] [CrossRef]
- Dou, X.; Zhang, W.; Zhang, X. Exploring the Immunological Underpinnings of Allergic Conjunctivitis: The Role of CD4 + T Cells and SLAM Expression in Ocular Surface Disease. Int. Ophthalmol. 2025, 45, 77. [Google Scholar] [CrossRef]
- Rabensteiner, D.F.; Rabensteiner, J.; Horwath-Winter, J.; Lang-Loidolt, D.; Wedrich, A.; Heidinger, A.; Schwantzer, G.; Schmut, O. Extracts of Different Pollen Species and Their Effect on Human Tear Fluid and an Epithelial Cell Line. Cutan. Ocul. Toxicol. 2019, 38, 93–103. [Google Scholar] [CrossRef]
- Montoro, J.; Antolín-Amérigo, D.; Izquierdo-Domínguez, A.; Zapata, J.; García-Gallardo, M.; González, R.; Armentia, A.; Rondón, C.; Fernández, M.; Pedrero, S.; et al. Climate Change–Associated Environmental Factors and Pollutants: Impact on Allergic Diseases, Epidemiology, Severity, and Health Care Burden. J. Investig. Allergy Clin. Immunol. 2025, 35, 240–250. [Google Scholar] [CrossRef]
- Olivieri, M.; Marchetti, P.; Murgia, N.; Nicolis, M.; Torroni, L.; Spiteri, G.; Ferrari, M.; Marcon, A.; Verlato, G. Natural Pollen Exposure Increases in a Dose-dependent Way Fraction of Exhaled Nitric Oxide (FeNO) Levels in Patients Sensitized to One or More Pollen Species. Clin. Transl. Allergy 2022, 12, e12096. [Google Scholar] [CrossRef] [PubMed]
- Klangkalya, N.; Watcharoot, K.; Adithep, S.; Potjanee, K.; Wanlapa, J.; Wiparat, M. Skin Prick Test and Serum Specific IgE in Predicting Dust Mite-Induced Allergic Rhinitis Diagnosed from Nasal Provocation Test in Chronic Rhinitis Children. Asian Pac. J. Allergy Immunol. 2025, 42, 354–360. [Google Scholar] [CrossRef]
- Kurowski, M.; Majkowska-Wojciechowska, B.; Wardzyńska, A.; Kowalski, M.L. Associations of Allergic Sensitization and Clinical Phenotypes with Innate Immune Response Genes Polymorphisms Are Modified by House Dust Mite Allergen Exposure. Arch. Med. Sci. 2011, 6, 1029–1036. [Google Scholar] [CrossRef]
- Majkowska-Wojciechowska, B.; Laskowska, B.; Wojciechowski, Z.; Kowlaski, M. Występowanie Alergii Wśród Dzieci Łódzkich Szkół Podstawowych: Związek z Warunkami Środowiska Domowego i Szkolnego. Alerg. Astma Immunol. 2000, 5, 115–122. [Google Scholar]
- Góra, D.J.; Kupiec, J. Analysis of the Incidence of Asthma among Pupils of Primary Schools in Bielsko-Biala Located in Areas with Various Degrees of Industrialization. Alergol. Pol. Pol. J. Allergol. 2024, 11, 211–216. [Google Scholar] [CrossRef]
- Stelmach, I.; Smejda, K.; Kaczmarek, J.; Stelmach, W.; Kuna, P. Prevalence of Atopy and Atopic Diseases in Children Living in an Orphanage in Lodz Area Pilot Study. Pol. Merkur. Lekarski 2006, 20, 531–534. (In Polish) [Google Scholar]
- Stelmach, I.; Smejda, K.; Jerzynska, J.; Stelmach, W.; Majak, P.; Stelmach, P.; Kuna, P. Decreased Markers of Atopy in Children with Presumed Early Exposure to Allergens, Unhygienic Conditions, and Infections. Ann. Allergy Asthma Immunol. 2007, 99, 170–177. [Google Scholar] [CrossRef]





| Group I <10 years | Group II ≥10–50 years | Group III >50 years | |
|---|---|---|---|
| Number of subjects (n) | 190 | 1280 | 241 |
| Mean age ± SD | 6.87 ± 2.0 | 28.11 ± 11.06 | 60.02 ± 6.65 |
| Age range (years) | 2.57–9.99 | 10.04–49.96 | 50.28–86.42 |
| % of the total population | 11.1% | 74.81% | 14.09% |
| Number of Subjects with Monovalent Reactivity in a Given Group | Percentage of Subjects with Monovalent Reactivity in a Given Group | |
|---|---|---|
| Group I <10 years (n = 190) | 26 | 13.68% |
| Group II ≥10–50 years (n = 1280) | 140 | 10.94% |
| Group III >50 years (n = 241) | 69 | 28.63% |
| Total (n = 1711) | 235 | 13.73% |
| Variables | Factor Loadings Extraction Principal Components (PC). Marked Loadings > 0.7 | ||||
|---|---|---|---|---|---|
| PC1_Trees Pollen 1 | PC2_ House Dust Mites 2 | PC3_Grass Pollen 3 | PC4_Pets 4 | ||
| 1. | D. farinae | −0.010730 | 0.948330 | 0.014072 | 0.080939 |
| 2. | D. pteronyssinus | −0.013067 | 0.949340 | 0.044677 | 0.050046 |
| 3. | Alder | 0.935816 | 0.004489 | 0.190270 | 0.099719 |
| 4. | Hazel | 0.918262 | −0.010066 | 0.201667 | 0.092477 |
| 5. | Birch | 0.927786 | −0.014525 | 0.153930 | 0.102391 |
| 6. | Timothy | 0.142750 | −0.020950 | 0.929728 | 0.084068 |
| 7. | Rye | 0.114222 | −0.013704 | 0.935631 | 0.101022 |
| 8. | Mugwort | 0.192302 | 0.069246 | 0.371463 | 0.048909 |
| 9. | Dog | 0.142326 | 0.170201 | 0.021874 | 0.715538 |
| 10. | Cat | 0.235508 | 0.186921 | 0.080663 | 0.712500 |
| 11. | Alternaria | −0.087785 | −0.185442 | 0.122141 | 0.588676 |
| Explained variance | 2.733860 | 1.904627 | 2.002449 | 1.423891 | |
| Proportion of variance | 0.248533 | 0.173148 | 0.182041 | 0.129445 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majkowska-Wojciechowska, B.; Kulma, M.; Kurowski, M. Aeroallergen IgE-Reactivity Patterns and Respiratory Allergy in Children and Adults: A Retrospective Study in 1711 Patients from the Central Poland Urban Area. Medicina 2025, 61, 1676. https://doi.org/10.3390/medicina61091676
Majkowska-Wojciechowska B, Kulma M, Kurowski M. Aeroallergen IgE-Reactivity Patterns and Respiratory Allergy in Children and Adults: A Retrospective Study in 1711 Patients from the Central Poland Urban Area. Medicina. 2025; 61(9):1676. https://doi.org/10.3390/medicina61091676
Chicago/Turabian StyleMajkowska-Wojciechowska, Barbara, Maciej Kulma, and Marcin Kurowski. 2025. "Aeroallergen IgE-Reactivity Patterns and Respiratory Allergy in Children and Adults: A Retrospective Study in 1711 Patients from the Central Poland Urban Area" Medicina 61, no. 9: 1676. https://doi.org/10.3390/medicina61091676
APA StyleMajkowska-Wojciechowska, B., Kulma, M., & Kurowski, M. (2025). Aeroallergen IgE-Reactivity Patterns and Respiratory Allergy in Children and Adults: A Retrospective Study in 1711 Patients from the Central Poland Urban Area. Medicina, 61(9), 1676. https://doi.org/10.3390/medicina61091676







