How Does Turner Syndrome Affect Quality of Life? A Systematic Review
Abstract
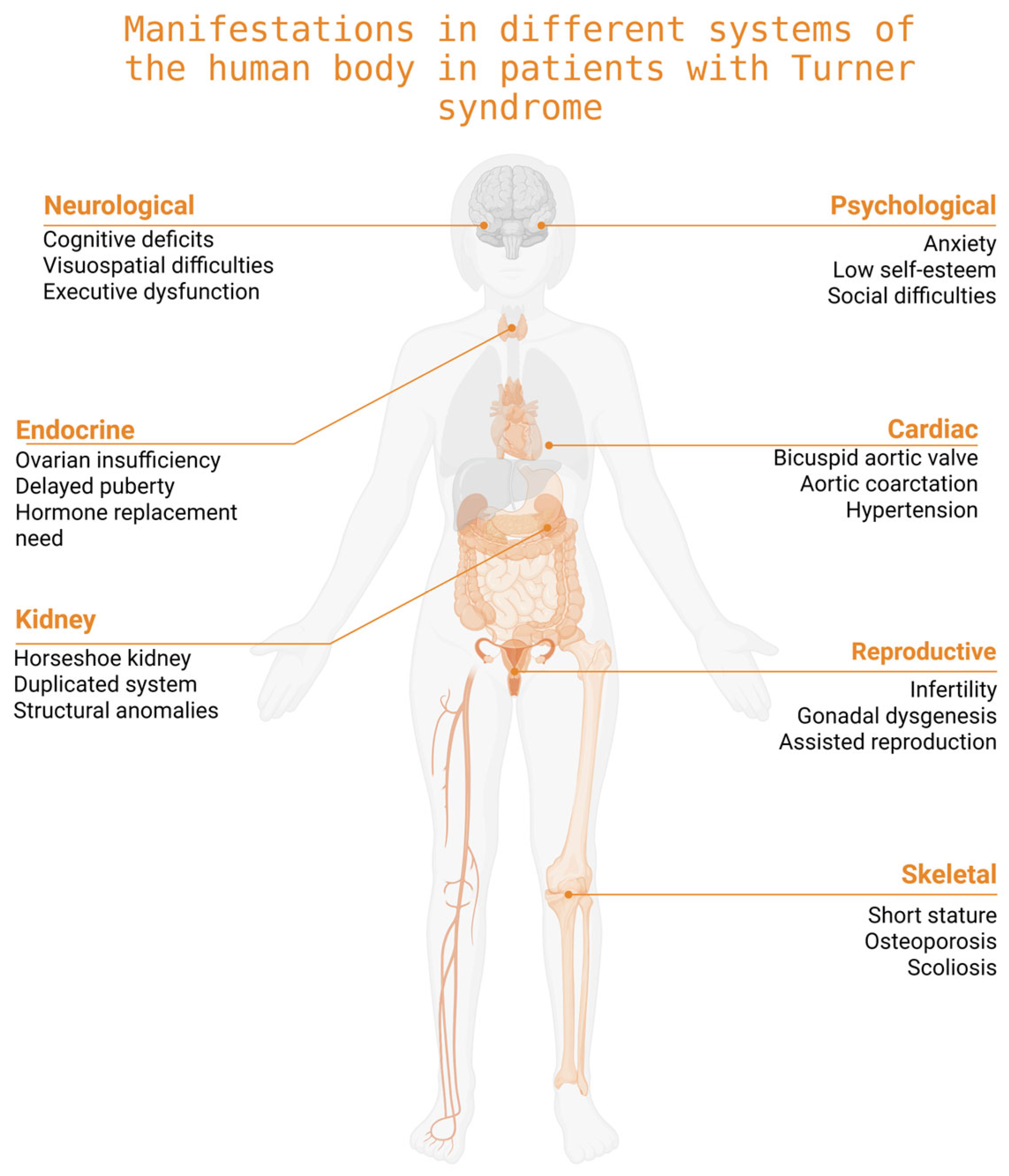
1. Introduction
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Data Synthesis
3. Results
3.1. Characteristics of Studies Included
3.2. Quality of Life in Children and Adolescents with Turner Syndrome
3.3. HRQoL in Adult Women with Turner Syndrome
3.4. Role of Growth Hormone Therapy and Estrogen Replacement
3.5. Comorbidities in Patients with Turner Syndrome
3.6. Measurement Tools Used Across Studies
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| TS | Turner Syndrome |
| QoL | Quality of Life |
| HRQoL | Health-Related Quality of Life |
| GH | Growth Hormone |
| HRT | Hormone Replacement Therapy |
| PROMIS | Patient-Reported Outcomes Measurement Information System |
| PedsQL™ | Pediatric Quality of Life Inventory |
| PGWB | Psychological General Well-Being Index |
| WHOQOL-BREF | World Health Organization Quality of Life–BREF |
| BIDQ | Body Image Disturbances Questionnaire |
| PSS-10 | Perceived Stress Scale (10-item version) |
| CIS-20 | Checklist Individual Strength (20-item version) |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
References
- Yoon, S.H.; Kim, G.Y.; Choi, G.T.; Do, J.T. Organ Abnormalities Caused by Turner Syndrome. Cells 2023, 12, 1365. [Google Scholar] [CrossRef] [PubMed]
- Clemente, E.G.; Penukonda, S.K.; Doan, T.; Sullivan, B.; Kanungo, S. Turner Syndrome. Endocrines 2022, 3, 240–254. [Google Scholar] [CrossRef]
- Porcu, E.; Cipriani, L.; Damiano, G. Reproductive Health in Turner’s Syndrome: From Puberty to Pregnancy. Front. Endocrinol. 2023, 14, 1269009. [Google Scholar] [CrossRef] [PubMed]
- Hutaff-Lee, C.; Bennett, E.; Howell, S.; Tartaglia, N. Clinical Developmental, Neuropsychological, and Social-Emotional Features of Turner Syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2019, 181, 126–134. [Google Scholar] [CrossRef]
- Donnelly, S.L.; Wolpert, C.M.; Menold, M.M.; Bass, M.P.; Gilbert, J.R.; Cuccaro, M.L.; Delong, G.R.; Pericak-Vance, M.A. Female with autistic disorder and monosomy X (Turner syndrome): Parent-of-origin effect of the X chromosome. Am. J. Med. Genet. 2000, 96, 312–316. [Google Scholar] [CrossRef]
- Gawlik, A.; Kaczor, B.; Kaminska, H.; Zachurzok-Buczynska, A.; Gawlik, T.; Malecka-Tendera, E. Quality of medical follow-up of young women with Turner syndrome treated in one clinical center. Horm. Res. Paediatr. 2012, 77, 222–228. [Google Scholar] [CrossRef]
- Wilson, I.B.; Cleary, P.D. Linking Clinical Variables with Health-Related Quality of Life. JAMA 1995, 273, 59–65. [Google Scholar] [CrossRef]
- Landry, B.W.; Ratterman, N.L.; Nielson, K.A.; Payne, J.B.; Ramsey, R.R. A Mixed Methods Study of Physical Activity and Quality of Life in Girls with Turner Syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2019, 181, 103–110. [Google Scholar] [CrossRef]
- Morgan, T. Turner Syndrome: Diagnosis and Management. Am. Fam. Physician 2007, 76, 405–410. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Thompson, T.; Zieba, B.; Howell, S.; Karakash, W.; Davis, S. A Mixed Methods Study of Physical Activity and Quality of Life in Adolescents with Turner Syndrome. Am. J. Med. Genet. A 2020, 182, 386–396. [Google Scholar] [CrossRef] [PubMed]
- Van den Hoven, A.T.; Bons, L.R.; Dykgraaf, R.H.M.; Dessens, A.B.; Pastoor, H.; de Graaff, L.C.G.; Metselaar, M.R.; Kneppers-Swets, A.; Kardys, I.; Mijnarends, H.; et al. A Value-Based Healthcare Approach: Health-Related Quality of Life and Psychosocial Functioning in Women with Turner Syndrome. Clin. Endocrinol. 2020, 92, 434–442. [Google Scholar] [CrossRef] [PubMed]
- Rovet, J.F.; Van Vliet, G. Growth Hormone Supplementation and Psychosocial Functioning to Adult Height in Turner Syndrome: A Questionnaire Study of Participants in the Canadian Randomized Trial. Front. Endocrinol. 2019, 10, 125. [Google Scholar] [CrossRef] [PubMed]
- Ertl, D.A.; Gleiss, A.; Schubert, K.; Culen, C.; Hauck, P.; Ott, J.; Gessl, A.; Haeusler, G. Health Status, Quality of Life and Medical Care in Adult Women with Turner Syndrome. Endocr. Connect. 2018, 7, 534–543. [Google Scholar] [CrossRef]
- Amedro, P.; Tahhan, N.; Bertet, H.; Jeandel, C.; Guillaumont, S.; Mura, T.; Picot, M.C. Health-Related Quality of Life among Children with Turner Syndrome: Controlled Cross-Sectional Study. J. Pediatr. Endocrinol. Metab. 2017, 30, 863–868. [Google Scholar] [CrossRef]
- Krantz, E.; Landin-Wilhelmsen, K.; Trimpou, P.; Bryman, I.; Wide, U. Health-Related Quality of Life in Turner Syndrome and the Influence of Growth Hormone Therapy: A 20-Year Follow-Up. J. Clin. Endocrinol. Metab. 2019, 104, 5073–5083. [Google Scholar] [CrossRef]
- Taback, S.P.; Van Vliet, G. Health-Related Quality of Life of Young Adults with Turner Syndrome Following a Long-Term Randomized Controlled Trial of Recombinant Human Growth Hormone. BMC Pediatr. 2011, 11, 49. [Google Scholar] [CrossRef]
- Boman, U.W.; Bryman, I.; Möller, A. Psychological Well-Being in Women with Turner Syndrome: Somatic and Social Correlates. J. Psychosom. Obstet. Gynaecol. 2004, 25, 211–219. [Google Scholar] [CrossRef]
- Karakök, B.; Akdemir, D.; Yalçın, S.; Özusta, H.S.; Utine, G.E.; Doğan, Ö.; Şimşek Kiper, P.O.; Demir, G.U. Psychometric and Psychosocial Evaluation of Adolescents with Turner Syndrome in a Multidisciplinary Approach: A Preliminary Study. J. Curr. Pediatr. 2021, 19, 363–372. [Google Scholar] [CrossRef]
- Jeż, W.; Tobiasz-Adamczyk, B.; Brzyski, P.; Majkowicz, M.; Pankiewicz, P.; Irzyniec, T.J. Social and Medical Determinants of Quality of Life and Life Satisfaction in Women with Turner Syndrome. Adv. Clin. Exp. Med. 2018, 27, 229–236. [Google Scholar] [CrossRef]
- Yusof, A.A.B.; Chii, M.L.S.; Yusoff, N.I.M.; Kama, R.N.I.F.R.M.; Raj, J.R.; Ghani, N.A.A.; Ali, A.; Hong Soo Syn, J.; Shah, S.A.; Ishak, N.A.; et al. The Quality of Life and Body Image Disturbances of Turner Syndrome Patients in Malaysia: A Cross-Sectional Study. BMC Women’s Health 2023, 23, 614. [Google Scholar] [CrossRef]
- Okada, Y. The Quality of Life of Turner Women in Comparison with Grown-Up GH-Deficient Women. Endocr. J. 1994, 41, 345–354. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Krzyścin, M.; Sowińska-Przepiera, E.; Gruca-Stryjak, K.; Soszka-Przepiera, E.; Syrenicz, I.; Przepiera, A.; Bumbulienė, Z.; Syrenicz, A. Are Young People with Turner Syndrome Who Have Undergone Treatment with Growth and Sex Hormones at Higher Risk of Metabolic Syndrome and Its Complications? Biomedicines 2024, 12, 1034. [Google Scholar] [CrossRef]
- Viuff, M.; Gravholt, C.H. Turner Syndrome and Fertility. Ann. Endocrinol. 2022, 83, 244–249. [Google Scholar] [CrossRef]
- Gravholt, C.H.; Andersen, N.H.; Christin-Maitre, S.; Davis, S.M.; Duijnhouwer, A.; Gawlik, A.; Maciel-Guerra, A.T.; Gutmark-Little, I.; Fleischer, K.; Hong, D.; et al. Clinical Practice Guidelines for the Care of Girls and Women with Turner Syndrome. Eur. J. Endocrinol. 2024, 190, G53–G151. [Google Scholar] [CrossRef]
- Kesler, S.R. Turner Syndrome. Child Adolesc. Psychiatr. Clin. N. Am. 2007, 16, 709–722. [Google Scholar] [CrossRef]

| Parameter | Description |
|---|---|
| Population | Individuals diagnosed with TS (any age group) |
| Intervention | Studies assessed QoL outcomes without examining the effect of a defined intervention. |
| Comparison | Studies with or without a control group (e.g., general population, other clinical conditions) |
| Outcome | Assessed QoL or HRQoL using quantitative or qualitative methods |
| Study Design | Cross-sectional studies, cohort studies, pre-post studies, interventional prospective studies, case–control studies, and other original research articles; reviews, editorials, and commentaries were excluded |
| Author, Year | Country | Study Design | Sample Size | Objective | Study Outcomes and Main Result |
|---|---|---|---|---|---|
| Thompson et al., 2020 [11] | USA | Mixed methods (cross-sectional + interviews) Qualitive + quantitative methods | n = 21 adolescent girls with TS and 21 parents | To examine physical activity levels and QoL in adolescents with TS and explore TS-specific factors affecting physical activity. | Only 19% met activity guidelines. The Patient-Reported Outcomes Measurement Information System (PROMIS) indicated reduced physical activity and impaired peer relations (as reported by parents). Fatigue and psychosocial barriers (short stature, anxiety, and transport issues) limited activity. Structured routines and social support improved engagement. |
| Van den Hoven AT et al., 2020 [12] | Netherlands | Prospective observational study | n = 177 women with TS | To evaluate HRQoL and psychosocial functioning in adult women with TS as part of a value-based healthcare approach. | Women with TS reported significantly lower HR-QoL (EQ-5D), higher stress (PSS-10), and increased fatigue (CIS-20) compared to controls. Fatigue, stress, diabetes, and orthopedic issues were linked to poorer QoL. |
| Joanne F. Rovet et al., 2019 [13] | Canada | Cross-sectional, retrospective | n = 131 women with TS (70 on growth hormone (GH) and 61 without) | To assess the impact of GH therapy on adult height and QoL in women with TS. | Women with GH treatment were significantly taller and had higher QoL scores (measured via SF-36) than untreated women. Mental health scores were higher in GH-treated group. GH therapy showed long-term benefits beyond height increase. |
| Ertl. et al., 2018 [14] | Austria | Cross-sectional survey study | n = 39 women with TS | To assess the health status, QoL, and satisfaction with medical care among adult women with TS. | QoL was lower in TS women compared to the general population (SF-36). Poorer health (e.g., hearing loss, obesity, and hypertension) correlated with lower QoL. Many participants reported discontinuity of care after childhood, with insufficient transition from pediatric to adult healthcare. Women who received structured follow-up as adults reported better QoL and higher satisfaction with care. |
| Amedro et al., 2019 [15] | France | Controlled cross-sectional study | n = 16 girls with TS and 64 female controls | To evaluate HRQoL in children with TS compared to healthy controls. | Girls with TS showed significantly lower HRQoL scores (measured by PedsQL™ 4.0) than controls, particularly in physical, emotional, and school functioning. These findings highlight the psychosocial and functional impact of TS even in childhood, underlining the need for early support and interventions. |
| Krandz et al., 2019 [16] | Sweden | Longitudinal cohort (20-year follow-up) | n = 178 women with TS | To assess HRQoL in adult women with TS, with a focus on the impact of previous growth hormone treatment and comorbidities and to compare their HRQoL to that of women from the general population. | HRQoL was assessed using validated Swedish versions of the Psychological General Well-Being Index (PGWB) and the Nottingham Health Profile (NHP). Women with TS reported overall HRQoL comparable to that of the general population. GH treatment during childhood was not significantly associated with improved HRQoL, despite resulting in an average height gain of 5.7 cm. Lower HRQoL was significantly associated with older age, later age at diagnosis, and hearing impairment. |
| Taback & Van Vliet, 2011 [17] | Canada | Randomized controlled trial with long-term follow-up | n = 34 women with TS | To investigate whether long-term GH treatment in individuals with TS influences HRQoL in young adulthood—either positively, due to increased height or treatment perception, or negatively, due to prolonged medicalization through years of injections. | HRQoL was assessed using the SF-36 questionnaire. No significant differences were found between GH-treated and untreated groups across all domains. Despite increased adult height from GH therapy, there was no measurable benefit in HRQoL. Results suggest that height gain alone may not influence overall well-being in young adults with TS. |
| Wide Boman et al., 2004 [18] | Sweden | Cross-sectional observational study | n = 63 adult women with TS (mean age 31.5 years) | To investigate how somatic factors and social experiences, including the role of hormone replacement therapy (HRT), are associated with psychological well-being in adult women with TS. | Psychological well-being was assessed using the Psychological General Well-Being (PGWB) Index, complemented by clinical examination data and medical records. Lower well-being was associated with absence of sex hormone therapy in adulthood, hearing impairment, later age at diagnosis and menarche (or induced bleeding), older age, and reported academic difficulties. Age at diagnosis and school-related challenges together accounted for 25% of the variance in well-being. The findings underscore the relevance of these factors in the clinical care of adult women with TS. |
| Karakök et al., 2021 [19] | Turkey | Preliminary study | n = 7 adolescent girls with TS (TS), n = 7 with short stature (SS) and normal karyotype | To evaluate and compare the neurocognitive and psychosocial profiles of adolescents with TS and peers with short stature and normal karyotype. | No significant differences were observed between the two groups in terms of psychiatric diagnoses, social cognition skills, quality of life, self-esteem, and coping strategies. However, adolescents with TS had significantly lower scores in cognitive functioning (working memory, processing speed, and total IQ) than those with SS. Anxiety and conduct problems were more prominent in the SS group. Findings support early neurocognitive assessment and psychosocial support in TS. |
| Jeż et al., 2018 [20] | Poland | Cross-sectional study | n = 176 adult women with TS | To assess the impact of TS and its biological and psychosocial consequences on quality of life, with a focus on life satisfaction. | Life satisfaction was assessed through a standardized questionnaire and logistic regression. The main independent predictors of lower life satisfaction were dissatisfaction with short stature, loneliness, and the feeling of being disabled. Other relevant factors included social stigmatization, family attitudes, and negative self-perception. Findings emphasize the importance of psychosocial support in managing TS. |
| Yusof et al., 2023 [21] | Malaysia | Cross-sectional study | n = 24 TS patients and n = 60 controls | To assess the QoL and body image disturbances in adult patients with TS compared to age-matched healthy controls at a tertiary hospital in Kuala Lumpur, using the World Health Organization Quality of Life (WHOQOL-BREF) Questionnaire and the Body Image Disturbances Questionnaire (BIDQ). | TS patients had comparable overall QoL to controls but significantly lower scores in the social relationship domain. Body image concerns were significantly associated with impairment in social and occupational functioning. The main concern among TS patients was related to short stature and low self-esteem. |
| Okada, 1994 [22] | Japan | Cross-sectional comparative study | n = 20 women with TS; n = 22 GH-deficient women | To evaluate QoL in adult women with TS in comparison with GH-deficient women, based on aspects such as education, employment, income, social life, physical complaints, and emotional well-being. | Turner women had significantly higher university enrollment than the general population (68% vs. 38.2%), similar employment levels to controls, but experienced more body image and marriage-related anxiety. Both groups reported psychosomatic symptoms such as shoulder stiffness and fatigue. |
| Parameter | Children and Adolescents | Adult Women |
|---|---|---|
| Physical Activity | Significantly lower than peers; common barriers include fatigue, short stature, and motor coordination difficulties [11,15] | Reduced stamina, increased fatigue; difficulty engaging in daily activities [12,16] |
| Emotional Health | Anxiety, low self-esteem, and emotional lability [11,15,19] | Increased stress, risk of depression, and feelings of isolation [12,18,20] |
| Social Integration | Difficulties in forming friendships; sense of being “different” [11,15] | Loneliness, low self-confidence, and challenges in intimate relationships [18,20,21] |
| Educational and Cognitive Functioning | Learning difficulties—particularly in mathematics and visuospatial reasoning [19] | Executive function deficits; frequently undiagnosed cognitive impairments [16,18] |
| Impact of Therapy (GH/HRT) | GH improves height but has limited impact on QoL; early psychological support is crucial [13,17] | HRT improves physical outcomes; lack of therapy associated with reduced psychological well-being [18] |
| Psychosocial Support | Better QoL observed in presence of strong family and social support [11,15,19] | Structured care and coordinated transition to adult services enhance overall QoL [14,20] |
| Instrument | Age Group | Domains | Studies Using the Instrument |
|---|---|---|---|
| SF-36 Health Survey | Adults | Physical functioning, role–physical, bodily pain, general health, vitality, social functioning, role–emotional, and mental health | Rovet et al., 2019 [13]; Ertl. et al., 2018 [14]; Taback & Van Vliet, 2011 [17] |
| EQ-5D | Adults | Mobility, self-care, usual activities, pain/discomfort, and anxiety/depression | Van den Hoven et al., 2020 [12] |
| Pediatric Quality of Life Inventory (PedsQL™ 4.0) | Children and adolescents | Physical, emotional, social, and school functioning | Amedro et al., 2017 [15] |
| Psychological General Well-Being Index (PGWB) | Adults | Anxiety, depression, well-being, self-control, vitality, and general health | Krantz et al., 2019 [16]; Wide Boman et al., 2004 [18] |
| WHOQOL-BREF | Adults | Physical health, psychological, social relationships, and environment | Yusof et al., 2023 [21] |
| Body Image Disturbances Questionnaire (BIDQ) | Adults | Body image perception, associated social and occupational impairments | Yusof et al., 2023 [21] |
| Perceived Stress Scale (PSS-10) | Adults | Perceived stress levels | Van den Hoven et al., 2020 [12] |
| Checklist Individual Strength (CIS-20) | Adults | Fatigue, concentration, motivation, and physical activity | Van den Hoven et al., 2020 [12] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stoynova, H.; Staynova, R.; Kafalova, D. How Does Turner Syndrome Affect Quality of Life? A Systematic Review. Medicina 2025, 61, 1643. https://doi.org/10.3390/medicina61091643
Stoynova H, Staynova R, Kafalova D. How Does Turner Syndrome Affect Quality of Life? A Systematic Review. Medicina. 2025; 61(9):1643. https://doi.org/10.3390/medicina61091643
Chicago/Turabian StyleStoynova, Hristina, Radiana Staynova, and Daniela Kafalova. 2025. "How Does Turner Syndrome Affect Quality of Life? A Systematic Review" Medicina 61, no. 9: 1643. https://doi.org/10.3390/medicina61091643
APA StyleStoynova, H., Staynova, R., & Kafalova, D. (2025). How Does Turner Syndrome Affect Quality of Life? A Systematic Review. Medicina, 61(9), 1643. https://doi.org/10.3390/medicina61091643






