Clinical Performance of Endocrowns in Molars: A Scoping Review
Abstract
1. Introduction
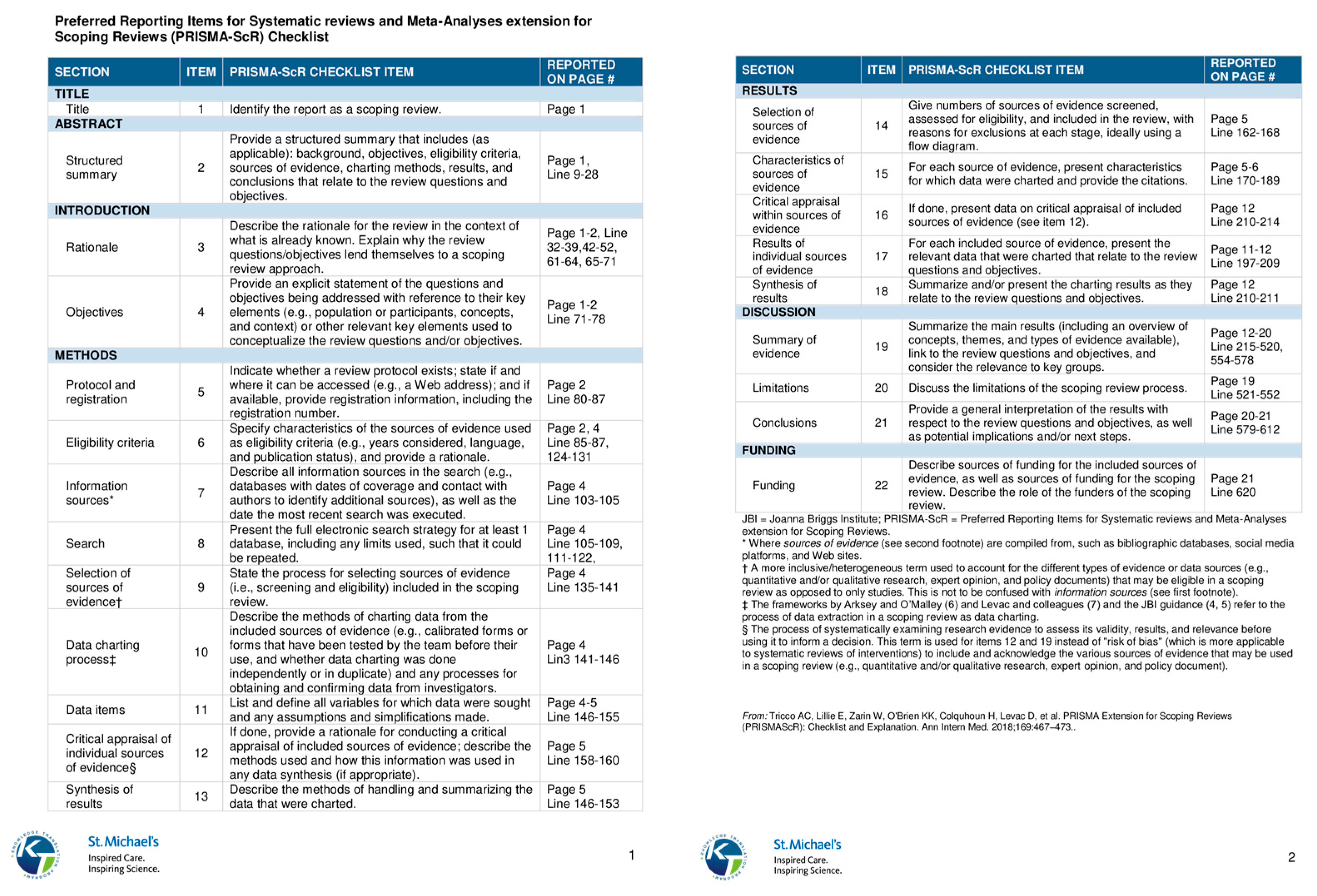
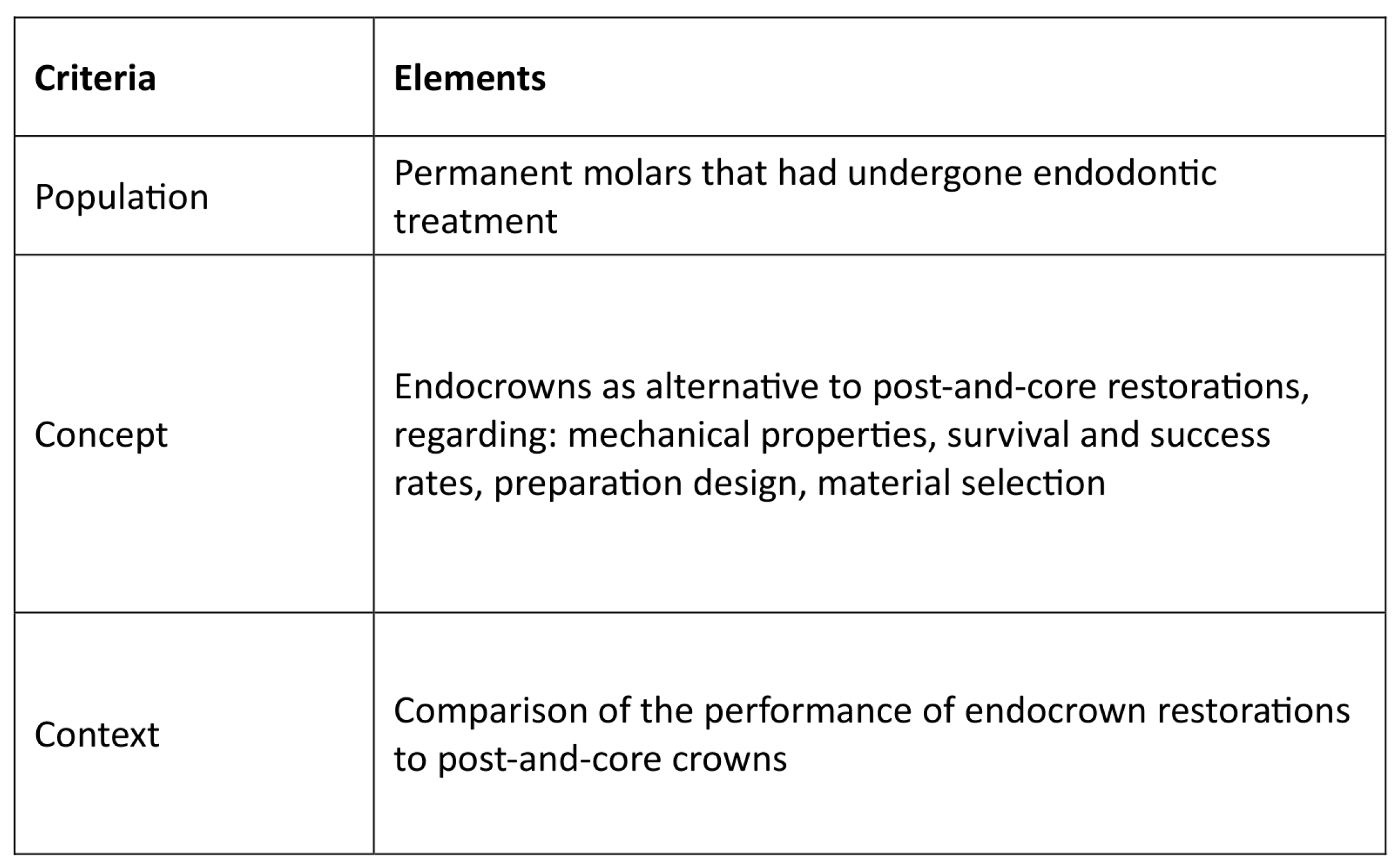
2. Materials and Methods
2.1. Sources of Information and Search Strategy
2.2. Eligibility Criteria
2.3. Data Extraction, Screening, and Charting
3. Results
| Author(s)/Publication Year | Study Type | Objective | Study Design | Main Findings/Conclusion |
|---|---|---|---|---|
| Clinical Performance and Long-Term Outcomes | ||||
| [35] Otto et al., 2015 | Clinical Trial | Evaluation of long-term outcomes of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns | 55 patients, with test group: 25 endocrowns (20 molars, five premolars) and control group: 40 shoulder crowns (8 conventional crowns and 32 “reduced prep” crowns) produced using a CAD/CAM system with feldspathic ceramic and examined at baseline and up to 12 years (mean 10 years, 8 months). |
|
| [30] Belleflamme et al., 2017 | Retrospective Study | Evaluation of ceramic and composite endocrowns with IDS, analyzing failures about tooth preparation and occlusal parameters. | Evaluation of 99 cases with a mean observation period of 44.7 ± 34.6 months using FDI criteria, based on residual tooth tissue and preparation characteristics |
|
| [31] Fages et al., 2017 | Clinical Trial | Determination of the survival rates of chairside CAD/CAM-fabricated all-ceramic crowns and endocrowns for molars in clinical practice. | Between 2003 and 2008, 323 patients received 447 chairside CAD/CAM feldspathic ceramic restorations (212 crowns and 235 endocrowns) on molars by the same dentist, who then followed them up for 7 years. |
|
| [1] Alhamdan et al., 2024 | Narrative Review | Assessment and comparison of treatment options to provide clinical recommendations for restoring posterior ETT. | PubMed and Google Scholar published between 1977 and 2024. |
|
| [14] Ciobanu et al., 2023 | Literature Review | A comprehensive overview of endocrowns and evaluation of the impact of various materials and preparation designs on their mechanical properties, survival, success rate, and esthetics. | PubMed, Scopus, Web of Science, and Scielo Identified records: 163 Included records: 37 |
|
| [8] Morimoto et al., 2024 | Umbrella Review | Synthesis of evidence from systematic reviews on 1-piece endodontic crowns in posterior teeth, assessing clinical outcomes, survival, success rates, and PROMs, with a null hypothesis of no significant difference from complete crowns. | MEDLINE/PubMed, WOS, Cochrane, OpenGrey, and manually (up to June 2024) Identified records: 468 Included records: 9 |
|
| [10] Papalexopoulos et al., 2021 | Literature Review | Evaluation of endocrowns as a reliable alternative for extensively damaged ETT, focusing on their indications, contraindications, preparation, and materials. | Review of the literature with keywords “Endocrowns”, “Endodontically treated teeth’, “Literature review”, “Restorative dentistry” |
|
| [32] Fathi et al., 2022 | Umbrella Review | Evaluation and comparison of the success rates of various prosthetic restorations on ETT. | MEDLINE/PubMed, Cochrane, and Google Scholar (up to November 2020) Identified records: 43 Included records: 14 |
|
| [33] Keskin et al., 2024 | Clinical Trial | Comparison of the clinical efficacy of RNC and ZLS ceramic endocrowns in treating ETT using a chairside CAD/CAM system. | Ninety endocrown restorations were fabricated in posterior teeth (52 RNC, 38 ZLS) using a CAD/CAM system with a three-year follow-up period. |
|
| [34] Kuang et al., 2022 | Retrospective Study | Evaluation of the survival rate and clinical performance of CAD/CAM ceramic endocrowns in posterior ETT. | A total of 101 CAD/CAM ceramic endocrowns on posterior teeth were performed on 74 patients from January 2016 to June 2017 and evaluated for their survival rate after 5 years. |
|
| Design and Adhesion Considerations | ||||
| [38] Magne et al., 2014 | In Vitro Study | Evaluation of the influence of different adhesive core buildup designs on the fatigue resistance and failure mode of endodontically treated molars restored with RNC CAD/CAM crowns using self-adhesive resin cement. | Forty-five human molars were divided into three groups (n = 15) based on the restorative technique: Group I: 4 mm adhesive core buildup with complete crown restorations. Group II: 2 mm adhesive core buildup with complete crown restorations. Group III: No adhesive buildup (endocrown restoration). All groups were subjected to a failure test. |
|
| [36] Dartora et al., 2018 | In Vitro Study | Comparison of the biomechanical behavior of ETT restored with different endocrown extensions into the pulp chamber. | 30 human molars were divided into 3 groups (n = 10) based on intracoronal extension depth (5 mm, 3 mm, 1 mm) and loaded to fracture. |
|
| [15] Einhorn et al., 2019 | In Vitro Study | Evaluation of the impact of ferrule inclusion on the fracture resistance of endocrowns specifically for mandibular molars. | Mandibular third molars (n = 12/group) were prepared by removing coronal tooth structure and restoring the chamber with resin core material. Ferrule heights were 1 mm, 2 mm, or none for each group. CAD/CAM LDS restorations were placed and subjected to failure testing. |
|
| [18] Ribeiro et al., 2023 | In Vitro Study | Exploration and characterization of the influence of the height discrepancy between the pulp chamber floor and the crestal bone on the mechanical fatigue performance of ETT restored with resin composite endocrowns. | 75 human molars were divided into 5 groups (n = 15) based on the pulp chamber floor position relative to crestal bone height (2 mm above, 1 mm above, leveled, 1 mm below, and 2 mm below). All were restored with 1.5 mm-thick composite resin endocrowns and subjected to fatigue failure testing. |
|
| [37] Huang et al., 2023 | In Vitro Study | Analysis of stress distribution in an endodontically treated mandibular molar with various endocrown configurations, particularly focusing on those with significant defects in the mesial wall. | Four distinct finite element models were constructed based on different endocrown configurations for a mandibular molar. Control Model: butt joint preparation with a 2 mm occlusal thickness. Experimental Models: three butt joint designs with varying distances between the bottom of the mesial wall preparation and the cemento-enamel junction set at 2 mm, 1 mm, and 0 mm, respectively. All models are loaded with vertical and oblique forces. |
|
| [39] Zeng et al., 2024 | In Vitro Study | Evaluation of the stress distribution in endocrown restorations applied to ETT, focusing on the effects of different margin designs and loading conditions, and determining how these factors influence stress concentrations and the overall mechanical performance of endocrowns. | Three-dimensional finite element models were created to simulate ETT molars restored with endocrowns. Groups: butt-joint (E0), 90° shoulder (E90), and 135° shoulder (E135) with shoulder group dimensions 1.5 mm height and 1 mm width. Static loads totaling 225 N were applied in 9 locations on the occlusal surface under both buccal and lingual loading conditions. |
|
| Mechanical Strength and Load Resistance | ||||
| [13] Biacchi et al., 2012 | In Vitro Study | Comparison of the fracture strength of endocrowns and glass fiber post-retained conventional crowns, focusing on their mechanical performance under load to ensure the durability and functionality of ETT. | 20 human molars divided into two groups: glass fiber post-retained crowns and endocrowns anchored in the pulp chamber, subjected to controlled loading to assess fracture resistance and failure modes. |
|
| [41] El Ghoul et al., 2019 | In Vitro Study | Evaluation of the fracture resistance and failure modes of endocrowns made of three CAD/CAM materials subjected to thermos-mechanical cycling loading | 80 human molars were divided into 4 groups (n = 20), (LDS crowns, CAD/CAM LDS endocrowns, CAD/CAM ZLS endocrowns, and CAD/CAM RNC endocrowns) with half of them from each group being loaded axially and the other half laterally until fracture. |
|
| [40] Anton Y Otero et al., 2021 | In Vitro Study | Evaluation of the fatigue resistance of cracked endodontically treated molars restored with CAD/CAM resin composite endocrowns reinforced with different fiber-reinforced composite bases. | 50 human molars were simulated with cracks and divided in 5 groups (group 1: cavity floors lined with 0.5 mm of flowable composite, group 2: cavity floors covered with one layer of FRC-net, group 3: cavity floors covered with three layers of FRC-net, group 4: cavity floors covered with 1 mm of flowable FRC-resin, group 5: cavity floors covered with 2 mm of flowable FRC-resin. Groups 1,2,3 use a different flowable resin composite for the preparation of the chamber than groups 4 and 5, with alterations in composition. All groups submitted to loading testing for fatigue resistance. |
|
| [4] Kassis et al., 2021 | In Vitro Study | Evaluation of the fracture resistance and failure modes of endodontically treated mandibular molars restored with different designs of inlays, onlays, and endocrowns. | 180 human third molars were divided into 6 groups (n = 30): control (no preparation), inlay with EverX Posterior, inlay with G-aenial Universal Flo, onlay with EverX Posterior, onlay with G-aenial Universal Flo, and endocrown with an empty pulp chamber and subjected to compressive load. |
|
| Material- Based Comparisons | ||||
| [42] Dartora et al., 2019 | In Vitro Study | Comparison of the fatigue performance and stress distribution of endodontically treated molars restored with CAD-CAM endocrowns made from lithium disilicate or polymer-infiltrated ceramic, and with direct composite restorations. | 48 human molars were divided into three groups (n = 16) and restored with: LD endocrowns, PICN endocrowns, and direct composite restorations. Specimens underwent step-stress fatigue testing, fractographic analysis, and finite element analysis. |
|
| [44] Manziuc et al., 2023 | Literature Review | A review of the literature about the mechanical and biological properties of ZLS in CAD/CAM systems. | PubMed, Web of Science, Cochrane, and manually. Identified records: 154 Included records: 71. |
|
| [20] Veselinova et al., 2023 | In Vitro Study | Comparison of the mechanical behavior of ETT restored with endocrowns or overlays made from either monolithic LDS or monolithic zirconia. | 48 human molars divided into 4 groups (n = 12): overlays restored with monolithic LDS, overlays restored with monolithic zirconia, endocrowns restored with monolithic LDS, endocrowns restored with monolithic zirconia) and subjected to a fracture strength test. |
|
| [19] Vervack et al., 2024 | In Vitro Study | Evaluation of the fracture strength and failure modes of LDS and RNC used as restorations (crown, overlay, or endocrown) on endodontically treated molars. | 60 molars were restored with two primary materials LDS and Hybrid Composite. Each material was employed in three-dimensional restoration designs: monolithic endocrown, crown with a separate composite core, and overlay without core buildup or pulpal extension, and subjected to fracture strength test. Ten sound served as a control group. |
|
| [43] Jalalian et al., 2024 | In Vitro Study | Comparison of the fracture resistance and marginal adaptation of CAD/CAM LDS and ZLS endocrowns. | 24 human molars were divided into 2 groups (n = 12) for ZLS and LDS endocrown fabrication using CAD/CAM. Vertical marginal gap was measured at three stages: before cementation, after cementation, and after thermomechanical cycling. Fracture resistance was tested at a 45° angle, and failure mode was assessed. |
|
| [45] Taha et al., 2024 | In Vitro Study | Comparison of marginal and internal gaps in endocrowns made from three different CAD/CAM materials. | 30 human molars were divided into 3 groups (n = 10): LDGC, resin-modified ceramic, and RNC, and assessed for their accuracy of marginal and internal adaptation of the endocrowns with CBCT. |
|
4. Discussion
4.1. Key Findings of This Scoping Review
4.1.1. Clinical Indications: When and Why to Choose Endocrowns
- Thus, endocrowns are best suited for molars with extensive coronal damage, limitations in root anatomy, or reduced interocclusal space, especially when preserving tooth structure is a clinical priority, as conventional post and core crowns may fail to provide adequate material strength, thickness, and structural support, making endocrowns a more reliable treatment modality.
4.1.2. The Impact of Cuspal Reduction and Intracoronal Extension on Retention and Fracture Resistance
- Therefore, an occlusal thickness of approximately 3 mm is generally recommended to optimize fracture resistance but should be carefully modified based on anatomical and material-related factors to prevent excessive tooth reduction.
- Overall, these findings suggest that while both underextension and overextension carry risks, a 2 mm pulp chamber depth may provide the best balance between retention, stress distribution, and clinical safety.
- Clinically, achieving an adequate pulp chamber depth and maintaining a favorable height-to-width ratio are essential to reduce debonding and stress concentrations—particularly in molars and in cases with limited bone support.
4.1.3. Pulp Chamber Cavity Preparation: Balancing Retention, Resistance, and Bond Strength
- Thus, optimal internal preparation, use of immediate dentin sealing, and careful resin cementation are essential to prevent microleakage, improve retention, and minimize stress at the tooth-restoration interface in endocrown restorations.
4.1.4. The Effect of Finish Line Design on Flexural Strength, Stress Distribution, and Internal Adaptation
- To sum up, while the butt-joint margin remains a minimally invasive and effective option, shoulder finish lines with short ferrules may enhance fracture resistance and stress distribution. Cervical margin placement should be supragingival whenever possible to preserve enamel and maximize bond strength. Individual anatomical characteristics, enamel availability, and material choice should all be taken into consideration when choosing a margin in clinical practice.
4.1.5. Choosing the Right Material: Mechanical and Esthetic Considerations in Endocrown Performance
4.1.6. CAD/CAM-Fabricated Endocrowns: Precision, Efficiency, and Material Compatibility
- Even though CAD/CAM endocrowns have extremely high survival rates and seem a successful long-term alternative, careful case selection and proper bonding techniques are essential to minimize risks and ensure successful outcomes.
4.2. Survival and Success Rates: Long-Term Outcomes and Clinical Predictability of Endocrowns
- The success rate of endocrowns varies across different studies but consistently remains high, making them an excellent conservative option for restoring endodontically treated teeth.
4.3. Limitations of This Scoping Review
Methodological Limitations of the Included Studies
4.4. Clinical Implications and Recommendations
- Indications: Endocrowns are best suited for posterior ETT, particularly molars with short, calcified, or divergent roots where post-and-core restorations are not feasible.
- Case selection: Avoid endocrowns in teeth with insufficient pulp chamber depth (<2 mm), limited enamel margins, or unfavorable height-to-width ratios.
- Pulp chamber depth: A 2 mm extension into the pulp chamber is generally recommended, as it balances retention and stress distribution while minimizing catastrophic failures.
- Occlusal thickness: Maintain around 3 mm occlusal reduction for optimal fracture resistance, but avoid unnecessary removal of tooth structure.
- Ferrule and finish line: A 1 mm ferrule with shoulder finish line improves stress distribution and reduces irreparable fractures; if not possible, a butt-joint margin is a conservative alternative.
- Preparation design: Ensure a flat pulpal floor, 6° divergence, and rounded internal angles, and consider immediate dentin sealing (IDS) to enhance adhesion.
- Material selection:
- LDS: Strong adhesive bond and esthetics, first choice when high strength and reliability are needed.
- ZLS: Combines good strength and moderate esthetics.
- RNC/PICN: More elastic and repairable, reducing catastrophic fractures, but higher risk of debonding.
- Cementation: Resin cements are preferred, ensuring adequate adhesion to minimize debonding and stress accumulation.
5. Conclusions
- Clinical Recommendations:
- Endocrowns are best suited for molars with extensive coronal loss, short roots, or limited interocclusal space.
- Preservation of enamel at the restoration margins is essential for optimal adhesion and long-term success.
- Lithium disilicate or resin-based materials should be preferred due to their superior fracture resistance and esthetics.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Databases/Keywords | Endocrowns | Endocrowns and Materials | Endocrowns and Ferrule Effect | Endocrowns and Survival Rate | Endocrowns and Post-and-Core Restorations | Total |
|---|---|---|---|---|---|---|
| PubMed (MEDLINE) | 343 | 274 | 38 | 27 | 61 | 743 |
| Scopus | 315 | 264 | 39 | 32 | 41 | 691 |
Appendix B
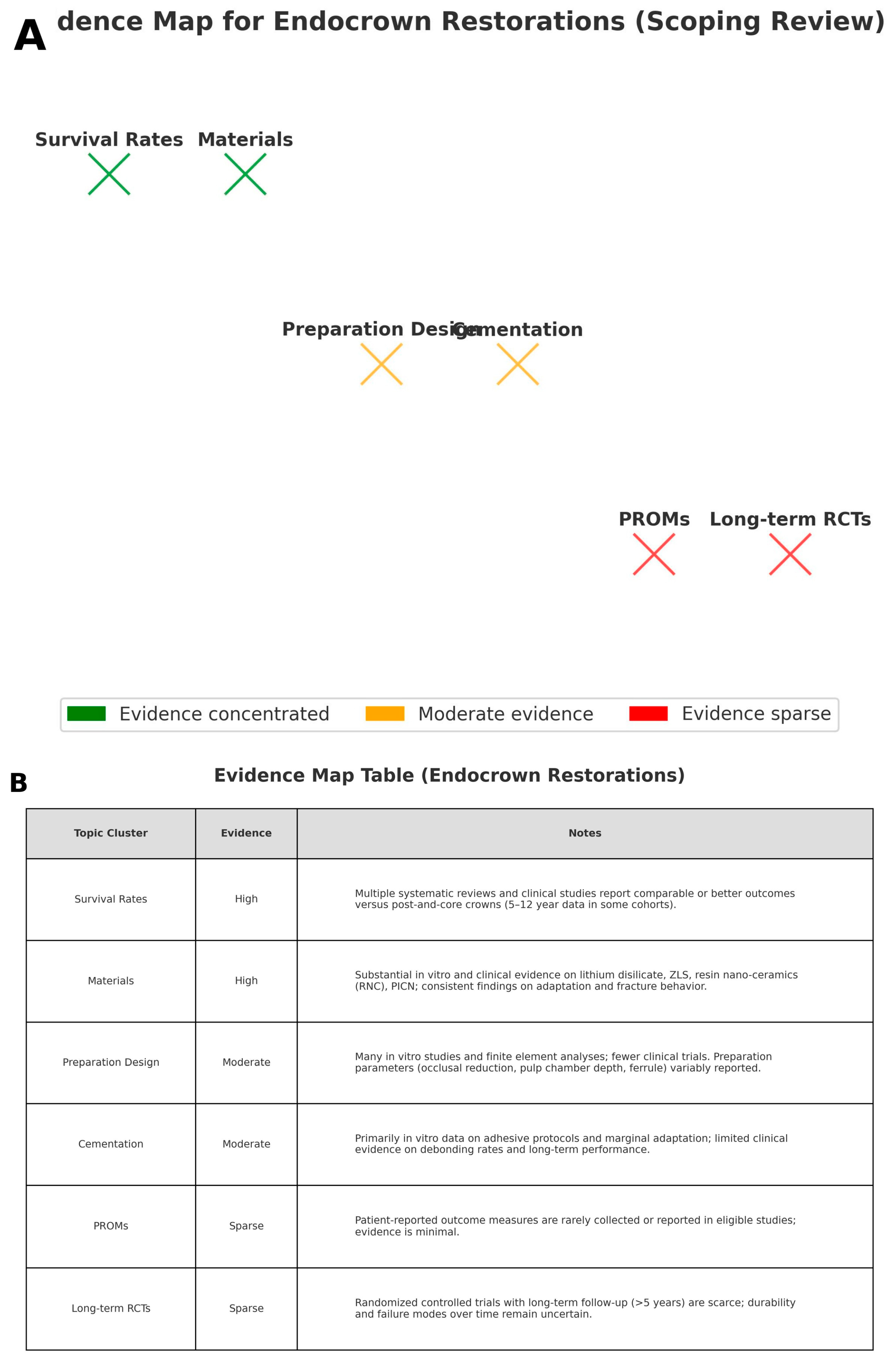
Appendix C. Evidence Map of Endocrown Restorations
References
- Alhamdan, M.M.; Aljamaan, R.F.; Abuthnain, M.M.; Alsumikhi, S.A.; Alqahtani, G.S.; Alkharaiyef, R.A. Direct Versus Indirect Treatment Options of Endodontically Treated Posterior Teeth: A Narrative Review. Cureus 2024, 16, e67698. [Google Scholar] [CrossRef]
- Beji Vijayakumar, J.; Varadan, P.; Balaji, L.; Rajan, M.; Kalaiselvam, R.; Saeralaathan, S.; Ganesh, A. Fracture resistance of resin based and lithium disilicate endocrowns. Which is better?—A systematic review of in-vitro studies. Biomater. Investig. Dent. 2021, 8, 104–111. [Google Scholar] [CrossRef]
- Carvalho, M.A.; Lazari, P.C.; Gresnigt, M.; Del Bel Cury, A.A.; Magne, P. Current options concerning the endodontically-treated teeth restoration with the adhesive approach. Braz. Oral. Res. 2018, 32, e74. [Google Scholar] [CrossRef]
- Kassis, C.; Khoury, P.; Mehanna, C.Z.; Baba, N.Z.; Bou Chebel, F.; Daou, M.; Hardan, L. Effect of Inlays, Onlays and Endocrown Cavity Design Preparation on Fracture Resistance and Fracture Mode of Endodontically Treated Teeth: An In Vitro Study. J. Prosthodont. 2021, 30, 625–631. [Google Scholar] [CrossRef] [PubMed]
- AlDabeeb, D.S.; Alakeel, N.S.; Al Jfshar, R.M.; Alkhalid, T.K. Endocrowns: Indications, Preparation Techniques, and Material Selection. Cureus 2023, 15, e49947. [Google Scholar] [CrossRef]
- Al-Dabbagh, R.A. Survival and success of endocrowns: A systematic review and meta-analysis. J. Prosthet. Dent. 2021, 125, 415.e411–415.e419. [Google Scholar] [CrossRef] [PubMed]
- Papia, E.; Habib, W.; Larsson, C. The Influence of Different Designs, Materials and Cements on the Success and Survival Rate of Endocrowns. A Systematic Review. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 100–111. [Google Scholar] [CrossRef]
- Morimoto, S.; Arakaki, Y.; Raggio, D.P.; Özcan, M. One-piece endodontic crowns in posterior teeth: An overview of systematic reviews. J. Prosthet. Dent. 2024. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.M.; Kelly, A.; Tagiyeva, N.; Kanagasingam, S. Comparing endocrown restorations on permanent molars and premolars: A systematic review and meta-analysis. Br. Dent. J. 2020. [Google Scholar] [CrossRef]
- Papalexopoulos, D.; Samartzi, T.K.; Sarafianou, A. A Thorough Analysis of the Endocrown Restoration: A Literature Review. J. Contemp. Dent. Pract. 2021, 22, 422–426. [Google Scholar] [CrossRef]
- AlHelal, A.A. Biomechanical behavior of all-ceramic endocrowns fabricated using CAD/CAM: A systematic review. J. Prosthodont. Res. 2024, 68, 50–62. [Google Scholar] [CrossRef]
- Alwadai, G.S.; Al Moaleem, M.M.; Daghrery, A.A.; Albar, N.H.; Daghriri, A.A.; AlGhamdi, M.M.; Ageel, S.E.; Daghreeri, F.A.A.; Al-Amri, T.M.A.; Aridhi, W.H.; et al. A Comparative Analysis of Marginal Adaptation Values between Lithium Disilicate Glass Ceramics and Zirconia-Reinforced Lithium Silicate Endocrowns: A Systematic Review of In Vitro Studies. Med. Sci. Monit. 2023, 29, e942649. [Google Scholar] [CrossRef]
- Biacchi, G.R.; Basting, R.T. Comparison of fracture strength of endocrowns and glass fiber post-retained conventional crowns. Oper. Dent. 2012, 37, 130–136. [Google Scholar] [CrossRef]
- Ciobanu, P.; Manziuc, M.M.; Buduru, S.D.; Dudea, D. Endocrowns—A literature review. Med. Pharm. Rep. 2023, 96, 358–367. [Google Scholar] [CrossRef]
- Einhorn, M.; DuVall, N.; Wajdowicz, M.; Brewster, J.; Roberts, H. Preparation Ferrule Design Effect on Endocrown Failure Resistance. J. Prosthodont. 2019, 28, e237–e242. [Google Scholar] [CrossRef]
- Mostafavi, A.S.; Allahyari, S.; Niakan, S.; Atri, F. Effect of Preparation Design on Marginal Integrity and Fracture Resistance of Endocrowns: A Systematic Review. Front. Dent. 2022, 19, 37. [Google Scholar] [CrossRef]
- Pissis, P. Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract. Periodontics Aesthet. Dent. 1995, 7, 83–94. [Google Scholar] [PubMed]
- Ribeiro, V.F.; da Rosa, L.S.; Tribst, J.P.M.; Bier, C.A.S.; Morgental, R.D.; Valandro, L.F.; Baldi, A.; Scotti, N.; Pereira, G.K.R. Influence of height discrepancy between pulp chamber floor and crestal bone in the mechanical fatigue performance of endodontically-treated teeth restored with resin composite endocrowns. J. Mech. Behav. Biomed. Mater. 2023, 142, 105854. [Google Scholar] [CrossRef]
- Vervack, V.; Johansson, C.; Coster, P.; Fokkinga, W.; Papia, E.; Vandeweghe, S. The fracture strength and the failure mode of lithium disilicate or resin nano ceramics as a crown, overlay, or endocrown restoration on endodontically treated teeth. J. Esthet. Restor. Dent. 2024, 36, 796–803. [Google Scholar] [CrossRef]
- Veselinova, M.; Diamantopoulou, S.; Paximada, C.; Papazoglou, E. In-Vitro Comparison of Fracture Strength of Endocrowns and Overlays in Endodontically Treated Teeth Manufactured with Monolithic Lithium Disilicate and Zirconia. J. Funct. Biomater. 2023, 14, 422. [Google Scholar] [CrossRef]
- Bindl, A.; Mörmann, W.H. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years—Preliminary results. J. Adhes. Dent. 1999, 1, 255–265. [Google Scholar]
- Ghajghouj, O.; Taşar-Faruk, S. Evaluation of Fracture Resistance and Microleakage of Endocrowns with Different Intracoronal Depths and Restorative Materials Luted with Various Resin Cements. Materials 2019, 12, 2528. [Google Scholar] [CrossRef]
- Sedrez-Porto, J.A.; Rosa, W.L.; da Silva, A.F.; Münchow, E.A.; Pereira-Cenci, T. Endocrown restorations: A systematic review and meta-analysis. J. Dent. 2016, 52, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Qamar, Z.; Alghamdi, A.M.S.; Haydarah, N.K.B.; Balateef, A.A.; Alamoudi, A.A.; Abumismar, M.A.; Mathur, A.; Minervini, G. In Vitro Evaluation of Lithium Disilicate Endocrowns and Post and Core Crowns—A Systematic Review. J. Funct. Biomater. 2023, 14, 276. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Govare, N.; Contrepois, M. Endocrowns: A systematic review. J. Prosthet. Dent. 2020, 123, 411–418.e419. [Google Scholar] [CrossRef]
- Lenz, U.; Bacchi, A.; Della Bona, A. Biomechanical performance of endocrown and core-crown restorations: A systematic review. J. Esthet. Restor. Dent. 2024, 36, 303–323. [Google Scholar] [CrossRef]
- Matos, L.M.R.; Silva, M.L.; Cordeiro, T.O.; Cardoso, S.A.M.; Campos, D.E.S.; de Muniz, I.A.F.; Barros, S.A.L.; Seraidarian, P.I. Clinical and laboratorial performance of rehabilitation of endodontically treated teeth: A systematic review. J. Esthet. Restor. Dent. 2024, 36, 1281–1300. [Google Scholar] [CrossRef]
- Belleflamme, M.M.; Geerts, S.O.; Louwette, M.M.; Grenade, C.F.; Vanheusden, A.J.; Mainjot, A.K. No post-no core approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases. J. Dent. 2017, 63, 1–7. [Google Scholar] [CrossRef]
- Fages, M.; Raynal, J.; Tramini, P.; Cuisinier, F.J.; Durand, J.C. Chairside Computer-Aided Design/Computer-Aided Manufacture All-Ceramic Crown and Endocrown Restorations: A 7-Year Survival Rate Study. Int. J. Prosthodont. 2017, 30, 556–560. [Google Scholar] [CrossRef]
- Fathi, A.; Ebadian, B.; Dezaki, S.N.; Mardasi, N.; Mosharraf, R.; Isler, S.; Tabatabaei, S.S. An Umbrella Review of Systematic Reviews and Meta-Analyses Evaluating the Success Rate of Prosthetic Restorations on Endodontically Treated Teeth. Int. J. Dent. 2022, 2022, 4748291. [Google Scholar] [CrossRef]
- Keskin, S.C.; Sakar, A.; Bolay, S. A 3-year clinical evaluation of endocrown restorations with two different materials using the computer-aided design/ computer-aided manufacture system. J. Dent. 2024, 151, 105405. [Google Scholar] [CrossRef]
- Kuang, J.X.; Wu, H.Z.; Pan, Y.T.; Cheng, X.G.; Tian, Y.; Yu, Q. A 5-year retrospective study of computer aided design and computer aided manufacturing ceramic endocrowns in endodontically treated posterior teeth. Chin. J. Stomatol. 2022, 57, 1043–1047. [Google Scholar] [CrossRef]
- Otto, T.; Mörmann, W.H. Clinical performance of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns up to 12 years. Int. J. Comput. Dent. 2015, 18, 147–161. [Google Scholar]
- Dartora, N.R.; de Conto Ferreira, M.B.; Moris, I.C.M.; Brazão, E.H.; Spazin, A.O.; Sousa-Neto, M.D.; Silva-Sousa, Y.T.; Gomes, E.A. Effect of Intracoronal Depth of Teeth Restored with Endocrowns on Fracture Resistance: In Vitro and 3-dimensional Finite Element Analysis. J. Endod. 2018, 44, 1179–1185. [Google Scholar] [CrossRef]
- Huang, Y.; Fokkinga, W.A.; Zhang, Q.; Creugers, N.H.J.; Jiang, Q. Biomechanical properties of different endocrown designs on endodontically treated teeth. J. Mech. Behav. Biomed. Mater. 2023, 140, 105691. [Google Scholar] [CrossRef]
- Magne, P.; Carvalho, A.O.; Bruzi, G.; Anderson, R.E.; Maia, H.P.; Giannini, M. Influence of no-ferrule and no-post buildup design on the fatigue resistance of endodontically treated molars restored with resin nanoceramic CAD/CAM crowns. Oper. Dent. 2014, 39, 595–602. [Google Scholar] [CrossRef]
- Zeng, B.; Luo, B.; Hu, J.; Meng, D.; Zhang, J.; Cao, X.; Jiang, Q. Effect of margin designs and loading conditions on the stress distribution of endocrowns: A finite element analysis. BMC Oral. Health 2024, 24, 657. [Google Scholar] [CrossRef]
- Anton Y Otero, C.; Bijelic-Donova, J.; Saratti, C.M.; Vallittu, P.K.; di Bella, E.; Krejci, I.; Rocca, G.T. The influence of FRC base and bonded CAD/CAM resin composite endocrowns on fatigue behavior of cracked endodontically-treated molars. J. Mech. Behav. Biomed. Mater. 2021, 121, 104647. [Google Scholar] [CrossRef]
- El Ghoul, W.; Özcan, M.; Silwadi, M.; Salameh, Z. Fracture resistance and failure modes of endocrowns manufactured with different CAD/CAM materials under axial and lateral loading. J. Esthet. Restor. Dent. 2019, 31, 378–387. [Google Scholar] [CrossRef]
- Dartora, G.; Rocha Pereira, G.K.; Varella de Carvalho, R.; Zucuni, C.P.; Valandro, L.F.; Cesar, P.F.; Caldas, R.A.; Bacchi, A. Comparison of endocrowns made of lithium disilicate glass-ceramic or polymer-infiltrated ceramic networks and direct composite resin restorations: Fatigue performance and stress distribution. J. Mech. Behav. Biomed. Mater. 2019, 100, 103401. [Google Scholar] [CrossRef]
- Jalalian, E.; Zarbakhsh, A.; Khorshidi, S.; Golalipour, S.; Mohammadnasl, S.; Sayyari, M. Comparative analysis of endocrown fracture resistance and marginal adaptation: CAD/CAM technology using lithium disilicate vs. zirconia-reinforced lithium silicate ceramics. Saudi Dent. J. 2024, 36, 353–358. [Google Scholar] [CrossRef]
- Manziuc, M.; Kui, A.; Chisnoiu, A.; Labuneț, A.; Negucioiu, M.; Ispas, A.; Buduru, S. Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding. Medicine 2023, 59, 2135. [Google Scholar] [CrossRef]
- Taha, A.I.; Hatata, N. Marginal and internal gaps evaluation of endocrown restoration fabricated of different CAD/CAM materials using CBCT: An In vitro study. Adv. Dent. J. 2024, 6, 208–215. [Google Scholar] [CrossRef]
- Soliman, M.; Alshamrani, L.; Yahya, B.; Alajlan, G.; Aldegheishem, A.; Eldwakhly, E. Monolithic Endocrown Vs. Hybrid Intraradicular Post/Core/Crown Restorations for Endodontically Treated Teeth; Cross-sectional Study. Saudi J. Biol. Sci. 2021, 28, 6523–6531. [Google Scholar] [CrossRef]
- Taha, D.; Spintzyk, S.; Schille, C.; Sabet, A.; Wahsh, M.; Salah, T.; Geis-Gerstorfer, J. Fracture resistance and failure modes of polymer infiltrated ceramic endocrown restorations with variations in margin design and occlusal thickness. J. Prosthodont. Res. 2018, 62, 293–297. [Google Scholar] [CrossRef]
- Zhang, Y.; Lai, H.; Meng, Q.; Gong, Q.; Tong, Z. The synergetic effect of pulp chamber extension depth and occlusal thickness on stress distribution of molar endocrowns: A 3-dimensional finite element analysis. J. Mater. Sci. Mater. Med. 2022, 33, 56. [Google Scholar] [CrossRef]
- Hayes, A.; Duvall, N.; Wajdowicz, M.; Roberts, H. Effect of Endocrown Pulp Chamber Extension Depth on Molar Fracture Resistance. Oper. Dent. 2017, 42, 327–334. [Google Scholar] [CrossRef]
- Alqarni, H.; Qadoumi, M.; AlShehri, N.; AlNowaiser, N.; Alaqeely, R.; AlHelal, A.A.; Alrabiah, M.; Alshihri, A.; Alsayed, H. Resistance of Resin-Bonded Ceramic Endocrowns of Different Intracoronal Depths. Oral. Health Prev. Dent. 2025, 23, 51–58. [Google Scholar] [CrossRef]
- Yılmaz, K.; Aydın, H.; Gönüldaş, F.; Kara, S.; Çiloğlu, Ö.; Özdemir, E.; Bilen, Z. Effect of Pulpal Base, Restorative Material, and Preparation Type on Marginal and Internal Fit and Fracture Strength of Endocrowns. Materials 2025, 18, 2137. [Google Scholar] [CrossRef]
- Dong, X.; Ban, J.; Guo, H.; Zeng, Z.; Ren, N.; Bai, S.; Wang, Z. Optimization of endocrown design parameters for mandibular second molars: A 3D finite element analysis. J. Mech. Behav. Biomed. Mater. 2025, 168, 107038. [Google Scholar] [CrossRef]
- Karn, G.; Shetty, M.; Hegde, C. Effect of different restorative design on stress concentration of lithium disilicate and monolithic zirconia endocrown on a mandibular molar—A finite element analysis. BMC Oral. Health 2025, 25, 205. [Google Scholar] [CrossRef]
- Kumar, M.; Sidhu, K.; Bhushan, J. Comparative evaluation of marginal and internal fit of endocrowns with lithium disilicate, biocompatible high-performance polymer, and monolithic ceramic materials using computer-aided design and computer-aided manufacturing technology. J. Conserv. Dent. Endod. 2025, 28, 389–393. [Google Scholar] [CrossRef]
- Falahchai, M.; Ardekani, F.R.; Musapoor, N.; Hemmati, Y.B.; Asli, H.N. Effects of the Presence of Adjacent Tooth and Material Type on the Marginal and Internal Adaptation of Endocrowns Fabricated by the Digital Impression Technique. Clin. Exp. Dent. Res. 2025, 11, e70077. [Google Scholar] [CrossRef]
- Facenda, J.C.; Borba, M.; Corazza, P.H. A literature review on the new polymer-infiltrated ceramic-network material (PICN). J. Esthet. Restor. Dent. 2018, 30, 281–286. [Google Scholar] [CrossRef]
- Hiraba, H.; Nishio, K.; Takeuchi, Y.; Ito, T.; Yamamori, T.; Kamimoto, A. Application of one-piece endodontic crowns fabricated with CAD-CAM system to molars. Jpn. Dent. Sci. Rev. 2024, 60, 81–94. [Google Scholar] [CrossRef]
- Ayata, M.; Küçükömeroğlu Oktay, E.; Albayrak, H.; Çakar, M.; Özcan, M. Evaluation of the clinical performance of endocrown and overlay restorations: A 4-year retrospective study. J. Dent. 2025, 160, 105874. [Google Scholar] [CrossRef]


| Author(s)/Publication Year | Aim | Materials and Methods | Conclusion |
|---|---|---|---|
| Comparison of Endocrown Restorations to Conventional Crowns | |||
| [23] Sendrez-Porte et al., 2016 | Systematic review of clinical and in vitro studies comparing endocrown restorations with conven [tional treatments (posts-and-core crowns, composite resin, inlays/onlays), testing the hypothesis that endocrowns perform similarly. | Pubmed (MedLine), Lilacs, Ibecs, Web of Science, BBO, Scielo, and Scopus Identified records: 103 Included records: 8 published between 1999 and 2014 | Endocrowns offer comparable or superior performance to traditional methods, such as posts-and-core crowns, with demonstrated high success rates (94–100%), greater fracture strength, and favorable biomechanical performance, particularly in terms of failure patterns. Further studies are needed to validate long-term outcomes. |
| [27] Govare et al., 2020 | Evaluation of endocrowns as a restorative option for extensively damaged teeth, assessing their predictability, success, survival rates, and fracture strength compared to post-retained restorations. | PubMed, Scopus, Embase, and the Cochrane Library Identified records: 110 Included records: 41 published between 1999 and 2018. | Endocrowns offer a reliable alternative to post-retained restorations, especially for molars, with comparable or superior fracture strength. |
| [6] Al-Dabbagh et al., 2021. | A review and analysis of the survival and success rates of endocrowns vs. conventional crowns, offering evidence—based guidance for restoring extensively damaged teeth. | PubMed, Scopus, EMBASE, Cochrane, and Google Scholar (up to June 2019) Identified records: 2584 Included records: 10 articles for systematic review and 3 clinical studies for meta-analysis. | Endocrowns showed a 5-year survival rate of 91.4% and a success rate of 77.7%, compared to 98.3% and 94% for conventional crowns, with no significant differences (p > 0.05). |
| [24] Qamar et al., 2023 | Comparison of the physical and mechanical properties of LDS endocrowns on posterior teeth and post-and-core restorations. | PubMed, Embase, Scopus, ISI Web of Knowledge (WoS), Google Scholar, unpublished studies, conference proceedings, and cross-references up to 31 January 2023 Identified records: 291 Included records: 10 | There is no significant difference between the fracture strength and failure rates of LDS endocrowns and conventional post-and-core crowns. |
| [28] Lenz et al., 2024 | Comparison of the biomechanical performance of endocrowns and traditional post-and-core crown restorations (with and without intracanal posts) for rehabilitating ETT with severe coronal structure damage. | MEDLINE/PubMed, Scopus, and Web of Science, based on in vitro studies Identified records: 291 Included records: 31 published between 2015 and 2023. | Endocrowns exhibited similar or greater biomechanical performance than post-and-core crown restorations across most evaluated studies. Demonstrated favorable survival rates under fatigue and monotonic loads, lower stress levels in restorative materials, and better failure patterns compared to post-and core-crowns. |
| [29] Matos et al., 2024 | Assessment of clinical performance (survival rate, failure risk, fracture incidence) and laboratory outcomes (fracture mode, failure analysis) of rehabilitated ETT. | Pubmed, Scopus, Web of Science, Embase, Cochrane, Open Grey, and manually Identified records: 89 articles Included records: 38 (31 in vitro and 7 RCTs) | No significant difference in fracture resistance or failure modes between ETT with or without posts. Survival rates were similar, though failure risk was lower with posts. The need to consider tooth characteristics and remaining structure for each case. |
| Material-Based Comparison | |||
| [2] Beji Vijayakumar et al., 2021 | Evaluation of whether RB endocrowns exhibit better fracture resistance and fewer catastrophic failures compared to LDS endocrowns in vitro studies. | PubMed, EBSCOhost, Cochrane Central Register of Clinical Trials, Google Scholar, and manually. Identified records: 229 Included records: 5 published between 2015 and 2020. | RB endocrowns demonstrated similar or higher fracture resistance under axial forces and fewer catastrophic failures compared to LDS endocrowns. |
| [12] Alwadai et al., 2023 | Analysis of in vitro studies on marginal adaptation of CAD/CAM and heat-pressed LDS and ZLS endocrowns. | Web of Science, PubMed, EMBASE, Scopus, Cochrane, Google Scholar, and ProQuest Identified records: 428 Included records: 17 published between 2016 and 2023. | All-ceramic LDGC and zirconia endocrowns for posterior teeth, fabricated via CAD/CAM or heat-press, showed acceptable marginal adaptation. |
| [11] AlHelal et al., 2024 | Assessment of fracture resistance of CAD/CAM vs. non-CAD/CAM endocrowns. | Embase, Web of Science, and Scopus. Identified records: 1591 Included records: 17 | CAD/CAM endocrowns show superior fracture resistance compared to non-CAD/CAM options. |
| Survival and Success Rates | |||
| [7] Papia et al., 2020 | A review of the literature on endocrowns, focusing on success, survival rates, and how designs, materials, and cements influence outcomes, provides guidance for restoring extensively damaged teeth. | Searches in PubMed, Cochrane, and Scopus Identified records: 3472 Included records: 6 Published between 1999 and 2017. | Feldspathic endocrowns with a 1–4 mm pulp cavity, 1–2 mm shoulder preparation, and adhesive resin cement show promise for molars. |
| [16] Mostafavi et al., 2022 | Evaluation of how preparation designs affect marginal integrity and fracture resistance of endocrowns, aiming to identify optimal designs for restoring severely damaged teeth. | Searches in PubMed, Embase, Scopus, and the Cochrane Library Identified records: 200 included records: 16 published up to February 2021. | Endocrown preparation design impacts marginal adaptation and fracture resistance, with excessive preparation reducing performance and increasing non-repairable fractures. Simpler cavity configurations are recommended. |
| Material | Elastic Modulus | Fracture Resistance | Esthetics | Bonding | Failure Type | Recommended Application |
|---|---|---|---|---|---|---|
| LDS | ~90–95 GPa | Excellent | Excellent | Strong micromechanical bond | Often catastrophic | High-esthetic zones, molars with deep chambers |
| ZLS | ~70 GPa | Very good | Moderate–High | Good | Mixed failures (some catastrophic) | Balanced cases with moderate esthetic needs |
| RNC | ~20 GPa | Moderate–High | Moderate | Weaker than LDS | Mostly restorable, flexible, debonding at adhesive interface | Bruxism, minimal preparations, repairable restorations intraorally |
| PICN | ~30 GPa | Moderate | Moderate | Moderate | Deformable, restorable, debonding at adhesive interface | Patients with parafunctional activity or low occlusal clearance |
| Monolithic Zirconia | >200 GPa | High but brittle | Low–Moderate | Weak | Catastrophic, root fracture | Not commonly recommended, low-esthetic/high-load areas only, good marginal fit |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kontakou Zoniou, A.; Tzimas, K.; Pappa, E.; Rahiotis, C. Clinical Performance of Endocrowns in Molars: A Scoping Review. Medicina 2025, 61, 1562. https://doi.org/10.3390/medicina61091562
Kontakou Zoniou A, Tzimas K, Pappa E, Rahiotis C. Clinical Performance of Endocrowns in Molars: A Scoping Review. Medicina. 2025; 61(9):1562. https://doi.org/10.3390/medicina61091562
Chicago/Turabian StyleKontakou Zoniou, Anna, Konstantinos Tzimas, Eftychia Pappa, and Christos Rahiotis. 2025. "Clinical Performance of Endocrowns in Molars: A Scoping Review" Medicina 61, no. 9: 1562. https://doi.org/10.3390/medicina61091562
APA StyleKontakou Zoniou, A., Tzimas, K., Pappa, E., & Rahiotis, C. (2025). Clinical Performance of Endocrowns in Molars: A Scoping Review. Medicina, 61(9), 1562. https://doi.org/10.3390/medicina61091562







