Establishing the Neck Disability Index as a Valid Tool for Assessing Persistent Neck Pain in the Albanian Population
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
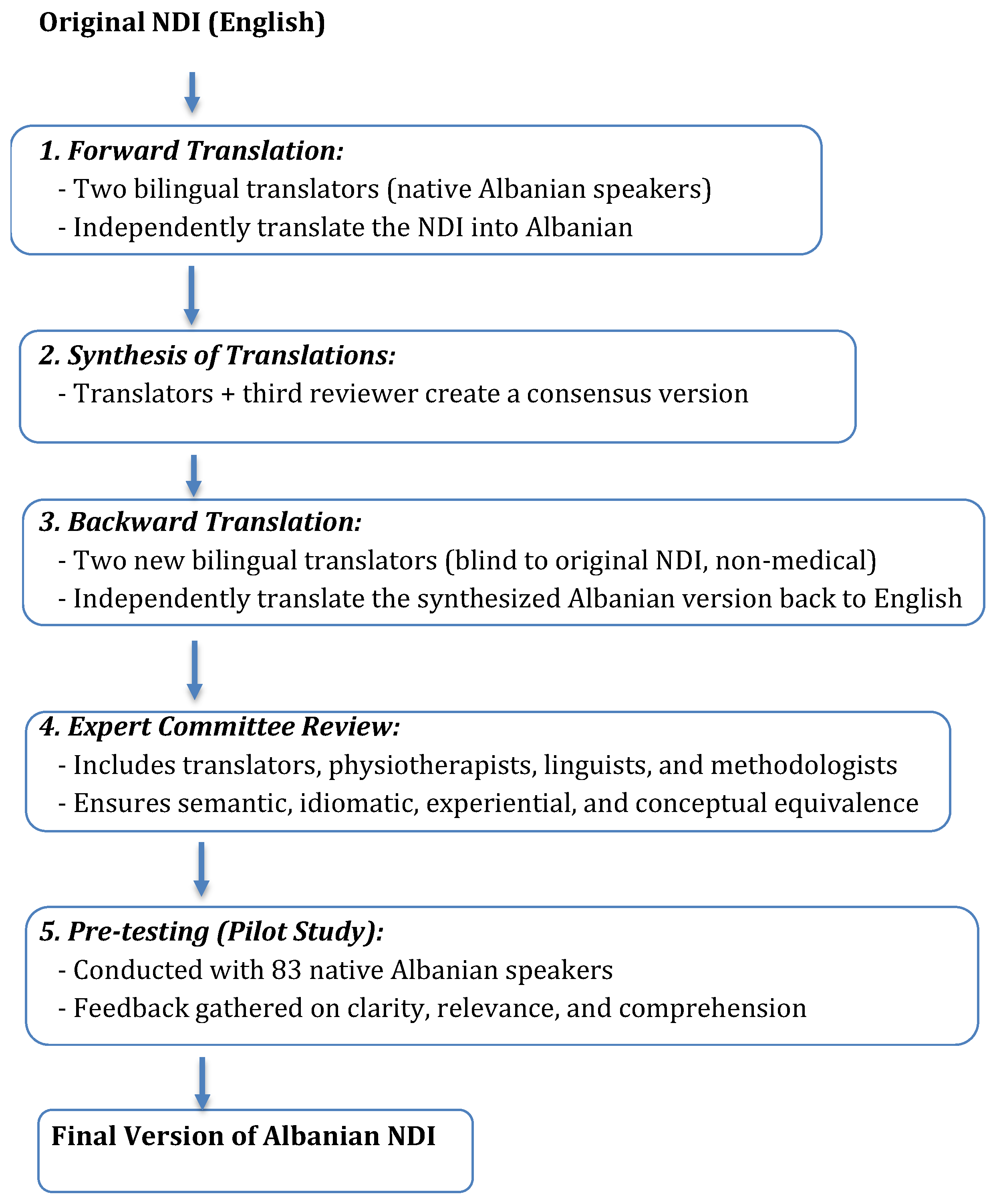
2.2. Translation and Cross-Cultural Adaptation
- Forward Translation: Two independent bilingual translators, whose native language was Albanian and who were fluent in English, translated the original English version of the NDI into Albanian.
- Synthesis: A consensus version of the forward translations was synthesized by the translators and a third reviewer.
- Backward Translation: Two different bilingual translators, blinded to the original version and with no medical background, independently translated the synthesized Albanian version back into English.
- Expert Committee Review: An expert committee composed of translators, physiotherapists, linguists, and methodologists reviewed all versions to achieve semantic, idiomatic, experiential, and conceptual equivalence.
- Pre-testing: The pre-final version was administered to a pilot group of 83 native Albanian speakers. Participants were asked to provide feedback regarding clarity, relevance, and comprehensibility of the items. Necessary modifications were made based on their input.
2.3. Participants
2.4. Instrument: Neck Disability Index (NDI)
2.5. Procedure
2.6. Psychometric Testing
2.7. Data Analysis
3. Results
4. Discussion
4.1. Implications for Practice and Research
4.2. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kazeminasab, S.; Nejadghaderi, S.A.; Amiri, P.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.; Safiri, S. Neck Pain: Global Epidemiology, Trends and Risk Factors. BMC Musculoskelet. Disord. 2022, 23, 26. [Google Scholar] [CrossRef] [PubMed]
- Rushton, A.; Carlesso, L.C.; Flynn, T.; Hing, W.A.; Rubinstein, S.M.; Vogel, S.; Kerry, R. International Framework for Examination of the Cervical Region for Potential of Vascular Pathologies of the Neck Prior to Musculoskeletal Intervention: International IFOMPT Cervical Framework. J. Orthop. Sports Phys. Ther. 2023, 53, 7–22. [Google Scholar] [CrossRef] [PubMed]
- Bobos, P.; MacDermid, J.C.; Walton, D.M.; Gross, A.; Santaguida, P.L. Patient-Reported Outcome Measures Used for Neck Disorders: An Overview of Systematic Reviews. J. Orthop. Sports Phys. Ther. 2018, 48, 775–788. [Google Scholar] [CrossRef] [PubMed]
- MacDermid, J.C.; Walton, D.M. Development and Validation of the ND10 to Measure Neck-Related Functional Disability. BMC Musculoskelet. Disord. 2022, 23, 605. [Google Scholar] [CrossRef]
- Vernon, H.; Mior, S. The Neck Disability Index: A Study of Reliability and Validity. J. Manip. Physiol. Ther. 1991, 14, 409–415. [Google Scholar]
- Santiago-Reynoso, G.M.; Alvarado-Luna, A.E.; Fernandez-Matias, R.; Pecos-Martin, D.; Gallego-Izquierdo, T. Transcultural Adaptation of the Neck Disability Index to Mexican Spanish and Assessment of Its Psychometric Properties. Eur. Spine J. 2021, 30, 2654–2660. [Google Scholar] [CrossRef]
- Lim, H.H.R.; Tan, S.T.; Tang, Z.Y.; Yang, M.; Koh, E.Y.L.; Koh, K.H. Cross-Cultural Adaptation and Psychometric Evaluation of the Malay Version of the Neck Disability Index. Disabil. Rehabil. 2022, 44, 124–130. [Google Scholar] [CrossRef]
- Geete, D.B.; Mhatre, B.S.; Vernon, H. Cross-Cultural Adaptation and Psychometric Validation of the Hindi Version of the Neck Disability Index in Patients with Chronic Neck Pain. Spine 2023, 48, 1663–1669. [Google Scholar] [CrossRef]
- Lim, H.H.R.; Tang, Z.Y.; Hashim, M.A.B.M.; Yang, M.; Koh, E.Y.L.; Koh, K.H. Cross-Cultural Adaptation, Reliability, Validity, and Responsiveness of the Simplified-Chinese Version of Neck Disability Index. Spine 2020, 45, 541–548. [Google Scholar] [CrossRef]
- Shashua, A.; Geva, Y.; Levran, I. Translation, Validation, and Crosscultural Adaptation of the Hebrew Version of the Neck Disability Index. Spine 2016, 41, 1036–1040. [Google Scholar] [CrossRef]
- Farooq, M.N.; Naz, S.; Kousar, A.; Gul, A. Translation and Validation of the Urdu Version of the Neck Pain and Disability Scale. Disabil. Rehabil. 2024, 46, 2145–2154. [Google Scholar] [CrossRef] [PubMed]
- Lauridsen, H.H.; O’Neill, L.; Kongsted, A.; Hartvigsen, J. The Danish Neck Disability Index: New Insights into Factor Structure, Generalizability, and Responsiveness. Pain Pract. 2017, 17, 480–493. [Google Scholar] [CrossRef] [PubMed]
- Swanenburg, J.; Humphreys, K.; Langenfeld, A.; Brunner, F.; Wirth, B. Validity and reliability of a German version of the Neck Disability Index (NDI-G). Man. Ther. 2014, 19, 52–58. [Google Scholar] [CrossRef]
- Takeshita, K.; Oshima, Y.; Ono, T.; Kato, S.; Hosono, N.; Kawaguchi, Y.; Hasegawa, K.; Isomura, T.; Oshina, M.; Oda, T.; et al. Validity, reliability and responsiveness of the Japanese version of the Neck Disability Index. J. Orthop. Sci. 2013, 18, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Sidiq, M.; Ramachandran, A.; Janakiraman, B.; Kashoo, F.Z.; Chahal, A.; Singh, J.; Almotairi, Y.; Almotairi, A.A.; Miraj, M.; Ch, S.J.P.; et al. Adaption and psychometric evaluation of the Hindi version of Neck Disability Index in the rural population of Northern India: A cross-cultural study. F1000Res 2024, 12, 1599. [Google Scholar] [CrossRef]
- Jovicic, M.D.; Konstantinovic, L.M.; Grgurevic, A.D.; Milovanovic, N.D.; Trajkovic, G.; Jovicic, V.Z.; Dedic, S.I.K.; Hrkovic, M.K.; Draganac, S.M. Validation of the Neck Disability Index in Serbian patients with cervical radiculopathy. J. Manip. Physiol. Ther. 2018, 41, 496–502. [Google Scholar] [CrossRef]
- Jorritsma, W.; de Vries, G.E.; Dijkstra, P.U.; Geertzen, J.H.B.; Reneman, M.F. Neck Pain and Disability Scale and Neck Disability Index: Validity of Dutch language versions. Eur. Spine J. 2012, 21, 93–100. [Google Scholar] [CrossRef]
- Bicer, A.; Yazici, A.; Camdeviren, H.; Erdogan, C. Assessment of pain and disability in patients with chronic neck pain: Reliability and construct validity of the Turkish version of the Neck Pain and Disability Scale. Disabil. Rehabil. 2004, 26, 959–962. [Google Scholar] [CrossRef]
- Saltychev, M.; Pylkäs, K.; Karklins, A.; Juhola, J. Psychometric Properties of Neck Disability Index—A Systematic Review and Meta-Analysis. Disabil. Rehabil. 2024, 46, 5415–5431. [Google Scholar] [CrossRef]
- Wheeler, A.H.; Goolkasian, P.; Baird, A.C.; Darden, B.V. Development of the neck pain and disability scale. Item analysis, face, and criterion-related validity. Spine 1999, 24, 1290–1294. [Google Scholar] [CrossRef]
- Bolton, J.E.; Humphreys, B.K. The Bournemouth Questionnaire: A short-form comprehensive outcome measure. II. Psychometric properties in neck pain patients. J. Manip. Physiol. Ther. 2002, 25, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Wright, J.G.; Katz, J.N.; Upper Extremity Collaborative Group. Development of the QuickDASH: Comparison of three item-reduction approaches. J. Bone Jt. Surg. Am. 2005, 87, 1038–1046. [Google Scholar] [CrossRef] [PubMed]
- Tsang, S.; Royse, C.F.; Terkawi, A.S. Guidelines for Developing, Translating, and Validating a Questionnaire in Perioperative and Pain Medicine. Saudi J. Anaesth. 2017, 11 (Suppl. S1), S80–S89. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the Process of Cross-Cultural Adaptation of Self-Report Measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef]
- Kyriazos, T.A. Applied psychometrics: Sample size and sample power considerations in factor analysis (EFA, CFA) and SEM in general. Psychology 2018, 9, 2207–2230. [Google Scholar] [CrossRef]
- Khalifé, M.; Marie-Hardy, L.; Vafadar, S.; Pietton, R.; Duray, C.; Guigui, P.; Ferrero, E. Validation of the Total Disability Index (TDI) in French version. Orthop. Traumatol. Surg. Res. 2023, 109, 103311. [Google Scholar] [CrossRef]
- Yao, M.; Sun, Y.-L.; Cao, Z.-Y.; Dun, R.-L.; Yang, L.; Zhang, B.-M.; Jiang, H.-R.; Wang, Y.-J.; Cui, X.-J. A systematic review of crosscultural adaptation of the Neck Disability Index. Spine 2015, 40, 480–490. [Google Scholar] [CrossRef]
- Farooq, M.N.; Mohseni-Bandpei, M.A.; Gilani, S.A.; Khuwaja, F.M.; Ali, S.S. Urdu version of the Neck Disability Index: A reliability and validity study. BMC Musculoskelet. Disord. 2017, 18, 167. [Google Scholar] [CrossRef][Green Version]
- Corp, N.; Mansell, G.; Stynes, S.; Wynne-Jones, G.; Morsø, L.; Hill, J.C.; van der Windt, D.A. Evidence-based treatment recommendations for neck and low back pain across Europe: A systematic review of guidelines. Eur. J. Pain. 2021, 25, 275–295. [Google Scholar] [CrossRef]
- Wu, A.M.; Cross, M.; Elliott, J.M.; Culbreth, G.T.; Haile, L.M.; Steinmetz, J.D.; Hagins, H.; Kopec, J.A.; Brooks, P.M.; Woolf, A.D.; et al. Global, regional, and national burden of neck pain, 1990–2020, and projections to 2050: A systematic analysis of the Global Burden of Disease Study 2021. Lancet Rheumatol. 2024, 6, e142–e155. [Google Scholar] [CrossRef] [PubMed]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27 (Suppl. S6), 796–801. [Google Scholar] [CrossRef] [PubMed]
| NDI Language | Authors (Year) | Cronbach’s Alpha | ICC | Population |
|---|---|---|---|---|
| Mexican Spanish | Santiago-Reynoso et al. (2021) [6] | 0.91 | 0.97 | Chronic neck pain patients |
| Malay | Koh & Koh (2022) [7] | 0.89 | 0.96 | Multilingual urban population |
| Hindi | Geete et al. (2023) [8] | 0.9 | 0.96 | Indian patients with neck pain |
| Simplified Chinese | Yang et al. (2020) [9] | 0.88 | 0.93 | Chinese population |
| Hebrew | Shashua et al. (2016) [10] | 0.89 | 0.95 | Israeli patients |
| Urdu | Farooq et al. (2024) [11] | 0.88 | 0.93 | Pakistani patients |
| Danish | Lauridsen et al. (2017) [12] | 0.92 | 0.94 | General Danish population |
| German | Swanenburg et al. (2014) [13] | 0.92 | 0.96 | Rehabilitation patients |
| Japanese | Takeshita et al. (2013) [14] | 0.88 | 0.9 | Japanese patients with neck pain |
| Hindi (rural) | Sidiq et al. (2024) [15] | 0.91 | 0.94 | Rural population, northern India |
| Serbian | Jovicic et al. (2018) [16] | 0.88 | 0.95 | Cervical radiculopathy patients |
| Dutch | Jorritsma et al. (2012) [17] | 0.9 | 0.94 | Dutch-speaking patients |
| Turkish | Bicer et al. (2004) [18] | 0.88 | 0.93 | Turkish patients with chronic pain |
| Participants Characteristics | N | Mean | SD | |
|---|---|---|---|---|
| Age | 83 | 41.75 | 14.99 | |
| Weight | 83 | 72.43 | 14.09 | |
| Height | 83 | 171.41 | 8.81 | |
| Gender | Female | 47 | ||
| Male | 36 | |||
| Study level | Middle level | 2 | ||
| Higher graduation | 47 | |||
| Postgraduation | 30 | |||
| PhD | 4 | |||
| Profession | Economist | 14 | ||
| Student | 13 | |||
| Nurse | 7 | |||
| Retired | 7 | |||
| Secretary | 7 | |||
| Professor | 6 | |||
| Other | 36 | |||
| ANDI Section Analysis | Factor 1 |
|---|---|
| Kaiser–Meyer–Olkin Measure of Sampling Adequacy | 0.91 |
| Bartlett’s Test of Sphericity | 516.51 |
| Sig. | 0.00 |
| Section 1 | 0.86 |
| Section 2 | 0.87 |
| Section 3 | 0.96 |
| Section 4 | 0.90 |
| Section 5 | 0.91 |
| Section 6 | 0.80 |
| Section 7 | 0.82 |
| Section 8 | 0.77 |
| Section 9 | 0.87 |
| Section 10 | 0.75 |
| NDI | ANDI | 1st Measurement (N = 83) Mean ± SD | 2nd Measurement (N = 83) Mean ± SD | ICC | 95% CI | ITC | Cronbach’s Alpha |
|---|---|---|---|---|---|---|---|
| Section 1—PAIN INTENSITY | INTENSITETI I DHIMBJES | 1.72 ± 1.15 | 1.72 ± 1.06 | 0.98 | 0.97–0.99 | 0.96 | 0.96 |
| Section 2—PERSONAL CARE | KUJDESI PERSONAL | 1.54 ± 1.33 | 1.55 ± 1.29 | 0.99 | 0.97–0.99 | 0.98 | 0.96 |
| Section 3—LIFTING | NGRITJA | 1.63 ± 1.07 | 1.64 ± 0.98 | 0.95 | 0.93–0.97 | 0.91 | 0.96 |
| Section 4—READING | LEXIMI | 1.88 ± 1.07 | 1.87 ± 1.03 | 0.98 | 0.97–0.99 | 0.96 | 0.96 |
| Section 5—HEADACHES | DHIMBJA E KOKËS | 2.05 ± 1.14 | 2.01 ± 1.05 | 0.97 | 0.97–0.98 | 0.95 | 0.96 |
| Section 6—CONCENTRATION | PËRQËNDRIMI | 1.93 ± 1.23 | 1.82 ± 1.20 | 0.96 | 0.94–0.98 | 0.93 | 0.96 |
| Section 7—WORK | PUNA | 1.72 ± 1.27 | 1.70 ± 1.15 | 0.97 | 0.95–0.98 | 0.95 | 0.96 |
| Section 8—DRIVING | DREJTIMI I MAKINËS | 1.83 ± 1.32 | 1.83 ± 1.21 | 0.97 | 0.95–0.99 | 0.94 | 0.96 |
| Section 9—SLEEPING | GJUMI | 1.87 ± 1.28 | 1.80 ± 1.19 | 0.97 | 0.95–0.100 | 0.94 | 0.96 |
| Section 10—RECREATION | RECREACIONI | 1.78 ± 1.18 | 1.75 ± 1.06 | 0.97 | 0.95–0.98 | 0.94 | 0.96 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeqiri, E.; Qorri, E.; Todri, J.; Lena, O. Establishing the Neck Disability Index as a Valid Tool for Assessing Persistent Neck Pain in the Albanian Population. Medicina 2025, 61, 955. https://doi.org/10.3390/medicina61060955
Zeqiri E, Qorri E, Todri J, Lena O. Establishing the Neck Disability Index as a Valid Tool for Assessing Persistent Neck Pain in the Albanian Population. Medicina. 2025; 61(6):955. https://doi.org/10.3390/medicina61060955
Chicago/Turabian StyleZeqiri, Elda, Erda Qorri, Jasemin Todri, and Orges Lena. 2025. "Establishing the Neck Disability Index as a Valid Tool for Assessing Persistent Neck Pain in the Albanian Population" Medicina 61, no. 6: 955. https://doi.org/10.3390/medicina61060955
APA StyleZeqiri, E., Qorri, E., Todri, J., & Lena, O. (2025). Establishing the Neck Disability Index as a Valid Tool for Assessing Persistent Neck Pain in the Albanian Population. Medicina, 61(6), 955. https://doi.org/10.3390/medicina61060955






