Artificial Intelligence in Pediatric Orthopedics: A Comprehensive Review
Abstract
1. Introduction
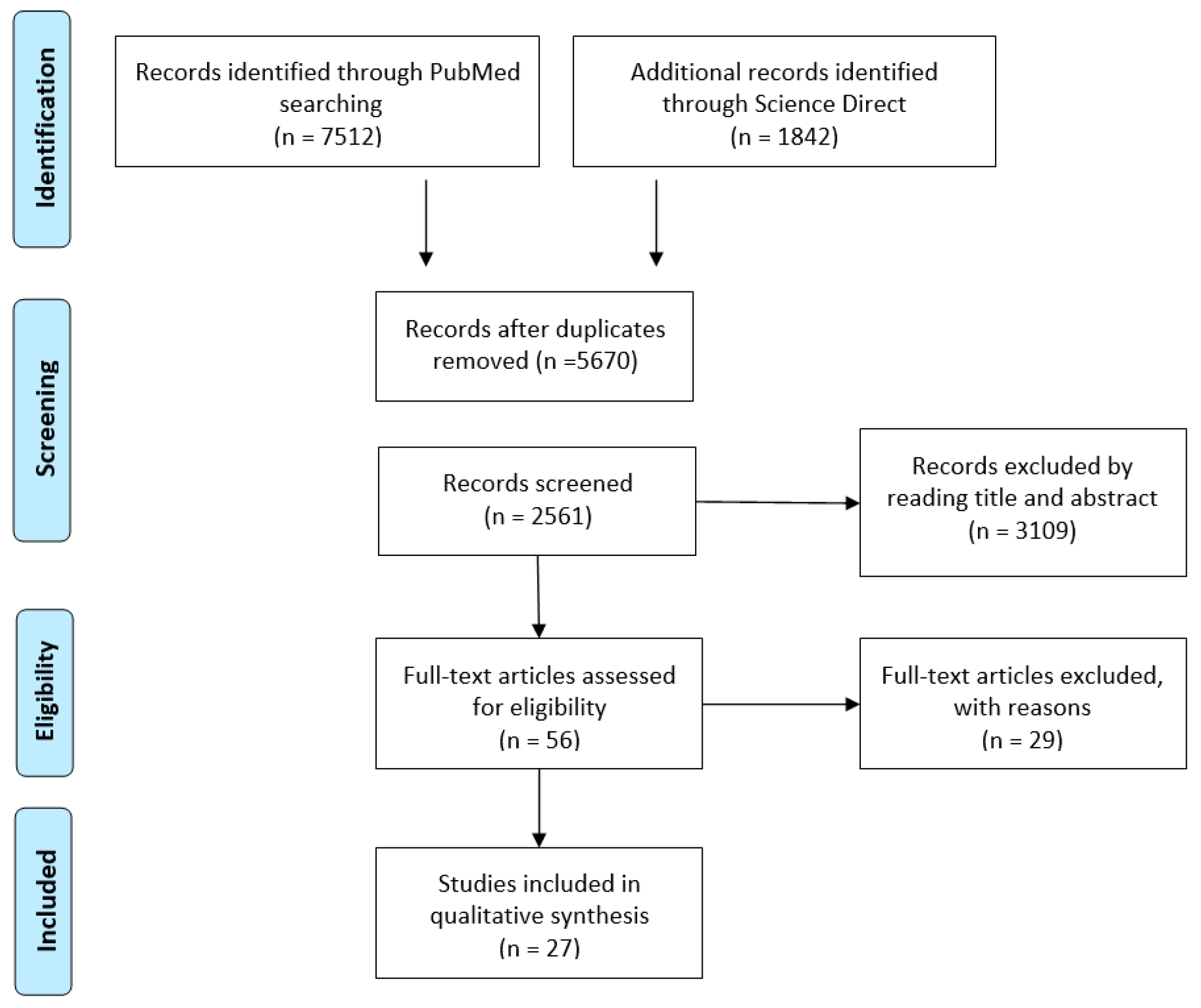
2. Materials and Methods
3. Results
3.1. Spine Deformities
3.2. Pediatric Hip Disorders
3.3. Pediatric Trauma
3.4. Bone Age Assessment
3.5. Leg Length Discrepancy
3.6. Other Pediatric Orthopedic Conditions
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Amisha; Malik, P.; Pathania, M.; Rathaur, V.K. Overview of Artificial Intelligence in Medicine. J. Family. Med. Prim. Care 2019, 8, 2328–2331. [Google Scholar] [CrossRef] [PubMed]
- Cui, Z.; Hung, A.J. Chapter 2—What Is Artificial Intelligence, Machine Learning, and Deep Learning: Terminologies Explained. In Artificial Intelligence in Urology; Hung, A.J., Ed.; Academic Press: Cambridge, MA, USA, 2025; pp. 3–17. ISBN 978-0-443-22132-3. [Google Scholar]
- Villarreal-Espinosa, J.B.; Berreta, R.S.; Allende, F.; Garcia, J.R.; Ayala, S.; Familiari, F.; Chahla, J. Accuracy Assessment of ChatGPT Responses to Frequently Asked Questions Regarding Anterior Cruciate Ligament Surgery. Knee 2024, 51, 84–92. [Google Scholar] [CrossRef]
- Miró Catalina, Q.; Vidal-Alaball, J.; Fuster-Casanovas, A.; Escalé-Besa, A.; Ruiz Comellas, A.; Solé-Casals, J. Real-World Testing of an Artificial Intelligence Algorithm for the Analysis of Chest X-Rays in Primary Care Settings. Sci. Rep. 2024, 14, 5199. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Nagahama, K.; Abe, Y.; Hyugaji, Y.; Ukeba, D.; Endo, T.; Ohnishi, T.; Ura, K.; Sudo, H.; Iwasaki, N.; et al. Evaluation of Surgical Indications for Full Endoscopic Discectomy at Lumbosacral Disc Levels Using Three-Dimensional Magnetic Resonance/Computed Tomography Fusion Images Created with Artificial Intelligence. Medicina 2023, 59, 860. [Google Scholar] [CrossRef]
- Popa, S.L.; Ismaiel, A.; Abenavoli, L.; Padureanu, A.M.; Dita, M.O.; Bolchis, R.; Munteanu, M.A.; Brata, V.D.; Pop, C.; Bosneag, A.; et al. Diagnosis of Liver Fibrosis Using Artificial Intelligence: A Systematic Review. Medicina 2023, 59, 992. [Google Scholar] [CrossRef]
- Nayarisseri, A.; Khandelwal, R.; Tanwar, P.; Madhavi, M.; Sharma, D.; Thakur, G.; Speck-Planche, A.; Singh, S.K. Artificial Intelligence, Big Data and Machine Learning Approaches in Precision Medicine & Drug Discovery. Curr. Drug Targets 2021, 22, 631–655. [Google Scholar]
- Rodriguez-Merchan, E.C. Some Artificial Intelligence Tools May Currently Be Useful in Orthopedic Surgery and Traumatology. World J. Orthop. 2025, 16, 102252. [Google Scholar] [CrossRef]
- Vaish, A.; Migliorini, F.; Vaishya, R. Artificial Intelligence in Foot and Ankle Surgery: Current Concepts. Orthopädie 2023, 52, 1011–1016. [Google Scholar] [CrossRef]
- Guan, J.; Li, Z.; Sheng, S.; Lin, Q.; Wang, S.; Wang, D.; Chen, X.; Su, J. An Artificial Intelligence-Driven Revolution in Orthopedic Surgery and Sports Medicine. Int. J. Surg. 2025, 111, 2162–2181. [Google Scholar] [CrossRef]
- Alomran, A.K.; Alomar, M.F.; Akhdher, A.A.; Qanber, A.R.A.; Albik, A.K.; Alumran, A.; Abdulwahab, A.H. Artificial Intelligence Awareness and Perceptions among Pediatric Orthopedic Surgeons: A Cross-Sectional Observational Study. World J. Orthop. 2024, 15, 1023–1035. [Google Scholar] [CrossRef]
- Mulford, K.L.; Regan, C.M.; Todderud, J.E.; Nolte, C.P.; Pinter, Z.; Chang-Chien, C.; Yan, S.; Wyles, C.; Khosravi, B.; Rouzrokh, P.; et al. Deep Learning Classification of Pediatric Spinal Radiographs for Use in Large Scale Imaging Registries. Spine Deform. 2024, 12, 1607–1614. [Google Scholar] [CrossRef]
- Chen, K.; Zhai, X.; Chen, Z.; Wang, H.; Yang, M.; Yang, C.; Bai, Y.; Li, M. Deep Learning Based Decision-Making and Outcome Prediction for Adolescent Idiopathic Scoliosis Patients with Posterior Surgery. Sci. Rep. 2025, 15, 3389. [Google Scholar] [CrossRef]
- Ghasseminia, S.; Lim, A.K.S.; Concepcion, N.D.P.; Kirschner, D.; Teo, Y.M.; Dulai, S.; Mabee, M.; Kernick, S.; Brockley, C.; Muljadi, S.; et al. Interobserver Variability of Hip Dysplasia Indices on Sweep Ultrasound for Novices, Experts, and Artificial Intelligence. J. Pediatr. Orthop. 2022, 42, e315–e323. [Google Scholar] [CrossRef]
- van der Lelij, T.J.N.; Grootjans, W.; Braamhaar, K.J.; de Witte, P.B. Automated Measurements of Long Leg Radiographs in Pediatric Patients: A Pilot Study to Evaluate an Artificial Intelligence-Based Algorithm. Children 2024, 11, 1182. [Google Scholar] [CrossRef]
- Zech, J.R.; Ezuma, C.O.; Patel, S.; Edwards, C.R.; Posner, R.; Hannon, E.; Williams, F.; Lala, S.V.; Ahmad, Z.Y.; Moy, M.P.; et al. Artificial Intelligence Improves Resident Detection of Pediatric and Young Adult Upper Extremity Fractures. Skelet. Radiol. 2024, 53, 2643–2651. [Google Scholar] [CrossRef]
- Fraiwan, M.; Audat, Z.; Fraiwan, L.; Manasreh, T. Using Deep Transfer Learning to Detect Scoliosis and Spondylolisthesis from X-Ray Images. PLoS ONE 2022, 17, e0267851. [Google Scholar] [CrossRef]
- Kavak, N.; Kavak, R.P.; Güngörer, B.; Turhan, B.; Kaymak, S.D.; Duman, E.; Çelik, S. Detecting Pediatric Appendicular Fractures Using Artificial Intelligence. Rev. Assoc. Med. Bras. 2024, 70, e20240523. [Google Scholar] [CrossRef]
- Parpaleix, A.; Parsy, C.; Cordari, M.; Mejdoubi, M. Assessment of a Combined Musculoskeletal and Chest Deep Learning-Based Detection Solution in an Emergency Setting. Eur. J. Radiol. Open 2023, 10, 100482. [Google Scholar] [CrossRef]
- Lv, Z.; Lv, W.; Wang, L.; Ou, J. Development and Validation of Machine Learning-Based Models for Prediction of Adolescent Idiopathic Scoliosis: A Retrospective Study. Medicine 2023, 102, e33441. [Google Scholar] [CrossRef]
- Tajmir, S.H.; Lee, H.; Shailam, R.; Gale, H.I.; Nguyen, J.C.; Westra, S.J.; Lim, R.; Yune, S.; Gee, M.S.; Do, S. Artificial Intelligence-Assisted Interpretation of Bone Age Radiographs Improves Accuracy and Decreases Variability. Skelet. Radiol. 2019, 48, 275–283. [Google Scholar] [CrossRef]
- Akal, F.; Batu, E.D.; Sonmez, H.E.; Karadağ, Ş.G.; Demir, F.; Ayaz, N.A.; Sözeri, B. Diagnosing Growing Pains in Children by Using Machine Learning: A Cross-Sectional Multicenter Study. Med. Biol. Eng. Comput. 2022, 60, 3601–3614. [Google Scholar] [CrossRef]
- Papillon, S.C.; Pennell, C.P.; Master, S.A.; Turner, E.M.; Arthur, L.G.; Grewal, H.; Aronoff, S.C. Derivation and Validation of a Machine Learning Algorithm for Predicting Venous Thromboembolism in Injured Children. J. Pediatr. Surg. 2023, 58, 1200–1205. [Google Scholar] [CrossRef]
- Rassmann, S.; Keller, A.; Skaf, K.; Hustinx, A.; Gausche, R.; Ibarra-Arrelano, M.A.; Hsieh, T.-C.; Madajieu, Y.E.D.; Nöthen, M.M.; Pfäffle, R.; et al. Deeplasia: Deep Learning for Bone Age Assessment Validated on Skeletal Dysplasias. Pediatr. Radiol. 2024, 54, 82–95. [Google Scholar] [CrossRef]
- Zheng, Q.; Shellikeri, S.; Huang, H.; Hwang, M.; Sze, R.W. Deep Learning Measurement of Leg Length Discrepancy in Children Based on Radiographs. Radiology 2020, 296, 152–158. [Google Scholar] [CrossRef]
- Kim, M.J.; Choi, Y.H.; Lee, S.B.; Cho, Y.J.; Lee, S.H.; Shin, C.H.; Shin, S.-M.; Cheon, J.-E. Development and Evaluation of Deep-Learning Measurement of Leg Length Discrepancy: Bilateral Iliac Crest Height Difference Measurement. Pediatr. Radiol. 2022, 52, 2197–2205. [Google Scholar] [CrossRef]
- Kabir, M.H.; Reformat, M.; Hryniuk, S.S.; Stampe, K.; Lou, E. Validity of Machine Learning Algorithms for Automatically Extract Growing Rod Length on Radiographs in Children with Early-Onset Scoliosis. Med. Biol. Eng. Comput. 2025, 63, 101–110. [Google Scholar] [CrossRef]
- Wu, Q.; Ma, H.; Sun, J.; Liu, C.; Fang, J.; Xie, H.; Zhang, S. Application of Deep-Learning–Based Artificial Intelligence in Acetabular Index Measurement. Front. Pediatr. 2023, 10, 1049575. [Google Scholar] [CrossRef]
- Hou, T.; An, D.; Hicks, C.W.; Haut, E.; Nasr, I.W. Using Supervised Machine Learning and ICD10 to Identify Non-Accidental Trauma in Pediatric Trauma Patients in the Maryland Health Services Cost Review Commission Dataset. Child Abus. Negl. 2025, 160, 107228. [Google Scholar] [CrossRef]
- Shelmerdine, S.C.; Pauling, C.; Allan, E.; Langan, D.; Ashworth, E.; Yung, K.W.; Barber, J.; Haque, S.; Rosewarne, D.; Woznitza, N.; et al. Artificial intelligence (AI) for paediatric fracture detection: A multireader multicase (MRMC) study protocol. BMJ Open 2024, 14, e084448. [Google Scholar] [CrossRef] [PubMed]
- Binh, L.N.; Nhu, N.T.; Vy, V.P.T.; Son, D.L.H.; Hung, T.N.K.; Bach, N.; Huy, H.Q.; Tuan, L.V.; Le, N.Q.K.; Kang, J.-H. Multi-Class Deep Learning Model for Detecting Pediatric Distal Forearm Fractures Based on the AO/OTA Classification. J. Digit. Imaging Inform. Med. 2024, 37, 725–733. [Google Scholar] [CrossRef]
- Yao, W.; Wang, Y.; Zhao, X.; He, M.; Wang, Q.; Liu, H.; Zhao, J. Automatic Diagnosis of Pediatric Supracondylar Humerus Fractures Using Radiomics-Based Machine Learning. Medicine 2024, 103, e38503. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Zhu, C.; Zhao, Y.; Zhao, M.; Wang, Z.; Song, R.; Meng, N.; Sial, A.; Diwan, A.; Liu, J.; et al. Deep Learning Model to Classify and Monitor Idiopathic Scoliosis in Adolescents Using a Single Smartphone Photograph. JAMA Netw. Open 2023, 6, e2330617. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.-C.; Sun, J.; Liu, C.-B.; Fang, J.-H.; Xie, H.-T.; Ning, B. Clinical Application of Artificial Intelligence-Assisted Diagnosis Using Anteroposterior Pelvic Radiographs in Children with Developmental Dysplasia of the Hip. Bone Jt. J. 2020, 102-B, 1574–1581. [Google Scholar] [CrossRef]
- Zech, J.R.; Santos, L.; Staffa, S.; Zurakowski, D.; Rosenwasser, K.A.; Tsai, A.; Jaramillo, D. Lower Extremity Growth According to AI Automated Femorotibial Length Measurement on Slot-Scanning Radiographs in Pediatric Patients. Radiology 2024, 311, e231055. [Google Scholar] [CrossRef]
- Negrini, F.; Cina, A.; Ferrario, I.; Zaina, F.; Donzelli, S.; Galbusera, F.; Negrini, S. Developing a New Tool for Scoliosis Screening in a Tertiary Specialistic Setting Using Artificial Intelligence: A Retrospective Study on 10,813 Patients: 2023 SOSORT Award Winner. Eur. Spine J. 2023, 32, 3836–3845. [Google Scholar] [CrossRef]
- Xu, W.; Shu, L.; Gong, P.; Huang, C.; Xu, J.; Zhao, J.; Shu, Q.; Zhu, M.; Qi, G.; Zhao, G.; et al. A Deep-Learning Aided Diagnostic System in Assessing Developmental Dysplasia of the Hip on Pediatric Pelvic Radiographs. Front. Pediatr. 2021, 9, 785480. [Google Scholar] [CrossRef]
- Gstoettner, M.; Sekyra, K.; Walochnik, N.; Winter, P.; Wachter, R.; Bach, C.M. Inter- and Intraobserver Reliability Assessment of the Cobb Angle: Manual versus Digital Measurement Tools. Eur. Spine J. 2007, 16, 1587–1592. [Google Scholar] [CrossRef]
- Manzetti, M.; Ruffilli, A.; Barile, F.; Viroli, G.; Traversari, M.; Vita, F.; Cerasoli, T.; Arceri, A.; Artioli, E.; Mazzotti, A.; et al. Is There a Skeletal Age Index That Can Predict Accurate Curve Progression in Adolescent Idiopathic Scoliosis? A Systematic Review. Pediatr. Radiol. 2024, 54, 299–315. [Google Scholar] [CrossRef]
- Lenz, M.; Oikonomidis, S.; Harland, A.; Fürnstahl, P.; Farshad, M.; Bredow, J.; Eysel, P.; Scheyerer, M.J. Scoliosis and Prognosis—A Systematic Review Regarding Patient-Specific and Radiological Predictive Factors for Curve Progression. Eur. Spine J. 2021, 30, 1813–1822. [Google Scholar] [CrossRef]
- Pandey, R.A.; Johari, A.N. Screening of Newborns and Infants for Developmental Dysplasia of the Hip: A Systematic Review. Indian J. Orthop. 2021, 55, 1388–1401. [Google Scholar] [CrossRef]
- Kilsdonk, I.; Witbreuk, M.; Van Der Woude, H.-J. Ultrasound of the Neonatal Hip as a Screening Tool for DDH: How to Screen and Differences in Screening Programs between European Countries. J. Ultrason. 2021, 21, e147–e153. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.G.; Ossendorff, R.; Yagdiran, A.; Hockmann, J.; Bornemann, R.; Placzek, S. Four Decades of Developmental Dysplastic Hip Screening According to Graf: What Have We Learned? Front. Pediatr. 2022, 10, 990806. [Google Scholar] [CrossRef] [PubMed]
- Peterson, H. Growing Pains. Pediatr. Clin. N. Am. 1986, 33, 1365–1372. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Valenti, F.; Sapienza, M.; Sessa, G.; Testa, G. Growing Pains: What Do We Know about Etiology? A Systematic Review. World J. Orthop. 2019, 10, 192–205. [Google Scholar] [CrossRef]
- Pavone, V.; Vescio, A.; Lucenti, L.; Amico, M.; Caldaci, A.; Pappalardo, X.G.; Parano, E.; Testa, G. Diagnostic Tools in the Detection of Physical Child Abuse: A Systematic Review. Children 2022, 9, 1257. [Google Scholar] [CrossRef]
- Umapathy, V.R.; Rajinikanth, B.S.; Samuel Raj, R.D.; Yadav, S.; Munavarah, S.A.; Anandapandian, P.A.; Mary, A.V.; Padmavathy, K.; Akshay, R. Perspective of Artificial Intelligence in Disease Diagnosis: A Review of Current and Future Endeavours in the Medical Field. Cureus 2023, 15, e45684. [Google Scholar] [CrossRef]
- Kamal, A.H.; Zakaria, O.M.; Majzoub, R.A.; Nasir, E.W.F. Artificial Intelligence in Orthopedics: A Qualitative Exploration of the Surgeon Perspective. Medicine 2023, 102, e34071. [Google Scholar] [CrossRef]
- Luo, S.; Deng, L.; Chen, Y.; Zhou, W.; Canavese, F.; Li, L. Revolutionizing Pediatric Orthopedics: GPT-4, a Groundbreaking Innovation or Just a Fleeting Trend? Int. J. Surg. 2023, 109, 3694–3697. [Google Scholar] [CrossRef]
- Leng, L. Challenge, Integration, and Change: ChatGPT and Future Anatomical Education. Med. Educ. Online 2024, 29, 2304973. [Google Scholar] [CrossRef]
- van Dis, E.A.M.; Bollen, J.; Zuidema, W.; van Rooij, R.; Bockting, C.L. ChatGPT: Five Priorities for Research. Nature 2023, 614, 224–226. [Google Scholar] [CrossRef]
| # | Authors (Year) | Medical Condition | AI | Population | Results |
|---|---|---|---|---|---|
| 1 | van der Lelij, T. J. N. et al. (2024) [15] | LLD | ML | 58 legs | 76% of the cases for LLD measurements, 88% for FLL and femur length, 91% for mLDFA, 97% for HKA, 98% for mMPTA, and 100% for tibia length. |
| 2 | Zech JR et al. (2024) [16] | Trauma | DL | 240 upper extremity fractures | AUC varying between 0.876 ([0.845–0.908, p < 0.001) and 0.844 ([0.805–0.883] with AI, p < 0.001) |
| 3 | Fraiwan M et al. (2022) [17] | AIS and SPL | DL | 338 patients | accuracy for three-class classification varying between 96.73% and 98.02% |
| 4 | Kavak N. et al. (2024) [18] | Trauma | CNN | 5150 radiographs | accuracy varying between 93 and 95% in detecting fractures |
| 5 | Parpaleix A et al. (2023) [19] | Trauma | DL | 1772 patients, musculoskeletal and chest detection | Accuracy was 90.1% |
| 6 | Lv Z et al. (2023) [20] | AIS | ML | 1581 patients | AUC: 0.767–0.899 |
| 7 | Tajmir SH et al. (2019) [21] | BAA | ML | 280 patients | Accuracy was 68.2% overall and 98.6% within 1 year. |
| 8 | Akal F et al. (2022) [22] | GP | ML | 398 patients | 0.99 sensitivity, 0.97 specificity, 0.98 accuracy, |
| 9 | Papillon SC et al. (2023) [23] | VTE | ML | 383,814 Patients | Baseline rate of VTE (0.15%) with a predicted rate of 0.01–0.02% and 1.13–1.32% for low and high risk, respectively |
| 10 | Rassmann S et al. (2024) [24] | BAA | CNN | 568 radiographs from 189 patients with molecularly confirmed diagnoses of seven different genetic bone disorders | 98.5% accuracy on the test set of the Radiological Society of North America |
| 11 | Zheng Q et al. (2020) [25] | LLD | DL | 179 patients | (Dice similarity coefficient, 0.94). Mean absolute error ([MAE], 0.45 cm), full pediatric leg lengths (r = 0.99; MAE, 0.45 cm), and full LLD (r = 0.92; MAE, 0.51 cm) |
| 12 | Kim MJ et al. (2022) [26] | LLD | DL | 300 patients | Interclass correlations (ICCs) ranged from 0.914 to 0.997. The mean absolute error was 2.3 ± 5.2 mm. |
| 13 | Mulford et al. (2024) [12] | AIS | DL | 7777 AP images and 5621 lateral images | Precision ranged from 0.98 to 1.00 in the AP images, and from 0.91 to 1.00 on the lateral images for classification of pediatric spinal disorders. |
| 14 | Kabir, M. H. et al. (2025) [27] | EOS | DL | 387 patients | Average precision (AP) varying between 67.6% and 94.8%. The MAD ± SD of the rod length change was 0.98 ± 0.88 mm, and the ICC was 0.90 between the manual and artificial intelligence (AI) adjustment measurements. |
| 15 | Chen, K. et al. (2025) [13] | AIS | DL | 425 patients | Mean square error of 2.77 × 10−5 and an average absolute error of 0.00350 on the validation set |
| 17 | Wu, Q. et al. (2023) [28] | HIP | DL | 1000 patients | The 95% limits of agreement (95% LOA) of the system were −0.93° to 2.86° (bias = −0.03°, p = 0.647). |
| 18 | Hou, T. et al. (2025) [29] | NAT | ML | 364,217 patients | Confirmed NAT specificity 99.94, sensitivity 36.59, Suspected NAT specificity 99.93, sensitivity 70.12 |
| 19 | Shelmerdine, S. C. et al. (2024) [30] | Trauma | ML | 500 patients | Protocol aims for 92% accuracy in pediatric fracture detection. |
| 20 | Binh, L. N. et al. (2024) [31] | Trauma | DL | An 88-image distal forearm fracture dataset | 92% accuracy in distal forearm fracture detection. |
| 21 | Yao, W. et al. (2024) [32] | Trauma | ML | 411 supracondylar humerus fractures | The area under the curve (AUC) of anteroposterior and lateral elbow radiographs is 0.65 and 0.72. |
| 22 | Zhang et al. (2023) [33] | AIS | DL | 2158 patients | Sensitivity 84.88% (75.54–91.70), negative predictive value 89.22% (84.25–93.70), specificity 67.44% (59.89–74.38), positive predictive value 56.59 (50.81–62.20), accuracy 73.26% (67.41–78.56) |
| 23 | Zhang, S. C. et al. (2020) [34] | HIP | DL | 1138 patients grouped according to age and into ‘dislocation’ and ‘non-dislocation’ | Sensitivity 95.5% and specificity 99.5% for dislocation. Bland–Altman 95% limits of agreement for acetabular index, non-dislocated and dislocated hips were −3.27–2.94° and −7.36–5.36°, respectively (p < 0.001). |
| 24 | Ghasseminia et al. (2022) [14] | HIP | ML | 240 hips | AI versus subspecialists (ICC = 0.87 for sweeps, 0.90 for single images) |
| 25 | Zech JR et al. (2024) [35] | LLD | CNN | 523 patients | Absolute errors of AI measurements of the femur, tibia, and lower extremity in the test data set were 0.25, 0.27, and 0.33 cm, respectively |
| 26 | Negrini et al. (2023) [36] | AIS | ML | 10,813 patients | Accuracies of 74, 81, 79, 79, and 84% for 15-, 20-, 25-, 30- and 40-degree thresholds for predicting AIS evolution |
| 27 | Xu W. et al. (2022) [37] | HIP | CNN | 1398 x-rays | Tönnis and International Hip Dysplasia Institute (IHDI) classification accuracies for both hips ranged from 0.86 to 0.95 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vescio, A.; Testa, G.; Sapienza, M.; Familiari, F.; Mercurio, M.; Gasparini, G.; de Salvatore, S.; Donati, F.; Canavese, F.; Pavone, V. Artificial Intelligence in Pediatric Orthopedics: A Comprehensive Review. Medicina 2025, 61, 954. https://doi.org/10.3390/medicina61060954
Vescio A, Testa G, Sapienza M, Familiari F, Mercurio M, Gasparini G, de Salvatore S, Donati F, Canavese F, Pavone V. Artificial Intelligence in Pediatric Orthopedics: A Comprehensive Review. Medicina. 2025; 61(6):954. https://doi.org/10.3390/medicina61060954
Chicago/Turabian StyleVescio, Andrea, Gianluca Testa, Marco Sapienza, Filippo Familiari, Michele Mercurio, Giorgio Gasparini, Sergio de Salvatore, Fabrizio Donati, Federico Canavese, and Vito Pavone. 2025. "Artificial Intelligence in Pediatric Orthopedics: A Comprehensive Review" Medicina 61, no. 6: 954. https://doi.org/10.3390/medicina61060954
APA StyleVescio, A., Testa, G., Sapienza, M., Familiari, F., Mercurio, M., Gasparini, G., de Salvatore, S., Donati, F., Canavese, F., & Pavone, V. (2025). Artificial Intelligence in Pediatric Orthopedics: A Comprehensive Review. Medicina, 61(6), 954. https://doi.org/10.3390/medicina61060954












