Does Position Affect Reduction? Comparison of the Effects of Three Different Positions on Reduction in Intertrochanteric Femur Fracture Nailing
Abstract
:1. Introduction
2. Materials and Methods
- Operation with Supine Position Assisted by Traction Table
- Operation in Lateral Decubitus Position
- Operation in Supine Position
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DAP | Anterior–posterior distance |
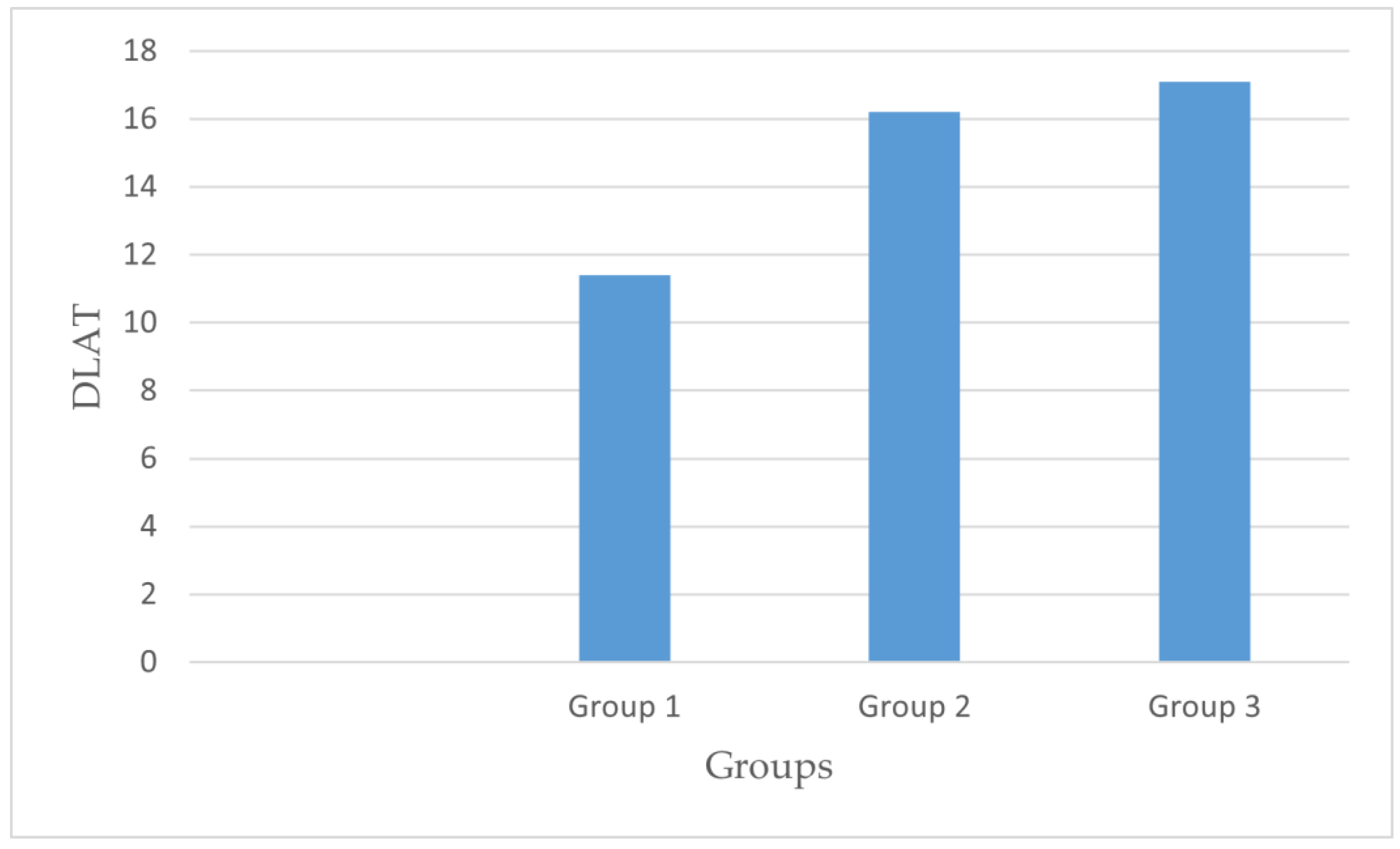
| DLAT | Lateral distance |
| PFN | Proximal femoral nail |
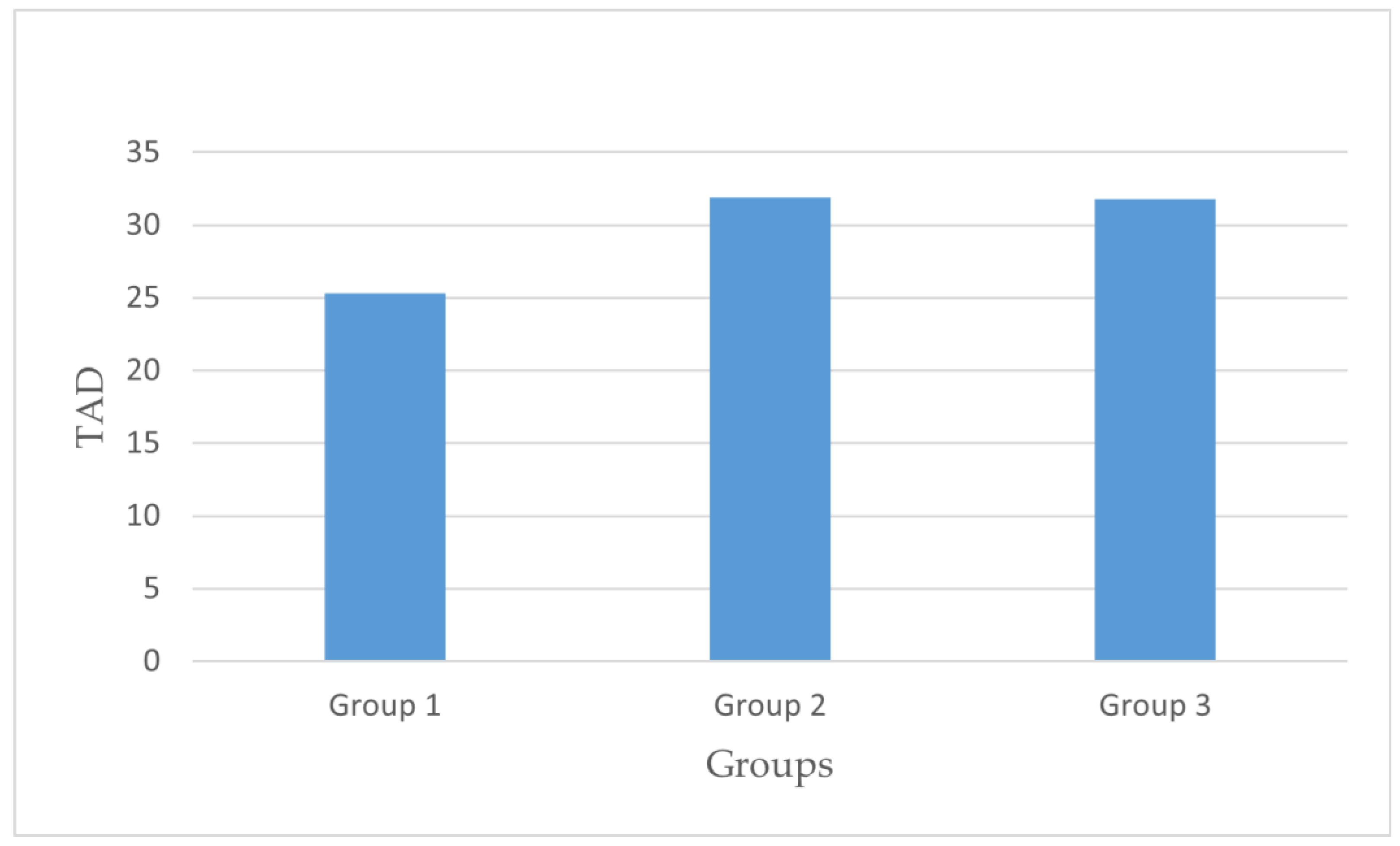
| TAD | Tip–apex distance |
References
- Jonnes, C.; Sm, S.; Najimudeen, S. Type II Intertrochanteric Fractures: Proximal Femoral Nailing (PFN) Versus Dynamic Hip Screw (DHS). Arch. Bone Jt. Surg. 2016, 4, 23–28. [Google Scholar] [PubMed]
- Jones, H.W.; Johnston, P.; Parker, M. Are short femoral nails superior to the sliding hip screw? A. meta-analysis of 24 studies involving 3,279 fractures. Int. Orthop. 2006, 30, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Turgut, A.; Kalenderer, Ö.; Günaydın, B.; Önvural, B.; Karapınar, L.; Ağuş, H. Fixation of intertrochanteric femur fractures using Proximal Femoral Nail Antirotation (PFNA) in the lateral decubitus position without a traction table. Acta Orthop. Traumatol. Turc. 2014, 48, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Ozkan, K.; Unay, K.; Demircay, C.; Cakir, M.; Eceviz, E. Distal unlocked proximal femoral intramedullary nailing for intertrochanteric femur fractures. Int. Orthop. 2009, 33, 1397–1400. [Google Scholar] [CrossRef]
- Connelly, C.L.; Archdeacon, M.T. The lateral decubitus approach for complex proximal femur fractures: Anatomic reduction and locking plate neutralization: A technical trick. J. Orthop. Trauma. 2012, 26, 252–257. [Google Scholar] [CrossRef]
- Bishop, J.A.; Rodriguez, E.K. Closed intramedullary nailing of the femur in the lateral decubitus position. J. Trauma. 2010, 68, 231–235. [Google Scholar] [CrossRef]
- Stephen, D.J.; Kreder, H.J.; Schemitsch, E.H.; Conlan, L.B.; Wild, L.; McKee, M.D. Femoral intramedullary nailing: Comparison of fracture-table and manual traction. a prospective; randomized study. J. Bone Jt. Surg. Am. 2002, 84, 1514–1521. [Google Scholar] [CrossRef]
- Saini, R.; Jain, M.; Shah, S.; Shah, N. Significance of tip apex distance (tad) in proximal femoral nail antirotation (pfna) II system used in trauma cases of proximal femoral fractures. Int. J. Orthop. Traumatol. Surg. Sci. 2019, 5, 296–299. [Google Scholar] [CrossRef]
- Tahir, A.; Hassan, A.W.; Umar, I.M. A study of the collodiaphyseal angle of the femur in the North-Eastern Sub-Region of Nigeria. Niger J. Med. 2001, 10, 34–36. [Google Scholar]
- Li, F.; Fisher, K.J.; Bauman, A.; Ory, M.G.; Chodzko-Zajko, W.; Harmer, P.; Bosworth, M.; Cleveland, M. Neighborhood influences on physical activity in middle-aged and older adults: A multilevel perspective. J. Aging Phys. Act. 2005, 13, 87–114. [Google Scholar] [CrossRef]
- Ikuta, Y.; Nagata, Y.; Iwasaki, Y. Preoperative radiographic features of trochanteric fractures irreducible by closed reduction. Injury 2019, 50, 2014–2021. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Solberg, B.D. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. J. Bone Jt. Surg. Br. 1997, 79, 969–971. [Google Scholar] [CrossRef]
- Baumgaertner, M.R.; Curtin, S.L.; Lindskog, D.M.; Keggi, J.M. The value of the tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J. Bone Joint Surg. Am. 1995, 77, 1058–1064. [Google Scholar] [CrossRef]
- Kakumanu, R.K.; Kunadharaju, R.T.; Beesetty, M.; Golla, D. Ease of doing proximal femoral nailing in lateral position in the management of peri-trochanteric femoral fractures in adults: A prospective study. Int. J. Orthop. 2019, 5, 39–46. [Google Scholar] [CrossRef]
- Chaudhary, D. The Proximal Femoral Nail-A. Minimal Invasive Treatment for the Stabilization of Pertrochanteric and Subtrochanteric Femoral Fractures. JK Sci. 2012, 14, 120–124. [Google Scholar]
- Souza, E.F.; Hungria, J.O.; Rezende, L.R.; Bellan, D.G.; Borracini, J.A. Comparative Study between Lateral Decubitus and Traction Table for Treatment of Pertrochanteric Fractures with Cephalomedullary Nails. Rev. Bras. Ortop. 2016, 52, 24–28. [Google Scholar] [CrossRef] [PubMed]
- Liu, Z.; Wang, H.; Wu, H.; Pan, L.; Ning, T.; Cao, Y. Reduction Quality in Lateral View of X-ray and Hypoalbuminemia Are Associated with Postoperative Mortality in Elderly Pertrochanteric Fracture Patients. Quant. Imaging Med. Surg. 2023, 13, 7247–7257. [Google Scholar] [CrossRef]
- Kozono, N.; Ikemura, S.; Yamashita, A.; Harada, T.; Watanabe, T.; Shirasawa, K. Direct Reduction May Need to Be Considered to Avoid Postoperative Subtype P in Patients with an Unstable Trochanteric Fracture: A Retrospective Study Using a Multivariate Analysis. Arch. Orthop. Trauma Surg. 2014, 134, 1649–1654. [Google Scholar] [CrossRef]
- Tsukada, S.; Okumura, G.; Matsueda, M. Postoperative Stability on Lateral Radiographs in the Surgical Treatment of Pertrochanteric Hip Fractures. Arch. Orthop. Trauma Surg. 2012, 132, 839–846. [Google Scholar] [CrossRef]
- Takigawa, N.; Moriuchi, H.; Abe, M.; Yasui, K.; Eshiro, H.; Kinoshita, M. Complications and Fixation Techniques of Trochanteric Fractures with the TARGON(®) PF. Injury 2014, 45 (Suppl. S1), S44–S48. [Google Scholar] [CrossRef]
- Takigami, I.; Matsumoto, K.; Ohara, A.; Yamanaka, K.; Naganawa, T.; Ohashi, M.; Date, K.; Shimizu, K. Treatment of trochanteric fractures with the PFNA (proximal femoral nail antirotation) nail system—Report of early results. Bull. NYU Hosp. Jt. Dis. 2008, 66, 276–279. [Google Scholar] [PubMed]
- Saraf, H.; Munot, S. Comparative study of PFN antirotation vs bipolar hemiarthroplasty in unstable senile intertrochanteric fractures. Indian J. Orthop. Surg. 2023, 4, 380–385. [Google Scholar]
- Li, X.; Zhang, L.; Hou, Z.; Meng, Z.; Chen, W.; Wang, P.; Zhang, Y. Distal locked and unlocked nailing for perthrochanteric fractures—A prospective comparative randomized study. Int. Orthop. 2015, 39, 1645–1652. [Google Scholar] [CrossRef]
- Yam, M.; Chawla, A.; Kwek, E. Rewriting the Tip Apex Distance for the Proximal Femoral Nail Anti-Rotation. Injury 2017, 48, 1843–1847. [Google Scholar] [CrossRef] [PubMed]
- Mereddy, P.; Kamath, S.; Ramakrishnan, M.; Malik, H.; Donnachie, N. The AO/ASIF proximal femoral nail antirotation (PFNA): A new design for the treatment of unstable proximal femoral fractures. Injury 2009, 40, 428–432. [Google Scholar] [CrossRef] [PubMed]
- Penzkofer, J.; Mendel, T.; Bauer, C.; Brehme, K.J.D.U. Treatment results of pertrochanteric and subtrochanteric femoral fractures: A retrospective comparison of PFN and PFNA. Der Unfallchirurg 2009, 112, 699–705. [Google Scholar] [CrossRef]
- Geller, J.A.; Saifi, C.; Morrison, T.A.; Macaulay, W. Tip-apex distance of intramedullary devices as a predictor of cut-out failure in the treatment of peritrochanteric elderly hip fractures. Int. Orthop. 2010, 34, 719–722. [Google Scholar] [CrossRef]
- Duramaz, A.; İlter, M.H. The impact of proximal femoral nail type on clinical and radiological outcomes in the treatment of intertrochanteric femur fractures: A comparative study. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 1441–1449. [Google Scholar] [CrossRef]
- Fisher, N.D.; Parola, R.; Anil, U.; Herbosa, C.; Boadi, B.; Ganta, A.; Tejwani, N.; Konda, S.R.; Egol, K.A. A Good Tip-Apex Distance Does Not Make Up For a Poor Reduction in Intertrochanteric Hip Fractures Treated with a Cephalomedullary Nail: The Utility of the Neck-Shaft Angle in Preventing Fixation Failure. J. Am. Acad. Orthop. Surg. 2024, 32, 83–91. [Google Scholar] [CrossRef]
- Yu, W.; Zhang, X.; Zhu, X.; Hu, J.; Liu, Y. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J. Orthop. Surg. Res. 2016, 11, 10. [Google Scholar] [CrossRef]
- Radaideh, A.M.; Qudah, H.A.; Audat, Z.A.; Jahmani, R.A.; Yousef, I.R.; Saleh, A.A.A. Functional and Radiological Results of Proximal Femoral Nail Antirotation (PFNA) Osteosynthesis in the Treatment of Unstable Pertrochanteric Fractures. J. Clin Med. 2018, 7, 78. [Google Scholar] [CrossRef] [PubMed]
- Mahaisavariya, C.; Pradhan, N.; Riansuwan, K.; Tharmviboonsri, T.; Rugpolmuang, L.; Mahaisavariya, B.; Tantigate, D. Risk factor of proximal lag screw cut-out after cephalomedullary nail fixation in trochanteric femoral fractures: A retrospective analytic study. Siriraj Med. J. 2022, 74, 627–633. [Google Scholar] [CrossRef]
- Kumar, P.M.; Madhav, A. Does the traditional tip-apex distance hold good for PFN-A.? Eur. J. Mol. Clin. Med. 2022, 9, 909–924. [Google Scholar]
- Fogagnolo, F.; Kfuri, M.; Paccola, C.A. Intramedullary fixation of pertrochanteric hip fractures with the short AO-ASIF proximal femoral nail. Arch. Orthop. Trauma Surg. 2004, 124, 31–37. [Google Scholar] [CrossRef]
- Hwang, S.W.; Gressot, L.V.; Chern, J.J.; Relyea, K.; Jea, A. Complications of occipital screw placement for occipitocervical fusion in children. J. Neurosurg. Pediatr. 2012, 9, 586–593. [Google Scholar] [CrossRef]
- Parker, M.J.; Palmer, C.R. A new mobility score for predicting mortality after hip fracture. J. Bone Jt. Surg. Br. 1993, 75, 797–798. [Google Scholar] [CrossRef]
- Abulsoud, M.I.; Ibrahim, M.A.A.; Mohammed, A.S.; Elmarghany, M.; Gaber, U.; Elsherbiny, E.A.; Nematallah, S.A.; Mohamed, M.A.; Elhalawany, M.F.; Hasanien, Y.A.; et al. Proximal femoral nailing for unstable trochanteric fractures: Lateral decubitus position or traction table? A case-control study of 96 patients. SICOT J. 2024, 10, 47. [Google Scholar] [CrossRef]
- Güran, O.; Gencer, B. Three Different Surgical Positions on Radiological Outcomes in the Proximal Femoral Nail: Supine, Lateral Decubitus and Traction Table. Eur. Rev. Med. Pharmacol. Sci. 2024, 28, 1384–1391. [Google Scholar]



| Group I | Group II | Group III | p | ||
|---|---|---|---|---|---|
| AO classification | 31A1: | 24 (33.8) | 20 (40.8) | 13 (35.1) | 0.102 |
| 31A2: | 35 (49.3) | 19 (38.8) | 23 (62.2) | ||
| 31A3: | 12 (16.9) | 11 (20.4) | 1 (2.7) | ||
| Modified Baumgaertner classification | Acceptable | 24 (33.8) | 18 (36.7) | 10 (27) | 0.420 |
| Good | 45 (63.4) | 29 (59.2) | 23 (62.2) | ||
| Bad | 2 (2.8) | 2 (4.1) | 4 (10.8) | ||
| Ikuta classification | Subtype N | 46 (64.8) | 34 (69.4) | 24 (64.9) | 0.879 |
| Subtype P | 12 (16.9) | 9 (18.4) | 8 (21.6) | ||
| Subtype A | 13 (18.3) | 6 (12.2) | 5 (13.5) | ||
| Group I | Group II | Group III | p | |
|---|---|---|---|---|
| DAP | 13.88 ± 4.48 | 15.72 ± 5.68 | 15.20 ± 6.72 | 0.156 |
| DLAT | 11.43 ± 4.10 | 16.21 ± 7.08 | 17.11 ± 6.30 | 0.000 |
| TAD | 25.31 ± 6.62 | 31.91 ± 11.32 | 31.79 ± 11.14 | 0.000 |
| Collodiaphyseal angle | 130.72 ± 6.38 | 130.29 ± 8.04 | 124.19 ± 6.41 | 0.000 |
| Group I | Group II | Group III | p | |
|---|---|---|---|---|
| Lag screw length | 97.21 ± 6.11 | 89.59 ± 7.06 | 93.78 ± 6.50 | 0.000 |
| Compression screw length | 92.18 ± 6.37 | 85 ± 6.9 | 88.78 ± 6.50 | 0.000 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okumuş, N.; Aydemir, A.N. Does Position Affect Reduction? Comparison of the Effects of Three Different Positions on Reduction in Intertrochanteric Femur Fracture Nailing. Medicina 2025, 61, 1005. https://doi.org/10.3390/medicina61061005
Okumuş N, Aydemir AN. Does Position Affect Reduction? Comparison of the Effects of Three Different Positions on Reduction in Intertrochanteric Femur Fracture Nailing. Medicina. 2025; 61(6):1005. https://doi.org/10.3390/medicina61061005
Chicago/Turabian StyleOkumuş, Nezir, and Ahmet Nadir Aydemir. 2025. "Does Position Affect Reduction? Comparison of the Effects of Three Different Positions on Reduction in Intertrochanteric Femur Fracture Nailing" Medicina 61, no. 6: 1005. https://doi.org/10.3390/medicina61061005
APA StyleOkumuş, N., & Aydemir, A. N. (2025). Does Position Affect Reduction? Comparison of the Effects of Three Different Positions on Reduction in Intertrochanteric Femur Fracture Nailing. Medicina, 61(6), 1005. https://doi.org/10.3390/medicina61061005





