Sex Differences in Epicardial Adipose Tissue and Other Risk Factors for Coronary Artery Disease
Abstract
1. Introduction
2. Materials and Methods
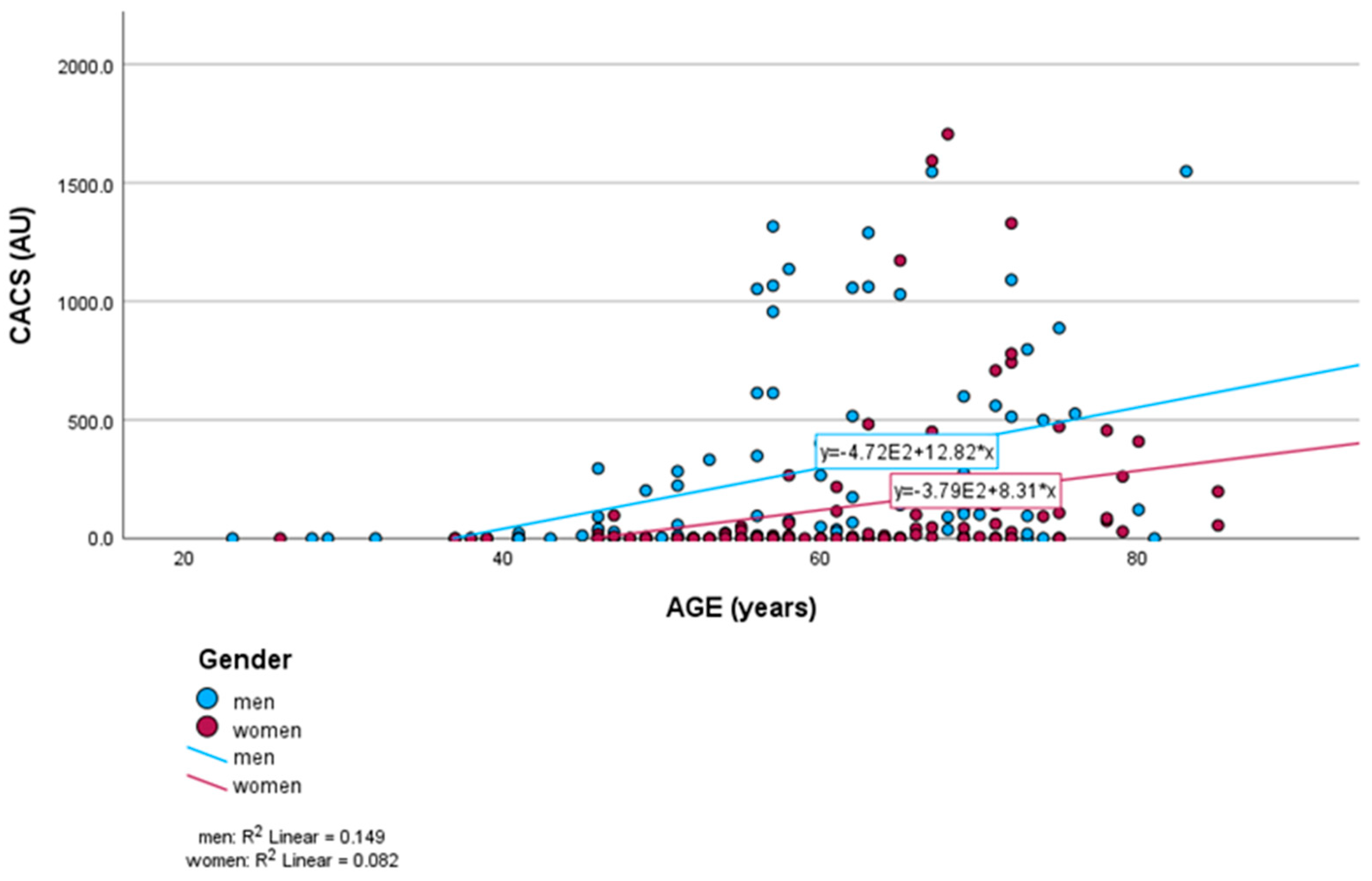
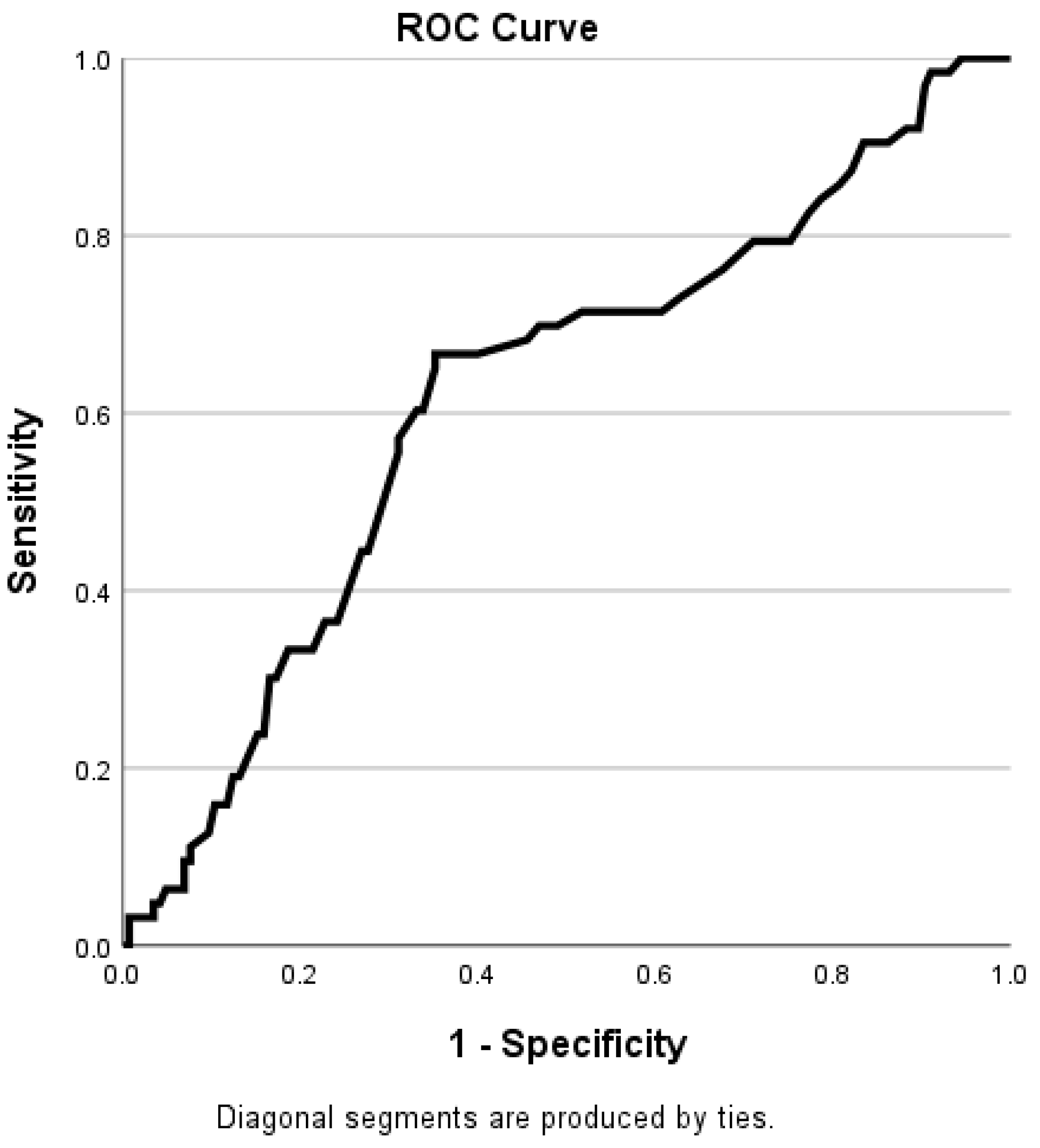
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EAT | Epicardial adipose tissue; |
| CAD | Coronary artery disease; |
| CCTA | Coronary computer tomography angiography; |
| CAC | Coronary artery calcifications; |
| BMI | Body mass index; |
| CVD | Cardiovascular disease; |
| CACS | Coronary artery calcium score; |
| CABG | Coronary artery bypass graft; |
| ROI | Region of interest; |
| HU | Hounsfield units; |
| LAD | Left anterior descending artery; |
| LCX | Left circumflex artery; |
| LMA | Left main coronary artery; |
| RCA | Right coronary artery. |
References
- World Health Organization. Global Health Estimates: Life Expectancy and Leading Causes of Death and Disability; World Health Organization: Geneva, Switzerland, 2023; Available online: https://www.who.int/data/gho/data/themes/mortality-and-global-health-estimates (accessed on 22 April 2025).
- Suman, S.; Pravalika, J.; Manjula, P.; Farooq, U. Gender and CVD- does it really matters? Curr. Probl. Cardiol. 2023, 48, 101604. [Google Scholar] [CrossRef] [PubMed]
- Daly, C.A.; Clemens, F.; Sendon, J.L.L.; Tavazzi, L.; Boersma, E.; Danchin, N.; Delahaye, F.; Gitt, A.; Julian, D.; Mulcahy, D.; et al. The clinical characteristics and investigations planned in patients with stable angina presenting to cardiologists in Europe: From the Euro Heart Survey of Stable Angina. Eur. Heart J. 2005, 26, 996–1010. [Google Scholar] [CrossRef]
- Maas, A.H.; Appelman, Y.E. Gender differences in coronary heart disease. Neth. Heart J. 2010, 18, 598–602. [Google Scholar] [CrossRef]
- Hochman, J.S.; Tamis, J.E.; Thompson, T.D.; Weaver, W.D.; White, H.D.; Van de Werf, F.; Aylward, P.; Topol, E.J.; Califf, R.M. Sex, clinical presentation, and outcome in patients with acute coronary syndromes. N. Engl. J. Med. 1999, 341, 226–232. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.L. Differences in Risk Factors for Coronary Atherosclerosis According to Sex. J. Lipid Atheroscler. 2024, 13, 97–110. [Google Scholar] [CrossRef]
- Khot, U.N.; Khot, M.B.; Bajzer, C.T.; Sapp, S.K.; Ohman, E.M.; Brener, S.J.; Ellis, S.G.; Lincoff, A.M.; Topol, E.J. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003, 290, 898–904. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Gebhard, C. Gender medicine: Effects of sex and gender on cardiovascular disease manifestation and outcomes. Nat. Rev. Cardiol. 2023, 20, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Greenland, P.; Bonow, R.O.; Brundage, B.H.; Budoff, M.J.; Eisenberg, M.J.; Grundy, S.M.; Lauer, M.S.; Post, W.S.; Raggi, P.; Redberg, R.F.; et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain. J. Am. Coll. Cardiol. 2007, 49, 378–402. [Google Scholar] [CrossRef]
- Sarwar, A.; Shaw, L.J.; Shapiro, M.D.; Blankstein, R.; Hoffman, U.; Cury, R.C.; Abbara, S.; Brady, T.J.; Budoff, M.J.; Blumenthal, R.S.; et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc. Imaging 2009, 2, 675–688. [Google Scholar] [CrossRef]
- Eckert, J.; Schmidt, M.; Magedanz, A.; Voigtländer, T.; Schmermund, A. Coronary CT Angiography in Managing Atherosclerosis. Int. J. Mol. Sci. 2015, 16, 3740–3756. [Google Scholar] [CrossRef]
- Sato, Y.; Kawakami, R.; Sakamoto, A.; Cornelissen, A.; Mori, M.; Kawai, K.; Ghosh, S.; Romero, M.E.; Kolodgie, F.D.; Finn, A.V.; et al. Sex Differences in Coronary Atherosclerosis. Curr. Atheroscler. Rep. 2022, 24, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Bigeh, A.; Shekar, C.; Gulati, M. Sex differences in coronary artery calcium and long-term CV mortality. Curr. Cardiol. Rep. 2020, 22, 21. [Google Scholar] [CrossRef] [PubMed]
- Konishi, M.; Sugiyama, S.; Sato, Y.; Oshima, S.; Sugamura, K.; Nozaki, T.; Ohba, K.; Matsubara, J.; Sumida, H.; Nagayoshi, Y.; et al. Pericardial fat inflammation correlates with coronary artery disease. Atherosclerosis 2010, 213, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Ma, R.; van Assen, M.; Sidorenkov, G.; Ties, D.; Pelgrim, G.J.; Stillman, A.; de Cecco, C.; van der Harst, P.; Vliegenthart, R. Relationships of pericoronary and epicardial fat measurements in male and female patients with and without coronary artery disease. Eur. J. Radiol. 2023, 169, 111154. [Google Scholar] [CrossRef]
- Liu, J.; Yu, Q.; Li, Z.; Zhou, Y.; Liu, Z.; You, L.; Tao, L.; Dong, Q.; Zuo, Z.; Gao, L.; et al. Epicardial adipose tissue density is a better predictor of cardiometabolic risk in HFpEF patients: A prospective cohort study. Cardiovasc. Diabetol. 2023, 22, 45. [Google Scholar] [CrossRef]
- Machado, A.K.F.; Ricardo, L.I.C.; Wendt, A.; Wehrmeister, F.C. Association between sleep duration and academic, cognitive and socioeconomic outcomes: A systematic literature review of population-based studies. Sleep Epidemiol. 2022, 2. [Google Scholar] [CrossRef]
- Agatston, A.S.; Janowitz, W.R.; Hildner, F.J.; Zusmer, N.R.; Viamonte, M., Jr.; Detrano, R. Quantification of coronary artery calcium using ultrafast computed tomography. J. Am. Coll. Cardiol. 1990, 15, 827–832. [Google Scholar] [CrossRef] [PubMed]
- Raggi, P.; Gadiyaram, V.; Zhang, C.; Chen, Z.; Lopaschuk, G.; Stillman, A.E. Statins reduce epicardial adipose tissue attenuation independent of lipid lowering: A potential pleiotropic effect. J. Am. Heart. Assoc. 2019, 8, e013104. [Google Scholar] [CrossRef]
- Ko, D.T.; Wijeysundera, H.C.; Udell, J.A.; Vaccarino, V.; Austin, P.C.; Guo, H.; Velianou, J.L.; Lau, K.; Tu, J.V. Traditional cardiovascular risk factors and the presence of obstructive coronary artery disease in men and women. Can. J. Cardiol. 2014, 30, 820–826. [Google Scholar] [CrossRef]
- Blum, A. Gender differences in vascular aging and in coronary artery disease pathophysiology. QJM 2023, 116, 745–749. [Google Scholar] [CrossRef]
- Kim, H.-L.; Kim, H.-J.; Kim, M.; Park, S.M.; Yoon, H.J.; Byun, Y.S.; Park, S.M.; Shin, M.S.; Hong, K.-S.; Kim, M.-A. Sex differences in coronary angiographic findings in patients with stable chest pain: Analysis of data from the KoRean wOmen’S chest pain rEgistry (KoROSE). Biol. Sex. Differ. 2022, 13, 2. [Google Scholar] [CrossRef]
- Mori, H.; Torii, S.; Kutyna, M.; Sakamoto, A.; Finn, A.V.; Virmani, R. Coronary Artery Calcification and its Progression: What Does it Really Mean? JACC Cardiovasc. Imaging 2018, 11, 127–142. [Google Scholar] [CrossRef]
- Pravda, N.S.; Karny-Rahkovich, O.; Shiyovich, A.; Pravda, M.S.; Rapeport, N.; Vaknin-Assa, H.; Eisen, A.; Kornowski, R.; Porter, A. Coronary Artery Disease in Women: A Comprehensive Appraisal. J. Clin. Med. 2021, 12, 4664. [Google Scholar] [CrossRef]
- Freaney, P.M.; Khan, S.S.; Lloyd-Jones, D.M.; Stone, N.J. The Role of Sex-Specific Risk Factors in the Risk Assessment of Atherosclerotic Cardiovascular Disease for Primary Prevention in Women. Curr. Atheroscler. Rep. 2020, 22, 46. [Google Scholar] [CrossRef]
- Gheisari, F.; Emami, M.; Raeisi Shahraki, H.; Samipour, S.; Nematollahi, P. The Role of Gender in the Importance of Risk Factors for Coronary Artery Disease. Cardiol. Res. Pract. 2020, 29, 6527820. [Google Scholar] [CrossRef]
- Mahabadi, A.A.; Balcer, B.; Dykun, I.; Forsting, M.; Schlosser, T.; Heusch, G.; Rassaf, T. Cardiac computed tomography-derived epicardial fat volume and attenuation independently distinguish patients with and without myocardial infarction. PLoS ONE 2017, 12, e0183514. [Google Scholar] [CrossRef] [PubMed]
- Rosito, G.A.; Massaro, J.M.; Hoffmann, U.; Ruberg, F.L.; Mahabadi, A.A.; Vasan, R.S.; O’Donnell, C.J.; Fox, C.S. Pericardial fat, visceral abdominal fat, cardiovascular disease risk factors, and vascular calcification in a community-based sample the Framingham heart study. Circulation 2008, 117, 605–613. [Google Scholar] [CrossRef]
- Lee, C.Y.; Liu, K.T.; Lu, H.T.; Ali, R.M.; Fong, A.Y.Y.; Ahmad, W.A.W. Sex and gender differences in presentation, treatment and outcomes in acute coronary syndrome, a 10 year study from a multi-ethnic Asian population: The Malaysian National Cardiovascular Disease Database-Acute Coronary Syndrome (NCVD-ACS) registry. PLoS ONE 2021, 16, e0246474. [Google Scholar] [CrossRef] [PubMed]
- Gerdts, E.; Sudano, I.; Brouwers, S.; Borghi, C.; Bruno, R.M.; Ceconi, C.; Cornelissen, V.; Diévart, F.; Ferrini, M.; Kahan, T.; et al. Sex differences in arterial hypertension. Eur. Heart J. 2022, 43, 4777–4788. [Google Scholar] [CrossRef]
- Cappuccio, F.P.; Cooper, D.; D’Elia, L.; Strazzullo, P.; Miller, M.A. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur. Heart J. 2011, 32, 1484–1492. [Google Scholar] [CrossRef]
- Wang, Q.; Xi, B.; Liu, M.; Zhang, Y.; Fu, M. Short sleep duration is associated with hypertension risk among adults: A systematic review and meta-analysis. Hypertens. Res. 2012, 35, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, M.; Kikuchi, H.; Tanaka, K.; Takahashi, M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. Sleep 2010, 33, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Domínguez, F.; Fuster, V.; Fernández-Alvira, J.M.; Fernández-Friera, L.; López-Melgar, B.; Blanco-Rojo, R.; Fernández-Ortiz, A.; García-Pavía, P.; Sanz, J.; Mendiguren, J.M.; et al. Association of sleep duration and quality with subclinical atherosclerosis. J. Am. Coll. Cardiol. 2019, 73, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.-W.; Chang, Y.; Zhao, D.; Cainzos-Achirica, M.; Ryu, S.; Jung, H.-S.; Yun, K.E.; Choi, Y.; Ahn, J.; Zhang, Y.; et al. Sleep Duration, Sleep Quality, and Markers of Subclinical Arterial Disease in Healthy Men and Women. Arter. Thromb. Vasc. Biol. 2015, 35, 2238–2245. [Google Scholar] [CrossRef] [PubMed]
- Vogel, B.; Acevedo, M.; Appelman, Y.; Merz, C.N.B.; Chieffo, A.; A Figtree, G.; Guerrero, M.; Kunadian, V.; Lam, C.S.P.; Maas, A.H.E.M.; et al. The Lancet Women and Cardiovascular Disease Commission: Reducing the global burden by 2030. Lancet 2021, 397, 2385–2438. [Google Scholar] [CrossRef]
| Variable | All (n = 208) | Men (n = 105) | Women (n = 103) | p-Value |
|---|---|---|---|---|
| BMI (kg/m2) | 29.2 ±5.6 | 29.5 ± 5.1 | 28.9 ± 6.2 | 0.334 |
| Age (years) | 59.7 ± 11.8 | 57.2 ± 12.0 | 62.3 ± 11.1 | 0.001 |
| EAT attenuation | −101.8 ± 12.9 | −98.4 ± 11.2 | −105.3 ± 13.8 | <0.001 |
| CACS (AU) | 344.6 (268.0) | 484.1 (515.2) | 202.3 (121.3) | 0.003 |
| CACS(AU) = 0 | 70 (33.7%) | 28 (26.7%) | 42 (40.8%) | 0.040 |
| CACS per vessel | ||||
| LMA | 45.9 (34.8) | 51.9 (51.3) | 39.8 (21.8) | 0.077 |
| LAD | 122.7 (92.9) | 117.9 (191.2) | 66.4 (59.3) | 0.009 |
| LCX | 50.5 (13.3) | 73.4 (29.5) | 27.2 (6.2) | 0.004 |
| RCA | 124.1 (28.8) | 177.3 (63.5) | 69.9 (3.9) | 0.001 |
| Smoking | 37 (17.9%) | 23 (22.3%) | 14 (13.4%) | 0.110 |
| Diabetes | 30 (14.5%) | 15 (14.6%) | 15 (14.4%) | 0.997 |
| Hypertension | 114 (55.1%) | 52 (50.4%) | 62 (59.6%) | 0.140 |
| Hypercholesterolemia | 54 (26.1%) | 21 (20.4%) | 33 (31.7%) | 0.052 |
| Family history of cardiovascular disease | 122 (58.9%) | 59 (57.3%) | 63 (60.5%) | 0.517 |
| Myocardial infarction | 11 (5.3%) | 7 (6.8%) | 4 (3.8%) | 0.361 |
| Angina pectoris | 93 (44.9%) | 38 (36.9%) | 55 (52.9%) | 0.015 |
| Presence of at least one coronary artery stenosis ≥ 50% | 63 (30.3%) | 40 (38.8%) | 23 (22.1%) | 0.013 |
| Presence of at least one coronary artery stenosis ≥ 70% | 27 (13.0%) | 19 (18.4%) | 8 (7.7%) | 0.027 |
| Men | p-Value | Women | p-Value | |||
|---|---|---|---|---|---|---|
| CAD > 50% | CAD < 50% | CAD > 50% | CAD < 50% | |||
| BMI | 30.28 ± 4.57 | 29.1 ± 5.3 | 0.217 | 29.2 ± 6.5 | 28.8 ± 6.1 | 0.798 |
| Age | 61.3 ± 8.8 | 54.9 ± 12.9 | 0.006 | 70.5 ± 7.1 | 60.3 ± 10.9 | <0.001 |
| Age > 65 years | 13 (32.5%) | 14 (21.5%) | 0.212 | 18 (78.3%) | 25 (31.3%) | <0.001 |
| EAT attenuation | −94.9 ± 10.8 | −100.5 ± 10.9 | 0.006 | −104.3 ± 12.8 | −105.5 ±14.1 | 0.797 |
| CACS (AU) | 1041.6 (854.3) | 142.5 (66.5) | <0.001 | 604.6 (828.8) | 85.8 (39.8) | <0.001 |
| CACS (AU) = 0 | 0 (0%) | 28 (43.1%) | <0.001 | 1 (4.3%) | 41 (51.2%) | <0.001 |
| CACS per vessel | ||||||
| LMA | 93.7 (114.0) | 26.3 (5.0) | <0.001 | 117.1 (117.8) | 17.5 (0.0) | <0.001 |
| LAD | 391.7 (419.5) | 46.8(18.8) | <0.001 | 186.0 (342.0) | 31.7 (11.0) | <0.001 |
| LCX | 180.1 (183.0) | 7.9 (2.7) | <0.001 | 88.8 (71.5) | 9.3 (0.0) | <0.001 |
| RCA | 375.5 (341.0) | 55.8 (1.0) | <0.001 | 217.3 (159.9) | 27.3 (0.0) | <0.001 |
| Smoking | 12 (30.7%) | 11 (16.9%) | 0.100 | 0 | 14 (17.5%) | 0.031 |
| Diabetes | 5 (12.8%) | 10 (15.4%) | 0.719 | 4 (17.4%) | 11 (13.7%) | 0.663 |
| Hypertension | 24 (61.5%) | 28 (43.1%) | 0.068 | 19 (82.6%) | 43 (53.7%) | 0.013 |
| Hypercholesterolemia | 12 (30.8%) | 9 (13.8%) | 0.037 | 10 (43.5%) | 23 (28.7%) | 0.182 |
| Family history of cardiovascular disease | 22 (56.4%) | 37 (56.9%) | 0.959 | 12 (52.2%) | 51 (63.7%) | 0.315 |
| Myocardial infarction | 4 (10.3%) | 3 (4.6%) | 0.266 | 2 (8.7%) | 2 (2.5%) | 0.175 |
| Angina pectoris | 17 (43.6%) | 21 (32.3%) | 0.247 | 12 (52.2%) | 43 (53.7%) | 0.894 |
| Hours of sleep | 0.733 | 0.008 | ||||
| <6 | 7 (31.8%) | 11 (26.1%) | 4 (40%) | 17 (37.8%) | ||
| 6–9 | 14 (63.6%) | 27 (64.3%) | 4 (40%) | 28 (62.2%) | ||
| >9 | 1 (4.6%) | 4 (9.5%) | 2 (20%) | 0 | ||
| Variable | All | Male | Female | ||||
|---|---|---|---|---|---|---|---|
| Units | OR | p-Value | OR | p-Value | OR | p-Value | |
| Age | +1 year | 1.058 | <0.001 | 1.052 | 0.008 | 1.122 | <0.001 |
| Gender | Male vs. female | 2.140 | 0.014 | ||||
| BMI | +1 kg/m2 | 1.030 | 0.227 | 1.048 | 0.258 | 1.010 | 0.795 |
| Diabetes | Present vs. absent | 1.003 | 0.995 | 0.719 | 0.809 | 1.321 | 0.663 |
| Hypertension | Present vs. absent | 2.359 | 0.008 | 2.114 | 0.07 | 4.087 | 0.048 |
| Hypercholesterolemia | Present vs. absent | 1.942 | 0.046 | 2.765 | 0.042 | 1.906 | 0.186 |
| Smoking | Present vs. absent | 1.152 | 0.716 | 2.182 | 0.104 | 0.000 | 0.999 |
| EAT | +1 HU | 1.032 | 0.013 | 1.053 | 0.011 | 1.005 | 0.068 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lesjak, V.; Kocet, L. Sex Differences in Epicardial Adipose Tissue and Other Risk Factors for Coronary Artery Disease. Medicina 2025, 61, 934. https://doi.org/10.3390/medicina61050934
Lesjak V, Kocet L. Sex Differences in Epicardial Adipose Tissue and Other Risk Factors for Coronary Artery Disease. Medicina. 2025; 61(5):934. https://doi.org/10.3390/medicina61050934
Chicago/Turabian StyleLesjak, Vesna, and Laura Kocet. 2025. "Sex Differences in Epicardial Adipose Tissue and Other Risk Factors for Coronary Artery Disease" Medicina 61, no. 5: 934. https://doi.org/10.3390/medicina61050934
APA StyleLesjak, V., & Kocet, L. (2025). Sex Differences in Epicardial Adipose Tissue and Other Risk Factors for Coronary Artery Disease. Medicina, 61(5), 934. https://doi.org/10.3390/medicina61050934





