Longitudinal Observational Study on Quality of Life in Patients with Chronic Wounds Using DLQI and EQ-5D
Abstract
1. Introduction
1.1. Primary Objective
1.2. Secondary Objectives
- To compare the evolution of QoL across different treatment strategies, including moist wound healing (MWH), foam dressings, alginate dressings, compression therapy, and negative-pressure wound therapy (NPWT).
- To explore the specific impacts of chronic wounds on pain, mobility, social participation, autonomy, and sexuality.
2. Materials and Methods
- The Ulcer and Wound Unit at the University Clinics of the Catholic University of Valencia (UCV);
- The Advanced Nursing Unit in Rheumatology and Rehabilitation at Sagunto Hospital;
- The Ulcer Unit at the Consorcio Hospital General Universitario de Valencia (CHGUV).
2.1. Participants and Sample
- Age ≥ 18 years;
- Diagnosis of venous leg ulcer confirmed by clinical evaluation and, when necessary, Doppler ultrasound;
- Ulcer duration greater than six weeks;
- Capacity to provide informed consent;
- Adequate understanding of Spanish to complete the QoL questionnaires.
- Presence of mixed etiology ulcers (arteriovenous, neuropathic);
- Severe cognitive impairment that precluded reliable questionnaire responses;
- Terminal illnesses or conditions with an expected survival of less than six months;
- Patients unwilling or unable to participate in scheduled follow-ups.
2.2. Variables and Instruments
- Dermatology Life Quality Index (DLQI): a specific tool composed of 10 questions grouped into six dimensions (symptoms and feelings, daily activities, leisure, work and school, personal relationships, and treatment) [19]. Each question is scored from 0 to 3, with higher scores indicating greater impairment of quality of life.
- EuroQol-5D (EQ-5D-5L): a generic instrument measuring five health dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) on a five-level scale, plus a visual analogue scale (VAS) ranging from 0 (worst imaginable health state) to 100 (best imaginable health state) [20].
- Baseline (Visit 1);
- One-month follow-up (Visit 2);
- Discharge after wound healing or completion of active treatment (Visit 3).
2.3. Treatment Modalities
- Moist Wound Healing (MWH): Application of moist dressings aimed at maintaining an optimal wound environment to promote autolytic debridement and tissue regeneration.
- Alginate Dressings: Indicated for wounds with moderate to heavy exudate, providing hemostatic properties and facilitating the removal of devitalized tissue.
- Foam Dressings: Polyurethane dressings used for moderate exudate control, cushioning, and protection against external contamination.
- Compression Therapy: Essential in the management of venous leg ulcers, employing multilayer systems, elastic or inelastic bandages, or compression stockings according to patient tolerance and clinical indication.
- Negative-Pressure Wound Therapy (NPWT): Applied in complex wounds or in cases requiring enhanced granulation tissue formation and exudate management.
2.4. Statistical Analysis
- Friedman’s test was applied to ordinal and non-normally distributed variables, followed by Wilcoxon signed-rank tests for post hoc pairwise comparisons with Bonferroni adjustment.
- Repeated-Measures ANOVA (with Greenhouse–Geisser correction when sphericity was violated) was used for normally distributed continuous variables.
2.5. Ethical Approval and Informed Consent
3. Results
3.1. Baseline Characteristics of the Sample
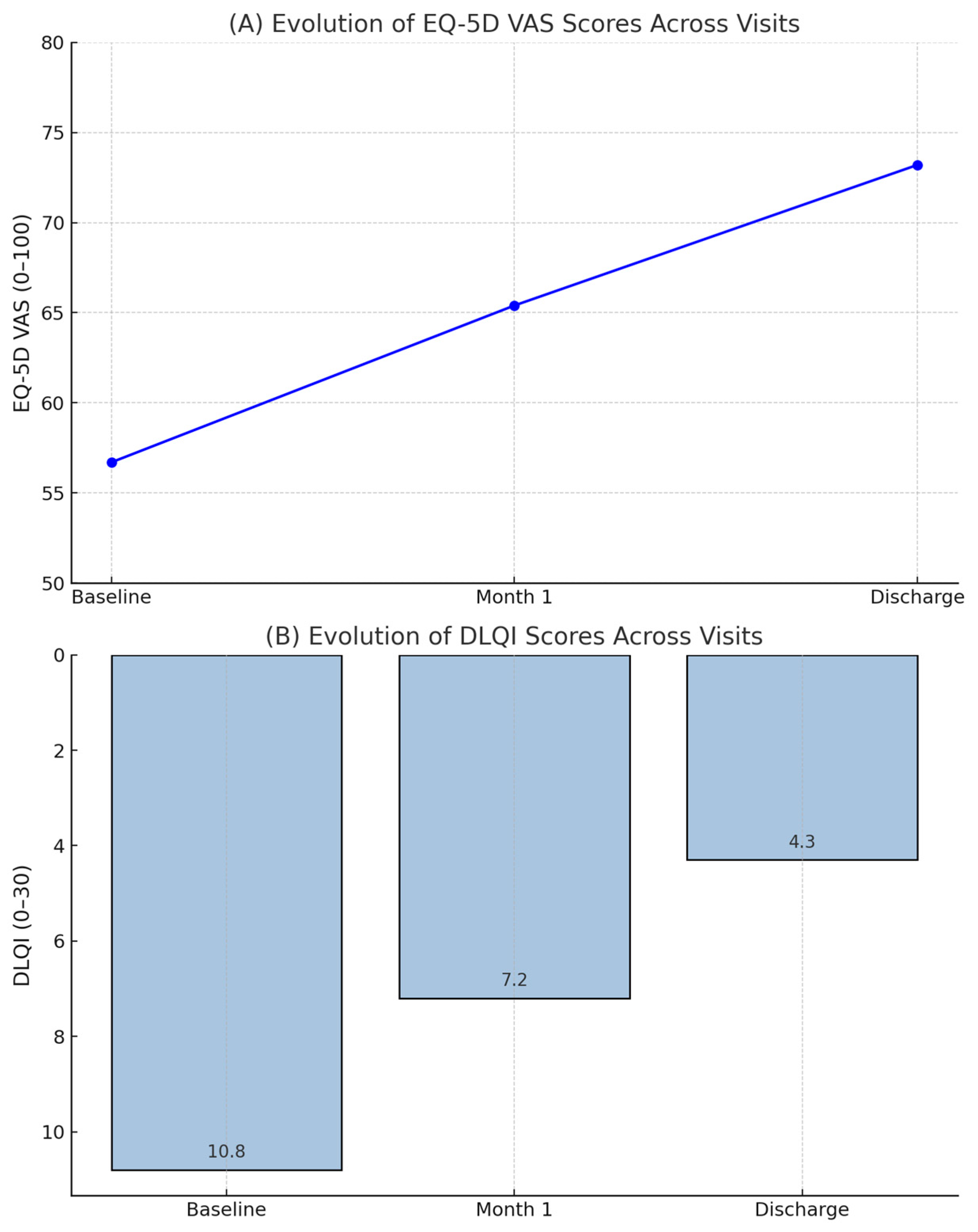
3.2. Evolution of Quality of Life over Time
- Baseline: 10.8 (SD: 5.4);
- One-month follow-up: 7.2 (SD: 4.9);
- Discharge: 4.3 (SD: 4.1).
- Baseline: 56.7 (SD: 17.5);
- One-month follow-up: 65.4 (SD: 18.1);
- Discharge: 73.2 (SD: 16.8).
3.3. Evolution of Specific Psychosocial and Functional Variables
- Pain: Decreased from a mean score of 1.81 to 1.24 (p < 0.001).
- Embarrassment: Reduced from 1.54 to 0.87 (p < 0.001).
- Clothing limitations: Slight reduction from 1.18 to 0.95 (p = 0.004).
- Social life impact: Decreased from 1.47 to 0.82 (p < 0.001).
- Work limitations: Limited change due to the high number of retired participants.
- Shopping difficulties: Decreased significantly (p < 0.001).
- Sexuality domain: No substantial change observed across time points, with mean scores consistently close to zero.
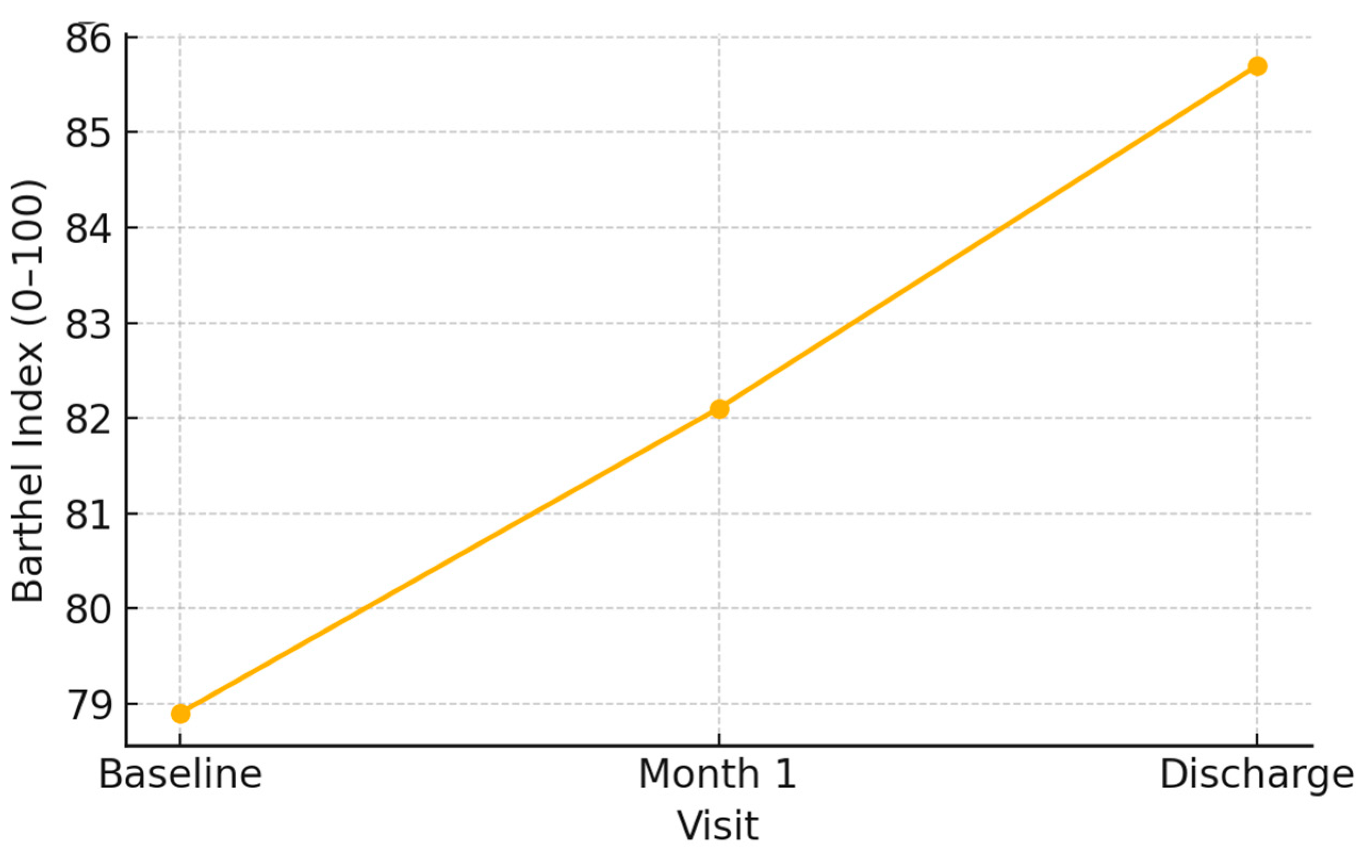
3.4. Evolution of Functional Independence
- Most patients improved slightly in autonomy, particularly regarding mobility and self-care domains.
- However, a subgroup with multiple comorbidities experienced a decline in independence over the study period (Figure 1).
3.5. Comparison of Quality-of-Life Outcomes Across Treatment Modalities
- Moist Wound Healing (MWH) and foam dressings were associated with the most notable improvements in both DLQI and EQ-5D scores.
- Patients treated predominantly with MWH achieved a mean DLQI reduction of 7.4 points and an EQ-5D VAS increase of 18.2 points from baseline to discharge (p < 0.001 for both comparisons). Foam dressings demonstrated similar outcomes, with slightly lower magnitudes of change.
- Alginate dressings produced moderate improvements in quality of life, particularly in domains related to exudate control and dressing comfort, though overall QoL gains were somewhat smaller compared to MWH and foam dressings.
- Compression therapy, used either as primary treatment or in combination with dressings, resulted in significant improvements in mobility and pain-related dimensions. Patients adhering strictly to compression regimens showed better gains in EQ-5D mobility and pain domains compared to non-adherent patients (p = 0.003).
- Negative-Pressure Wound Therapy (NPWT) showed less marked improvement in QoL scores compared to other modalities. While wound healing outcomes were favorable, patients treated with NPWT reported persistent difficulties related to autonomy and social life, likely reflecting the complexity and severity of their underlying wounds (Figure 2).
4. Discussion
4.1. Perspectives for Clinical Practice
4.2. Study Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
List of Abbreviations
| Abbreviation | Full Term |
| DLQI | Dermatology Life Quality Index |
| EQ-5D | EuroQol 5-Dimension Questionnaire |
| NPWT | Negative-Pressure Wound Therapy |
| CT | Compression Therapy |
| MWH | Moist Wound Healing |
| SD | Standard Deviation |
| VAS | Visual Analogue Scale |
| UCV | Universidad Católica de Valencia |
| CHGUV | Consorcio Hospital General Universitario de Valencia |
References
- Phillips, C.J.; Humphreys, I.; Fletcher, J.; Harding, K.; Chamberlain, G.; Macey, S. Estimating the costs associated with the management of patients with chronic wounds using linked routine data. Int. Wound J. 2016, 13, 1193–1197. [Google Scholar] [CrossRef] [PubMed]
- Sen, C.K.; Gordillo, G.M.; Roy, S.; Kirsner, R.; Lambert, L.; Hunt, T.K.; Gottrup, F.; Gurtner, G.C.; Longaker, M.T. Human skin wounds: A major and snowballing threat to public health and the economy. Wound Repair Regen. 2009, 17, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Lazarus, G.S.; Cooper, D.M.; Knighton, D.R.; Margolis, D.J.; Pecoraro, R.E.; Rodeheaver, G.; Robson, M.C. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch. Dermatol. 1994, 130, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Vowden, K.; Vowden, P. The economic impact of hard-to-heal wounds: Promoting practice change to address passivity in wound management. Wounds Int. 2016, 7, 10–15. [Google Scholar]
- Salcido, R. Societal burden of chronic wounds. Adv. Skin Wound Care 2017, 30, 511. [Google Scholar]
- Finlayson, K.J.; Wu, M.L.; Edwards, H.E. Identifying risk factors and protective factors for venous leg ulcer recurrence using a theoretical approach: A longitudinal study. Int. J. Nurs. Stud. 2015, 52, 1042–1051. [Google Scholar] [CrossRef] [PubMed]
- Gottrup, F.; Apelqvist, J.; Price, P. Outcomes in controlled and comparative studies on non-healing wounds: Recommendations to improve the quality of evidence in wound management. J. Wound Care 2010, 19, 237–268. [Google Scholar] [CrossRef] [PubMed]
- Finlay, A.Y.; Khan, G.K. Dermatology Life Quality Index (DLQI): A simple practical measure for routine clinical use. Clin. Exp. Dermatol. 1994, 19, 210–216. [Google Scholar] [CrossRef] [PubMed]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. World Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Cutting, K.F.; White, R.J. Criteria for identifying wound infection—Revisited. Ostomy Wound Manage. 2005, 51, 28–34. [Google Scholar] [PubMed]
- Järbrink, K.; Ni, G.; Sönnergren, H.; Schmidtchen, A.; Pang, C.; Bajpai, R.; Car, J. The humanistic and economic burden of chronic wounds: A systematic review. Wound Repair Regen. 2017, 25, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Price, P.; Harding, K.G. Measuring health-related quality of life in patients with chronic leg ulcers. Wound Repair Regen. 2004, 12, 434–439. [Google Scholar]
- Margolis, D.J.; Berlin, J.A.; Strom, B.L. Which venous leg ulcers will heal with limb compression bandages? Am. J. Med. 2000, 109, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Szewczyk, M.T.; Jawień, A.; Cwajda, J.; Cierzniakowska, K.; Al-Hadidi, D.; Karnafel, W. Quality of life in patients with venous leg ulcers: Polish experience. J. Wound Care 2012, 21, 236–241. [Google Scholar]
- Persoon, A.; Heinen, M.M.; van der Vleuten, C.J.M.; de Rooij, M.J.; van de Kerkhof, P.C.M.; van Achterberg, T. Leg ulcers: A review of their impact on daily life. J. Clin. Nurs. 2004, 13, 341–354. [Google Scholar] [CrossRef] [PubMed]
- Charles, H. The impact of leg ulcers on patients’ quality of life. Prof. Nurse 2002, 17, 576–578. [Google Scholar]
- Augustin, M.; Herberger, K.; Rustenbach, S.J.; Schäfer, I.; Ehret, S.; Reusch, M. Prevalence and disease burden of chronic wounds. Wound Repair Regen. 2012, 20, 434–441. [Google Scholar]
- Norman, G.; Shi, C.; Goh, E.L.; Murphy, E.M.; Reid, A.; Chiverton, L.; Stankiewicz, M.; Dumville, J.C. Negative pressure wound therapy for surgical wounds healing by primary closure. Cochrane Database Syst. Rev. 2020, 6, CD009261. [Google Scholar] [PubMed]
- Wong, P.; Chua, K.; Tan, J.; Song, C. The impact of negative pressure wound therapy on wound healing: A systematic review and meta-analysis. Int. Wound J. 2015, 12, 383–388. [Google Scholar]
| Variable | Baseline (Mean ± SD) | Month 1 (Mean ± SD) | Discharge (Mean ± SD) | p-Value (Friedman Test) |
|---|---|---|---|---|
| Pain (0–3) | 1.81 ± 0.72 | 1.42 ± 0.65 | 1.24 ± 0.58 | <0.001 |
| Embarrassment (0–3) | 1.54 ± 0.68 | 1.02 ± 0.57 | 0.87 ± 0.49 | <0.001 |
| Clothing limitations (0–3) | 1.18 ± 0.55 | 1.05 ± 0.51 | 0.95 ± 0.48 | 0.004 |
| Social life impact (0–3) | 1.47 ± 0.66 | 0.95 ± 0.54 | 0.82 ± 0.47 | <0.001 |
| Shopping difficulties (0–3) | 1.39 ± 0.61 | 1.02 ± 0.58 | 0.83 ± 0.50 | <0.001 |
| Sexuality impact (0–3) | 0.26 ± 0.32 | 0.23 ± 0.30 | 0.22 ± 0.29 | 0.421 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Palomar-Albert, D.; Zamora-Ortiz, J.; Palomar-Llatas, F.; Escudero-Martínez, M.; Naranjo-Cuellar, A.; Pastor-Orduña, M.I. Longitudinal Observational Study on Quality of Life in Patients with Chronic Wounds Using DLQI and EQ-5D. Medicina 2025, 61, 907. https://doi.org/10.3390/medicina61050907
Palomar-Albert D, Zamora-Ortiz J, Palomar-Llatas F, Escudero-Martínez M, Naranjo-Cuellar A, Pastor-Orduña MI. Longitudinal Observational Study on Quality of Life in Patients with Chronic Wounds Using DLQI and EQ-5D. Medicina. 2025; 61(5):907. https://doi.org/10.3390/medicina61050907
Chicago/Turabian StylePalomar-Albert, David, Jorge Zamora-Ortiz, Federico Palomar-Llatas, Marta Escudero-Martínez, Alba Naranjo-Cuellar, and Maria Isabel Pastor-Orduña. 2025. "Longitudinal Observational Study on Quality of Life in Patients with Chronic Wounds Using DLQI and EQ-5D" Medicina 61, no. 5: 907. https://doi.org/10.3390/medicina61050907
APA StylePalomar-Albert, D., Zamora-Ortiz, J., Palomar-Llatas, F., Escudero-Martínez, M., Naranjo-Cuellar, A., & Pastor-Orduña, M. I. (2025). Longitudinal Observational Study on Quality of Life in Patients with Chronic Wounds Using DLQI and EQ-5D. Medicina, 61(5), 907. https://doi.org/10.3390/medicina61050907






