Analyzing Clinical Parameters and Bacterial Profiles to Uncover the COPD Exacerbations: A Focus on Intensive Care Unit Challenges
Abstract
1. Introduction
2. Materials and Methods
Inclusion and Exclusion Criteria
- Patients aged 45 years or older
- Patients diagnosed with COPD according to GOLD 2024 criteria [2] (Global Initiative for Chronic Obstructive Lung Disease 2024)
- Regularly monitoring by pulmonologists (at least once every 3 months)
- At least one moderate or severe documented exacerbation in the last year
- Patients presenting clinical signs for an AECOPD (such as purulent sputum, elevated body temperature, and increased respiratory rate) and laboratory parameters (elevated white blood cell count, C-reactive protein) indicative of bacterial superinfection
- Patients admitted to the ICU for an acute exacerbation of chronic respiratory failure that required mechanical ventilation or non-invasive ventilation
- Patients admitted outside the study period
- Patients with a secondary diagnosis of SARS-CoV-2 infection
- Patients with overlap syndrome between bronchial asthma and COPD
- Patients who were not experiencing severe clinical deterioration and did not require ICU transfer
- Inspiratory pressure (IPAP): 10–18 cmH2O
- Expiratory pressure (EPAP): 5–10 cmH2O
- Pressure support (PS)—difference between IPAP and EPAP—at least 5 cmH2O
- Tidal volume: 6 mL/kg (according to ideal weight)
- Tidal volume: 6–7 mL/kg (according to ideal weight)
- Respiratory rate: 10–12 respiration/min
- Inspire: Expire ratio: I:E—1:3
- Inspiratory flow: 70–100 L/min
- Positive end-expiratory pressure (PEEP): 4–6 cmH2O
- Inspiratory fraction of oxygen (FiO2)—55–70%
3. Results
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Chronic Obstructive Pulmonary Disease (COPD). 2017. Available online: https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd) (accessed on 7 November 2024).
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for Prevention, Diagnosis and Management of Copd: 2024 Report. 2024. Available online: https://goldcopd.org/2024-gold-report/ (accessed on 7 November 2024).
- Prevalence of Chronic Obstructive Pulmonary Disease (%). Available online: https://gateway.euro.who.int/en/indicators/hfa_403-2510-prevalence-of-chronic-obstructive-pulmonary-disease/#id=19388 (accessed on 18 November 2024).
- Ghid Local de Management al Bronhopneumopatiei Obstructive Cronice. Available online: https://legislatie.just.ro/Public/DetaliiDocument/125567 (accessed on 19 November 2024).
- Love, M.E.; Proud, D. Respiratory Viral and Bacterial Exacerbations of COPD—The Role of the Airway Epithelium. Cells 2022, 11, 1416. [Google Scholar] [CrossRef]
- Wei, M.; Zhao, Y.; Qian, Z.; Yang, B.; Xi, J.; Wei, J.; Tang, B. Pneumonia caused by Mycobacterium tuberculosis. Microbes Infect. 2020, 22, 278–284. [Google Scholar] [CrossRef] [PubMed]
- Kahnert, K.; Jörres, R.A.; Behr, J.; Welte, T. The Diagnosis and Treatment of COPD and Its Comorbidities. Dtsch. Arztebl. Int. 2023, 120, 434–444. [Google Scholar] [CrossRef]
- Steriade, A.T.; Davidoiu, A.; Afrasinei, A.; Tudose, C.; Radu, D.; Necula, D.; Bogdan, M.A.; Bumbacea, D. Predictors of Long-term Mortality after Hospitalization for Severe COPD Exacerbation. Maedica-A J. Clin. Med. 2019, 14, 86–92. [Google Scholar] [CrossRef]
- Hurst, J.R.; Vestbo, J.; Anzueto, A.; Locantore, N.; Müllerova, H.; Tal-Singer, R.; Miller, B.; Lomas, D.A.; Agusti, A.; MacNee, W.; et al. Susceptibility to Exacerbation in Chronic Obstructive Pulmonary Disease. N. Engl. J. Med. 2010, 363, 1128–1138. [Google Scholar] [CrossRef] [PubMed]
- JWedzicha, A.; Seemungal, T.A. COPD exacerbations: Defining their cause and prevention. Lancet 2007, 370, 786–796. [Google Scholar] [CrossRef] [PubMed]
- Seemungal, T.A.R.; Donaldson, G.C.; Paul, E.A.; Bestall, J.C.; Jeffries, D.J.; Wedzicha, J.A. Effect of Exacerbation on Quality of Life in Patients with Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 1998, 157, 1418–1422. [Google Scholar] [CrossRef]
- Barnes, H.; Morisset, J.; Molyneaux, P.; Westall, G.; Glaspole, I.; Collard, H.R.; Antoniou, K.M.; Barber, C.M.; Behr, J.; Bonella, F.; et al. A Systematically Derived Exposure Assessment Instrument for Chronic Hypersensitivity Pneumonitis. Chest 2020, 157, 1506–1512. [Google Scholar] [CrossRef]
- Bafadhel, M.; McKenna, S.; Terry, S.; Mistry, V.; Reid, C.; Haldar, P.; McCormick, M.; Haldar, K.; Kebadze, T.; Duvoix, A.; et al. Acute Exacerbations of Chronic Obstructive Pulmonary Disease. Am. J. Respir. Crit. Care Med. 2011, 184, 662–671. [Google Scholar] [CrossRef]
- Celli, B.R.; Barnes, P.J. Exacerbations of chronic obstructive pulmonary disease. Eur. Respir. J. 2007, 29, 1224–1238. [Google Scholar] [CrossRef]
- Chandra, D.; Stamm, J.A.; Taylor, B.; Ramos, R.M.; Satterwhite, L.; Krishnan, J.A.; Mannino, D.; Sciurba, F.C.; Holguín, F. Outcomes of Noninvasive Ventilation for Acute Exacerbations of Chronic Obstructive Pulmonary Disease in the United States, 1998–2008. Am. J. Respir. Crit. Care Med. 2012, 185, 152–159. [Google Scholar] [CrossRef]
- Papi, A.; Bellettato, C.M.; Braccioni, F.; Romagnoli, M.; Casolari, P.; Caramori, G.; Fabbri, L.M.; Johnston, S.L. Infections and Airway Inflammation in Chronic Obstructive Pulmonary Disease Severe Exacerbations. Am. J. Respir. Crit. Care Med. 2006, 173, 1114–1121. [Google Scholar] [CrossRef] [PubMed]
- Sethi, S.; Murphy, T.F. Bacterial Infection in Chronic Obstructive Pulmonary Disease in 2000: A State-of-the-Art Review. Clin. Microbiol. Rev. 2001, 14, 336–363. [Google Scholar] [CrossRef] [PubMed]
- Scala, R.; Pisani, L. Noninvasive ventilation in acute respiratory failure: Which recipe for success? Eur. Respir. Rev. 2018, 27, 180029. [Google Scholar] [CrossRef]
- Ballouz, T.; Aridi, J.; Afif, C.; Irani, J.; Lakis, C.; Nasreddine, R.; Azar, E. Risk Factors, Clinical Presentation, and Outcome of Acinetobacter baumannii Bacteremia. Front. Cell Infect. Microbiol. 2017, 7, 156. [Google Scholar] [CrossRef]
- Shorr, A.F.; Haque, N.; Taneja, C.; Zervos, M.; Lamerato, L.; Kothari, S.; Zilber, S.; Donabedian, S.; Perri, M.B.; Spalding, J.; et al. Clinical and Economic Outcomes for Patients with Health Care-Associated Staphylococcus aureus Pneumonia. J. Clin. Microbiol. 2010, 48, 3258–3262. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Coelho, L.; Póvoa, P.; Almeida, E.; Fernandes, A.; Mealha, R.; Moreira, P.; Sabino, H. Usefulness of C-reactive protein in monitoring the severe community-acquired pneumonia clinical course. Crit. Care 2007, 11, R92. [Google Scholar] [CrossRef]
- Schuetz, P.; Albrich, W.; Mueller, B. Procalcitonin for diagnosis of infection and guide to antibiotic decisions: Past, present and future. BMC Med. 2011, 9, 107. [Google Scholar] [CrossRef]
- Khatib, S.; Sabobeh, T.; Jaber, F.; Abdalla, K.; Singh, S.; Salzman, G. Use of Laboratory Tests and Their Prognostic Value in Patients with Stable Chronic Obstructive Pulmonary Disease. Mo. Med. 2022, 119, 545–552. [Google Scholar]
- Zheng, Y.; Xu, N.; Pang, J.; Han, H.; Yang, H.; Qin, W.; Zhang, H.; Li, W.; Wang, H.; Chen, Y. Colonization With Extensively Drug-Resistant Acinetobacter baumannii and Prognosis in Critically Ill Patients: An Observational Cohort Study. Front. Med. 2021, 8, 667776. [Google Scholar] [CrossRef]
- Kurihara, M.N.L.; de Sales, R.O.; da Silva, K.E.; Maciel, W.G.; Simionatto, S. Multidrug-resistant Acinetobacter baumannii outbreaks: A global problem in healthcare settings. Rev. Soc. Bras. Med. Trop. 2020, 53, e20200248. [Google Scholar] [CrossRef] [PubMed]
- Alrahmany, D.; Omar, A.F.; Alreesi, A.; Harb, G.; Ghazi, I.M. Acinetobacter baumannii Infection-Related Mortality in Hospitalized Patients: Risk Factors and Potential Targets for Clinical and Antimicrobial Stewardship Interventions. Antibiotics 2022, 11, 1086. [Google Scholar] [CrossRef]
- Hurley, J.C. Worldwide variation in Pseudomonas associated ventilator associated pneumonia. A meta-regression. J. Crit. Care 2019, 51, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Duan, C.; Wang, Y.; Wang, Q.; Li, J.; Xie, J.; Liu, S.; Yang, J.; Huang, Y.; Zhao, W.; Yin, W. Gram-negative bacterial infection causes aggravated innate immune response in sepsis: Studies from clinical samples and cellular models. Biochem. Biophys. Res. Commun. 2023, 650, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Yoon, E.C.; Koo, S.-M.; Park, H.Y.; Kim, H.C.; Kim, W.J.; Kim, K.U.; Jung, K.-S.; Yoo, K.H.; Yoon, H.K.; Yoon, H.-Y. Predictive Role of White Blood Cell Differential Count for the Development of Acute Exacerbation in Korean Chronic Obstructive Pulmonary Disease. Int. J. Chron. Obs. Pulmon Dis. 2024, 19, 17–31. [Google Scholar] [CrossRef]
- Gouda, A.M.; Sileem, A.E.; Elnahas, H.M.; Tawfik, A.E.; Eid, R.A.; Shati, A.A.; Al-Qahtani, S.M.; Dawood, S.A.; Alshehri, M.A.; Eissa, M.; et al. Exploring Ventilator-Associated Pneumonia: Microbial Clues and Biomarker Insights from a Retrospective Study. Medicina 2024, 60, 1346. [Google Scholar] [CrossRef] [PubMed]
- Inghammar, M.; Ekbom, A.; Engström, G.; Ljungberg, B.; Romanus, V.; Löfdahl, C.-G.; Egesten, A. COPD and the Risk of Tuberculosis—A Population-Based Cohort Study. PLoS ONE 2010, 5, e10138. [Google Scholar] [CrossRef]
- Uwingabiye, J.; Lemnouer, A.; Baidoo, S.; Frikh, M.; Kasouati, J.; Maleb, A.; Benlahlou, Y.; Bssaibis, F.; Mbayo, A.; Doghmi, N.; et al. Intensive care unit-acquired Acinetobacter baumannii infections in a Moroccan teaching hospital: Epidemiology, risk factors and outcome. Germs 2017, 7, 193–205. [Google Scholar] [CrossRef]
- Villar, M.; Cano, M.E.; Gato, E.; Garnacho-Montero, J.; Cisneros, J.M.; de Alegría, C.R.; Fernández-Cuenca, F.; Martínez-Martínez, L.; Vila, J.; Pascual, A.; et al. Epidemiologic and Clinical Impact of Acinetobacter baumannii Colonization and Infection. Medicine 2014, 93, 202–210. [Google Scholar] [CrossRef]
- Shimizu, K.; Yoshii, Y.; Morozumi, M.; Chiba, N.; Ubukata, K.; Uruga, H.; Hanada, S.; Saito, N.; Kadota, T.; Wakui, H.; et al. Pathogens in COPD exacerbations identified by comprehensive real-time PCR plus older methods. Int. J. Chronic Obstr. Pulm. Dis. 2015, 10, 2009–2016. [Google Scholar] [CrossRef]
- Albertson, T.E.; Louie, S.; Chan, A.L. The Diagnosis and Treatment of Elderly Patients with Acute Exacerbation of Chronic Obstructive Pulmonary Disease and Chronic Bronchitis. J. Am. Geriatr. Soc. 2010, 58, 570–579. [Google Scholar] [CrossRef] [PubMed]
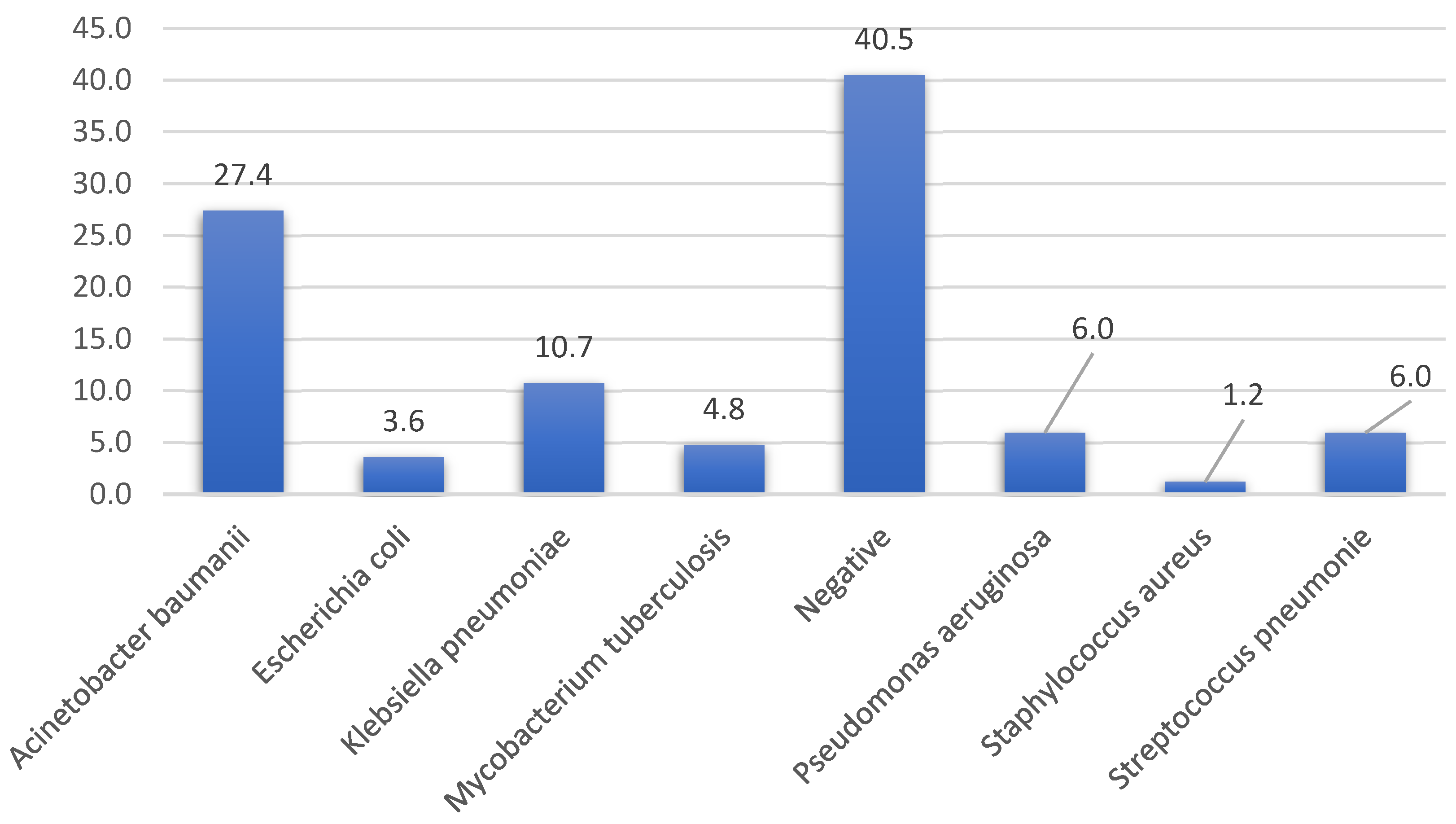
| Bacteriologic Agent | Acinetobacter baumanii | E. coli | Klebsiella pneumoniae | M. tuberculosis | Pseudomonas aeruginosa | Staph. aureus | Strep. pneumoniae | p *** |
|---|---|---|---|---|---|---|---|---|
| WBC count ×103/μL | 15.1 (14.3–17.5) | 24.5 (19.3–27.8) | 13.4 (13.0–13.8) | 12.2 (12.1–12.3) | 16.1 (14.9–16.7) | 12.3 (12.3–12.3) | 12.6 (12.4–14.7) | <0.001 |
| Bacteriologic Agent | Acinetobacter baumanii | E. coli | Klebsiella pneumoniae | M. tuberculosis | Pseudomonas aeruginosa | Staph. aureus | Strep. pneumoniae | p *** |
|---|---|---|---|---|---|---|---|---|
| CRP value | 1582 (1536–1682) | 578 (571–589) | 581 (550–730) | 1223 (1173–1348) | 906 (871–934) | 875 (821–954( | 605 (569–645) | <0.001 |
| Ventilation Mode | Acinetobacter baumanii | E. coli | Klebsiella pneumoniae | M. tuberculosis | Pseudomonas aeruginosa | Staph. aureus | Strep. pneumoniae | p * |
|---|---|---|---|---|---|---|---|---|
| OTI n (%) | 23 (100%) | 1 (33.3%) | 8 (88.9%) | 0 (0%) | 3 (60%) | 1 (100%) | 4 (80%) | <0.001 |
| Facial mask n (%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | |
| NIV n (%) | 0 (0%) | 2 (66.7%) | 1 (11.1%) | 3 (75%) | 2 (40%) | 0 (0%) | 1 (20%) |
| Superinfection Pathogen | Stable State n (%) | Deceased n (%) | p * |
|---|---|---|---|
| Acinetobacter baumani | 3 (9.1%) | 20 (39.2%) | <0.01 |
| E. coli | 0 (0%) | 3 (5.9%) | |
| Klebsiella pneumonie | 4 (12.1%) | 5 (9.8%) | |
| Mycobacterium tuberculosis | 2 (6.1%) | 2 (3.9%) | |
| Negative | 22 (66.7%) | 12 (23.5%) | |
| Pseudomonas aeruginosa | 1 (3%) | 4 (7.8%) | |
| Staph. aureus | 0 (0%) | 1 (2%) | |
| Strep. pneumonie | 1 (3%) | 4 (7.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huțanu, D.; Sárközi, H.-K.; Vultur, M.A.; Sabău, A.-H.; Cocuz, I.G.; Mărginean, C.; Chelemen, A.-M.; Budin, C.E. Analyzing Clinical Parameters and Bacterial Profiles to Uncover the COPD Exacerbations: A Focus on Intensive Care Unit Challenges. Medicina 2025, 61, 669. https://doi.org/10.3390/medicina61040669
Huțanu D, Sárközi H-K, Vultur MA, Sabău A-H, Cocuz IG, Mărginean C, Chelemen A-M, Budin CE. Analyzing Clinical Parameters and Bacterial Profiles to Uncover the COPD Exacerbations: A Focus on Intensive Care Unit Challenges. Medicina. 2025; 61(4):669. https://doi.org/10.3390/medicina61040669
Chicago/Turabian StyleHuțanu, Dragoș, Hédi-Katalin Sárközi, Mara Andreea Vultur, Adrian-Horațiu Sabău, Iuliu Gabriel Cocuz, Corina Mărginean, Andra-Maria Chelemen, and Corina Eugenia Budin. 2025. "Analyzing Clinical Parameters and Bacterial Profiles to Uncover the COPD Exacerbations: A Focus on Intensive Care Unit Challenges" Medicina 61, no. 4: 669. https://doi.org/10.3390/medicina61040669
APA StyleHuțanu, D., Sárközi, H.-K., Vultur, M. A., Sabău, A.-H., Cocuz, I. G., Mărginean, C., Chelemen, A.-M., & Budin, C. E. (2025). Analyzing Clinical Parameters and Bacterial Profiles to Uncover the COPD Exacerbations: A Focus on Intensive Care Unit Challenges. Medicina, 61(4), 669. https://doi.org/10.3390/medicina61040669






