Self-Management of Medications During Sick Days for Chronic Conditions: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Identifying the Research Question
2.2. Search Strategy and Eligibility Criteria
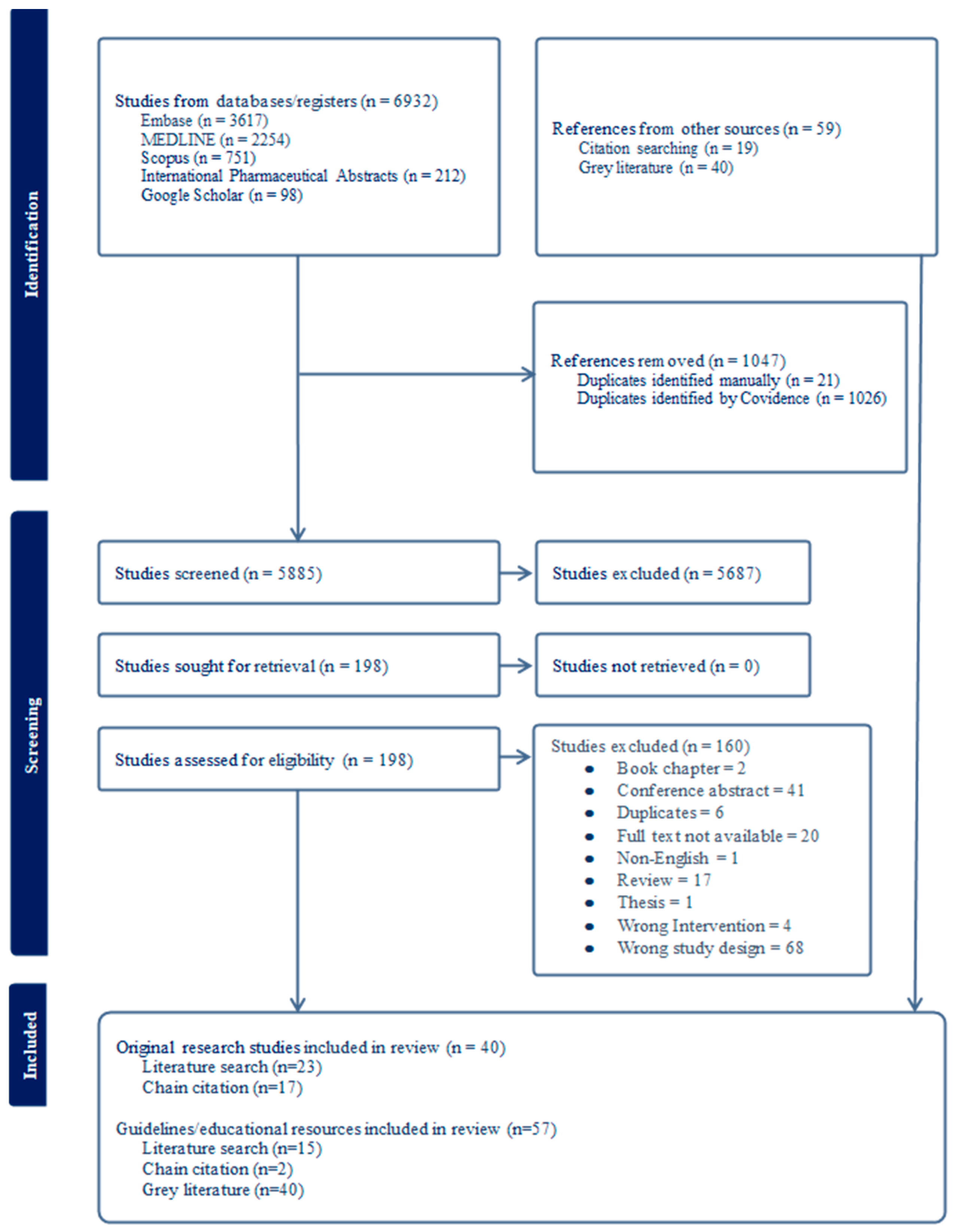
2.3. Study Selection, Data Extraction, and Analysis
3. Results
3.1. Document Characteristics—Original Research
3.2. Sick-Day Definition
3.3. Interventions Addressing Sick-Day Medication Management
3.4. Patient Engagement and Capability
3.5. Patient Experiences and Perceptions of Sick-Day Interventions
3.6. Outcomes Measured
3.6.1. Patient-Centred Outcomes
3.6.2. Healthcare System Utilisation
3.7. Healthcare Professional Experiences and Perceptions of Sick-Day Interventions
3.8. Document Characteristics—Guidelines and Educational Resources
4. Discussion
4.1. Interventions Available
4.2. Benefits and Practical Applications
4.3. Potential Risks and Harms
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AKI | Acute kidney injury |
| AI | Adrenal insufficiency |
| CKD | Chronic kidney disease |
| COPD | Chronic obstructive pulmonary disease |
| DRPs | Drug-related problems |
| HCPs | Healthcare professionals |
| N/A | Not available |
| PEF | Peak expiratory flow |
| SDMG | Sick-day medication guidance |
| T1DM | Type 1 diabetes mellitus |
| T2DM | Type 2 diabetes mellitus |
| TIDieR | Template for Intervention Description and Replication |
| GP | General practice/general practitioner |
References
- Australian Institute of Health and Welfare. Chronic Conditions and Multimorbidity; AIHW: Canberra, Australia, 2023.
- Lim, R.; Ellett, L.M.K.; Semple, S.; Roughead, E.E. The Extent of Medication-Related Hospital Admissions in Australia: A Review from 1988 to 2021. Drug Saf. 2022, 45, 249–257. [Google Scholar] [CrossRef]
- Lea-Henry, T.N.; Baird-Gunning, J.; Petzel, E.; Roberts, D.M. Medication management on sick days. Aust. Prescr. 2017, 40, 168–173. [Google Scholar] [CrossRef]
- Scarfone, R.J.; Zorc, J.J.; Capraro, G.A. Patient self-management of acute asthma: Adherence to national guidelines a decade later. Pediatrics 2001, 108, 1332–1338. [Google Scholar] [CrossRef]
- Duong, H.; Tesfaye, W.; Van, C.; Sud, K.; Truong, M.; Krass, I.; Castelino, R.L. Sick day management in people with chronic kidney disease: A scoping review. J. Nephrol. 2022, 1293–1306. [Google Scholar] [CrossRef] [PubMed]
- de Lemos, J.; Loewen, P.; Nagle, C.; McKenzie, R.; You, Y.D.; Dabu, A.; Zed, P.; Ling, P.; Chan, R. Preventable adverse drug events causing hospitalisation: Identifying root causes and developing a surveillance and learning system at an urban community hospital, a cross-sectional observational study. BMJ Open Qual. 2021, 10, e001161. [Google Scholar] [CrossRef] [PubMed]
- Watson, K.E.; Dhaliwal, K.; McMurtry, E.; Donald, T.; Lamont, N.; Benterud, E.; Kung, J.Y.; Robertshaw, S.; Verdin, N.; Drall, K.M.; et al. Sick Day Medication Guidance for People With Diabetes, Kidney Disease, or Cardiovascular Disease: A Systematic Scoping Review. Kidney Med. 2022, 4, 100491. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Marnie, C.; Tricco, A.C.; Pollock, D.; Munn, Z.; Alexander, L.; McInerney, P.; Godfrey, C.M.; Khalil, H. Updated methodological guidance for the conduct of scoping reviews. JBI Evid. Synth. 2020, 18, 2119–2126. [Google Scholar]
- Helbach, J.; Pieper, D.; Mathes, T.; Rombey, T.; Zeeb, H.; Allers, K.; Hoffmann, F. Restrictions and their reporting in systematic reviews of effectiveness: An observational study. BMC Med. Res. Methodol. 2022, 22, 230. [Google Scholar] [CrossRef]
- Covidence. Covidence. Available online: www.covidence.org (accessed on 1 April 2024).
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ Br. Med. J. 2014, 348, g1687. [Google Scholar] [CrossRef] [PubMed]
- Charlton, I.; Antoniou, A.G.; Atkinson, J.; Campbell, M.; Chapman, E.; Mackintosh, T.; Schapira, D. Asthma at the interface: Bridging the gap between general practice and a district general hospital. Arch. Dis. Child. 1994, 70, 313–318. [Google Scholar] [CrossRef]
- Thoonen, B.P.; Schermer, T.R.; Jansen, M.; Smeele, I.; Jacobs, A.J.; Grol, R.; van Schayck, O.C. Asthma education tailored to individual patient needs can optimise partnerships in asthma self-management. Patient Educ. Couns. 2002, 47, 355–360. [Google Scholar] [CrossRef]
- D’Souza, W.; Crane, J.; Burgess, C.; Te Karu, H.; Fox, C.; Harper, M.; Robson, B.; Howden-Chapman, P.; Crossland, L.; Woodman, K. Community-based asthma care: Trial of a “credit card” asthma self-management plan. Eur. Respir. J. 1994, 7, 1260–1265. [Google Scholar] [CrossRef] [PubMed]
- Van der Palen, J.; Klein, J.; Rovers, M. Compliance with inhaled medication and self-treatment guidelines following a self-management programme in adult asthmatics. Eur. Respir. J. 1997, 10, 652–657. [Google Scholar] [CrossRef] [PubMed]
- Côté, J.; Cartier, A.; Malo, J.-L.; Rouleau, M.; Boulet, L.-P. Compliance with peak expiratory flow monitoring in home management of asthma. Chest 1998, 113, 968–972. [Google Scholar] [CrossRef] [PubMed]
- Yoon, R.; McKenzie, D.; Bauman, A.; Miles, D. Controlled trial evaluation of an asthma education programme for adults. Thorax 1993, 48, 1110. [Google Scholar] [CrossRef]
- Wilson, S.R.; Scamagas, P.; German, D.F.; Hughes, G.W.; Lulla, S.; Coss, S.; Chardon, L.; Thomas, R.G.; Starr-Schneidkraut, N.; Stancavage, F.B. A controlled trial of two forms of self-management education for adults with asthma. Am. J. Med. 1993, 94, 564–576. [Google Scholar] [CrossRef]
- Cowie, R.L.; Revitt, S.G.; Underwood, M.F.; Field, S.K. The effect of a peak flow-based action plan in the prevention of exacerbations of asthma. Chest 1997, 112, 1534–1538. [Google Scholar] [CrossRef]
- Charlton, I.; Charlton, G.; Broomfield, J.; Mullee, M.A. Evaluation of peak flow and symptoms only self management plans for control of asthma in general practice. BMJ 1990, 301, 1355–1359. [Google Scholar] [CrossRef]
- Cote, J.; Bowie, D.M.; Robichaud, P.; Parent, J.-G.; Battisti, L.; Boulet, L.-P. Evaluation of two different educational interventions for adult patients consulting with an acute asthma exacerbation. Am. J. Respir. Crit. Care Med. 2001, 163, 1415–1419. [Google Scholar] [CrossRef]
- Gallefoss, F.; Bakke, P.S. How does patient education and self-management among asthmatics and patients with chronic obstructive pulmonary disease affect medication? Am. J. Respir. Crit. Care Med. 1999, 160, 2000–2005. [Google Scholar] [CrossRef]
- Madge, P.; McColl, J.; Paton, J. Impact of a nurse-led home management training programme in children admitted to hospital with acute asthma: A randomised controlled study. Thorax 1997, 52, 223–228. [Google Scholar] [CrossRef]
- Kovačević, M.; Ćulafić, M.; Jovanović, M.; Vučićević, K.; Kovačević, S.V.; Miljković, B. Impact of community pharmacists’ interventions on asthma self-management care. Res. Soc. Adm. Pharm. 2018, 14, 603–611. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Mullee, M.; Middleton, M.; Chapman, E.; Holgate, S. Peak flow based asthma self-management: A randomised controlled study in general practice. British Thoracic Society Research Committee. Thorax 1995, 50, 851–857. [Google Scholar] [CrossRef] [PubMed]
- Wong, L.-Y.; Chua, S.-S.; Husin, A.-R.; Arshad, H. A pharmacy management service for adults with asthma: A cluster randomised controlled trial. Fam. Pract. 2017, 34, 564–573. [Google Scholar] [CrossRef]
- Lahdensuo, A.; Haahtela, T.; Herrala, J.; Kava, T.; Kiviranta, K.; Kuusisto, P.; Peramaki, E.; Poussa, T.; Saarelainen, S.; Svahn, T. Randomised comparison of guided self management and traditional treatment of asthma over one year. BMJ 1996, 312, 748–752. [Google Scholar] [CrossRef] [PubMed]
- Beasley, R.; Cushley, M.; Holgate, S. A self management plan in the treatment of adult asthma. Thorax 1989, 44, 200–204. [Google Scholar] [CrossRef]
- Klein, J.J.; van der Palen, J.; van den Hof, S.; Rovers, M.M. Self-treatment by adults during slow-onset exacerbations of asthma. Patient Educ. Couns. 1997, 32, S61–S66. [Google Scholar] [CrossRef]
- Fireman, P.; Friday, G.A.; Gira, C.; Vierthaler, W.A.; Michaels, L. Teaching self-management skills to asthmatic children and their parents in an ambulatory care setting. Pediatrics 1981, 68, 341–348. [Google Scholar] [CrossRef]
- Garrett, J.; Williams, S.; Wong, C.; Holdaway, D. Treatment of acute asthmatic exacerbations with an increased dose of inhaled steroid. Arch. Dis. Child. 1998, 79, 12–17. [Google Scholar] [CrossRef]
- Campain, A.; Mulley, J.; Angell, B.; Ewald, D.; Carter, B.; Rose, V.; Wilcox, K.; Wheeler, M.; Peiris, D. The Winter Strategy—A Multifaceted Integrated Care Intervention to Support People with Chronic and Complex Care Needs during the Australian Winter Period. Int. J. Integr. Care 2023, 23, 12. [Google Scholar] [CrossRef]
- Watson, P.; Town, G.; Holbrook, N.; Dwan, C.; Toop, L.; Drennan, C. Evaluation of a self-management plan for chronic obstructive pulmonary disease. Eur. Respir. J. 1997, 10, 1267–1271. [Google Scholar] [CrossRef]
- Sridhar, M.; Taylor, R.; Dawson, S.; Roberts, N.J.; Partridge, M.R. A nurse led intermediate care package in patients who have been hospitalised with an acute exacerbation of chronic obstructive pulmonary disease. Thorax 2008, 63, 194–200. [Google Scholar] [CrossRef]
- Bourbeau, J.; Julien, M.; Maltais, F.; Rouleau, M.; Beaupré, A.; Bégin, R.; Renzi, P.; Nault, D.; Borycki, E.; Schwartzman, K. Reduction of hospital utilization in patients with chronic obstructive pulmonary disease: A disease-specific self-management intervention. Arch. Intern. Med. 2003, 163, 585–591. [Google Scholar] [CrossRef] [PubMed]
- Sedeno, M.F.; Nault, D.; Hamd, D.H.; Bourbeau, J. A self-management education program including an action plan for acute COPD exacerbations. COPD: J. Chronic Obstr. Pulm. Dis. 2009, 6, 352–358. [Google Scholar] [CrossRef] [PubMed]
- McGeoch, G.R.; Willsman, K.J.; Dowson, C.A.; Town, G.I.; Frampton, C.M.; McCartin, F.J.; Cook, J.M.; Epton, M.J. Self-management plans in the primary care of patients with chronic obstructive pulmonary disease. Respirology 2006, 11, 611–618. [Google Scholar] [CrossRef]
- Wood-Baker, R.; McGlone, S.; Venn, A.; Walters, E.H. Written action plans in chronic obstructive pulmonary disease increase appropriate treatment for acute exacerbations. Respirology 2006, 11, 619–626. [Google Scholar] [CrossRef] [PubMed]
- Fink, J.C.; Maguire, R.M.; Blakeman, T.; Tomlinson, L.A.; Tomson, C.; Wagner, L.-A.; Zhan, M. Medication holds in CKD during acute volume-depleting illnesses: A randomized controlled trial of a “sick-day” protocol. Kidney Med. 2022, 4, 100527. [Google Scholar] [CrossRef]
- Bowman, C.; Lunyera, J.; Alkon, A.; Boulware, L.E.; Russell, J.S.C.; Riley, J.; Fink, J.C.; Diamantidis, C. A patient safety educational tool for patients with chronic kidney disease: Development and usability study. JMIR Form. Res. 2020, 4, e16137. [Google Scholar] [CrossRef]
- Vicary, D.; Hutchison, C.; Aspden, T. Demonstrating the value of community pharmacists in New Zealand educating a targeted group of people to temporarily discontinue medicines when they are unwell to reduce the risk of acute kidney injury. Int. J. Pharm. Pract. 2020, 28, 569–578. [Google Scholar] [CrossRef]
- Morrison, C.; Wilson, M. Medicine Sick Day Rules Cards–Interim Evaluation. NHS Highland. 2014. Available online: https://margaretmccartney.com/wp-content/uploads/2014/10/NHSH-interim-evaluation-medicine-sick-day-rules.pdf (accessed on 2 March 2025).
- Wang, T.; Kang, H.-C.; Wu, C.-C.; Wu, T.-L.; Huang, C.-F.; Wu, V.-C. The effect of pharmacist-led medication therapy management in the multidisciplinary care of acute kidney injury survivors. Kidney Res. Clin. Pract. 2024, 43, 548. [Google Scholar] [CrossRef] [PubMed]
- Vitale, R.J.; Card, C.E.; Lichtman, J.H.; Weyman, K.; Michaud, C.; Sikes, K.; Tamborlane, W.V.; Weinzimer, S.A. An effective diabetic ketoacidosis prevention intervention in children with type 1 diabetes. SAGE Open Nurs. 2018, 4, 2377960818804742. [Google Scholar] [CrossRef] [PubMed]
- Kime, N.; Zwolinsky, S.; Pringle, A. Evaluation of the DigiBete app, a self-management app for type 1 diabetes: Experiences of young people, families, and healthcare professionals. Children 2023, 10, 1933. [Google Scholar] [CrossRef]
- Dye, A.M.; Alemzadeh, R.; Wang, J.; Tolley, E.A.; Lahoti, A. Intensive sick day rules to prevent recurrent diabetic ketoacidosis-An intervention that exemplifies health disparities. J. Natl. Med. Assoc. 2022, 114, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Farrell, K.; Holmes–Walker, D. Mobile phone support is associated with reduced ketoacidosis in young adults. Diabet. Med. 2011, 28, 1001–1004. [Google Scholar] [CrossRef]
- Pichert, J.W.; Snyder, G.M.; Kinzer, C.K.; Boswell, E.J. Problem solving anchored instruction about sick days for adolescents with diabetes. Patient Educ. Couns. 1994, 23, 115–124. [Google Scholar] [CrossRef]
- Farrell, K.; Brunero, S.; Holmes-Walker, D.J.; Griffiths, R.; Salamonson, Y. Self-management of sick days in young people with type 1 diabetes enhanced by phone support: A qualitative study. Contemp. Nurse 2019, 55, 171–184. [Google Scholar] [CrossRef]
- Kado, K.; Okada, H.; Suzuki, S.; Satake, M.; Yamazaki, T.; Kurosawa, M.; Yamamoto, M.; Takahashi, M.; Nakayama, T. Study of assessment of knowledge and understanding for coping with sick days among patients with diabetes in community pharmacy: A cluster randomized controlled trial (SAKURA trial). J. Pharm. Policy Pract. 2023, 16, 104. [Google Scholar] [CrossRef]
- Herges, J.R.; May, H.P.; Meade, L.; Anderson, B.; Tinaglia, A.G.; Schreier, D.J.; Kashani, K.B.; Kattah, A.; McCoy, R.G.; Rule, A.D.; et al. Pharmacist-provider collaborative visits after hospital discharge in a comprehensive acute kidney injury survivor model. J. Am. Pharm. Assoc. 2023, 63, 909–914. [Google Scholar] [CrossRef]
- Tse, M.; Bridges-Webb, C. Asthma management in general practice. Med. J. Aust. 1993, 158, 766–770. [Google Scholar] [CrossRef]
- Roy, S.R.; Milgrom, H. Managing outpatient asthma exacerbations. Curr. Allergy Asthma Rep. 2003, 3, 179–189. [Google Scholar] [CrossRef]
- Mahesh, S.; Ramamurthy, M.B. Management of Acute Asthma in Children. Indian J. Pediatr. 2022, 89, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Lahdensuo, A. Guided self management of asthma—How to do it. BMJ 1999, 319, 759. [Google Scholar] [CrossRef] [PubMed]
- Asthma Australia. Asthma Action Plan. Available online: https://asthma.org.au/manage-asthma/asthma-action-plan/ (accessed on 4 March 2025).
- National Asthma council Australia. Asthma Action Plans. Available online: https://www.nationalasthma.org.au/health-professionals/asthma-action-plans (accessed on 6 April 2025).
- Asthma and Allergy Foundation of America. Asthma Action Plan. Available online: https://aafa.org/asthma/asthma-treatment/asthma-treatment-action-plan/ (accessed on 6 March 2025).
- American Lung Association. Create an Asthma Action Plan. Available online: https://www.lung.org/lung-health-diseases/lung-disease-lookup/asthma/managing-asthma/create-an-asthma-action-plan (accessed on 5 April 2025).
- Asthma and Respiratory Foundation New Zealand. AIR Asthma Action Plan. Available online: https://www.asthmafoundation.org.nz/resources/air-asthma-action-plans (accessed on 22 March 2025).
- Asthma Canada. Asthma Action Plan. Available online: https://asthma.ca/get-help/living-with-asthma/asthma-action-plan/ (accessed on 22 March 2025).
- Asthma United Kingdom. Your Asthma Action Plan. Available online: https://www.brit-thoracic.org.uk/media/70105/annex-3-asthma-action-and-recovery-plans.pdf (accessed on 22 March 2025).
- Asthma and Allergy Network. SMART Asthma Action Plan. Available online: https://allergyasthmanetwork.org/images/Asthma/SMART_Action_Plan_Dec2022.pdf (accessed on 13 March 2025).
- Breathe The Lung Association. Adult Asthma Action Plan. Available online: https://www.lung.ca/sites/default/files/Adult%20Asthma%20Action%20Plan%202778%20%28AODA%20compliant%29%20%281%29.pdf (accessed on 15 March 2025).
- Royal College of Paediatrics and Child Health. Asthma Action Plan. Available online: https://nenc-healthiertogether.nhs.uk/professionals/safety-netting-and-parent-information-leaflets-pil/asthma-action-plan (accessed on 6 April 2025).
- Wiebke Arlt, S.P.; Simpson, H.; Wass, J. Sick Day Rules. Available online: https://www.addisonsdisease.org.uk/newly-diagnosed-sick-day-rules (accessed on 3 March 2025).
- Society for Endocrinology. Steroid Sick Day Rules. Available online: https://www.endocrinology.org/media/4169/ai-and-exogenous-steroids_patient-information-sheet.pdf (accessed on 6 March 2025).
- Endocrine Society of Australia. Sick Day Management for Patients on Glucocorticoid Therapy. Available online: https://www.hormones-australia.org.au/wp-content/uploads/2020/11/Sick-Day-Management-Plan-FINAL-fillable.pdf (accessed on 10 March 2025).
- The Pituitary Foundation. Steroid Sick Day Rules (Hydocortisone and Prednisolone). Available online: https://www.pituitary.org.uk/app/uploads/2025/03/HYDROCORTISONE-SICK-DAY-RULES_Feb-2025-update.pdf (accessed on 6 March 2025).
- Justin Davies, D.L. Management of Sick Day Episodes in Children and Young People Treated with Regular Glucocorticoids. Available online: https://www.piernetwork.org/sick-day-steroids.html (accessed on 6 March 2025).
- King’s College Hospital. Adrenal Insufficiency—How to Stay Safe on Steroids. Available online: https://www.kch.nhs.uk/wp-content/uploads/2023/01/pl-1098.1-adrenal-insufficiency-%E2%80%93-how-to-stay-safe-on-steroids.pdf (accessed on 3 March 2025).
- Worcestershire Acute Hospitals. Adrenal Insufficiency Sick Day Rule Information. Available online: https://www.worcsacute.nhs.uk/documents/documents/patient-information-leaflets-a-z/adrenal-insufficiency-sick-day-rule-information-information-for-patients-on-long-term-steroid-hormone-replacement-therapy/?layout=file (accessed on 6 March 2025).
- The Royal Children’s Hospital Melbourne. Adrenal Crisis and Acute Adrenal Insufficiency. Available online: https://www.rch.org.au/clinicalguide/guideline_index/Adrenal_crisis_and_acute_adrenal_insufficiency/ (accessed on 14 March 2025).
- NHS Highland. Steroid Treatment Advice for Adults During Intercurrent Illness (When You Are Unwell). Available online: https://patientinfo.nhshighland.scot.nhs.uk/TAM401-499/TAM452%20sterioid%20treatment%20advice.pdf (accessed on 7 March 2025).
- Amelia Cook, M.S.; Kaur, G. Sick Day Rules: How To Manage Type 2 Diabetes If You Become Unwell with Coronavirus and What to Do with Your Medication. Available online: https://www.england.nhs.uk/midlands/wp-content/uploads/sites/46/2020/11/Covid-19-Sick-Day-Rules-T2DM.pdf (accessed on 3 April 2025).
- Gurpreet Kaur, S.C. Primary Care Sick Day Guidance for the Management of Adult Patients with Diabetes Mellitus. Available online: https://sandwellandwestbhamccgformulary.nhs.uk/docs/Encs2c_BSSEAPC%20DMMAG%20Primary%20Care%20Sick%20Day%20Information%20for%20Adult%20patients%20with%20diabetes%20v10.pdf (accessed on 10 March 2025).
- Diabetes Canada. Diabetes Canada 2018 Clinical Practice Guidelines for the Prevention and Management of Diabetes in Canada. Available online: https://guidelines.diabetes.ca/appendices/appendix8 (accessed on 4 April 2025).
- Diabetes Canada. Stay Safe When You Have Diabetes and Are Sick or at Risk of Dehydration. Available online: https://www.diabetes.ca/DiabetesCanadaWebsite/media/Managing-My-Diabetes/Tools%20and%20Resources/stay-safe-when-you-have-diabetes-and-sick-or-at-risk-of-dehydration.pdf?ext=.pdf (accessed on 4 April 2025).
- Rx Files. Type 2 Diabetes and Sick Days Medications to Pause. Available online: https://www.rxfiles.ca/rxfiles/uploads/documents/SADMANS-Rx.pdf (accessed on 5 April 2025).
- Baker Heart and Diabetes Institute. Type 2 Diabetes and Sick Day Management. Available online: https://baker.edu.au/-/media/documents/fact-sheets/baker-institute-factsheet-type2-diabetes-sickday-management.pdf (accessed on 14 March 2025).
- Ponen, S. Diabetes—Type 2 Sick Day Plan. Available online: https://healthify.nz/health-a-z/d/diabetes-type-2-sick-day-plan (accessed on 6 April 2025).
- Australian Diabetes Educators Association. Managing Sick Days for Adults with Type 2 Diabetes Who Use Insulin. Available online: https://www.integratedspecialistmedicalcare.com.au/wp-content/uploads/2022/12/Consumer_03_03.pdf (accessed on 9 March 2025).
- New Zealand Society for the Study of Diabetes. Sick Day Management in Patients with Diabetes. Available online: https://t2dm.nzssd.org.nz/Section-95-Sick-day-management-in-patients-with-diabetes (accessed on 4 April 2025).
- Laffel, L.M.; Limbert, C.; Phelan, H.; Virmani, A.; Wood, J.; Hofer, S.E. ISPAD Clinical Practice Consensus Guidelines 2018: Sick day management in children and adolescents with diabetes. Pediatr. Diabetes 2018, 19, 193–204. [Google Scholar] [CrossRef]
- Bismuth, E.; Laffel, L. Can we prevent diabetic ketoacidosis in children? Pediatr. Diabetes 2007, 8, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Brink, S.; Joel, D.; Laffel, L.; Lee, W.W.R.; Olsen, B.; Phelan, H.; Hanas, R. Sick day management in children and adolescents with diabetes. Pediatr. Diabetes 2014, 15, 193–202. [Google Scholar] [CrossRef]
- Laffel, L. Sick-Day Management in Type 1 Diabetes. Endocrinol. Metab. Clin. North Am. 2000, 29, 707–723. [Google Scholar] [CrossRef]
- Miles, J.M.; Jensen, M.D. Complications of Insulin-Dependent Diabetes Mellitus: Management of Insulin Reactions and Acute Illness. Mayo Clin. Proc. 1986, 61, 820–824. [Google Scholar] [CrossRef]
- Trend Diabetes. Managing Diabetes During Intercurrent Illness. Available online: https://trenddiabetes.online/wp-content/uploads/2022/04/HCP_Illness_TREND_2022.pdf (accessed on 13 March 2025).
- Diabetes UK. Diabetes When You’re Unwell. Available online: https://www.diabetes.org.uk/living-with-diabetes/life-with-diabetes/illness (accessed on 1 April 2025).
- Royal Australian College of General Practitioners. Diabetes Sick-Day Management. Available online: https://www.racgp.org.au/getattachment/93adfae0-c1ed-4388-8f7e-ff068b8bb9ec/Diabetes-sick-day-management.pdf.aspx (accessed on 1 April 2025).
- NovoCare. Managing Diabetes Safely During Sick Days. Available online: https://www.novomedlink.com/content/dam/novonordisk/novomedlink/new/diabetes/patient/disease/library/documents/managing-diabetes-safely-during-sick-days.pdf (accessed on 3 April 2025).
- Lung Foundation Australia. COPD Action Plan. Available online: https://lungfoundation.com.au/support-resources/resource-hub/copd-action-plan-2/ (accessed on 3 March 2025).
- American Lung Association. COPD Action Plan & Management Tools. Available online: https://www.lung.org/lung-health-diseases/lung-disease-lookup/copd/living-with-copd/copd-management-tools (accessed on 10 March 2025).
- Kidney Health Australia. How to Sick Day Action Plan. Available online: https://assets.kidney.org.au/resources/KHA-How-To-Sick-Day-Action-Plan-FINAL.pdf (accessed on 9 March 2025).
- Stevens, P.E.; Ahmed, S.B.; Carrero, J.J.; Foster, B.; Francis, A.; Hall, R.K.; Herrington, W.G.; Hill, G.; Inker, L.A.; Kazancıoğlu, R.; et al. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [Google Scholar] [CrossRef]
- Kidney Health: At Home Sick Day Advice HE2647. Available online: https://healthed.govt.nz/products/kidney-health-at-home-sick-day-advice-he2647 (accessed on 18 March 2025).
- London Kidney Network. Sick Day Medication Guidance in Chronic Kidney Disease. Available online: https://londonkidneynetwork.nhs.uk/wp-content/uploads/2024/04/Sick-Day-Rules.pdf (accessed on 21 March 2025).
- Arnold, J.M.O.; Howlett, J.G.; Dorian, P.; Ducharme, A.; Giannetti, N.; Haddad, H.; Heckman, G.A.; Ignaszewski, A.; Isaac, D.; Jong, P. Canadian Cardiovascular Society Consensus Conference recommendations on heart failure update 2007: Prevention, management during intercurrent illness or acute decompensation, and use of biomarkers. Can. J. Cardiol. 2007, 23, 21–45. [Google Scholar] [CrossRef]
- Rx Files. What To Do with Heart Failure Medications If I’m Sick. Available online: https://www.rxfiles.ca/rxfiles/uploads/documents/Heart-Failure-Sick-Days.pdf (accessed on 2 March 2025).
- Sylvian Cote, S.W. How to Manage Your Heart Failure Medication on Sick Days? Available online: https://heartfailure.ca/sites/default/files/sick_days_hf_tool_021221.pdf (accessed on 2 March 2025).
- Scottish Government Polypharmacy Model of Care Group. Polypharmacy Guidance, Realistic Prescribing; Scottish Government: Edinburgh, UK, 2018.
- Duck, B.; Albertyn, R.; Vicary, D.; Jones, J.; Firestone, S.; Firestone, B.; Adie, M.; McNeill, R.; Spedding, T.; Milman, O.; et al. Managing Medicines During ‘Sick Days’. Available online: https://healthhb.co.nz/wp-content/uploads/2023/12/Best-Practice-Managing-Medicines-During-Sick-Days.pdf (accessed on 25 March 2025).
- Think Kidneys. “Sick Day” Guidance in Patients at Risk of Acute Kidney Injury: A Position Statement from the Think Kidneys Board. Available online: https://www.thinkkidneys.nhs.uk/aki/wp-content/uploads/sites/2/2018/01/Think-Kidneys-Sick-Day-Guidance-2018.pdf (accessed on 22 March 2025).
- Battersby, M.W.; Ask, A.; Reece, M.M.; Markwick, M.J.; Collins, J.P. The Partners in Health scale: The development and psychometric properties of a generic assessment scale for chronic condition self-management. Aust. J. Prim. Health 2003, 9, 41–52. [Google Scholar] [CrossRef]
- Grady, P.A.; Gough, L.L. Self-management: A comprehensive approach to management of chronic conditions. Am. J. Public Health 2014, 104, e25–e31. [Google Scholar] [CrossRef]
- Duong, H.; Tesfaye, W.; Van, C.; Sud, K.; Castelino, R.L. Hospitalisation Due to Community-Acquired Acute Kidney Injury and the Role of Medications: A Retrospective Audit. J. Clin. Med. 2023, 12, 3347. [Google Scholar] [CrossRef]
- Shepherd, L.M.; Schmidtke, K.A.; Hazlehurst, J.M.; Melson, E.; Dretzke, J.; Hawks, N.; Arlt, W.; Tahrani, A.A.; Swift, A.; Carrick-Sen, D.M. Interventions for the prevention of adrenal crisis in adults with primary adrenal insufficiency: A systematic review. Eur. J. Endocrinol. 2022, 187, S1–S20. [Google Scholar] [CrossRef] [PubMed]
- Harrison, S.L.; Janaudis-Ferreira, T.; Brooks, D.; Desveaux, L.; Goldstein, R.S. Self-Management Following an Acute Exacerbation of COPD: A Systematic Review. Chest 2015, 147, 646–661. [Google Scholar] [CrossRef]
- Martindale, A.M.; Elvey, R.; Howard, S.J.; McCorkindale, S.; Sinha, S.; Blakeman, T. Understanding the implementation of ’sick day guidance’ to prevent acute kidney injury across a primary care setting in England: A qualitative evaluation. BMJ Open 2017, 7, e017241. [Google Scholar] [CrossRef]
- Morris, R.L.; Ashcroft, D.; Phipps, D.; Bower, P.; O’Donoghue, D.; Roderick, P.; Harding, S.; Lewington, A.; Blakeman, T. Preventing Acute Kidney Injury: A qualitative study exploring ‘sick day rules’ implementation in primary care. BMC Fam. Pract. 2016, 17, 91. [Google Scholar] [CrossRef]
- Reeder, K.M.; Ercole, P.M.; Peek, G.M.; Smith, C.E. Symptom Perceptions and Self-care Behaviors in Patients Who Self-manage Heart Failure. J. Cardiovasc. Nurs. 2015, 30, E1–E7. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, S.M. Action plans, self-monitoring and adherence: Changing behaviour to promote better self-management. Med. J. Aust. 2002, 177, S72–S74. [Google Scholar] [CrossRef] [PubMed]
- The Australian Digital Health Agency. My Health Record. Available online: https://www.digitalhealth.gov.au/healthcare-providers/initiatives-and-programs/my-health-record (accessed on 26 June 2025).
- Taylor, D.M.; Fraser, S.D.S.; Bradley, J.A.; Bradley, C.; Draper, H.; Metcalfe, W.; Oniscu, G.C.; Tomson, C.R.V.; Ravanan, R.; Roderick, P.J.; et al. A Systematic Review of the Prevalence and Associations of Limited Health Literacy in CKD. Clin. J. Am. Soc. Nephrol. 2017, 12, 1070–1084. [Google Scholar] [CrossRef]
- Fraser, S.D.S.; Roderick, P.J.; Casey, M.; Taal, M.W.; Yuen, H.M.; Nutbeam, D. Prevalence and associations of limited health literacy in chronic kidney disease: A systematic review. Nephrol. Dial. Transplant. 2013, 28, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Lorig, K.R.; Holman, H.R. Self-management education: History, definition, outcomes, and mechanisms. Ann. Behav. Med. 2003, 26, 1–7. [Google Scholar] [CrossRef]
- Dhaliwal, K.K.; Watson, K.E.; Lamont, N.C.; Drall, K.M.; Donald, M.; James, M.T.; Robertshaw, S.; Verdin, N.; Benterud, E.; McBrien, K.; et al. Managing ‘sick days’ in patients with chronic conditions: An exploration of patient and healthcare provider experiences. Health Expect. 2023, 26, 1746–1756. [Google Scholar] [CrossRef]
- Coppes, T.; Philbert, D.; van Gelder, T.; Bouvy, M.L.; Koster, E.S. Medication management during sick days: No differences between patients with and without impaired renal function. Eur. J. Clin. Invest. 2024, 54, e14231. [Google Scholar] [CrossRef] [PubMed]
- Calleja, L.; Glass, B.; Taylor, S.; Neville, K.; Brown, L.; Miller, A.; Cairns, A. Sick Day Management Plans for Aboriginal and/or Torres Strait Islander Peoples With Chronic Kidney Disease on the Cape York Peninsula of Australia: Health Workers’ Perspectives. Aust. J. Rural Health 2025, 33, e13223. [Google Scholar] [CrossRef] [PubMed]
- Watson, K.E.; Dhaliwal, K.; Robertshaw, S.; Verdin, N.; Benterud, E.; Lamont, N.; Drall, K.M.; McBrien, K.; Donald, M.; Tsuyuki, R.T. Consensus recommendations for sick day medication guidance for people with diabetes, kidney, or cardiovascular disease: A modified Delphi process. Am. J. Kidney Dis. 2023, 81, 564–574. [Google Scholar] [CrossRef]
| Characteristic | Number of Documents n (%) |
|---|---|
| Study design | |
| Descriptive | 1 (3%) |
| Development and usability study | 1 (3%) |
| Evaluation | 2 (5%) |
| Mixed methods | 1 (3%) |
| Prospective cohort study | 1 (3%) |
| Retrospective cohort study | 3 (8%) |
| Randomised controlled trial | 23 (58%) |
| Uncontrolled trial | 8 (20%) |
| Publication year | |
| Before 2000 | 18 (45%) |
| 2000–2009 | 7 (18%) |
| 2010–2019 | 4 (10%) |
| 2019–2025 | 11 (28%) |
| Study age group | |
| Children (<18 years old) | 9 (23%) |
| Children and adults | 6 (15%) |
| Adults | 25 (63%) |
| Disease state(s) | |
| Asthma | 19 (48%) |
| Acute kidney injury prevention | 4 (10%) |
| Chronic kidney disease | 2 (5%) |
| Chronic obstructive pulmonary disease | 6 (15%) |
| Type 1 diabetes mellitus | 6 (15%) |
| Type 2 diabetes mellitus | 1 (3%) |
| Mixture of chronic conditions, i.e., cardiovascular disease | 2 (5%) |
| Region of origin | |
| Asia | 3 (8%) |
| Europe | 13 (33%) |
| North America | 14 (35%) |
| Oceania | 10 (25%) |
| Author(s), Year | Condition | Intervention Type | Intervention Name | Intervention Description | Setting (Format) | Facilitator | How Often Intervention Was Delivered by Facilitator | Tailoring to Participant |
|---|---|---|---|---|---|---|---|---|
| Charlton et al., 1994 [14] | Asthma | Education, written information, ongoing support | Patient education program and self-management plan | Interview to determine history of the asthma, provoking factors, and current symptoms. Medications were adjusted if needed. Brief education and provision of tailored self-management plan. Follow-up review with either GP nurse or GP every 3 months. | Hospital—outpatient clinic, community—medical centre (individual) | Education—asthma nurse, reinforcement —GP nurse, GP | Once at baseline | Management as per personal PEF |
| Farrell et al., 2011 [49] | T1DM | Phone support service | 24 h mobile phone support service | Participants educated about testing for ketones when unwell and to contact the 24 h mobile phone support in the presence of ketones. | Hospital—outpatient clinic (individual) | N/A | Discussion at every clinic visit | N/A |
| Fink et al., 2022 [41] | CKD | Written information | NHS Scotland’s card-sized “Medicine Sick Day Rules” with weekly remote monitoring | Participants followed instructions on the card to withhold medications for up to 48 h while sick and recommence once well again. Additional pamphlet describing a sick-day event and providing further instructions also given. | Community—medical centre (individual) | N/A | N/A | N/A |
| Madge et al., 1997 [25] | Asthma | Education, written information, ongoing support | Education program and “Going home with asthma” booklet, card-sized management plan | Education and resources given to participants. Telephone support of nurse available throughout study. | Hospital—inpatient (individual) | Education—asthma nurse | Education over 2 sessions | Individualised plan |
| Vicary et al., 2020 [43] | AKI prevention | Education and written information | Education program and sick-day guidance sheet | Education and resource given to participants. | Community—pharmacy (individual) | Education—pharmacist | Once at baseline | N/A |
| Wilson et al., 1993 [20] | Asthma | Education | Education program with workbook | Either group education with group discussion and group exercises, or individual education (content dependent on patient’s needs as per nurse educator’s assessment). Both arms received the workbook for self-study and could call the educator with any questions. | Community—medical centre (individual or group) | Education—nurse educator | For group education: 4 times, for individual education: 3–5 times | Individual education individualised |
| Cote et al., 2001 [23] | Asthma | Education and written information | Self-action plan with or without structured education | All participants received a self-action plan based on symptoms or PEF. Some participants also received structured education. | Hospital (individual or group) | N/A | Education at baseline, 6 months | Management as per predicted PEF or personal PEF |
| Kime et al., 2023 [47] | T1DM | Education | “DigiBete” mobile phone application | Participants self-navigated 200 educational videos on topics including “My Sick Day Rules”. The application can be used to receive direct communication from diabetes team. | Hospital (individual) | Not applicable | N/A | N/A |
| Kovacevic et al., 2018 [26] | Asthma | Education and written information | Structured education and asthma action plan | Participants were given structured education and an asthma action plan. | Community—pharmacy (individual) | Pharmacist | Education at baseline and 3 months (optional) | N/A |
| Thoonen et al., 2002 [15] | Asthma | Education | Education program | Education was provided and participant completed feedback form on whether they received information during the previous session. Gaps in knowledge were filled in subsequent education sessions. | Community—medical centre (individual) | GP | Education over 4 sessions | Education tailored according to participant’s needs |
| Bowman et al., 2020 [42] | CKD | Education | Tablet-based mobile educational tool | Participants were given a tablet and listened to auditory explanations with complimentary graphics, i.e., photographs of medications to be withheld during acute illness. They were then given a clinical scenario and questions regarding the hypothetical patient. They were then assessed and had to choose which medications the patient in the clinical scenario had to withhold. | Hospital—outpatient (individual) | Not applicable | Once at baseline | N/A |
| Klein et al., 1997 [31] | Asthma | Education and written information | Group education and written guidelines to self-adjust medications | Participants attended group-education sessions and received written guidelines to self-adjust medication according to PEF values/symptoms. | Hospital—outpatient (group) | Nurse | Education over 4 sessions | Management as per personal PEF |
| Morrison et al., 2014 [44] | Not specified | Written information | “Medicine Sick Day Rules” | HCPs provided cards to participants who were taking at-risk medications. | Community—pharmacy, medical centre, hospital (individual) | GP, pharmacist | Whenever medication was supplied | N/A |
| Kado et al., 2022 [52] | T2DM | Education and written information | A5 sick-day card | Education was provided and sick-day card with recommended medication adjustments was inserted into the participant’s medication handbook. Recommended adjustments needed to be signed off by GP at next visit and cited by pharmacist. | Community—pharmacy (individual) | Pharmacist | Baseline | N/A |
| Pichert et al., 1994 [50] | T1DM | Education | Anchored instruction via “Sydney Meets the Ketone Challenge” | Participants watched a video case study on diabetes sick-day management. Facilitators led group discussion about issues related to the video and solutions were discussed. | Community—camp (group) | Diabetes nurse educator | Education over 2 sessions | N/A |
| Dye et al., 2022 [48] | T1DM | Education and written information | Sick-day plan | Education was provided to participants after diabetic ketoacidosis admission and sick-day rule plan was provided. Plan was reviewed at every outpatient visit and when emergency line for assistance with blood glucose management was called. | Hospital—outpatient clinic (individual) | N/A | Baseline | N/A |
| Sedeno et al., 2009 [38] | COPD | Education, written information, ongoing support | Education modules “Living Well with COPD” and action plan | Participants were educated via modules and received a written action plan. A case manager periodically reviewed the participant’s general health and use of self-management strategies. | Community—medical centre (individual) | Case manager, GP | Baseline | N/A |
| Campain et al., 2023 [34] | COVID, asthma, COPD, CKD, T1DM, T2DM, heart failure, suicide, opioid use | Written information and ongoing support | Sick-day plan | Watch list participants were identified and received a sick-day action plan with regular follow-up from GP teams. GP teams were also notified when these patients entered/were discharged from hospital. Participants were also provided with chronic disease management services, e.g., nursing and allied health assistance, etc., in collaboration with the GP. | Community—medical centre, chronic disease clinic, hospital—inpatient (individual) | GPs, nurses, other allied health | N/A | Individualised |
| Garrett et al., 1998 [33] | Asthma | Written information | Asthma action plan | Participants received an asthma action plan and adjusted medications according to PEF/symptoms. They were followed up by paediatrician if the exacerbation was not resolved within 3 days. | Hospital—outpatient clinic, inpatient, community—medical centre (individual) | Paediatrician | N/A | Management as per personal PEF |
| Vitale et al., 2018 [46] | T1DM | Education and written information | Sick-day guideline with fridge magnetic backing | HCPs reviewed the sick-day management guidelines with the participant and were provided with a sick-day plan. | Community—clinic (individual) | Doctor, advanced practice nurse, diabetes educator | Baseline | N/A |
| Farrell et al., 2019 [51] | T1DM | Phone support service | Mobile phone support | People who experienced sick days contacted the mobile number of the service via a call or text message, to receive advice and take self-action. | Hospital—outpatient clinic (individual) | N/A | N/A | Yes, tailored advice given to patient during contact |
| Wang et al., 2024 [45] | AKI prevention | Medication review, education and written information | Medication therapy management including action plan | Multidisciplinary care was provided, which included a pharmacist who provided medication therapy management as per the KAMPS framework. This included “kidney function check, advocacy, medication, pressure, and sick-day protocols”. | Hospital—outpatient clinic (individual) | Pharmacist | Baseline, 3 months | N/A |
| Fireman et al., 1981 [32] | Asthma | Education, phone support service | Individualised education | Management plan was developed based on laboratory studies. The nurse–educator provided education to the patient and family. This was followed by group education with discussion and questions. Patients could contact the nurse via the phone with concerns. | Hospital—outpatient clinic (individual and group) | Nurse educator | Education over 3 sessions | Education tailored to participant/parent’s knowledge |
| D’Souza et al., 1994 [16] | Asthma | Education, written information, ongoing care | Card-sized self-management plan | Participants attended education clinic and received a self-management plan via GP. They attended a second clinic after 8 weeks. Māori community health workers kept in contact with participants and encouraged them to complete their symptom diaries. | Community—centre (individual) | GP, community health workers | Baseline, 8 weeks | Management as per personal PEF |
| Charlton et al., 1990 [22] | Asthma | Education, written information, ongoing care | Self-management plan | Participants were randomised to receive a management plan based on symptoms or PEF. They were educated by the practice nurse. Reviewed after 1 week and the plan was altered if necessary. Reviewed every 8 weeks or as often as practice nurse believed appropriate. | Community—clinic (individual) | Practice nurse | Baseline, 1 week, then every 8 weeks | N/A |
| Yoon et al., 1993 [19] | Asthma | Education and written information | Education program and treatment plan | Five-part education: (1) lecture about asthma, (2) video about asthma treatment, (3) individual training on using a peak flow meter, asthma diaries, and inhaler, (4) a video on typical questions and misconceptions about asthma, and (5) a practical session in using the treatment plan. | Hospital—outpatient clinic (group) | N/A | Baseline | Management as per personal PEF |
| Cowie et al., 1997 [21] | Asthma | Education and written information | Education session and asthma management plan | Participants were interviewed about their asthma to assess severity of disease, exposure to triggers, etc. Nurse practitioner provided tailored advice before participant was allocated to ‘no action plan’, ‘peak-flow-based action plan’, or ‘symptom-based action plan’ study arms. | Hospital—outpatient clinic (individual) | Nurse practitioner | Baseline | Individualised |
| Lahdensuo et al., 1996 [29] | Asthma | Education | Patient education and self-adjustment of anti-inflammatory therapy | Participants were educated about asthma via specially trained nurses and learnt breathing and relaxation techniques via physiotherapist. Participants adjusted medications according to daily PEF. | Hospital—outpatient clinic (individual) | Nurse, physiotherapist | Baseline | N/A |
| Jones et al., 1995 [27] | Asthma | Education and written information | Self-management plan | Participants were provided a self-management plan (symptom-based/PEF-based) and were given education about adjusting medications according to plan. Management plan was revised at 10- and 18-week visits. | Community—medical centre (individual) | GP, practice nurse | 5 times: baseline, 2 weeks, 10 weeks, 18 weeks, 26 weeks | Management as per personal PEF |
| Côté et al., 1998 [18] | Asthma | Education, written information, ongoing care | Individualised education and action plan | Participants attended individualised asthma education program and received an action plan based on PEF. Review by educator every 3 months, who reinforced the usefulness of PEF monitoring. | Hospital—outpatient clinic (individual) | Specialised educator | Baseline, every 3 months | Education was individualised, action plan management as per personal PEF |
| Beasley et al., 1989 [30] | Asthma | Written information | Self-management plan | Participants provided with self-management action plan. The plan was revised after 2 months of use, if needed. | Hospital—outpatient clinic (individual) | N/A | Baseline, 2 months | Management as per personal PEF |
| Wong et al., 2017 [28] | Asthma | Education and written information | Pharmaceutical care including Written Asthma Action Plan | Education sessions about asthma, and participants were given an action plan, which was counterchecked by another two pharmacists and two family medicine specialists. Pharmacists also made recommendations for medication changes to physicians. | Community—clinic (individual) | Pharmacist | Baseline, 1 month, 2 months, 3 months, 6 months | Individualised plan |
| Gallefoss et al., 1999 [24] | Asthma, COPD | Education and written information | Education and self-management Plan | Participants were provided group education about asthma/COPD and received a self-care management plan. They then received individual sessions, where understanding of treatment plan was discussed. | Hospital—outpatient clinic (individual and group) | Nurse, physiotherapist | Baseline | Management as per personal PEF |
| Van der Palen et al., 1997 [17] | Asthma | Education and written information | Education and personalised written guidelines | Participants were provided with group education and given personalised written guidelines in the last group education session. | Hospital—outpatient clinic (group) | Doctor | Education over 4 sessions | Guidelines personalised as per personal PEF |
| Bourbeau et al., 2003 [37] | COPD | Education, written information, ongoing support, phone support service | “Living well with COPD” education and action plan | Participants received “Living well with COPD” education at home. They were followed up weekly during the education period and then monthly for the remainder of the study by case managers (HCPs). Participants received a personalised action plan and could contact case managers for advice. | Home (individual) | Case managers (nurse, respiratory therapist, physiotherapist) | Education over 8 weeks | Individualised plan |
| Sridhar et al., 2008 [36] | COPD | Education, written information, ongoing support | Care package: pulmonary rehabilitation, self-management education, action plan, follow-up | Rehabilitation programme that involved general education and individualised physical training. After the program, a respiratory nurse conducted a home visit and provided a COPD action plan. Nurse followed up with monthly telephone calls and 3-monthly home visits. | Hospital, home (individual) | Respiratory nurse | Education conducted over 4 weeks | Individualised plan |
| Watson et al., 1997 [35] | COPD | Education and written information | COPD action plan, “A Guide to Living Positively with Chronic Obstructive Pulmonary Disease” education booklet | Practice nurse introduced participants to action plan and education booklet. | Community—medical centre (individual) | Practice nurse | Baseline | Individualised plan |
| Wood-Baker et al., 2006 [40] | COPD | Education and written information | Education session, COPD written-self management plan, COPD information booklet | Nurse provided education about COPD management, a COPD information booklet, and a card-sized COPD self-management plan. | Community—medical centre (individual) | Respiratory nurse | Baseline | Individualised plan |
| McGeoch et al., 2006 [39] | COPD | Education and written information | Self-management plan | Participants received standardised self-management education and an individualised self-management plan in additional to usual care. | Community—medical centre (individual) | Practice nurse, respiratory educator | Baseline | Individualised |
| Herges et al., 2023 [53] | AKI prevention | Medication review, education and written information | Medication review and KAMPS framework implementation | Pharmacists conducted a medication review 30 min before participant visit with their GP, and problems were reviewed with the doctor. Pharmacist reviewed all components of KAMPS framework (kidney function assessment, advocacy/education, medication review, blood pressure assessment, and sick-day counselling). | Community—medical centre (individual) | Pharmacist | Baseline | N/A |
| Number of Documents n (%) | |
|---|---|
| Disease state | |
| Adrenal insufficiency | 9 (16%) |
| Acute kidney injury prevention | 3 (5%) |
| Asthma | 14 (25%) |
| Chronic kidney disease | 4 (7%) |
| Chronic obstructive pulmonary disease | 2 (4%) |
| Heart failure | 3 (5%) |
| Type 1 diabetes | 5 (9%) |
| Type 1 diabetes and type 2 diabetes | 8 (14%) |
| Type 2 diabetes | 9 (16%) |
| Level of organisation (n = 49) | |
| International | 8 (16%) |
| National | 31 (63%) |
| Local/independent | 10 (20%) |
| Publication year | |
| Before 2000 | 3 (5%) |
| 2000–2009 | 5 (9%) |
| 2010–2019 | 9 (16%) |
| 2019–2025 | 26 (46%) |
| N/A | 14 (25%) |
| Region of origin | |
| Asia | 1 (2%) |
| Europe | 16 (28%) |
| North America | 18 (32%) |
| Oceania | 15 (26%) |
| International | 7 (12%) |
| Format of patient resource (n = 34) | |
| Action plan | 19 (56%) |
| Card | 1 (3%) |
| Fact sheet | 2 (6%) |
| Pamphlet | 1 (3%) |
| Patient information sheet | 9 (26%) |
| Website | 2 (6%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Truong, M.; Sud, K.; Van, C.; Tesfaye, W.; Nayak, V.; Castelino, R.L. Self-Management of Medications During Sick Days for Chronic Conditions: A Scoping Review. Medicina 2025, 61, 1742. https://doi.org/10.3390/medicina61101742
Truong M, Sud K, Van C, Tesfaye W, Nayak V, Castelino RL. Self-Management of Medications During Sick Days for Chronic Conditions: A Scoping Review. Medicina. 2025; 61(10):1742. https://doi.org/10.3390/medicina61101742
Chicago/Turabian StyleTruong, Mimi, Kamal Sud, Connie Van, Wubshet Tesfaye, Vani Nayak, and Ronald L. Castelino. 2025. "Self-Management of Medications During Sick Days for Chronic Conditions: A Scoping Review" Medicina 61, no. 10: 1742. https://doi.org/10.3390/medicina61101742
APA StyleTruong, M., Sud, K., Van, C., Tesfaye, W., Nayak, V., & Castelino, R. L. (2025). Self-Management of Medications During Sick Days for Chronic Conditions: A Scoping Review. Medicina, 61(10), 1742. https://doi.org/10.3390/medicina61101742








