Is There a Pathologic Running Motion Associated with Running-Related Injuries? A Methodological Study Using a Motion Analysis System Without Sensors
Abstract
1. Introduction
2. Materials and Methods
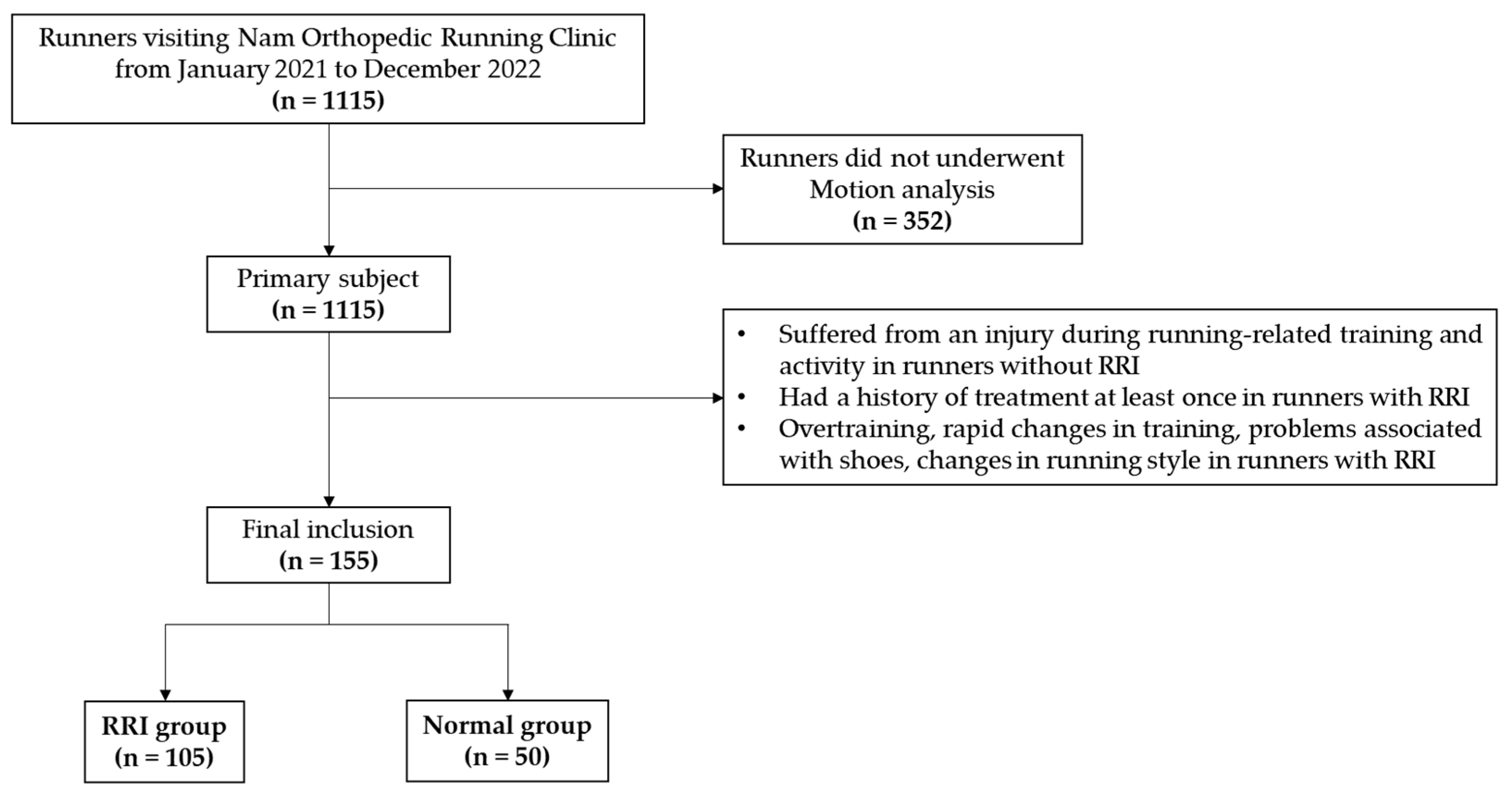
2.1. Study Design, Participants and the Inclusion and Exclusion Criteria
2.2. The Data Collection from Questionnaire
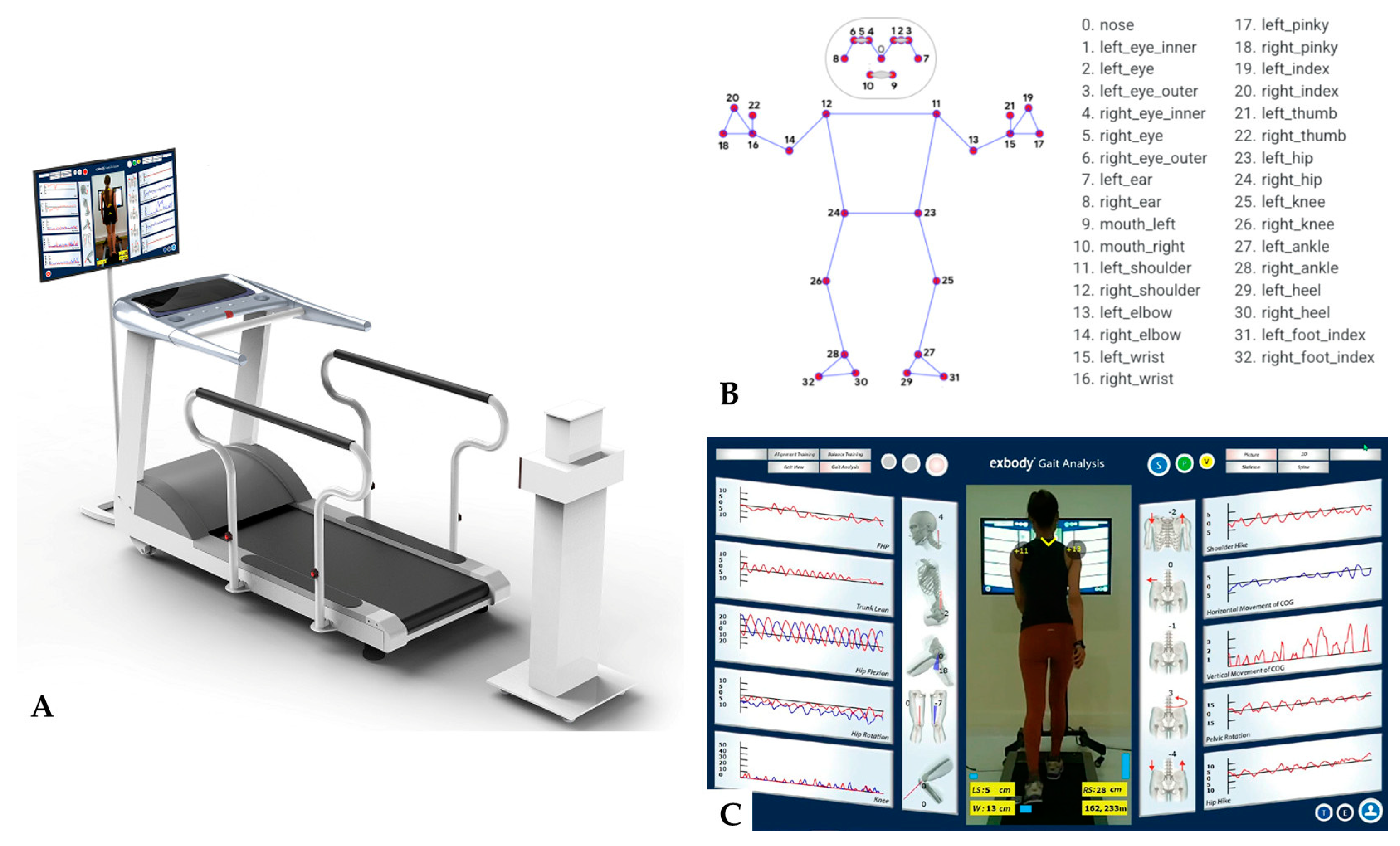
2.3. Running Motion Analysis
2.4. Statistical Analysis
3. Results
3.1. Demographic Data and Running Analysis Measurements
3.2. The Type of Foot Strike during Running
3.3. Relationship between Running Experience and RRI
3.4. Logistic Regression Analysis between Running Motion Analysis Items and RRI
3.5. ICC for Measured Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lopes, A.D.; Hespanhol Júnior, L.C.; Yeung, S.S.; Costa, L.O. What are the main running-related musculoskeletal injuries? A Systematic Review. Sports Med. 2012, 42, 891–905. [Google Scholar] [CrossRef] [PubMed]
- Saragiotto, B.T.; Yamato, T.P.; Hespanhol Junior, L.C.; Rainbow, M.J.; Davis, I.S.; Lopes, A.D. What are the main risk factors for running-related injuries? Sports Med. 2014, 44, 1153–1163. [Google Scholar] [CrossRef] [PubMed]
- Powers, C.M. The influence of abnormal hip mechanics on knee injury: A biomechanical perspective. J. Orthop. Sports Phys. Ther. 2010, 40, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Souza, R.B.; Powers, C.M. Differences in hip kinematics, muscle strength, and muscle activation between subjects with and without patellofemoral pain. J. Orthop. Sports Phys. Ther. 2009, 39, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Bennett, J.E.; Reinking, M.F.; Pluemer, B.; Pentel, A.; Seaton, M.; Killian, C. Factors contributing to the development of medial tibial stress syndrome in high school runners. J. Orthop. Sports Phys. Ther. 2001, 31, 504–510. [Google Scholar] [CrossRef]
- Becker, J.; James, S.; Wayner, R.; Osternig, L.; Chou, L.S. Biomechanical Factors Associated With Achilles Tendinopathy and Medial Tibial Stress Syndrome in Runners. Am. J. Sports Med. 2017, 45, 2614–2621. [Google Scholar] [CrossRef]
- Ryan, M.; Grau, S.; Krauss, I.; Maiwald, C.; Taunton, J.; Horstmann, T. Kinematic analysis of runners with achilles mid-portion tendinopathy. Foot Ankle Int. 2009, 30, 1190–1195. [Google Scholar] [CrossRef] [PubMed]
- van Gent, R.N.; Siem, D.; van Middelkoop, M.; van Os, A.G.; Bierma-Zeinstra, S.M.; Koes, B.W. Incidence and determinants of lower extremity running injuries in long distance runners: A systematic review. Br. J. Sports Med. 2007, 41, 469–480, discussion 480. [Google Scholar] [CrossRef]
- Taunton, J.E.; Ryan, M.B.; Clement, D.B.; McKenzie, D.C.; Lloyd-Smith, D.R.; Zumbo, B.D. A retrospective case-control analysis of 2002 running injuries. Br. J. Sports Med. 2002, 36, 95–101. [Google Scholar] [CrossRef]
- Barton, C.J.; Bonanno, D.R.; Carr, J.; Neal, B.S.; Malliaras, P.; Franklyn-Miller, A.; Menz, H.B. Running retraining to treat lower limb injuries: A mixed-methods study of current evidence synthesised with expert opinion. Br. J. Sports Med. 2016, 50, 513–526. [Google Scholar] [CrossRef]
- Willems, T.M.; De Clercq, D.; Delbaere, K.; Vanderstraeten, G.; De Cock, A.; Witvrouw, E. A prospective study of gait related risk factors for exercise-related lower leg pain. Gait Posture 2006, 23, 91–98. [Google Scholar] [CrossRef] [PubMed]
- Bramah, C.; Preece, S.J.; Gill, N.; Herrington, L. Is There a Pathological Gait Associated with Common Soft Tissue Running Injuries? Am. J. Sports Med. 2018, 46, 3023–3031. [Google Scholar] [CrossRef]
- Koike, S.; Nakaya, S.; Mori, H.; Ishikawa, T.; Willmott, A.P. Modelling error distribution in the ground reaction force during an induced-acceleration analysis of running in rear-foot strikers. J. Sports Sci. 2019, 37, 968–979. [Google Scholar] [CrossRef] [PubMed]
- Tripodi, N.; Feehan, J.; Corcoran, D.; Vaughan, B.; McLaughlin, P. Introduction to running analysis in the clinical setting: A masterclass. Int. J. Osteopath. Med. 2024, 51, 100698. [Google Scholar] [CrossRef]
- Aderem, J.; Louw, Q.A. Biomechanical risk factors associated with iliotibial band syndrome in runners: A systematic review. BMC Musculoskelet. Disord. 2015, 16, 356. [Google Scholar] [CrossRef] [PubMed]
- Creaby, M.W.; Dixon, S.J. External frontal plane loads may be associated with tibial stress fracture. Med. Sci. Sports Exerc. 2008, 40, 1669–1674. [Google Scholar] [CrossRef] [PubMed]
- Willy, R.W.; Manal, K.T.; Witvrouw, E.E.; Davis, I.S. Are mechanics different between male and female runners with patellofemoral pain? Med. Sci. Sports Exerc. 2012, 44, 2165–2171. [Google Scholar] [CrossRef] [PubMed]
- van der Kruk, E.; Reijne, M.M. Accuracy of human motion capture systems for sport applications; state-of-the-art review. Eur. J. Sport. Sci. 2018, 18, 806–819. [Google Scholar] [CrossRef] [PubMed]
- Davis, I.S.; Bowser, B.J.; Mullineaux, D.R. Greater vertical impact loading in female runners with medically diagnosed injuries: A prospective investigation. Br. J. Sports Med. 2016, 50, 887–892. [Google Scholar] [CrossRef]
- Kerrigan, D.C.; Frates, E.P.; Rogan, S.; Riley, P.O. Hip hiking and circumduction: Quantitative definitions. Am. J. Phys. Med. Rehabil. 2000, 79, 247–252. [Google Scholar] [CrossRef]
- Dunphy, C.; Casey, S.; Lomond, A.; Rutherford, D. Contralateral pelvic drop during gait increases knee adduction moments of asymptomatic individuals. Hum. Mov. Sci. 2016, 49, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Semciw, A.; Neate, R.; Pizzari, T. Running related gluteus medius function in health and injury: A systematic review with meta-analysis. J. Electromyogr. Kinesiol. 2016, 30, 98–110. [Google Scholar] [CrossRef]
- Tateuchi, H.; Shiratori, S.; Ichihashi, N. The effect of angle and moment of the hip and knee joint on iliotibial band hardness. Gait Posture 2015, 41, 522–528. [Google Scholar] [CrossRef] [PubMed]
- Fairclough, J.; Hayashi, K.; Toumi, H.; Lyons, K.; Bydder, G.; Phillips, N.; Best, T.M.; Benjamin, M. Is iliotibial band syndrome really a friction syndrome? J. Sci. Med. Sport 2007, 10, 74–76, discussion 77–78. [Google Scholar] [CrossRef] [PubMed]
- Merican, A.M.; Amis, A.A. Iliotibial band tension affects patellofemoral and tibiofemoral kinematics. J. Biomech. 2009, 42, 1539–1546. [Google Scholar] [CrossRef] [PubMed]
- Lorimer, A.V.; Hume, P.A. Stiffness as a Risk Factor for Achilles Tendon Injury in Running Athletes. Sports Med. 2016, 46, 1921–1938. [Google Scholar] [CrossRef] [PubMed]
- Warrener, A.; Tamai, R.; Lieberman, D.E. The effect of trunk flexion angle on lower limb mechanics during running. Hum. Mov. Sci. 2021, 78, 102817. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, D.E.; Venkadesan, M.; Werbel, W.A.; Daoud, A.I.; D’Andrea, S.; Davis, I.S.; Mang’eni, R.O.; Pitsiladis, Y. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature 2010, 463, 531–535. [Google Scholar] [CrossRef] [PubMed]
- Knorz, S.; Kluge, F.; Gelse, K.; Schulz-Drost, S.; Hotfiel, T.; Lochmann, M.; Eskofier, B.; Krinner, S. Three-Dimensional Biomechanical Analysis of Rearfoot and Forefoot Running. Orthop. J. Sports Med. 2017, 5, 2325967117719065. [Google Scholar] [CrossRef]
- Macera, C.A.; Pate, R.R.; Powell, K.E.; Jackson, K.L.; Kendrick, J.S.; Craven, T.E. Predicting lower-extremity injuries among habitual runners. Arch. Intern. Med. 1989, 149, 2565–2568. [Google Scholar] [CrossRef]

| Variables (n = 155) | Mean | SD | Min | Max | Cohen D |
|---|---|---|---|---|---|
| Mean age (years) | 38.97 | 8.90 | 15 | 62 | 8.88 |
| Weight (kg) | 66.57 | 10.37 | 41.0 | 98.0 | 10.32 |
| Height (cm) | 174.04 | 44.55 | 150 | 717 | 44.56 |
| Body mass index (kg/m2) | 22.77 | 2.26 | 17.1 | 29.6 | 2.26 |
| Running distance (km/week) | 33.32 | 19.15 | 5 | 105 | 19.11 |
| FHP (turtle neck, °) | 8.19 | 4.51 | −6 | 24 | 4.12 |
| Trunk lean (°) | 6.19 | 2.68 | 0 | 15 | 2.66 |
| Hip rotation RT (°) | 7.79 | 1.52 | 4 | 12 | 1.52 |
| Hip rotation LT (°) | 5.41 | 1.50 | 2 | 11 | 1.50 |
| Horizontal movement of COG RT (cm) | 1.69 | 1.70 | 0 | 7 | 1.69 |
| Horizontal movement of COG LT (cm) | 2.46 | 1.70 | 0 | 9 | 1.68 |
| Vertical movement of COG (cm) | 2.78 | 1.18 | 0 | 4 | 1.18 |
| Pelvic rotation RT (°) | 5.84 | 2.59 | 0 | 14 | 2.58 |
| Pelvic rotation LT (°) | 7.97 | 2.64 | 1 | 15 | 2.65 |
| Hip hike RT (°) | 3.08 | 1.17 | 1 | 5 | 0.87 |
| Hip hike LT (°) | 0.74 | 0.58 | 0 | 2 | 0.53 |
| Difference of hip rotation (°) | 2.37 | 1.41 | −1 | 6 | 1.41 |
| Difference of horizontal movement of COG (cm) | −0.77 | 3.09 | −9 | 7 | 3.06 |
| Difference of pelvic rotation (°) | −2.12 | 2.98 | −8 | 7 | 2.96 |
| Difference of hip hike (cm) | 2.34 | 1.52 | −1 | 5 | 1.13 |
| Variables (n = 155) | Normal (n = 50) | RRI (n = 105) | t | p |
|---|---|---|---|---|
| Sex (n, Male/Female) | 33:17 | 77:45 | N/A | 0.347 * |
| Mean age (years) | 40.18 ± 9.56 | 38.39 ± 8.55 | 1.17 | 0.243 |
| Weight (kg) | 64.65 ± 9.90 | 67.49 ± 10.50 | −1.60 | 0.111 |
| Height (cm) | 169.12 ± 8.10 | 176.38 ± 53.76 | −0.95 | 0.344 |
| Body mass index (kg/m2) | 22.51 ± 2.12 | 22.90 ± 2.32 | −0.98 | 0.327 |
| Running distance (km/week) | 36.16 ± 20.93 | 31.97 ± 18.19 | 1.28 | 0.204 |
| FHP (turtle neck, °) | 5.50 ± 2.96 | 9.47 ± 4.56 | −6.49 | <0.001 |
| Trunk lean (°) | 5.58 ± 2.16 | 6.48 ± 2.86 | −1.96 | 0.051 |
| Hip rotation RT (°) | 7.88 ± 1.44 | 7.74 ± 1.56 | 0.53 | 0.600 |
| Hip rotation LT (°) | 5.54 ± 1.54 | 5.35 ± 1.48 | 0.73 | 0.468 |
| Horizontal movement of COG RT (cm) | 1.38 ± 1.67 | 1.84 ± 1.70 | −1.58 | 0.116 |
| Horizontal movement of COG LT (cm) | 2.88 ± 1.93 | 2.27 ± 1.55 | 2.13 | 0.035 |
| Vertical movement of COG (cm) | 2.78 ± 1.09 | 2.78 ± 1.23 | −0.01 | 0.996 |
| Pelvic rotation RT (°) | 6.24 ± 2.72 | 5.65 ± 2.52 | 1.34 | 0.184 |
| Pelvic rotation LT (°) | 7.78 ± 3.01 | 8.06 ± 2.46 | −0.61 | 0.544 |
| Hip hike RT (°) | 1.96 ± 0.57 | 3.61 ± 0.99 | −13.15 | <0.001 |
| Hip hike LT (°) | 1.10 ± 0.54 | 0.57 ± 0.52 | 5.75 | <0.001 |
| Difference of hip rotation (°) | 2.34 ± 1.47 | 2.39 ± 1.39 | −0.21 | 0.836 |
| Difference of horizontal movement of COG (cm) | −1.50 ± 3.14 | −0.43 ± 3.03 | −2.04 | 0.043 |
| Difference of pelvic rotation (°) | −1.54 ± 3.27 | −2.41 ± 2.81 | 1.71 | 0.090 |
| Difference of hip hike (°) | 0.86 ± 0.64 | 3.04 ± 1.29 | −14.03 | <0.001 |
| Variables | Type of Strike | p | |
|---|---|---|---|
| Rearfoot | Midfoot + Forefoot | ||
| Normal (n = 50) | 31 (62.0%) | 19 (38.0%) | 0.351 |
| RRI (n = 105) | 73 (69.5%) | 32 (30.5%) | |
| Total (n = 155) | 104 (67.1%) | 51 (32.9%) | |
| Variables | Elite + Pro | Beginner | Recreational | p |
|---|---|---|---|---|
| Normal (n = 50) | 3 (6.0%) | 10 (20.0%) | 37 (74.0%) | 0.033 * |
| RRI (n = 105) | 1 (1.0%) | 37 (35.2%) | 67 (63.8%) | |
| Total (n = 155) | 4 | 47 (30.3%) | 104 (67.1%) |
| Independent Variables | B | SE | p | Exp (B) | 95% CI |
|---|---|---|---|---|---|
| FHP (turtle neck, °) | 0.42 | 0.11 | <0.001 | 1.52 | 1.22–1.89 |
| Trunk lean (°) | −0.07 | 0.17 | 0.703 | 0.94 | 0.67–1.31 |
| Difference of hip rotation (°) | 0.14 | 0.28 | 0.604 | 1.16 | 0.67–1.99 |
| Difference of horizontal movement of COG (cm) | 0.03 | 0.12 | 0.805 | 1.03 | 0.81–1.32 |
| Vertical movement of COG (cm) | 0.09 | 0.30 | 0.778 | 1.09 | 0.60–1.97 |
| Difference of pelvic rotation (°) | −0.05 | 0.12 | 0.707 | 0.96 | 0.76–1.21 |
| Difference of hip hike (°) | 2.84 | 0.59 | <0.001 | 17.17 | 5.40–54.62 |
| Variables (n = 15) | ICC | p | Interpretation |
|---|---|---|---|
| FHP (turtle neck, °) | 0.73 | 0.009 | Acceptable reliability |
| Trunk lean (°) | 0.70 | 0.016 | Acceptable reliability |
| Hip rotation RT (°) | 0.89 | <0.001 | Good reliability |
| Hip rotation LT (°) | 0.93 | <0.001 | Excellent reliability |
| Horizontal movement of COG RT (cm) | 0.63 | 0.038 | Questionable reliability |
| Horizontal movement of COG LT (cm) | 0.64 | 0.035 | Questionable reliability |
| Vertical movement of COG (cm) | 0.70 | 0.016 | Acceptable reliability |
| Pelvic rotation RT (°) | 0.94 | <0.001 | Excellent reliability |
| Pelvic rotation LT (°) | 0.81 | 0.002 | Good reliability |
| Hip hike RT (°) | 0.87 | <0.001 | Good reliability |
| Hip hike LT (°) | 0.88 | <0.001 | Good reliability |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nam, H.W.; Yang, J.H.; Park, S.G.; Rhim, H.C.; Kim, H.J. Is There a Pathologic Running Motion Associated with Running-Related Injuries? A Methodological Study Using a Motion Analysis System Without Sensors. Medicina 2024, 60, 1249. https://doi.org/10.3390/medicina60081249
Nam HW, Yang JH, Park SG, Rhim HC, Kim HJ. Is There a Pathologic Running Motion Associated with Running-Related Injuries? A Methodological Study Using a Motion Analysis System Without Sensors. Medicina. 2024; 60(8):1249. https://doi.org/10.3390/medicina60081249
Chicago/Turabian StyleNam, Hyok Woo, Jae Hyuk Yang, Seul Gi Park, Hye Chang Rhim, and Hong Jin Kim. 2024. "Is There a Pathologic Running Motion Associated with Running-Related Injuries? A Methodological Study Using a Motion Analysis System Without Sensors" Medicina 60, no. 8: 1249. https://doi.org/10.3390/medicina60081249
APA StyleNam, H. W., Yang, J. H., Park, S. G., Rhim, H. C., & Kim, H. J. (2024). Is There a Pathologic Running Motion Associated with Running-Related Injuries? A Methodological Study Using a Motion Analysis System Without Sensors. Medicina, 60(8), 1249. https://doi.org/10.3390/medicina60081249






