Early Balloon Kyphoplasty Treatment for Osteoporotic Vertebral Fracture Reduces Adjacent Vertebral Fractures
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Patient Characteristics
3.2. Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tsuboi, M.; Hasegawa, Y.; Suzuki, S.; Wingstrand, H.; Thorngren, K.G. Mortality and mobility after hip fracture in Japan: A ten-year follow-up. J. BoneJoint Surg. Br. 2007, 89, 461–466. [Google Scholar] [CrossRef] [PubMed]
- Cauley, J.A.; Thompson, D.E.; Ensrud, K.C.; Scott, J.C.; Black, D. Risk of mortality following clinical fractures. Osteoporos. Int. 2000, 11, 556–561. [Google Scholar] [CrossRef] [PubMed]
- Wardlaw, D.; Cummings, S.R.; Meirhaeghe, J.V.; Bastian, L.; Tillman, J.B.; Ranstam, J.; Eastell, R.; Shabe, P.; Talmadge, K.; Boonen, S. Efficacy and safety of balloon kyphoplasty compared with nonsurgical care for vertebral compression fracture (FREE): A randomised controlled trial. Lancet 2009, 373, 1016–1024. [Google Scholar] [CrossRef] [PubMed]
- Minamide, A.; Maeda, T.; Yamada, H.; Murakami, K.; Okada, M.; Enyo, Y.; Nakagawa, Y.; Iwasaki, H.; Tsutsui, S.; Takami, M.; et al. Early varsus delayed kyphoplasty for thoracolumbar osteoprotic verterbral fractures: The effect of timing on clinical and radiographic outcomes and subsequent compression fractures. Clin. Neurol. Neurosurg. 2018, 173, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Trout, A.T.; Kallmes, D.F.; Lane, J.I.; Layton, K.F.; Marx, W.F. Subsequent vertebral fractures after vertebroplasty association with intraosseous clefts. Am. J. Neuroradial. 2006, 27, 1586–1591. [Google Scholar]
- Flankel, B.M.; Monroe, T.; Wang, C. Percutaneous vertebral augmentation: An elevation in adjacent-level fracture risk in kyphoplasty as compared with vertebroplasty. Spine J. 2007, 7, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Fribourg, D.; Tang, C.; Sra, P.; Delamarter, R.; Bae, H. Incidence of subsequent vertebral fracture after kyphoplasty. Spine 2004, 29, 2270–2276. [Google Scholar] [CrossRef]
- Iida, k.; Harimaya, K.; Tarukado, K.; Tono, O.; Matsumoto, Y.; Nakashima, Y. Kyhosis progression after balloon kyphoplasty compared with conservative treatment. Asian Spine J. 2019, 6, 928–935. [Google Scholar] [CrossRef] [PubMed]
- Grafe, I.A.; Fonseca, D.K.; Hillmeier, J.; Meeder, P.J.; Libicher, M.; Nöldge, G.; Bardenheuer, H.; Pyerin, W.; Basler, L.; Weiss, C.; et al. Reduction of pain and fracture incidence after kyphoplasty: 1-year outcomes of a prospective controlled trial of patients with primary osteoporosis. Osteoporos. Int. 2005, 16, 2005–2012. [Google Scholar] [CrossRef]
- Kato, T.; Inose, H.; Ichimura, S.; Tokuhashi, Y.; Nakamura, H.; Hoshino, M.; Togawa, D.; Hirano, T.; Haro, H.; Ohba, T.; et al. Comparison of Rigid and Soft-Brace Treatments for Acute Osteoporotic Vertebral Compression Fracture: A Prospective, Randomized, Multicenter Study. J. Clin. Med. 2019, 8, 198. [Google Scholar] [CrossRef]
- Matsumoto, T.; Hoshino, M.; Tsujio, T.; Terai, H.; Namikawa, T.; Matsumura, A.; Kato, M.; Toyoda, H.; Suzuki, A.; Takayama, K.; et al. Prognostic factors for reduction of activities of daily living following osteoporotic vertebral fractures. Spine 2012, 37, 1115–1121. [Google Scholar] [CrossRef] [PubMed]
- Phillis, F.M.; Ho, E.; Campbell-Hupp, M.; McNally, T.; Wetzel, F.T.; Gupta, P. Early radiographic and clinica results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine 2003, 28, 2260–2265. [Google Scholar] [CrossRef]
- Takahashi, S.; Hoshino, M.; Terai, H.; Toyoda, H.; Suzuki, A.; Tamai, K.; Watanabe, K.; Tsujio, T.; Yasuda, H.; Kono, H.; et al. Differences in short-term clinical and radiological outcomes depending on timing of balloon kyphoplasty for painful osteoporotic vertebral fracture. J. Orthop. Sci. 2018, 23, 51–56. [Google Scholar] [CrossRef] [PubMed]
- Sakai, T. Is Early Stage Balloon Kyphoplasty for Osteoporotic Vertebral Fracture Appropriate? J. Spine Res. 2018, 9, 1719–1722. [Google Scholar]
- Shawn, J.S.; Mark, H.Y.; Jun-Hao, T.; Hwee Weng, D.H. Early cement augmentation may be a good treatment option for pain relief for osteoporotic compression fractures: A systematic review and meta-analysis. Eur. Spine J. 2023, 32, 1751–1762. [Google Scholar]
- Tsujio, T.; Nakamura, H.; Terai, H.; Hoshino, M.; Namikawa, T.; Matsumura, A.; Kato, M.; Suzuki, A.; Takayama, K.; Fukushima, W.; et al. Characteristic radiographic or magnetic resonance images of fresh osteoporotic vertebral fractures predicting potential risk for nonunion: A prospective multicenter study. Spine 2011, 36, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Iwamae, M.; Terai, H.; Tamai, K.; Hoshino, M.; Takahashi, S.; Umano, M.; Kobayashi, Y.; Katsuda, H.; Kaneda, K.; Shimada, N.; et al. Risk of residual low back pain in conservative treatment of osteoporotic vertebral fractures without poor prognostic factors on magnetic resonance imaging. J. Spine Res. 2023, 14, 786–793. [Google Scholar]
- Zhang, T.; Wang, Y.; Zhang, P.; Xue, F.; Zhang, D.; Jiang, B. What are the risk factors for adjacent vertebral fracture after vertebral augmentation? A meta-analysis of published studies. Glob. Spine J. 2022, 12, 130–141. [Google Scholar] [CrossRef]
- Lindsay, R.; Silverman, S.L.; Cooper, C.; Hanley, D.A.; Barton, I.; Broy, S.B.; Licata, A.; Benhamou, L.; Geusens, P.; Flowers, K.; et al. Risk of new vertebral fracture in the year following a fracture. JAMA 2001, 285, 320–323. [Google Scholar] [CrossRef]
- Kadowaki, E.; Tamaki, J.; Iki, M.; Sato, Y.; Chiba, Y.; Kajita, E.; Kagamimori, S.; Kagawa, Y.; Yoneshima, H. Prevalent vertebral deformity independently increases incident vertebral fracture risk in middle-aged and elderly Japanese women: The Japanese Population-based Osteoporosis (JPOS) Cohort Study. Osteoporos. Int. 2010, 21, 1513–1522. [Google Scholar] [CrossRef]
- Yang, S.C.; Chen, W.J.; Yu, S.W.; Tu, Y.K.; Kao, Y.H.; Chung, K.C. Revision strategies for complications and failure of vertebroplasties. Eur. Spine J. 2008, 17, 982–988. [Google Scholar] [CrossRef] [PubMed]
- Takahara, K.; Kamimura, M.; Moriya, H.; Ashizawa, R.; Koike, T.; Hidai, Y.; Ikegami, S.; Nakamura, Y.; Kato, H. Risk factors of adjacent vertebral collapse after percutaneous vertebroplasty for osteoporotic vertebral fracture in postmenopausal women. BMC Muscoskel. Disord. 2016, 17, 12. [Google Scholar] [CrossRef] [PubMed]
- Hijikata, Y.; Kamitani, T.; Nakahara, M.; Kumamoto, S.; Sakai, T.; Itaya, T.; Yamazaki, H.; Ogawa, Y.; Kusumegi, A.; Inoue, T.; et al. Development and internal validation of a clinical prediction model for acute adjacent vertebral fracture after vertebral augmentation. Bone Joint J. 2022, 104, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Morozumi, M.; Matsubara, Y.; Muramoto, A.; Morita, Y.; Ando, K.; Kobayashi, K.; Machino, M.; Ota, K.; Tanaka, S.; Kanbara, S.; et al. A study of risk factors for early-onset adjacent vertebral fractures after kyphoplasty. Glob. Spine J. 2020, 10, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Paradhan, B.B.; Bae, H.W.; Kropf, M.A.; Patel, V.V.; Delamarter, R.B. Kyphoplasty reduction of osteoporotic vertebral compression fractures correction of local kyphosis versus overall sagittal alignment. Spine 2006, 15, 435–441. [Google Scholar] [CrossRef] [PubMed]
- Langdahl, B.L.; Rajzbaum, G.; Jakob, F.; Karras, D.; Ljunggren, O.; Lems, W.F.; Fahrleitner-Pammer, A.; Walsh, J.B.; Barker, C.; Kutahov, A.; et al. Reduction in fracture rate and back pain and increased quality of life in postmenopausal women treated with teriparatide: 18-month data from the European Forsteo Observational Study (EFOS). Calcif. Tissue Int. 2009, 85, 484–493. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Lin, W.; Zhao, S.; Mo, X.; Yuan, W.; Cheung, W.H.; Fu, D.; Chen, B. Effect of Teriparatide on pain relief, and quality of life in postmenopausal females with osteoporotic vertebral compression fractures, a retrospective cohort study. Ann. Palliat. Med. 2021, 10, 4000–4007. [Google Scholar] [CrossRef]
- Joyce, D.M.; Granville, M.; Berti, A.; Jacobson, R.E. Vertebral Augmentation Compared to Conservative Treatment of Vertebra Plana and High-Degree Osteoporotic Vertebral Fractures: A Review of 110 Fractures in 100 Patients. Cureus 2022, 14, e22006. [Google Scholar] [CrossRef]
- Pedicelli, A.; Lozupone, E.; Gatto, A.; Gulino, P.; D’Argento, F.; Capozzi, A.; Colosimo, C. Vertebra plana: Reappraisal of a contraindication to percutaneous vertebroplasty. Eur. J. Radiol. 2013, 82, 2303–2308. [Google Scholar] [CrossRef]
- Lamy, O.; Uebelhart, B.; Aubry-Rozier, B. Risks and benefits of percutaneous vertebroplasty or kyphoplasty in the management of osteoporotic vertebral fractures. Osteoporos. Int. 2014, 25, 807–819. [Google Scholar] [CrossRef]
- Capozzi, A.; Scambia, G.; Pedicelli, A.; Evangelista, M.; Sorge, R.; Lello, S. Clinical management of osteoporotic vertebral fracture treated with percutaneous vertebroplasty. Clin. Cases Miner. Bone Metab. 2016, 14, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Taha, K.A.; Lauper, N.; Bauer, D.F.; Tsoupras, A.; Tessitore, E.; Biver, E.; Dominguez, D.E. Multidisciplinary and Coordinated Management of Osteoporotic Vertebral Compression Fractures: Current State of the Art. J. Clin. Med. 2024, 13, 930. [Google Scholar] [CrossRef] [PubMed]

| Early Group (n = 62) | Non-Early Group (n = 33) | p-Value | |
|---|---|---|---|
| Age (years) | 81.8 ± 7.3 | 78.5 ± 8.2 | N.S. |
| Sex (male/female) | M15/F47 | M7/F26 | N.S. |
| Time from injury to surgery (days) | 8.2 ± 3.0 | 43.2 ± 34.1 | p < 0.05 |
| Fracture level | |||
| Thoracic spine (-T10) | 0 (0%) | 0(0%) | N.S. |
| Thoracolumbar spine (T11–L2) | 50 (80.6%) | 27 (81.8%) | N.S. |
| Lumbar spine (L3–L5) | 12 (19.4%) | 6 (18.2%) | N.S. |
| Old vertebral fracture | |||
| 0 | 46 (74.2%) | 19 (57.6%) | N.S. |
| ≧1 | 16 (25.8%) | 14 (42.4%) | N.S. |
| Posterior wall injury (%) | 25 (40.3%) | 14 (42.4%) | N.S. |
| Intravertebral cleft | 17 (27.4%) | 12 (36.3%) | N.S. |
| Preoperative NRS | 9.2 ± 0.7 | 9.0 ± 0.7 | N.S. |
| Early Group (n = 62) | Non-Early Group (n = 33) | p-Value | |
|---|---|---|---|
| Duration of surgery (min) | 24.0 ± 2.4 | 23.5 ± 2.5 | N.S. |
| Duration to hospitalization (days) | 32.8 ± 15.7 | 29.2 ± 17.7 | N.S. |
| Cement volume (mL) | 7.65 ± 1.37 | 7.42 ± 1.73 | N.S. |
| AVF | 4 (6.5%) | 11 (33.3%) | p < 0.05 |
| Duration to AVF (weeks) | 6.5 ± 1.8 | 4.1 ± 0.9 | p < 0.05 |
| Postoperative NRS | 0.4 ± 0.7 | 0.8 ± 1.3 | N.S. |
| Non-AVF Group (n = 80) | AVF Group (n = 15) | p-Value | |
|---|---|---|---|
| Age (years) | 81.2 ± 5.3 | 77.7 ± 9.3 | N.S. |
| Time from injury to surgery (days) | 15.8 ± 20.1 | 44.5 ± 38.6 | 0.001 |
| Old vertebral fracture | 0.44 ± 0.83 | 0.8 ± 0.9 | N.S. |
| Cement volume (mL) | 7.63 ± 1.43 | 7.27 ± 1.84 | N.S. |
| Preoperative vertebral kyphosis angle | −9.2 ± 5.3 | −13.3 ± 5.8 | 0.009 |
| Immediate postoperative vertebral kyphosis angle | −4 ± 3.5 | −6.3 ± 4.7 | 0.033 |
| Final postoperative vertebral kyphosis angle | −6.2 ± 4.5 | −9.7 ± 4.5 | 0.008 |
| Change in vertebral kyphosis angle | 5.1 ± 3.2 | 6.3 ± 3.1 | N.S. |
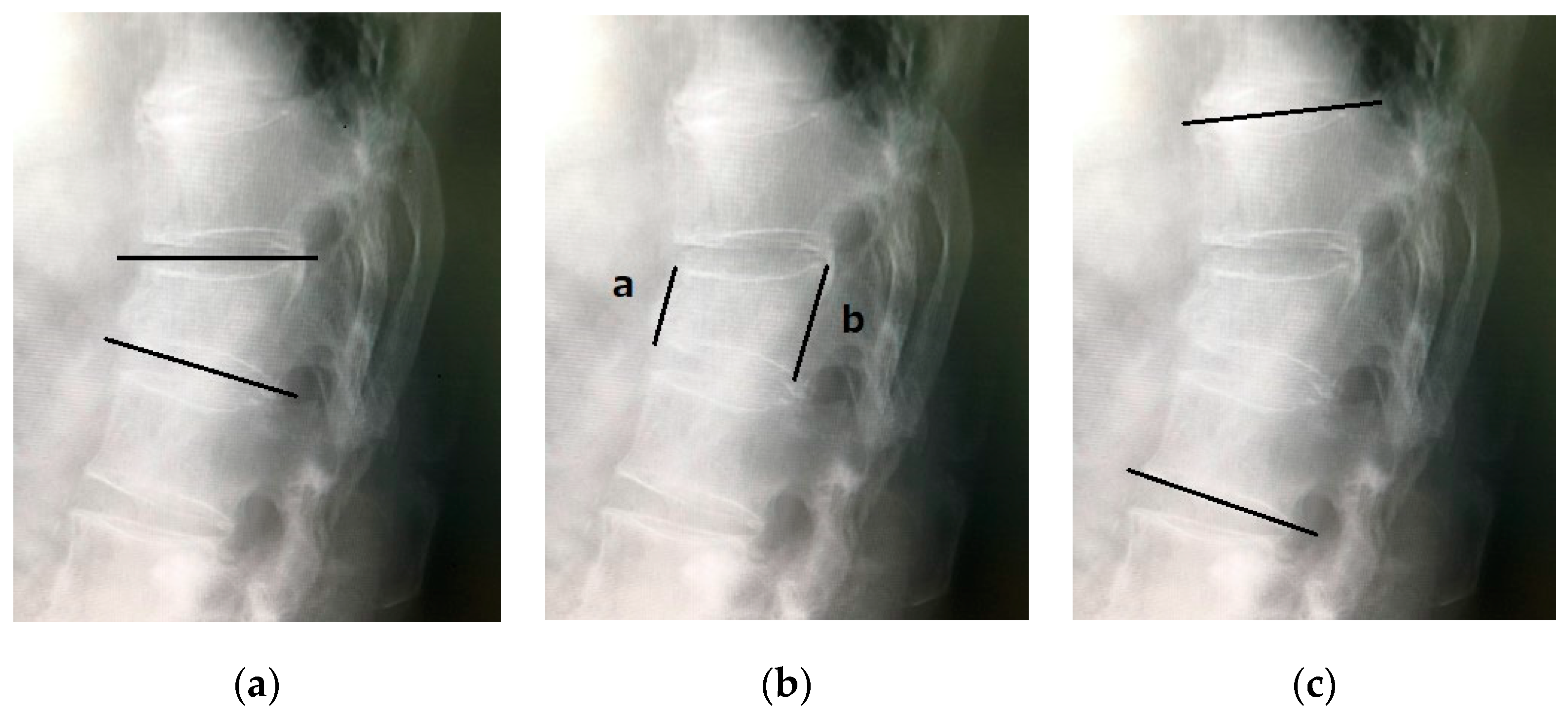
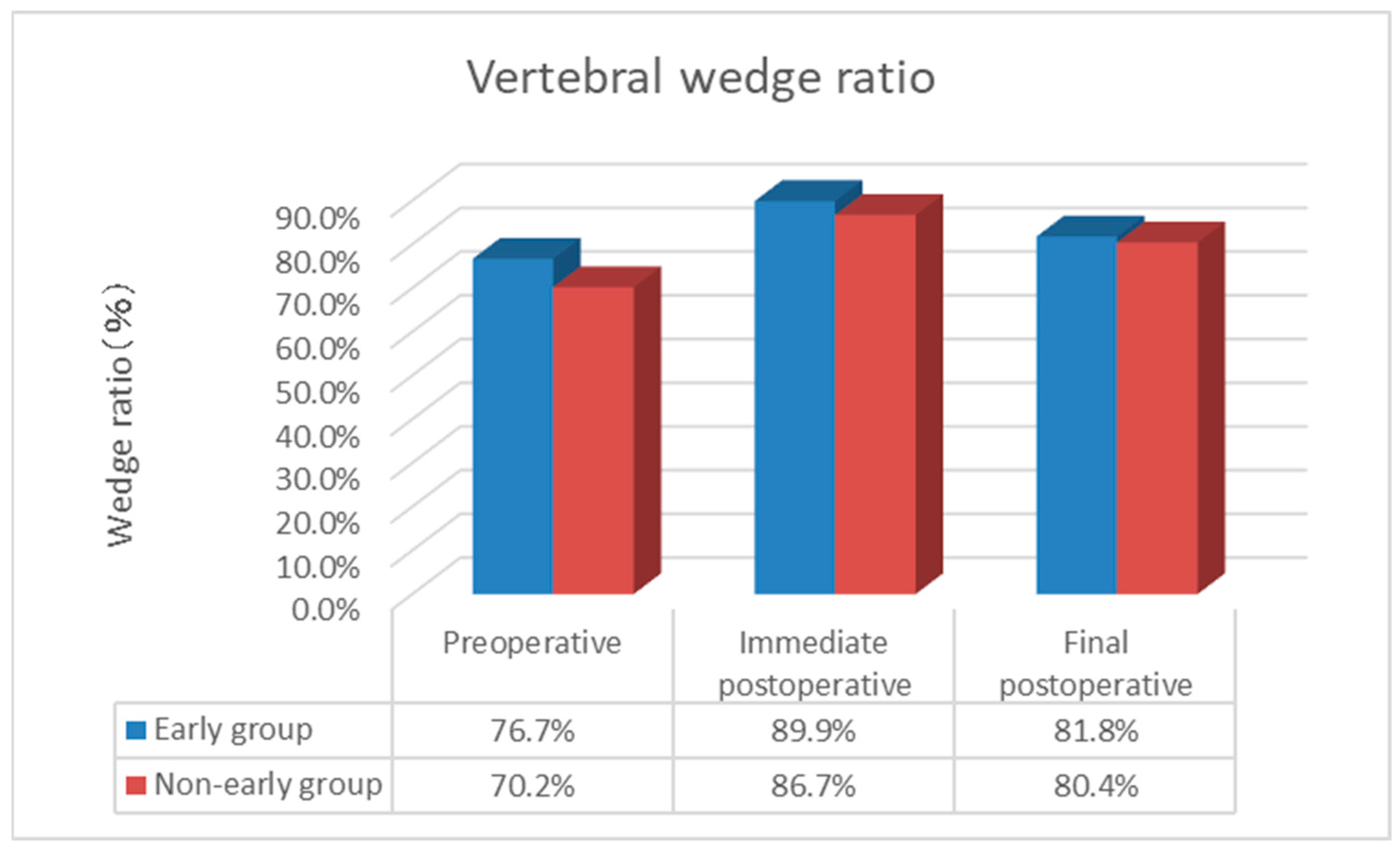
| Preoperative vertebral wedge ratio (%) | 77.0 ± 14.1 | 61.1 ± 17.4 | 0.001 |
| Immediate postoperative vertebral wedge ratio (%) | 90.1 ± 8.9 | 81.5 ± 13.6 | 0.003 |
| Final postoperative vertebral wedge ratio (%) | 83.3 ± 12.2 | 72.7 ± 12.6 | 0.001 |
| Change in vertebral wedge ratio (%) | 12.9 ± 10.1 | 20.4 ± 11.4 | N.S. |
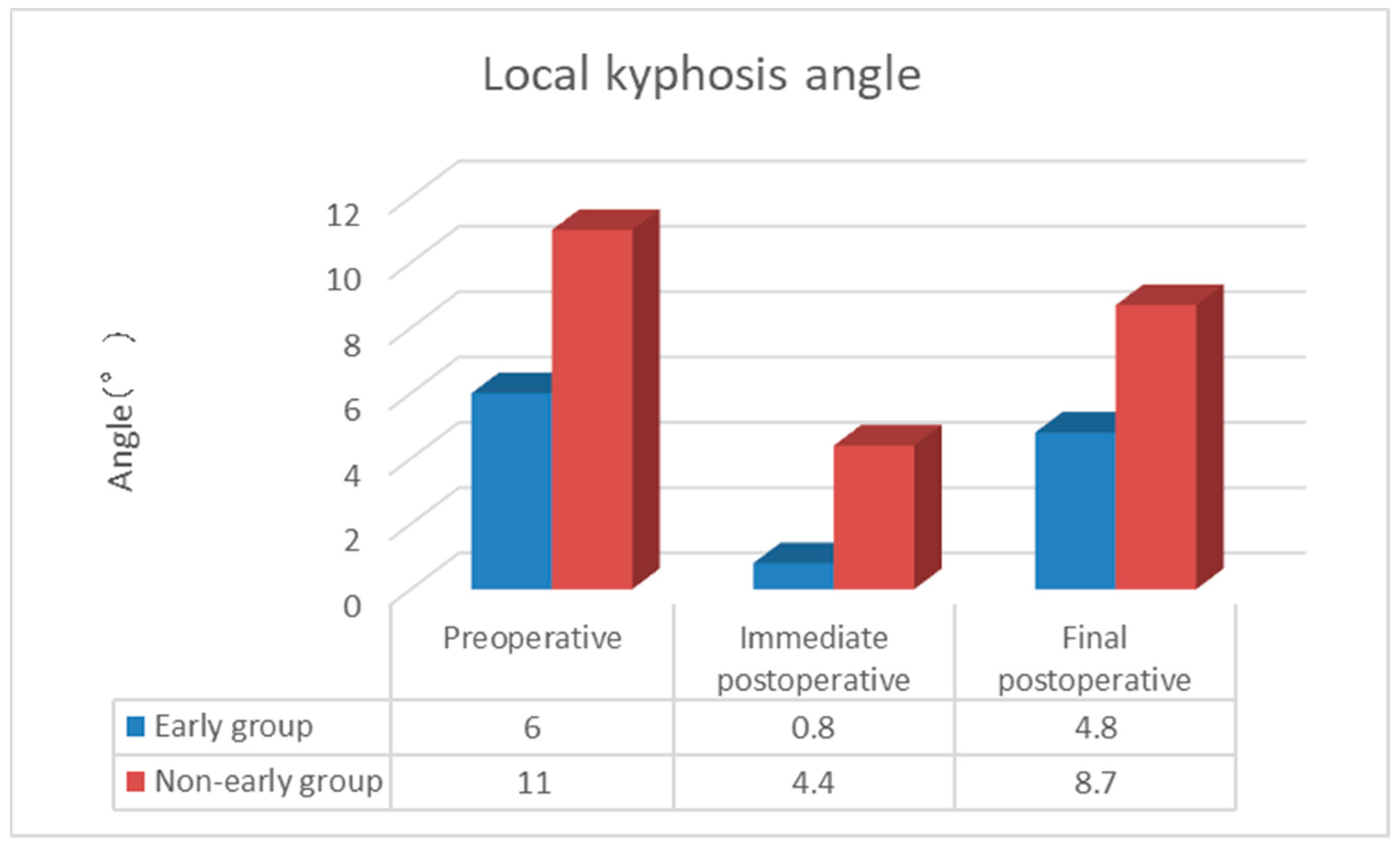
| Preoperative local kyphosis angle | −6.4 ± 13.3 | −14.9 ± 15.4 | 0.032 |
| Immediate postoperative local kyphosis angle | −1.2 ± 11.6 | −6.4 ± 12.7 | N.S. |
| Final postoperative local kyphosis angle | −4.8 ± 12.8 | −12.9 ± 13.8 | 0.020 |
| Change in local kyphosis angle | 4.9 ± 4.3 | 8.4 ± 5.6 | 0.025 |
| Risk Factor | Odds Ratio (95% Confidence Interval) | p-Value |
|---|---|---|
| Early BKP or Non-early BKP | 7.663 (1.802 to 32.582) | 0.006 |
| Change in vertebral wedge ratio | 1.058 (0.977 to 1.145) | 0.164 |
| Preoperative vertebral wedge ratio | 1.167 (1.036 to 1.315) | 0.011 |
| Preoperative local kyphosis angle | 0.777 (0.571 to 1.057) | 0.108 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takano, H.; Nojiri, H.; Shimura, A.; Teramoto, J.; Sugawara, Y.; Ishijima, M. Early Balloon Kyphoplasty Treatment for Osteoporotic Vertebral Fracture Reduces Adjacent Vertebral Fractures. Medicina 2024, 60, 1097. https://doi.org/10.3390/medicina60071097
Takano H, Nojiri H, Shimura A, Teramoto J, Sugawara Y, Ishijima M. Early Balloon Kyphoplasty Treatment for Osteoporotic Vertebral Fracture Reduces Adjacent Vertebral Fractures. Medicina. 2024; 60(7):1097. https://doi.org/10.3390/medicina60071097
Chicago/Turabian StyleTakano, Hiromitsu, Hidetoshi Nojiri, Arihisa Shimura, Juri Teramoto, Yuta Sugawara, and Muneaki Ishijima. 2024. "Early Balloon Kyphoplasty Treatment for Osteoporotic Vertebral Fracture Reduces Adjacent Vertebral Fractures" Medicina 60, no. 7: 1097. https://doi.org/10.3390/medicina60071097
APA StyleTakano, H., Nojiri, H., Shimura, A., Teramoto, J., Sugawara, Y., & Ishijima, M. (2024). Early Balloon Kyphoplasty Treatment for Osteoporotic Vertebral Fracture Reduces Adjacent Vertebral Fractures. Medicina, 60(7), 1097. https://doi.org/10.3390/medicina60071097







