High ADMA Is Associated with Worse Health Profile in Heart Failure Patients Hospitalized for Episodes of Acute Decompensation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Patients and Measurements
2.3. Statistical Analysis
3. Results
3.1. Characteristics of the Subjects
3.2. Variables Associated with High ADMA Levels
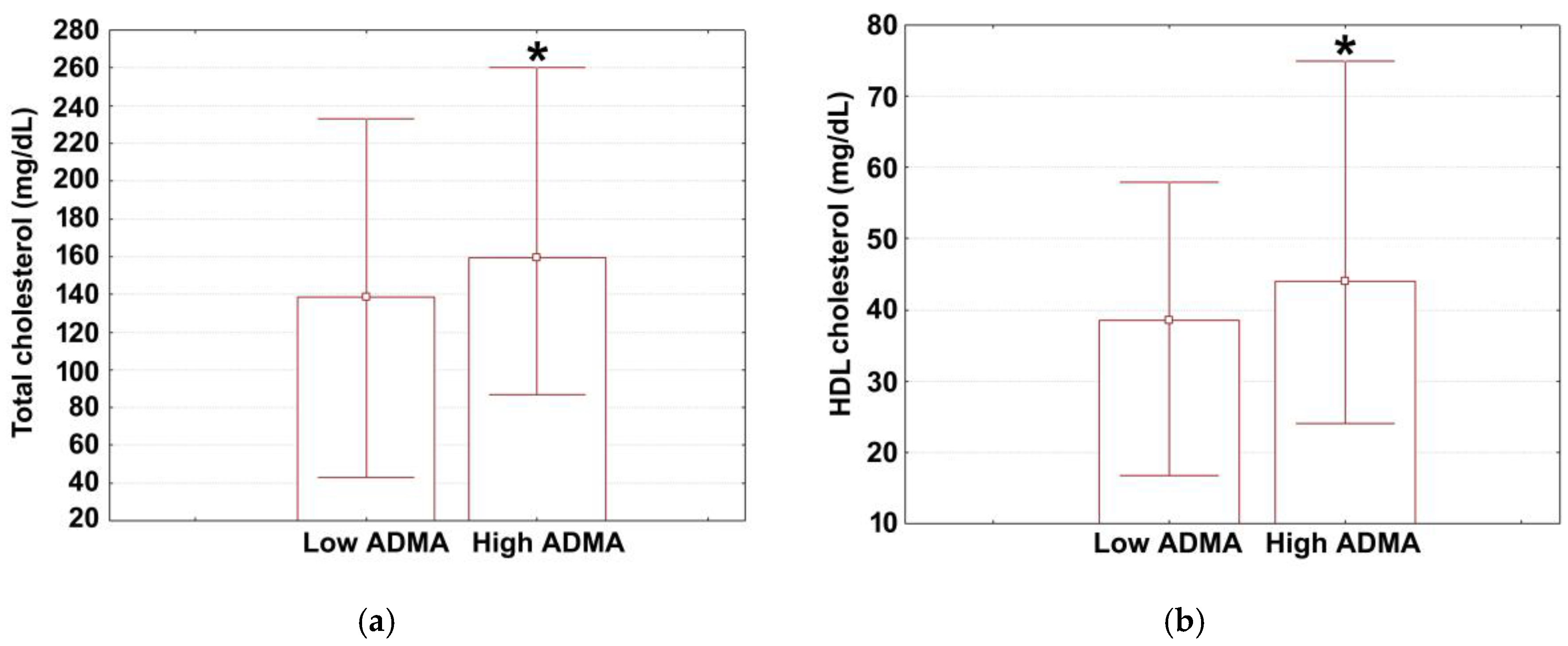
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mangini, S.; Pires, P.V.; Braga, F.G.M.; Bacal, F. Decompensated heart failure. Einstein 2013, 11, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Ide, T.; Kaku, H.; Matsushima, S.; Tohyama, T.; Enzan, N.; Funakoshi, K.; Sumita, Y.; Nakai, M.; Nishimura, K.; Miyamoto, Y.; et al. Clinical characteristics and outcomes of hospitalized patients with heart failure from the large-scale Japanese Registry Of Acute Decompensated Heart Failure (JROADHF). Circ. J. 2021, 85, 1438–1450. [Google Scholar] [CrossRef] [PubMed]
- Christiansen, M.N.; Køber, L.; Weeke, P.; Vasan, R.S.; Jeppesen, J.L.; Smith, J.G.; Gislason, G.H.; Torp-Pedersen, C.; Andersson, C. Age-specific trends in incidence, mortality, and comorbidities of heart failure in Denmark, 1995 to 2012. Circulation 2017, 135, 1214–1223. [Google Scholar] [CrossRef]
- Rosano, G.M.; Seferovic, P.; Savarese, G.; Spoletini, I.; Lopatin, Y.; Gustafsson, F.; Bayes-Genis, A.; Jaarsma, T.; Abdelhamid, M.; Miqueo, A.G.; et al. Impact analysis of heart failure across European countries: An ESC-HFA position paper. ESC Heart Fail. 2022, 9, 2767–2778. [Google Scholar] [CrossRef] [PubMed]
- Xanthopoulos, A.; Butler, J.; Parissis, J.; Polyzogopoulou, E.; Skoularigis, J.; Triposkiadis, F. Acutely decompensated versus acute heart failure: Two different entities. Heart Fail. Rev. 2020, 25, 907–916. [Google Scholar] [CrossRef] [PubMed]
- Kosowsky, J.M.; Abraham, W.T.; Storrow, A.B. Evaluation and management of acutely decompensated chronic heart failure in the Emergency Department. Congest. Heart Fail. 2001, 7, 124–136. [Google Scholar] [CrossRef] [PubMed]
- Lesyuk, W.; Kriza, C.; Kolominsky-Rabas, P. Cost-of-illness studies in heart failure: A systematic review 2004–2016. BMC Cardiovasc. Disord. 2018, 18, 74. [Google Scholar] [CrossRef]
- Voigt, J.; John, M.S.; Taylor, A.J.; Krucoff, M.W.; Reynolds, M.R.; Gibson, C.M. A reevaluation of the costs of heart failure and its implications for allocation of health resources in the United States. Clin. Cardiol. 2014, 37, 312–321. [Google Scholar] [CrossRef] [PubMed]
- Cyr, A.R.; Huckaby, L.V.; Shiva, S.S.; Zuckerbraun, B.S. Nitric oxide and endothelial dysfunction. Crit. Care Clin. 2020, 36, 307–321. [Google Scholar] [CrossRef]
- Sušić, L.; Maričić, L.; Šahinović, I.; Kralik, K.; Klobučar, L.; Ćosić, M.; Sušić, T.; Vincelj, J.; Burić, A.; Burić, M.; et al. The relationship of left ventricular diastolic dysfunction and asymmetrical dimethylarginine as a biomarker of endothelial dysfunction with cardiovascular risk assessed by systematic coronary risk Evaluation2 Algorithm and Heart Failure—A cross-sectional study. Int. J. Environ. Res. Public Health 2023, 20, 4433. [Google Scholar] [CrossRef]
- Dobbie, L.J.; Mackin, S.T.; Hogarth, K.; Lonergan, F.; Kannenkeril, D.; Brooksbank, K.; Delles, C. Validation of semi-automated flow-mediated dilation measurement in healthy volunteers. Blood Press. Monit. 2020, 25, 216–223. [Google Scholar] [CrossRef] [PubMed]
- Mućka, S.; Miodońska, M.; Jakubiak, G.K.; Starzak, M.; Cieślar, G.; Stanek, A. Endothelial function assessment by flow-mediated dilation method: A valuable tool in the evaluation of the cardiovascular system. Int. J. Environ. Res. Public Health 2022, 19, 11242. [Google Scholar] [CrossRef] [PubMed]
- Pan, W.; Lian, B.; Lu, H.; Liao, P.; Guo, L.; Zhang, M. Prognostic value of asymmetric dimethylarginine in patients with heart failure: A systematic review and meta-analysis. Biomed. Res. Int. 2020, 2020, 6960107. [Google Scholar] [CrossRef] [PubMed]
- Landim, M.B.P.; Casella Filho, A.; Chagas, A.C.P. Asymmetric dimethylarginine (ADMA) and endothelial dysfunction: Implications for atherogenesis. Clinics 2009, 64, 471–478. [Google Scholar] [CrossRef] [PubMed]
- Sibal, L.C.; Agarwal, S.; Home, P.D.; H Boger, R. The role of asymmetric dimethylarginine (ADMA) in endothelial dysfunction and cardiovascular disease. Curr. Cardiol. Rev. 2010, 6, 82–90. [Google Scholar] [CrossRef]
- Böger, R.H.; Sullivan, L.M.; Schwedhelm, E.; Wang, T.J.; Sullivan, L.M.; Schwedhelm, E.; Wang, T.J.; Maas, R.; Benjamin, E.J.; Schulze, F.; et al. Plasma asymmetric dimethylarginine and incidence of cardiovascular disease and death in the community. Circulation 2009, 119, 1592–1600. [Google Scholar] [CrossRef] [PubMed]
- Szuba, A.; Podgorski, M. Asymmetric dimethylarginine (ADMA) a novel cardiovascular risk factor-evidence from epidemiological and prospective clinical trials. Pharmacol. Rep. 2006, 58, 16–20. [Google Scholar] [PubMed]
- Lu, T.M.; Ding, Y.A.; Charng, M.J.; Lin, S.J. Asymmetrical dimethylarginine: A novel risk factor for coronary artery disease. Clin. Cardiol. 2003, 26, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Horowitz, J.D.; De Caterina, R.; Heresztyn, T.; Alexander, J.H.; Andersson, U.; Lopes, R.D.; Steg, P.G.; Hylek, E.M.; Moghan, P.; Hanna, M.; et al. Asymmetric and symmetric dimethylarginine predict outcomes in patients with atrial fibrillation: An ARISTOTLE substudy. J. Am. Coll. Cardiol. 2018, 72, 721–733. [Google Scholar] [CrossRef]
- Sen, N.; Ozlu, M.F.; Akgul, E.O.; Kanat, S.; Cayci, T.; Turak, O.; Yaman, H.; Sokmen, E.; Ozcan, F.; Maden, O.; et al. Elevated plasma asymmetric dimethylarginine level in acute myocardial infarction patients as a predictor of poor prognosis and angiographic impaired reperfusion. Atherosclerosis 2011, 219, 304–310. [Google Scholar] [CrossRef]
- Burger, A.L.; Stojkovic, S.; Diedrich, A.; Demyanets, S.; Wojta, J.; Pezawas, T. Elevated plasma levels of asymmetric dimethylarginine and the risk for arrhythmic death in ischemic and non-ischemic, dilated cardiomyopathy–A prospective, controlled long-term study. Clin. Biochem. 2020, 83, 37–42. [Google Scholar] [CrossRef]
- Zairis, M.N.; Patsourakos, N.G.; Tsiaousis, G.Z.; Georgilas, A.T.; Melidonis, A.; Makrygiannis, S.S.; Vellisaris, D.; Batika, P.C.; Argyrakis, K.S.; Tzeferos, S.P.; et al. Plasma asymmetric dimethylarginine and mortality in patients with acute decompensation of chronic heart failure. Heart 2012, 98, 860–864. [Google Scholar] [CrossRef] [PubMed]
- Saitoh, M.; Osanai, T.; Kamada, T.; Matsunaga, T.; Ishizaka, H.; Hanada, H.; Okumura, K. High plasma level of asymmetric dimethylarginine in patients with acutely exacerbated congestive heart failure: Role in reduction of plasma nitric oxide level. Heart Vessel. 2003, 18, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Zipes, L.D.; Libby, P.; Bonnow, O. Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 9th ed.; Elsevier: Amsterdam, The Netherlands, 2019; pp. 80–112. [Google Scholar]
- Getawa, S.; Bayleyegn, B. Platelet, neutrophil and lymphocyte quantitative abnormalities in patients with heart failure: A retrospective study. Vasc. Health Risk Manag. 2023, 5, 69–78. [Google Scholar] [CrossRef] [PubMed]
- Rayes, H.A.; Vallabhajosyula, S.; Barsness, G.W.; Anavekar, N.S.; Go, R.S.; Patnaik, M.S.; Kashani, K.B.; Jentzer, J.C. Association between anemia and hematological indices with mortality among cardiac intensive care unit patients. Clin. Res. Cardiol. 2020, 109, 6169–6627. [Google Scholar] [CrossRef] [PubMed]
- Pop-Busui, R.; Januzzi, J.L.; Bruemmer, D.; Butalia, S.; Green, J.B.; Horton, W.B.; Richardson, C.R. Heart failure: An underappreciated complication of diabetes. A consensus report of the American Diabetes Association. Diabetes Care 2022, 45, 1670–1690. [Google Scholar] [CrossRef] [PubMed]
- Laville, S.M.; Couturier, A.; Lambert, O.; Metzger, M.; Mansencal, N.; Jacquelinet, C.; Laville, M.; Frimat, L.; Fouque, D.; Combe, C.; et al. Urea levels and cardiovascular disease in patients with chronic kidney disease. Nephrol. Dial. Transplant. 2023, 38, 184–192. [Google Scholar] [CrossRef] [PubMed]
- Zanetti, D.; Bergman, H.; Burgess, S.; Assimes, T.L.; Bhalla, V.; Ingelsson, E. Urinary albumin, sodium, and potassium and cardiovascular outcomes in the UK Biobank: Observational and Mendelian randomization analyses. Hypertension 2020, 75, 714–722. [Google Scholar] [CrossRef] [PubMed]
- Ito, F.; Ito, T. High-density lipoprotein (HDL) triglyceride and oxidized HDL: New lipid biomarkers of lipoprotein-related atherosclerotic cardiovascular disease. Antioxidants 2020, 9, 362. [Google Scholar] [CrossRef] [PubMed]
- Soppert, J.; Lehrke, M.; Marx, N.; Jankowski, J.; Noels, H. Lipoproteins and lipids in cardiovascular disease: From mechanistic insights to therapeutic targeting. Adv. Drug Deliv. Rev. 2020, 159, 4–33. [Google Scholar] [CrossRef] [PubMed]
- Ewid, M.; Sherif, H.; Allihimy, A.S.; Alharbi, S.A.; Aldrewesh, D.A.; Alkuraydis, S.A.; Abazid, R. AST/ALT ratio predicts the functional severity of chronic heart failure with reduced left ventricular ejection fraction. BMC Res. Notes 2020, 13, 178. [Google Scholar] [CrossRef]
- Bellomo, R.; Kellum, J.A.; Ronco, C. Acute kidney injury. Lancet 2012, 380, 756–766. [Google Scholar] [CrossRef] [PubMed]
- Alam, S.; Hasan, M.K.; Neaz, S.; Hussain, N.; Hossain, M.F.; Rahman, T. Diabetes Mellitus: Insights from epidemiology, biochemistry, risk factors, diagnosis, complications and comprehensive management. Diabetology 2021, 2, 36–50. [Google Scholar] [CrossRef]
- Ginhină, C.; Vinereanu, D.; Popescu, B.A. Manual de Cardiologie al Societatii Romane de Cardiologie, 2nd ed.; Editura Medicală: Bucharest, Romania, 2020; pp. 456–510. [Google Scholar]
- Kernan, W.N.; Viscoli, C.M.; Makuch, R.W.; Brass, L.M.; Horwitz, R.I. Stratified randomization for clinical trials. J. Clin. Epidemiol. 1999, 52, 19–26. [Google Scholar] [PubMed]
- Popețiu, R.O.; Donath-Miklos, I.; Borta, S.M.; Moldovan, S.D.; Pilat, L.; Nica, D.V.; Pușchiță, M. Serum YKL-40 levels in patients with asthma or COPD: A pilot study. Medicina 2023, 59, 383. [Google Scholar] [CrossRef] [PubMed]
- Hadi, H.E.; Vincenzo, A.D.; Rossato, M. Relationship between heart disease and liver disease: A two-way street. Cells 2020, 9, 567. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, K.; Miyoshi, T.; Yoshida, M.; Akagi, S.; Saito, Y.; Ejiri, K.; Matsuo, N.; Ichikawa, K.; Iwasaki, K.; Naito, T.; et al. Pathophysiology and treatment of diabetic cardiomyopathy and heart failure in patients with diabetes mellitus. Int. J. Mol. Sci. 2022, 23, 3587. [Google Scholar] [CrossRef] [PubMed]
- Barlek, M.H.; Rouan, J.R.; Wyatt, T.G.; Helenowski, I.; Kibbe, M.R. The persistence of sex bias in high-impact clinical research. J. Surg. Res. 2022, 278, 364–374. [Google Scholar] [CrossRef] [PubMed]
- Guo, X.; Xing, Y.; Jin, W. Role of ADMA in the pathogenesis of microvascular complications in type 2 diabetes mellitus. Front. Endocrinol. 2023, 14, 1183586. [Google Scholar] [CrossRef] [PubMed]
- Schulze, F.; Vollert, J.; Maas, R.; Müller, R.; Schwedhelm, E.; Müller, C.; Böger, R.H.; Möckel, M. Asymmetric dimethylarginine predicts outcome and time of stay in hospital in patients attending an internal medicine emergency room. Clin. Chim. Acta 2009, 401, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Dückelmann, C.; Mittermayer, F.; Haider, D.G.; Altenberger, J.; Eichinger, J.; Wolzt, M. Asymmetric dimethylarginine enhances cardiovascular risk prediction in patients with chronic heart failure. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 2037–2042. [Google Scholar] [CrossRef]
- Sozio, E.; Hannemann, J.; Fabris, M.; Cifù, A.; Ripoli, A.; Sbrana, F.; Cescutti, D.; Vetrugno, L.; Fapranzi, S.; Bassi, F. The role of asymmetric dimethylarginine (ADMA) in COVID-19: Association with respiratory failure and predictive role for outcome. Sci. Rep. 2023, 13, 9811. [Google Scholar] [CrossRef] [PubMed]
- Papageorgiou, N.; Theofilis, P.; Oikonomou, E.; Lazaros, G.; Sagris, M.; Tousoulis, D. Asymmetric dimethylarginine as a biomarker in coronary artery disease. Curr. Top. Med. Chem. 2023, 23, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Zoccali, C.; Mallamaci, F.; Adamczak, M.; de Oliveira, R.B.; Massy, Z.A.; Sarafidis, P.; Agarwal, R.; Mark, P.B.; Kotanko, P.; Ferro, C.J. Cardiovascular complications in chronic kidney disease: A review from the European Renal and Cardiovascular Medicine Working Group of the European Renal Association. Cardiovasc. Res. 2023, 119, 2017–2032. [Google Scholar] [CrossRef]
- Varghese, T.P.; Tazneem, B. Unraveling the complex pathophysiology of heart failure: Insights into the role of renin-angiotensin-aldosterone system (RAAS) and sympathetic nervous system (SNS). Curr. Probl. Cardiol. 2024, 49, 102411. [Google Scholar] [CrossRef] [PubMed]
- Oliva-Damaso, E.; Oliva-Damaso, N.; Rodriguez-Esparragon, F.; Payan, J.; Baamonde-Laborda, E.; Gonzalez-Cabrera, F.; Rodriguez-Perez, J.C. Asymmetric (ADMA) and symmetric (SDMA) dimethylarginines in chronic kidney disease: A clinical approach. Int. J. Mol. Sci. 2019, 20, 3668. [Google Scholar] [CrossRef]
- Prowle, J.R.; Kolic, I.; Purdell-Lewis, J.; Taylor, R.; Pearse, R.M.; Kirwan, C.J. Serum creatinine changes associated with critical illness and detection of persistent renal dysfunction after AKI. Clin. J. Am. Soc. Nephrol. 2014, 9, 1015–1023. [Google Scholar] [CrossRef]
- Aronson, D.; Mittleman, M.A.; Burger, A.J. Elevated blood urea nitrogen level as a predictor of mortality in patients admitted for decompensated heart failure. Am. J. Med. 2004, 116, 466–473. [Google Scholar] [CrossRef]
- Filippatos, G.; Rossi, J.; Lloyd-Jones, D.M.; Gattis Stough, W.; Ouyang, J.; Shin, D.D.; O’connor, C.; Adams, K.A.; Orlandi, C.; Gheorghiade, M. Pronostic value of blood urea nitrogen in patients hospitalized withm worsening heart failure: Insights from the acute and chronic therapeutic impact of a vasopressin antagonist in chronic heart failure (ACTIV in CHF) study. J. Card. Fail. 2003, 13, 360–364. [Google Scholar] [CrossRef]
- Georgiopoulou, V.; Tang, W.H.W.; Giamouzis, G.; Li, S.; Deka, A.; Dunbar, S.A.; Butler, J.; Kalogeropoulos, A.P. Renal biomarkers and outcomes in outpatients with heart failure: The Atlanta cardiomyopathy consortium. Int. J. Cardiol. 2016, 218, 136–143. [Google Scholar] [CrossRef]
- Tall, A.R.; Yvan-Charvet, L. Cholesterol, inflammation and innate immunity. Nat. Rev. Immunol. 2015, 15, 104–116. [Google Scholar] [CrossRef]
- Pascariu, M.; Dinca, N.; Cojocariu, C.; Sisu, E.; Serb, A.; Birza, R.; Georgescu, M. Computed Mass-fragmentation energy profiles of some acetalized monosaccharides for identification in mass spectrometry. Symmetry 2022, 14, 1074. [Google Scholar] [CrossRef]
- Galvani, S.; Hla, T. Quality versus quantity: Making HDL great again. Arterioscler. Thromb. Vasc. Biol. 2017, 37, 1018–1019. [Google Scholar] [CrossRef] [PubMed]
- Trimarco, V.; Izzo, R.; Morisco, C.; Mone, P.; Virginia Manzi, M.; Falco, A.; Pacella, A.; Gallo, P.; Lembo, M.; Santulli, G.; et al. High HDL (high-density lipoprotein) cholesterol increases cardiovascular risk in hypertensive patients. Hypertension 2022, 79, 2355–2360. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Dhindsa, D.; Almuwaqqat, Z.; Ko, Y.A.; Mehta, A.; Alkhoder, A.A.; Alkhoder, A.A.; Alras, Z.; Desai, S.R.; Patel, K.J.; et al. Association between high-density lipoprotein cholesterol levels and adverse cardiovascular outcomes in high-risk populations. JAMA Cardiol. 2022, 7, 672–680. [Google Scholar] [CrossRef]
- Bojin, L.A.; Serb, A.F.; Pascariu, M.C.; Moaca, A.; Kostici, R.; Purcărea, V.L.; Penescu, M.; Ivan, M.H.; Georgescu, M.; Sisu, E. Assessment of antioxidant properties of different fomes fomentarius extracts. Farmacia 2020, 68, 322–328. [Google Scholar] [CrossRef]
- Popețiu, R.O.; Donath-Miklos, I.; Borta, S.M.; Rus, L.A.; Vîlcea, A.; Nica, D.V.; Pușchiță, M. Serum YKL-40 levels, leukocyte profiles, and acute exacerbations of advanced COPD. J. Clin. Med. 2023, 12, 6106. [Google Scholar] [CrossRef]
- Sim, J.; Lewis, M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef]
- Cleophas, T.J.; Zwinderman, A.H.; Cleophas, T.F.; Cleophas, E.P. Statistics Applied to Clinical Trials, 4th ed.; Springer: Dordrecht, The Netherlands, 2010; pp. 79–149. [Google Scholar]

| Characteristic | Strata | Low ADMA Patients | High ADMA Patients | p |
|---|---|---|---|---|
| Sex | Male | 32 (76.91%) | 34 (82.92%) | 0.588 |
| Female | 10 (23.81%) | 7 (17.08%) | ||
| Origin | Rural | 21 (50%) | 27 (65.86%) | 0.125 |
| Urban | 21 (50%) | 23 (56.09%) | ||
| Smoking status | Yes | 24 (57.41%) | 28 (68.29%) | 0.365 |
| No | 18 (42.86%) | 13 (31.71%) | ||
| Diabetes | Yes | 16 (38.09%) | 16 (39.02%) | 1 |
| No | 26 (61.91%) | 25 (60.98%) | ||
| Ischemic cardiomyopathy | Yes | 11 (26.19%) | 37 (90.24%) | 0.047 * |
| No | 31 (73.81%) | 4 (9.76%) | ||
| Tachyarrythmia | Yes | 13 (30.95%) | 20 (48.78%) | 0.144 |
| No | 29 (69.05%) | 21 (50.22%) | ||
| PH-LHD | Yes | 22 (52.39%) | 19 (46.34%) | 0.662 |
| No | 20 (47.61%) | 22 (53.66%) | ||
| Renal dysfunction | Yes | 22 (52.39%) | 20 (48.78%) | 0.624 |
| No | 20 (47.61%) | 21 (50.22%) |
| Characteristic | Low ADMA Patients | High ADMA Patients | Reference Range | p |
|---|---|---|---|---|
| Age | 69.5 (64; 79) | 70 (60; 77) | 0.396 | |
| SBP (mm Hg) | 142.5 (130; 155) | 140 (120; 160) | 90–130 | 0.761 |
| DBP (mm Hg) | 80 (73; 90) | 82 (120; 160) | 60–80 | 0.577 |
| HR (beats/min) | 91 (80; 120) | 90 (80; 108) | 60–100 | 0.741 |
| EF (%) | 40 (26; 55) | 45 (35; 54) | >50 | 0.471 |
| IVSd (cm) | 1.2 (1; 1.3) | 1.1. (1; 1.2) | 0.6–1.2 | 0.407 |
| LVPWT (cm) | 1.15 (1.1.; 1.3) | 1.1 (1; 1.2) | 0.8–1.1 | 0.155 |
| ALC (103 cells/μL) | 1.315 (1.080; 2.150) | 1.660 (1.130; 2.210) | 1–4 | 0.454 |
| ANC (103 cells/μL) | 5.375 (3.710; 6.850) | 6.470 (4.870; 7.940) | 2–8 | 0.104 |
| RDW-CV (%) | 15.1 (14.3; 16.4) | 14.55 (13.65; 16.20) | 11.5–15.4 | 0.116 |
| RDW-SD (fL) | 46.4 (44.6; 51)) | 45.6 (42.5; 49.5) | 39–46 | 0.229 |
| Hemoglobin (g/dL) | 13.25 (12.2; 14) | 13 (11.8; 14) | 12–18 | 0.362 |
| Glycemia (mg/dL) | 138 (113.8; 162.7) | 126 (107; 155) | <200 | 0.229 |
| GFR (mL/min) | 70.65 (47.5; 93.3) | 72.85 (61.5; 91.95) | >90 | 0.098 |
| Serum Na, admission (mmol/L) | 140.5 (138; 142) | 137 (134; 141) | 135–145 | 0.189 |
| Serum Na, discharge (mmol/L) | 139 (136; 142) | 137 (134; 141) | 135–145 | 0.110 |
| Serum K, admission (mmol/L) | 4.2 (4; 4.6) | 4.3 (3.9; 4.7) | 3.5–5 | 0.775 |
| Serum K, discharge (mmol/L) | 4.1 (3.9; 4.4) | 4.3. (3.9; 4.6) | 3.5–5 | 0.137 |
| LDL (mg/dL) | 94 (71; 121) | 96 (75.5; 123.40) | <100 | 0.755 |
| Triglycerides (mg/dL) | 103.5 (80; 135) | 105 (90; 155) | <150 | 0.676 |
| AST (UI/L) | 29 (20; 44) | 28 (21; 40) | 5–56 | 0.775 |
| ALT (UI/L) | 21.1 (16.4; 36) | 26 (16; 50) | 9–40 | 0.609 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vîlcea, A.; Borta, S.M.; Popețiu, R.O.; Alexandra, R.L.; Pilat, L.; Nica, D.V.; Pușchiță, M. High ADMA Is Associated with Worse Health Profile in Heart Failure Patients Hospitalized for Episodes of Acute Decompensation. Medicina 2024, 60, 813. https://doi.org/10.3390/medicina60050813
Vîlcea A, Borta SM, Popețiu RO, Alexandra RL, Pilat L, Nica DV, Pușchiță M. High ADMA Is Associated with Worse Health Profile in Heart Failure Patients Hospitalized for Episodes of Acute Decompensation. Medicina. 2024; 60(5):813. https://doi.org/10.3390/medicina60050813
Chicago/Turabian StyleVîlcea, Anamaria, Simona Maria Borta, Romana Olivia Popețiu, Rus Larisa Alexandra, Luminița Pilat, Dragoș Vasile Nica, and Maria Pușchiță. 2024. "High ADMA Is Associated with Worse Health Profile in Heart Failure Patients Hospitalized for Episodes of Acute Decompensation" Medicina 60, no. 5: 813. https://doi.org/10.3390/medicina60050813
APA StyleVîlcea, A., Borta, S. M., Popețiu, R. O., Alexandra, R. L., Pilat, L., Nica, D. V., & Pușchiță, M. (2024). High ADMA Is Associated with Worse Health Profile in Heart Failure Patients Hospitalized for Episodes of Acute Decompensation. Medicina, 60(5), 813. https://doi.org/10.3390/medicina60050813






