Associated Factor and Long-Term Clinical Outcomes for Patients with Postoperative Rotational Malreduction in Pediatric Supracondylar Humeral Fractures
Abstract
1. Introduction
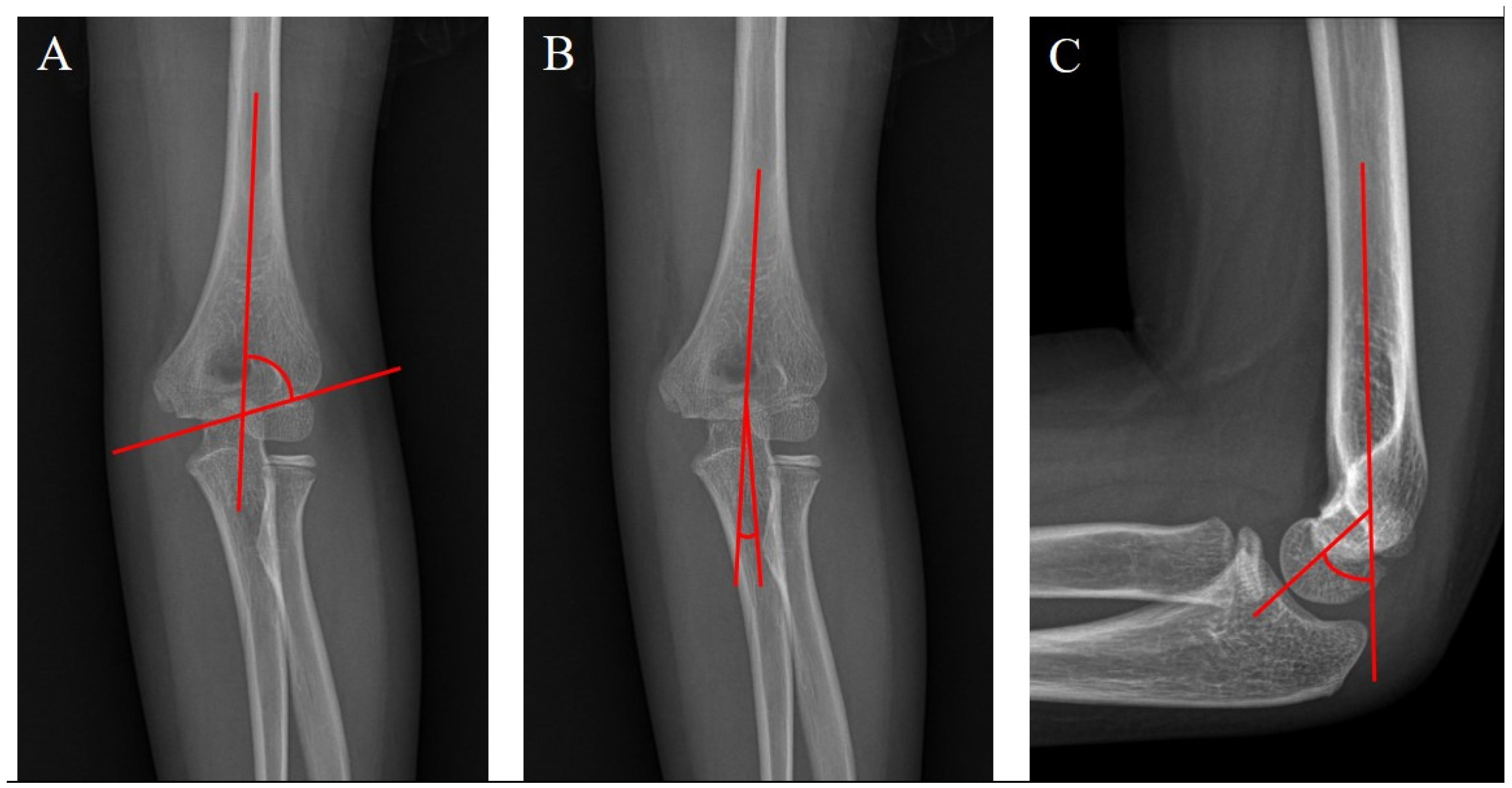
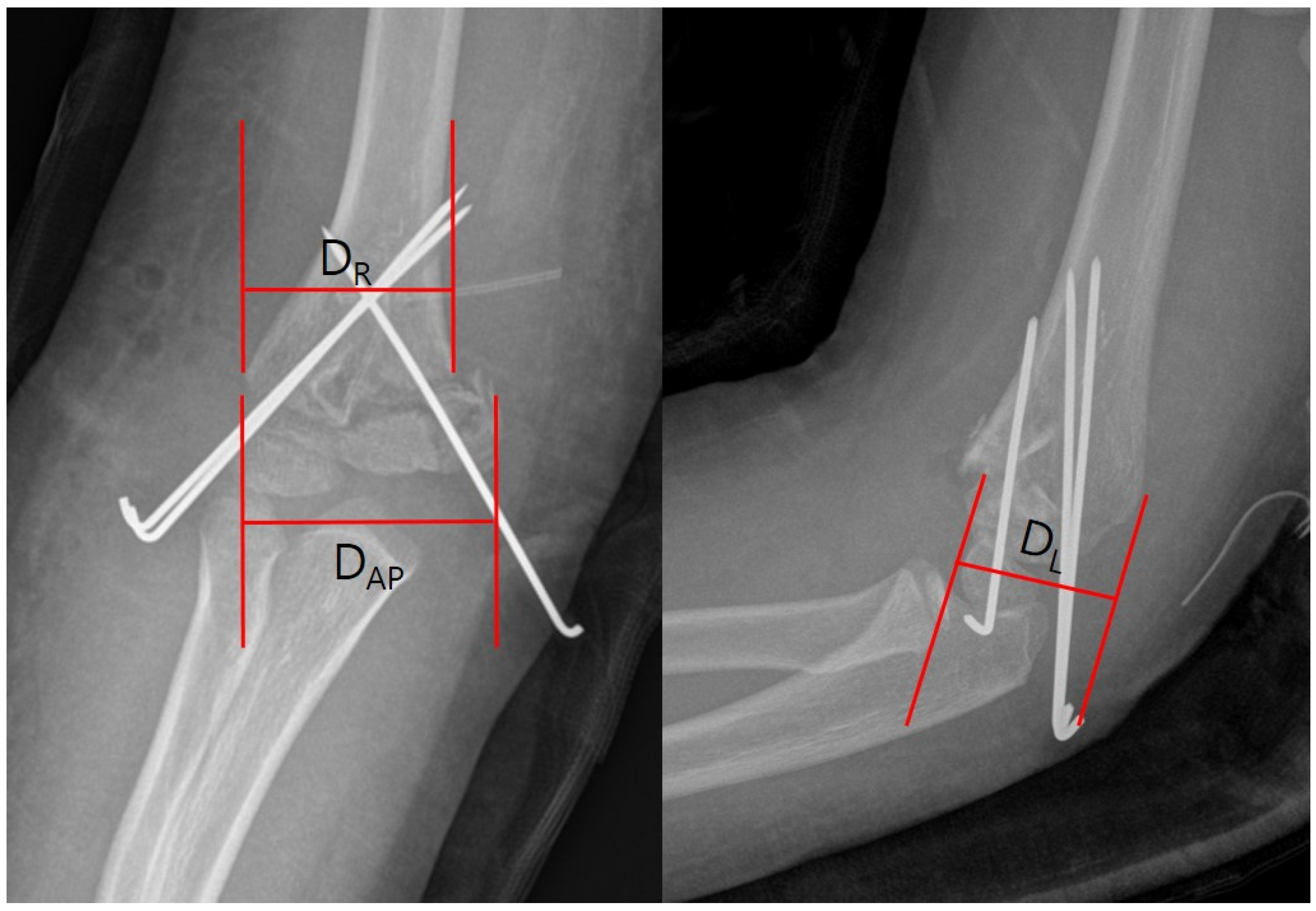
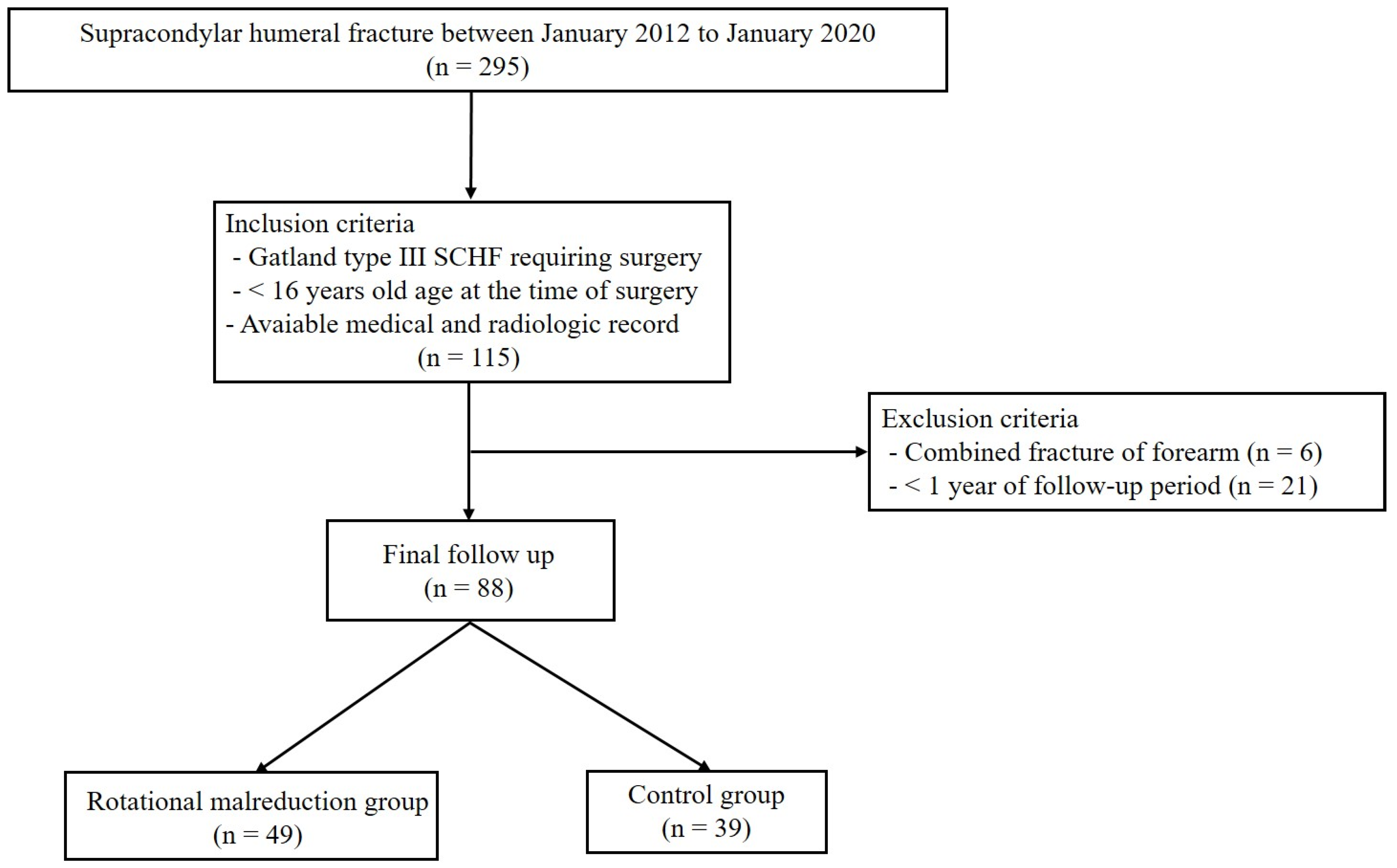
2. Methods
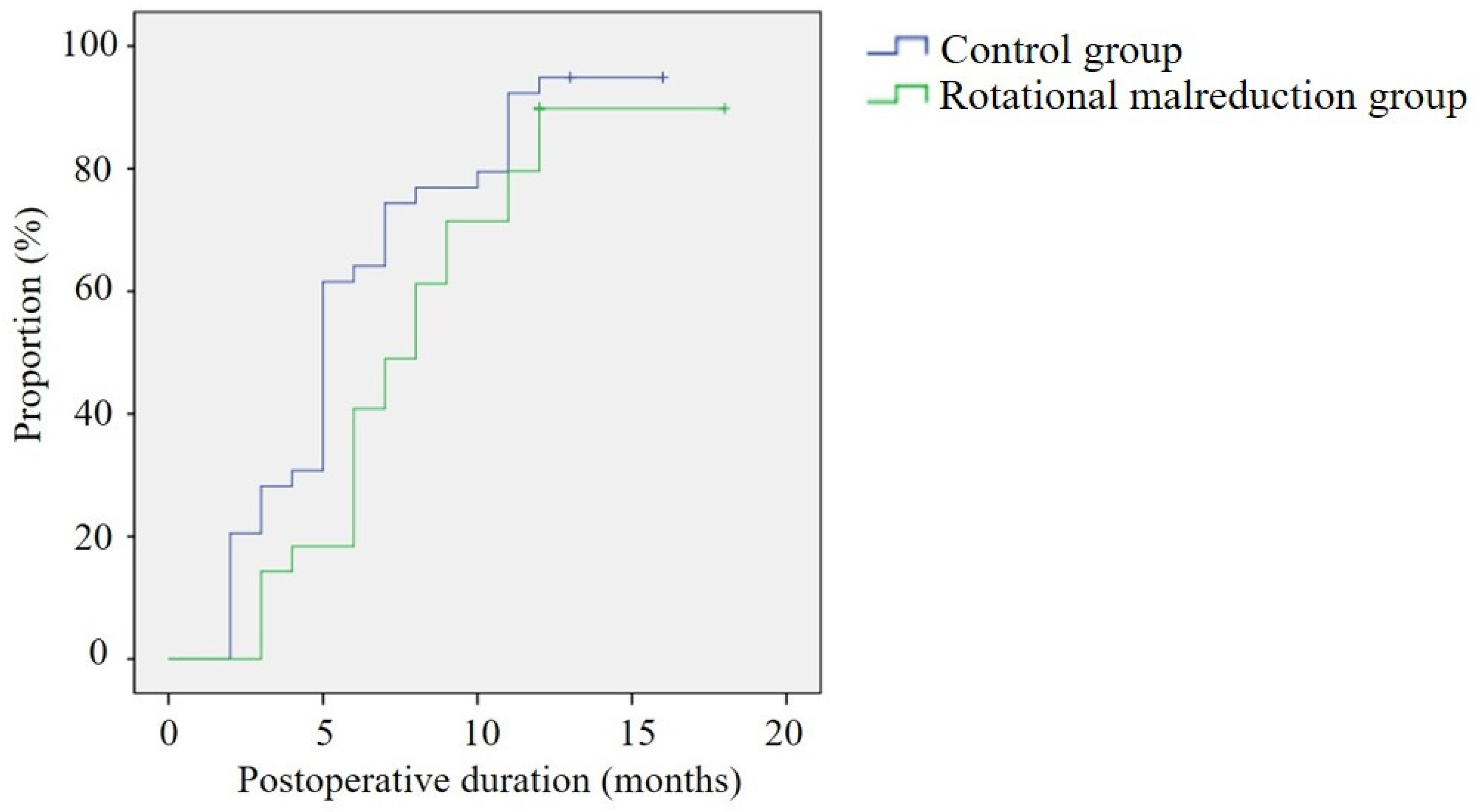
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Khoshbin, A.; Leroux, T.; Wasserstein, D.; Wolfstadt, J.; Law, P.W.; Mahomed, N.; Wright, J.G. The epidemiology of paediatric supracondylar fracture fixation: A population-based study. Injury 2014, 45, 701–708. [Google Scholar] [CrossRef] [PubMed]
- Omid, R.; Choi, P.D.; Skaggs, D.L. Supracondylar humeral fractures in children. J. Bone Joint Surg. Am. 2008, 90, 1121–1132. [Google Scholar] [CrossRef] [PubMed]
- Kropelnicki, A.; Ali, A.M.; Popat, R.; Sarraf, K.M. Paediatric supracondylar humerus fractures. Br. J. Hosp. Med. 2019, 80, 312–316. [Google Scholar] [CrossRef] [PubMed]
- Wilkins, K.E. The operative management of supracondylar fractures. Orthop. Clin. N. Am. 1990, 21, 269–289. [Google Scholar] [CrossRef]
- Ariyawatkul, T.; Eamsobhana, P.; Kaewpornsawan, K. The necessity of fixation in Gartland type 2 supracondylar fracture of the distal humerus in children (modified Gartland type 2A and 2B). J. Pediatr. Orthop. B 2016, 25, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Kivrak, A.; Ulusoy, I. How high is the quality of the videos about children’s elbow fractures on Toutube? J. Orthop. Surg. Res. 2023, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Lam, T.P.; Shen, W.Y. Closed reduction and percutaneous pinning for type III displaced supracondylar fractures of the humerus in children. J. Orthop. Trauma 1995, 9, 511–515. [Google Scholar] [CrossRef] [PubMed]
- Acton, J.D.; McNally, M.A. Baumann’s confusing legacy. Injury 2001, 32, 41–43. [Google Scholar] [CrossRef]
- Rashid, A.; Abdul-Jabar, H.; Bretherton, C.; Majed, A.; Corner, T. Sagittal plane malalignment in paediatric supracondylar fractures of the distal humerus: A review of the literature. Int. J. Orthop. 2016, 3, 609–615. [Google Scholar] [CrossRef]
- Linhart, W.E.; Kraus, T. Reconstruction of humeroradial joint. Oper. Orthop. Traumatol. 2008, 20, 396–408. [Google Scholar] [CrossRef] [PubMed]
- Greve, F.; Müller, M.; Wurm, M.; Biberthaler, P.; Singer, G.; Till, H.; Wegmann, H. Standalone axial malrotation after pediatric supracondylar fracture does not seem to be an indication for immediate postoperative revision surgery. Children 2022, 9, 1013. [Google Scholar] [CrossRef] [PubMed]
- Smith, L. Deformity following supracondylar fractures of the humerus. J. Bone Joint Surg. Am. 1965, 47, 1668. [Google Scholar] [CrossRef] [PubMed]
- Shin, H.D.; Kim, K.C.; Kim, D.K.; Lee, W.Y. The effect of rotational deformities on cubitus varus for supracondylar humerus fractures in children. J. Korean Orthop. Assoc. 2010, 45, 373–378. [Google Scholar] [CrossRef]
- Gartland, J.J. Management of supracondylar fractures of the humerus in children. Surg. Gynecol. Obstet. 1959, 109, 145–154. [Google Scholar] [PubMed]
- Wilkins, K.E. Fractures and dislocations of the elbow region. In Fractures in Children, 4th ed.; Rockwood, C.A., Wilkins, K.E., King, R.E., Eds.; Lippincott-Raven: Philadelphia, PA, USA, 1996; Volume 3, pp. 363–575. [Google Scholar]
- Leitch, K.K.; Kay, R.M.; Femino, J.D.; Tolo, V.T.; Storer, S.K.; Skaggs, D.L. Treatment of multidirectionally unstable supracondylar humeral fractures in children. A modified Gartland type-IV fracture. J. Bone Joint Surg. Am. 2006, 88, 980–985. [Google Scholar] [CrossRef] [PubMed]
- Henderson, E.R.; Egol, K.A.; van Bosse, H.J.; Schweitzer, M.E.; Pettrone, S.K.; Feldman, D.S. Calculation of rotational deformity in pediatric supracondylar humerus fractures. Skeletal. Radiol. 2007, 36, 229–235. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.C.; Matthews, J.G.; Benoit, R.L. Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J. Bone Joint Surg. Am. 1974, 56, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.S.; Mahar, A.T.; Miesen, D.; Newton, P.O. Displaced pediatric supracondylar humerus fractures: Biomechanical analysis of percutaneous pinning techniques. J. Pediatr. Orthop. 2002, 22, 440–443. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.; Han, J.H.; Park, H.; Kim, H.W.; Park, K.B. Prevalence and treatment outcome of displaced high-long oblique supracondylar humeral fractures in children. Front. Pediatr. 2021, 9, 739909. [Google Scholar] [CrossRef] [PubMed]
- Segal, D.; Cobb, L.; Little, K.J. Fracture obliquity is a predictor for loss of reduction in supracondylar humeral fractures in older children. J. Pediatr. Orthop. B 2020, 29, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Zionts, L.E.; McKellop, H.A.; Hathaway, R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J. Bone Joint Surg. 1994, 76, 253–256. [Google Scholar] [CrossRef] [PubMed]
- Skaggs, D.L.; Cluck, M.W.; Mostofi, A.; Flynn, J.M.; Kay, R.M. Lateral-entry pin fixation in the management of supracondylar fractures in children. J. Bone Joint Surg. 2004, 86, 702–707. [Google Scholar] [CrossRef]
- Archibeck, M.J.; Scott, S.M.; Peters, C.L. Brachialis muscle entrapment in displaced supracondylar humerus fractures: A technique of closed reduction and report of initial results. J. Pediatr. Orthop. 1997, 17, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Smuin, D.M.; Hennrikus, W.L. The effect of the pucker sign on outcomes of type III extension supracondylar fractures in children. J. Pediatr. Orthop. 2017, 37, e229–e232. [Google Scholar] [CrossRef] [PubMed]
- Aksakal, M.; Ermutlu, C.; Sarısözen, B.; Akesen, B. Approach to supracondylar humerus fractures with neurovascular compromise in children. Acta Orthop. Traumatol. Turc. 2013, 47, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Crombie, A.; Duncan, R. Closed reduction and percutaneous fixation of displaced paediatric supracondylar fractures of the elbow. Curr. Orthop. 2004, 18, 147–153. [Google Scholar] [CrossRef]
- Turgut, A.; Aksakal, A.M.; Öztürk, A.; Öztaş, S. A new method to correct rotational malalignment for closed reduction and percutaneous pinning in pediatric supracondylar humeral fractures. Acta Orthop. Traumatol. Turc. 2014, 48, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Novais, E.N.; Andrade, M.A.; Gomes, D.C. The use of a joystick technique facilitates closed reduction and percutaneous fixation of multidirectionally unstable supracondylar humeral fractures in children. J. Pediatr. Orthop. 2013, 33, 14–19. [Google Scholar] [CrossRef] [PubMed]
- Gedikbaş, M.; Balta, O.; Öztürk, T.; Erpala, F.; Eren, M.B.; Zengin, E.C. Does rotational deformity cause poor outcomes after pediatric supracondylar humerus fractures? Turk. J. Trauma Emerg. Surg. 2023, 29, 811–817. [Google Scholar] [CrossRef] [PubMed]

| Rotational Malreduction Group | Control Group | p | |
|---|---|---|---|
| No. of patients | 49 | 39 | |
| Age (mean ± SD) | 5.7 ± 2.3 | 5.7 ± 2.3 | |
| <5 | 18 | 12 | 0.695 |
| ≥5, <10 | 25 | 27 | 0.128 |
| >10 | 6 | 0 | |
| Sex, n (%) | 0.638 | ||
| Male | 27 (55.1) | 24 (61.5) | |
| Female | 22 (44.9) | 15 (38.5) | |
| Side, n (%) | |||
| Right | 21 (42.9) | 15 (38.5) | 1.000 |
| Left | 28 (47.1) | 24 (61.5) | |
| Type of fracture, n (%) | |||
| Extension type | 46 (93.9) | 38 (97.4) | 0.552 |
| Flexion type | 3 (6.1) | 1 (2.6) | |
| Pattern of fracture, n (%) | |||
| Transverse | 31 (63.3) | 34 (87.2) | 0.031 |
| Oblique | 18 (36.7) | 5 (12.8) | |
| Gartland type of fracture n (%) | 0.421 | ||
| III-a | 27 (55.1) | 27 (69.2) | |
| III-b | 19 (38.8) | 12 (30.8) | |
| IV | 4 (8.1) | 0 (0.0) | |
| Preoperative nerve palsy, n (%) | 9 (18.4) | 4 (10.3) | 0.309 |
| Pucker sign, n (%) | 5 (10.2) | 0 (0.0) | 0.016 |
| Time from injury to operation | 0.210 | ||
| <24 | 31 (63.3) | 27 (69.2) | |
| ≥24, <48 | 11 (22.4) | 5 (12.8) | |
| >48 | 8 (16.3) | 7 (17.9) | |
| Method of operation, n (%) | 0.116 | ||
| CRPP | 46 (93.9) | 39 (100.0) | |
| ORPP | 3 (6.1) | 0 (0.0) | |
| Operative time (mins) | 42.0 ± 24.7 | 31.7 ± 16.3 | 0.021 |
| Follow-up period (months) | 15.5 ± 4.0 | 16.6 ± 4.2 | 0.347 |
| Rotational Malreduction Group | Control Group | p | |
|---|---|---|---|
| Baumann angle (°) | |||
| Preoperative | 71.1 ± 13.2 | 76.3 ± 12.1 | 0.069 |
| Immediately postoperative | 75.2 ± 7.5 | 75.2 ± 6.3 | 0.983 |
| Final | 75.7 ± 6.2 | 74.9 ± 3.9 | 0.458 |
| Ulnohumeral angle (°) | |||
| Preoperative | 15.1 ± 9.6 | 13.8 ± 6.3 | 0.462 |
| Immediately postoperative | 16.3 ± 9.9 | 15.2 ± 9.6 | 0.385 |
| Final | 11.6 ± 5.7 | 12.8 ± 5.1 | 0.365 |
| Humerocapitellar angle (°) | |||
| Preoperative | 19.2 ± 15.4 | 31.1 ± 25.2 | 0.045 |
| Immediately postoperative | 42.2 ± 12.1 | 41.2 ± 11.6 | 0.475 |
| Final | 39.6 ± 11.9 | 40.3 ± 13.3 | 0.819 |
| Rotational angle (°) | |||
| Preoperative | 41.2 ± 20.2 | 26.2 ± 14.8 | 0.004 |
| Immediately postoperative | 25.8 ± 11.5 | 0.4 ± 1.1 | <0.001 |
| Final | 3.3 ± 6.7 | 0.0 ± 0.0 | 0.275 |
| Rotational Malreduction Group | Control Group | p | |
|---|---|---|---|
| Restoration of full ROM | |||
| achievement rate, n (%) | 44 (89.8) | 37 (94.9) | 0.456 |
| Time duration (months) | 7.8 ± 3.4 | 6.1 ± 3.7 | 0.018 |
| Flynn criteria, n (%) | 0.458 | ||
| Satisfactory | 44 (89.8) | 37 (94.9) | |
| Excellent | 34 (69.4) | 29 (78.4) | |
| Good | 10 (20.4) | 8 (20.5) | |
| Unsatisfactory | 5 (10.2) | 2 (5.1) | |
| Fair | 2 (4.1) | 1 (2.6) | |
| Poor | 3 (6.1) | 1 (2.6) | |
| Oxford elbow score | 94.5 ± 4.5 | 96.4 ± 3.7 | 0.684 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seo, K.B.; Kim, B.S.; Park, Y.-G.; Lim, C. Associated Factor and Long-Term Clinical Outcomes for Patients with Postoperative Rotational Malreduction in Pediatric Supracondylar Humeral Fractures. Medicina 2024, 60, 791. https://doi.org/10.3390/medicina60050791
Seo KB, Kim BS, Park Y-G, Lim C. Associated Factor and Long-Term Clinical Outcomes for Patients with Postoperative Rotational Malreduction in Pediatric Supracondylar Humeral Fractures. Medicina. 2024; 60(5):791. https://doi.org/10.3390/medicina60050791
Chicago/Turabian StyleSeo, Kyu Bum, Byung Suk Kim, Yong-Geun Park, and Chaemoon Lim. 2024. "Associated Factor and Long-Term Clinical Outcomes for Patients with Postoperative Rotational Malreduction in Pediatric Supracondylar Humeral Fractures" Medicina 60, no. 5: 791. https://doi.org/10.3390/medicina60050791
APA StyleSeo, K. B., Kim, B. S., Park, Y.-G., & Lim, C. (2024). Associated Factor and Long-Term Clinical Outcomes for Patients with Postoperative Rotational Malreduction in Pediatric Supracondylar Humeral Fractures. Medicina, 60(5), 791. https://doi.org/10.3390/medicina60050791





