Comparison of Oncological Outcomes between Transperitoneal and Retroperitoneal Approaches in Laparoscopic Nephroureterectomies for Upper Tract Urothelial Carcinoma
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Surgical Technique
2.3. Statistical Analysis
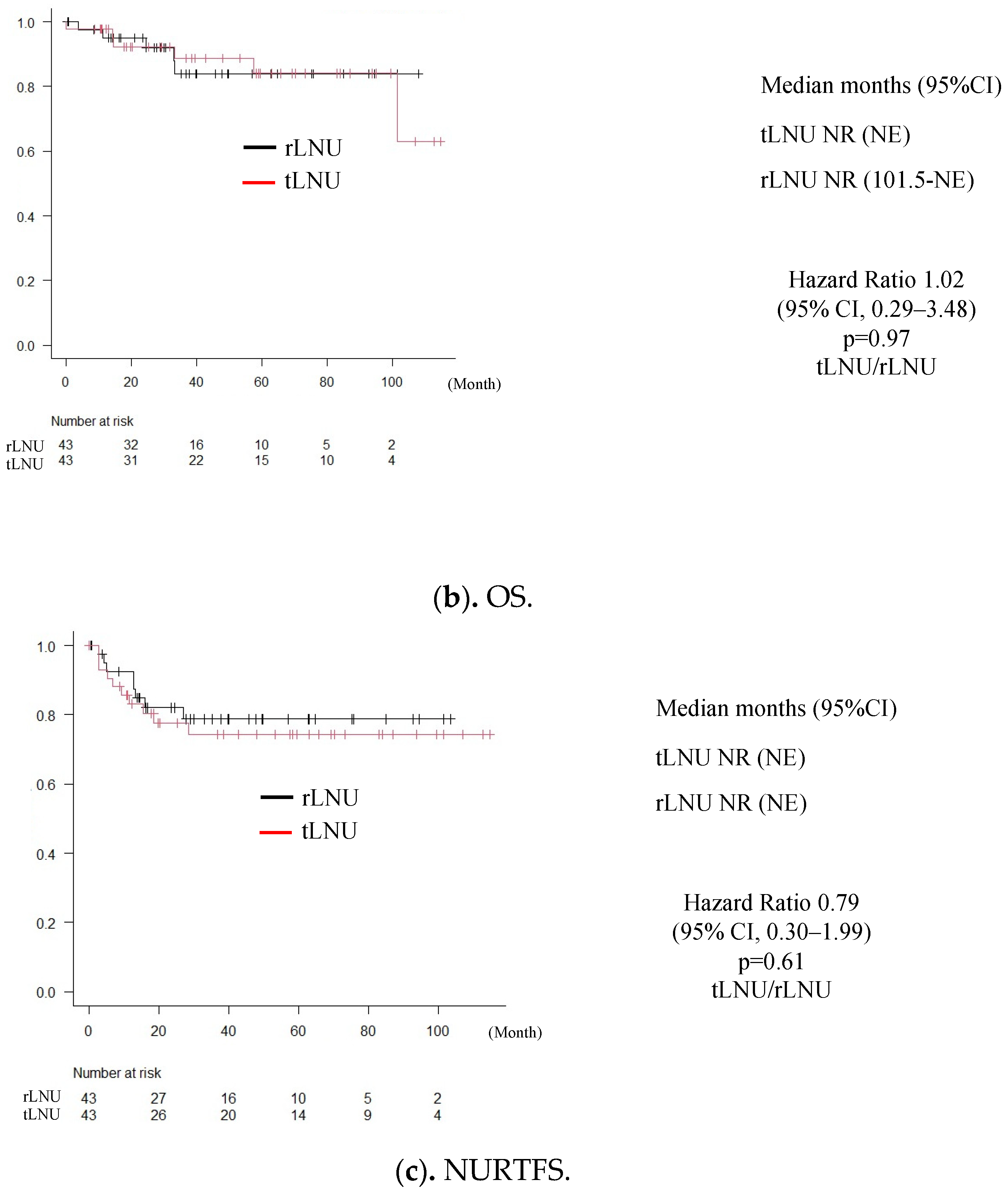
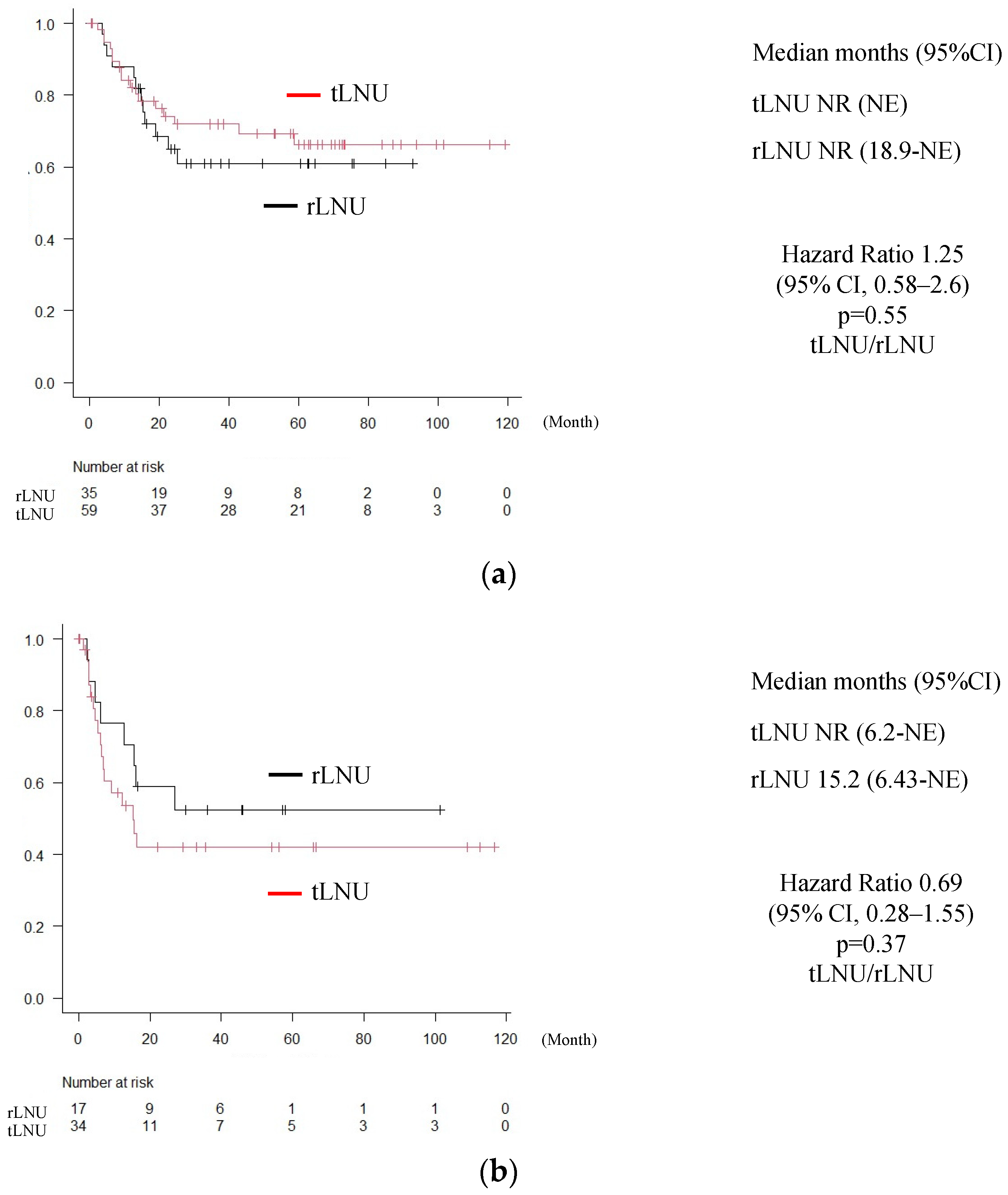
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Roupret, M.; Smyth, G.; Irani, J.; Guy, L.; Davin, J.L.; Saint, F.; Pfister, C.; Wallerand, H.; Rozet, F. Oncological risk of laparoscopic surgery in urothelial carcinomas. World J. Urol. 2009, 27, 81–88. [Google Scholar] [CrossRef]
- Clayman, R.V.; Kavoussi, L.R.; Figenshau, R.S.; Chandhoke, P.S.; Albala, D.M. Laparoscopic nephroureterectomy: Initial clinical case report. J. Laparoendosc. Surg. 1991, 1, 343–349. [Google Scholar] [CrossRef]
- Liu, F.; Guo, W.; Zhou, X.; Ding, Y.; Ma, Y.; Hou, Y.; Kong, X.; Wang, Z. Laparoscopic versus open nephroureterectomy for upper urinary tract urothelial carcinoma: A systematic review and meta-analysis. Medicine 2018, 97, e11954. [Google Scholar] [CrossRef]
- Piszczek, R.; Nowak, Ł.; Krajewski, W.; Chorbińska, J.; Poletajew, S.; Moschini, M.; Kaliszewski, K.; Zdrojowy, R. Oncological outcomes of laparoscopic versus open nephroureterectomy for the treatment of upper tract urothelial carcinoma: An updated meta-analysis. World J. Surg. Oncol. 2021, 19, 129. [Google Scholar] [CrossRef] [PubMed]
- Liu, G.; Yao, Z.; Chen, G.; Li, Y.; Liang, B. Laparoscopic compared with open nephroureterectomy in upper urinary tract urothelial carcinoma: A systemic review and a meta-analysis. Int. J. Clin. Pract. 2021, 75, e14639. [Google Scholar] [CrossRef]
- Rouprêt, M.; Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Cowan, N.C.; Dominguez-Escrig, J.L.; Gontero, P.; Hugh Mostafid, A.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur. Urol. 2021, 79, 62–79. [Google Scholar] [CrossRef] [PubMed]
- Shigeta, K.; Matsumoto, K.; Takeda, T.; Hattori, S.; Kaneko, G.; Matsushima, M.; Abe, T.; Tanaka, N.; Mizuno, R.; Asanuma, H.; et al. Evaluating the Oncological Outcomes of Pure Laparoscopic Radical Nephroureterectomy Performed for Upper-Tract Urothelial Carcinoma Patients: A Multicenter Cohort Study Adjusted by Propensity Score Matching. Ann. Surg. Oncol. 2021, 28, 465–473. [Google Scholar] [CrossRef] [PubMed]
- Xiao, C.; Wang, Y.; Hua, M.; Zhang, W.; Ren, G.; Yang, B.; Yang, Q. Complete transperitoneal laparoscopic nephroureterectomy in a single position for upper urinary tract urothelial carcinoma and comparative outcomes. World J. Surg. Oncol. 2021, 19, 195. [Google Scholar] [CrossRef]
- Miki, J.; Yanagisawa, T.; Iwatani, K.; Obayashi, K.; Fukuokaya, W.; Mori, K.; Urabe, F.; Tsuzuki, S.; Kimura, S.; Kimura, T.; et al. Supine extraperitoneal laparoscopic nephroureterectomy without patient repositioning. Int. J. Urol. 2021, 28, 163–168. [Google Scholar] [CrossRef]
- Ong, A.M.; Bhayani, S.B.; Pavlovich, C.P. Trocar site recurrence after laparoscopic nephroureterectomy. J. Urol. 2003, 170, 1301. [Google Scholar] [CrossRef]
- Liu, W.; Wang, Y.; Zhong, Z.; Jiang, H.; Ouyang, S.; Zhu, L.; Xu, R. Transperitoneal versus retroperitoneal laparoscopic nephroureterectomy in the management of upper urinary tract urothelial carcinoma: A matched-pair comparison based on perioperative outcomes. Surg. Endosc. 2016, 30, 5537–5541. [Google Scholar] [CrossRef]
- Ye, K.; Zhong, Z.; Zhu, L.; Ren, J.; Xiao, M.; Liu, W.; Xiong, W. Modified transperitoneal versus retroperitoneal laparoscopic radical nephroureterectomy in the management of upper urinary tract urothelial carcinoma: Best practice in a single center with updated results. J. Int. Med. Res. 2020, 48, 300060520928788. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Suh, Y.S.; Jeon, H.G.; Jeong, B.C.; Seo, S.I.; Jeon, S.S.; Lee, H.M.; Choi, H.Y.; Sung, H.H. Transperitoneal radical nephroureterectomy is associated with worse disease progression than retroperitoneal radical nephroureterectomy in patients with upper urinary tract urothelial carcinoma. Sci. Rep. 2019, 9, 6294. [Google Scholar] [CrossRef] [PubMed]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef] [PubMed]
- Zhu, P.Y.; Wang, L.; Li, K.P.; Yin, S.; Chen, X.B. Perioperative and oncologic outcomes of transperitoneal versus retroperitoneal laparoscopic nephroureterectomy for upper urinary tract urothelial carcinoma: A systematic review and pooled analysis of comparative outcomes. World J. Surg. Oncol. 2023, 21, 163. [Google Scholar] [CrossRef]
- Wang, X.; Yao, J.; Jin, X.; Zhang, X.; Lu, G.; Shao, Y.; Pan, J. Initial satisfying experience of total retroperitoneal laparoscopic radical nephroureterectomy: A retrospective comparative research. Transl. Androl. Urol. 2022, 11, 607–616. [Google Scholar] [CrossRef]
- Wu, J.F.; Lin, R.C.; Lin, Y.C.; Cai, W.H.; Zhu, Q.G.; Fang, D.; Xiong, G.Y.; Zhang, L.; Zhou, L.Q.; Ye, L.F.; et al. Comparison of efficacy and safety between two different methods of nephroureterectomy in two centers. Beijing Da Xue Xue Bao Yi Xue Ban 2019, 51, 646–652. [Google Scholar]
- Shigeta, K.; Matsumoto, K.; Ogihara, K.; Murakami, T.; Anno, T.; Umeda, K.; Izawa, M.; Baba, Y.; Sanjo, T.; Shojo, K.; et al. The clinicopathological characteristics of muscle-invasive bladder recurrence in upper tract urothelial carcinoma. Cancer Sci. 2021, 112, 1084–1094. [Google Scholar] [CrossRef] [PubMed]
- Margulis, V.; Shariat, S.F.; Matin, S.F.; Kamat, A.M.; Zigeuner, R.; Kikuchi, E.; Lotan, Y.; Weizer, A.; Raman, J.D.; Wood, C.G. Outcomes of radical nephroureterectomy: A series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer 2009, 115, 1224–1233. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, E.; Oya, M. Clinical practice patterns for upper tract urothelial carcinoma: A nationwide survey in Japan. Jpn. J. Clin. Oncol. 2016, 46, 768–774. [Google Scholar] [CrossRef]
- Ambrosini, F.; Mantica, G.; Marchi, G.; Vecchio, E.; Col, B.; Gaia Genova, L.; Trani, G.; Ferrari, A.; Terrone, C. Impact of Assistant Experience on Perioperative Outcomes of Simple and Radical Laparoscopic Nephrectomy: Does It Really Matter? Medicina 2023, 60, 45. [Google Scholar] [CrossRef] [PubMed]

| tLNU (n = 52) | rLNU (n = 93) | p-Value | |||
|---|---|---|---|---|---|
| Age, years | 76 (53–89) | 75 (43–88) | N.S. | ||
| Gender, male/female | 34/18 | 66/27 | N.S. | ||
| Body mass index, kg/m2 | 23.0 (16.4–42.1) | 21.9 (12.7–33.7) | |||
| Smoking (%) | 20 (38%) | 43 (46%) | |||
| Tumor location | |||||
| Renal pelvis | 21 | 54 | |||
| Ureter | 29 | 38 | |||
| Renal pelvis + ureter | 2 | 1 | |||
| Right/left | 19/33 | 43/50 | |||
| Neoadjuvant chemotherapy | 3 | 1 | |||
| Operative time, min | 294 (148–731) | 291 (143–490) | |||
| Laparoscopic surgery time, min | 211 (106–402) | 170 (50–314) | <0.001 | ||
| Estimated blood loss, mL | 50 (5–950) | 75 (5–720) | |||
| pT stage | |||||
| pT0, pTis, pTa, pT1, pT2 | 0, 3, 12, 11, 7 | 33 (63%) | 1, 15, 12, 18, 12 | 58 (62%) | |
| pT3, pT4 | 18, 1 | 19 (27%) | 31, 4 | 35 (38%) | N.S. |
| Location of metastasis | |||||
| Lymph node | 1 | 8 | |||
| Liver | 3 | 2 | |||
| Bone | 1 | 2 | |||
| Lung | 4 | 6 | |||
| Bladder | 13 | 20 | N.S. | ||
| Intrapelvic | 2 | 4 | |||
| Residual ureter | 1 | 1 | |||
| Adjuvant chemotherapy | 7 | 10 | |||
| Months after surgery | 34 (0.4–108) | 41.3 (0.1–120) | N.S. | ||
| History of bladder cancer | 12 | 9 | 0.03 | ||
| tLNU (n = 43) | rLNU (n = 43) | p-Value | |||
| Age, years | 76 (53–87) | 75 (54–86) | N.S. | ||
| Gender, male/female | 27/16 | 31/12 | N.S. | ||
| Body mass index, kg/m2 | 23.0 (16.4–42.1) | 21.9 (12.7–31.6) | |||
| Smoking (%) | 17 (40%) | 17 (40%) | |||
| Tumor location | |||||
| Renal pelvis | 21 | 54 | |||
| Ureter | 29 | 38 | |||
| Renal pelvis + ureter | 2 | 1 | |||
| Right/left | 17/26 | 20/23 | |||
| Neoadjuvant chemotherapy | 3 | 1 | |||
| Operative time, min | 279 (148–731) | 293 (143–490) | |||
| Laparoscopic surgery time, min | 200 (105–370) | 170 (79–314) | <0.001 | ||
| Estimated blood loss, mL | 45 (5–950) | 50 (5–720) | |||
| pT stage | |||||
| pT0, pTis, pTa, pT1, pT2 | 0, 3, 11, 10, 7 | 31 (72%) | 1, 8, 6, 11, 6 | 32 (74%) | |
| pT3, pT4 | 11, 1 | 12 (28%) | 9, 2 | 11 (26%) | N.S. |
| Location of metastasis | |||||
| Lymph node | 1 | 5 | |||
| Liver | 2 | 1 | |||
| Bone | 1 | 1 | |||
| Lung | 3 | 2 | |||
| Bladder | 12 | 11 | N.S. | ||
| Intrapelvic | 2 | 1 | |||
| Residual ureter | 1 | 1 | |||
| Adjuvant chemotherapy | 5 | 4 | |||
| Months after surgery | 33.3 (0.4–108) | 42.8 (0.1–115) | N.S. | ||
| History of bladder cancer | 11 | 3 | 0.02 | ||
| N.S.: not significant | |||||
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
| HR | 95%CI | p-Value | HR | 95%CI | p-Value | |
| Female vs. male | 1.35 | 0.76–2.33 | 0.28 | |||
| Age ≥ 75 vs. <75 | 1.02 | 0.98–1.05 | 0.21 | |||
| Smoking | 1.21 | 0.49–1.43 | 0.5 | |||
| Surgical approach (retro- vs. transperitoneal) | 1.03 | 0.599–1.83 | 0.91 | |||
| pT3≥ vs. pT2≤ | 2.09 | 1.21–3.56 | 0.01 | 2.31 | 1.33–3.99 | 0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Otoshi, T.; Yamasaki, T.; Matsue, T.; Yukimatsu, N.; Kato, M.; Machida, Y.; Iwai, T.; Kuratsukuri, K.; Uchida, J. Comparison of Oncological Outcomes between Transperitoneal and Retroperitoneal Approaches in Laparoscopic Nephroureterectomies for Upper Tract Urothelial Carcinoma. Medicina 2024, 60, 421. https://doi.org/10.3390/medicina60030421
Otoshi T, Yamasaki T, Matsue T, Yukimatsu N, Kato M, Machida Y, Iwai T, Kuratsukuri K, Uchida J. Comparison of Oncological Outcomes between Transperitoneal and Retroperitoneal Approaches in Laparoscopic Nephroureterectomies for Upper Tract Urothelial Carcinoma. Medicina. 2024; 60(3):421. https://doi.org/10.3390/medicina60030421
Chicago/Turabian StyleOtoshi, Taiyo, Takeshi Yamasaki, Taisuke Matsue, Nao Yukimatsu, Minoru Kato, Yuichi Machida, Tomoaki Iwai, Katsuyuki Kuratsukuri, and Junji Uchida. 2024. "Comparison of Oncological Outcomes between Transperitoneal and Retroperitoneal Approaches in Laparoscopic Nephroureterectomies for Upper Tract Urothelial Carcinoma" Medicina 60, no. 3: 421. https://doi.org/10.3390/medicina60030421
APA StyleOtoshi, T., Yamasaki, T., Matsue, T., Yukimatsu, N., Kato, M., Machida, Y., Iwai, T., Kuratsukuri, K., & Uchida, J. (2024). Comparison of Oncological Outcomes between Transperitoneal and Retroperitoneal Approaches in Laparoscopic Nephroureterectomies for Upper Tract Urothelial Carcinoma. Medicina, 60(3), 421. https://doi.org/10.3390/medicina60030421





