Successful Delayed Interval Delivery in Twin Pregnancy After Early Premature Rupture of Membranes of a Leading Fetus: A Case Report
Abstract
1. Introduction
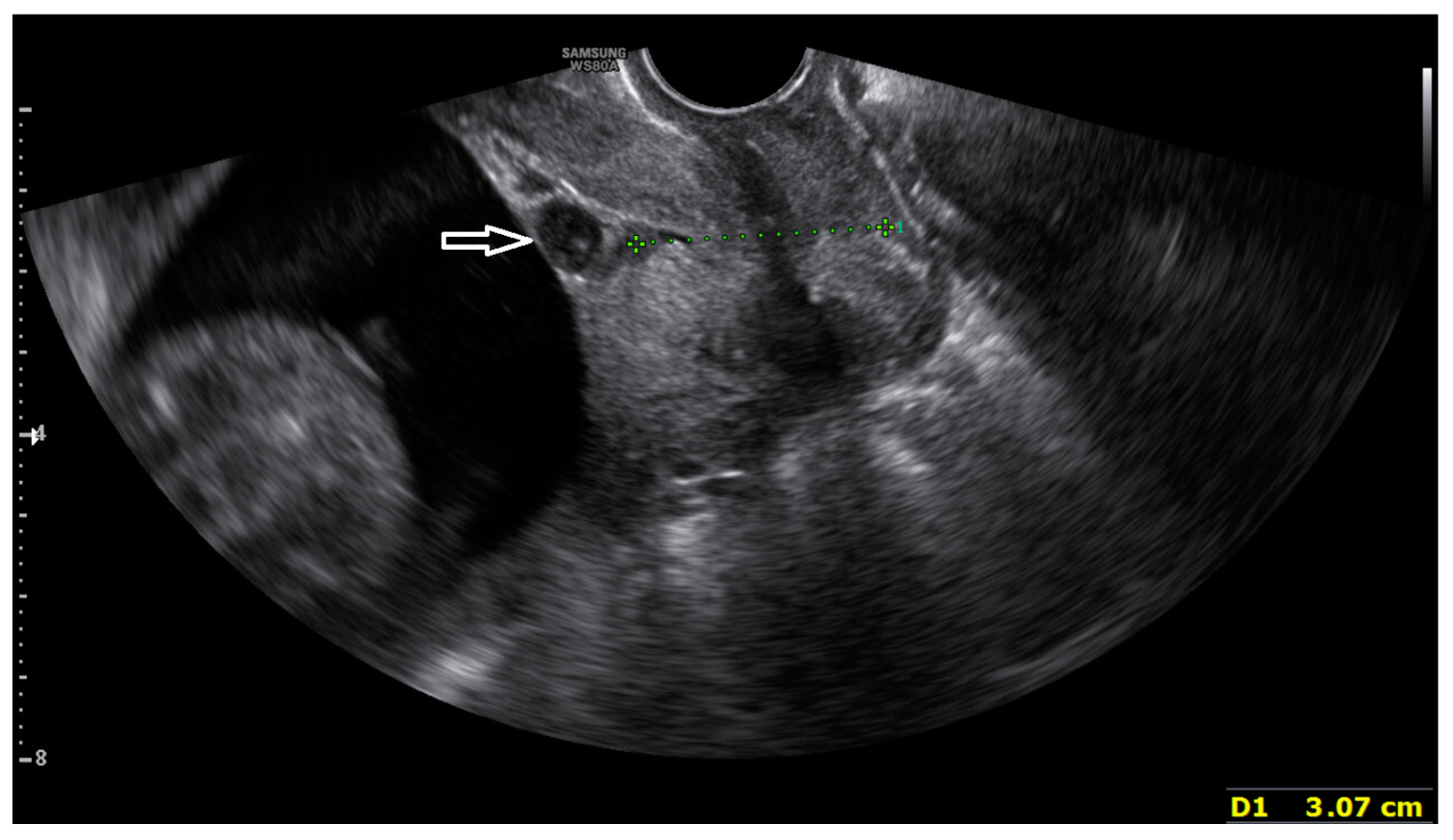
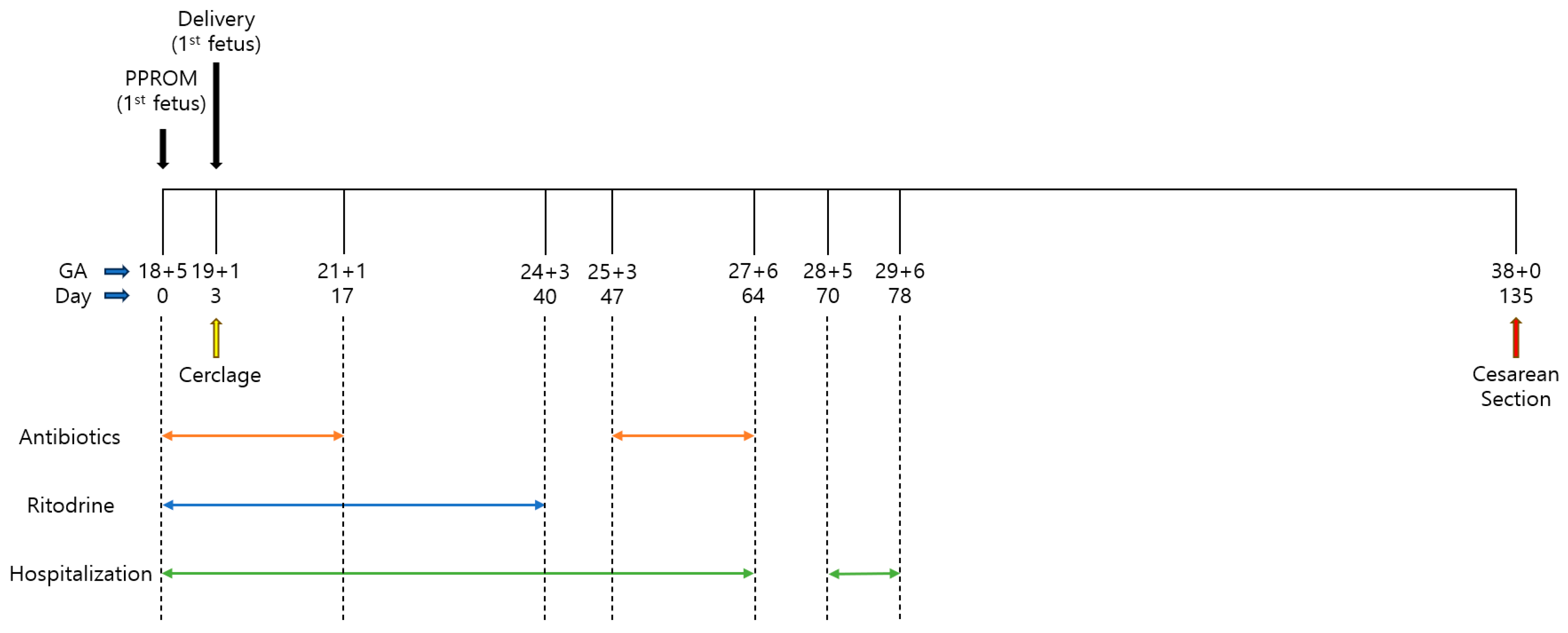
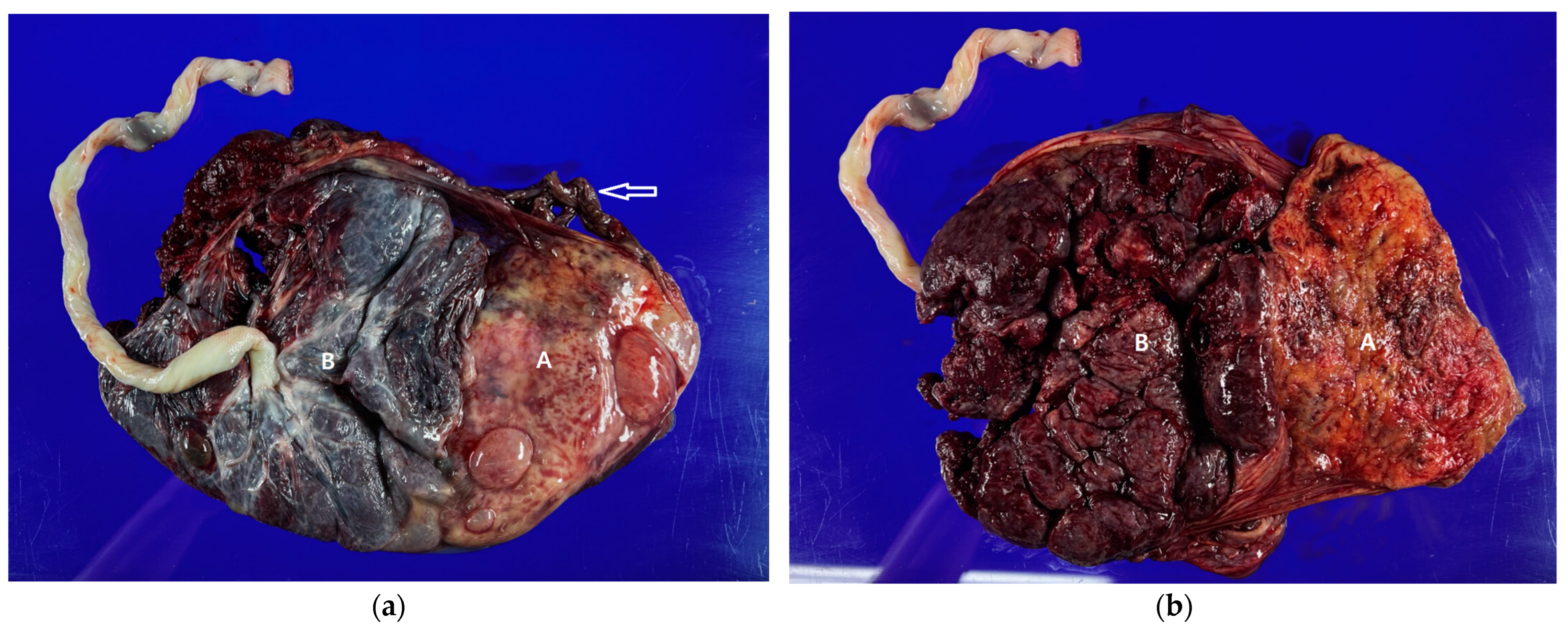
2. Case Report
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Osterman, M.J.; Hamilton, B.E.; Martin, J.A.; Driscoll, A.K.; Valenzuela, C.P. Births: Final Data for 2022. In National Vital Statistics Reports: From the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System; National Center for Health Statistics: Hyattsville, MD, USA, 2024; Volume 73, pp. 1–56. [Google Scholar]
- Feys, S.; Jacquemyn, Y. Delayed-interval delivery can save the second twin: Evidence from a systematic review. Facts Views Vis. ObGyn 2016, 8, 223. [Google Scholar] [PubMed]
- Caughey, A.B. Creasy and Resnik’s maternal-fetal medicine: Principles and practice. JAMA 2009, 302, 2154–2158. [Google Scholar] [CrossRef]
- Reinhard, J.; Reichenbach, L.; Ernst, T.; Reitter, A.; Antwerpen, I.; Herrmann, E.; Schlösser, R.; Louwen, F. Delayed interval delivery in twin and triplet pregnancies: 6 years of experience in one perinatal center. J. Perinat. Med. 2012, 40, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Doger, E.; Cakiroglu, Y.; Ceylan, Y.; Kole, E.; Ozkan, S.; Caliskan, E. Obstetric and neonatal outcomes of delayed interval delivery in cerclage and non-cerclage cases: An analysis of 20 multiple pregnancies. J. Obstet. Gynaecol. Res. 2014, 40, 1853–1861. [Google Scholar] [CrossRef] [PubMed]
- Kolben, T.; Fischer, D.; Ruehl, I.; Franz, M.; Hester, A.; Kolben, T.M.; Deppe, C.; Delius, M.; Friese, K.; Mahner, S. Delayed interval delivery in multiple gestations: The Munich experience. Arch. Gynecol. Obstet. 2019, 299, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Cui, H.; Li, H.; Yin, Z. Emergency cervical cerclage in delayed-interval delivery of twin pregnancies: A scoping review. BMC Pregnancy Childbirth 2024, 24, 323. [Google Scholar] [CrossRef] [PubMed]
- Raposo, M.I.; Cardoso, M.; Ormonde, M.; Stokreef, S.; Correia, L.; Pereira, A. Obstetric management of delayed-interval delivery. Case Rep. Women’s Health 2017, 16, 11–13. [Google Scholar] [CrossRef] [PubMed]
- Cheung, K.W.; Seto, M.T.Y.; Wang, W.; Lai, C.W.S.; Kilby, M.D.; Ng, E.H.Y. Effect of delayed interval delivery of remaining fetus(es) in multiple pregnancies on survival: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2020, 222, 306–319.e318. [Google Scholar] [CrossRef] [PubMed]
- Pakrashi, T.; Defranco, E.A. The relative proportion of preterm births complicated by premature rupture of membranes in multifetal gestations: A population-based study. Am. J. Perinatol. 2013, 30, 069–074. [Google Scholar] [CrossRef] [PubMed]
- Hamersley, S.L.; Coleman, S.K.; Bergauer, N.K.; Bartholomew, L.M.; Pinckert, T.L. Delayed-interval delivery in twin pregnancies. J. Reprod. Med. 2002, 47, 125–130. [Google Scholar] [PubMed]
- Petousis, S.; Goutzioulis, A.; Margioula-Siarkou, C.; Katsamagkas, T.; Kalogiannidis, I.; Agorastos, T. Emergency cervical cerclage after miscarriage of the first fetus in dichorionic twin pregnancies: Obstetric and neonatal outcomes of delayed delivery interval. Arch. Gynecol. Obstet. 2012, 286, 613–617. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, F.; Pereira, J.; Rodrigues, T.; Montenegro, N. The clinical challenge of delayed interval delivery in multiple pregnancies O desafio clínico do parto diferido na gravidez múltipla. Acta Obs. Ginecol. Port 2015, 9, 148–153. [Google Scholar]
- Aydin, Y.; Celiloglu, M. Delayed interval delivery of a second twin after the preterm labor of the first one in twin pregnancies: Delayed delivery in twin pregnancies. Case Rep. Obstet. Gynecol. 2012, 2012, 573824. [Google Scholar] [CrossRef] [PubMed]
- Oh, K.J.; Romero, R.; Park, J.Y.; Lee, J.; Conde-Agudelo, A.; Hong, J.-S.; Yoon, B.H. Evidence that antibiotic administration is effective in the treatment of a subset of patients with intra-amniotic infection/inflammation presenting with cervical insufficiency. Am. J. Obstet. Gynecol. 2019, 221, 140.e141–140.e118. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, T.; Sentilhes, L.; Lorthe, E.; Gallot, D.; Madar, H.; Doret-Dion, M.; Beucher, G.; Charlier, C.; Cazanave, C.; Delorme, P. Preterm premature rupture of the membranes: Guidelines for clinical practice from the French College of Gynaecologists and Obstetricians (CNGOF). Eur. J. Obstet. Gynecol. Reprod. Biol. 2019, 236, 1–6. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Prelabor rupture of membranes: ACOG practice bulletin, number 217. Obs. Gynecol. 2020, 135, e80–e97. [Google Scholar] [CrossRef] [PubMed]
- Yoneda, S.; Yoneda, N.; Fukuta, K.; Shima, T.; Nakashima, A.; Shiozaki, A.; Yoshino, O.; Kigawa, M.; Yoshida, T.; Saito, S. In which preterm labor-patients is intravenous maintenance tocolysis effective? J. Obstet. Gynaecol. Res. 2018, 44, 397–407. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jang, W.-K. Successful Delayed Interval Delivery in Twin Pregnancy After Early Premature Rupture of Membranes of a Leading Fetus: A Case Report. Medicina 2024, 60, 1800. https://doi.org/10.3390/medicina60111800
Jang W-K. Successful Delayed Interval Delivery in Twin Pregnancy After Early Premature Rupture of Membranes of a Leading Fetus: A Case Report. Medicina. 2024; 60(11):1800. https://doi.org/10.3390/medicina60111800
Chicago/Turabian StyleJang, Won-Kyu. 2024. "Successful Delayed Interval Delivery in Twin Pregnancy After Early Premature Rupture of Membranes of a Leading Fetus: A Case Report" Medicina 60, no. 11: 1800. https://doi.org/10.3390/medicina60111800
APA StyleJang, W.-K. (2024). Successful Delayed Interval Delivery in Twin Pregnancy After Early Premature Rupture of Membranes of a Leading Fetus: A Case Report. Medicina, 60(11), 1800. https://doi.org/10.3390/medicina60111800





