Spontaneous Retroperitoneal Bleeding in a Patient with Systemic Lupus Erythematosus
Abstract
1. Introduction
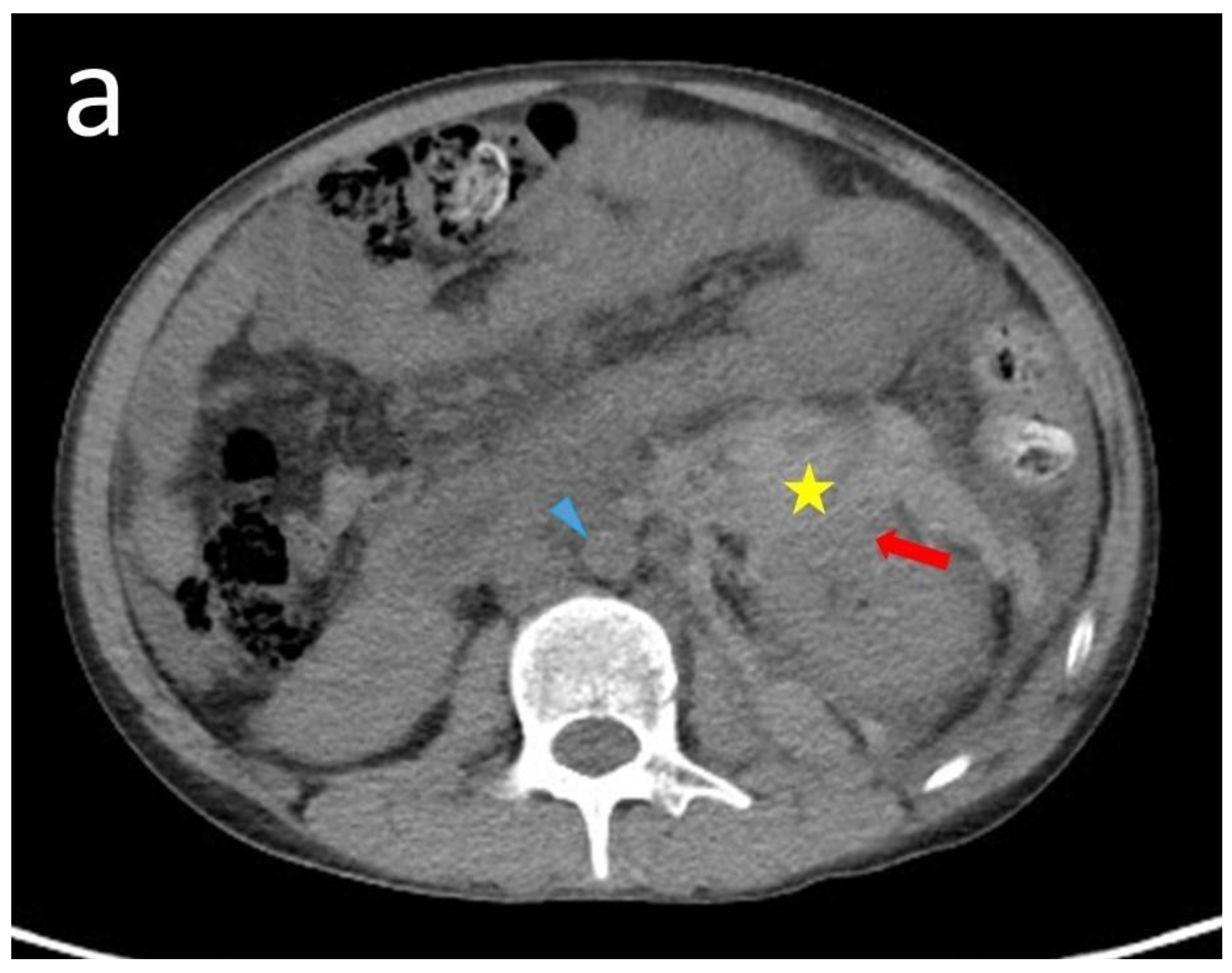
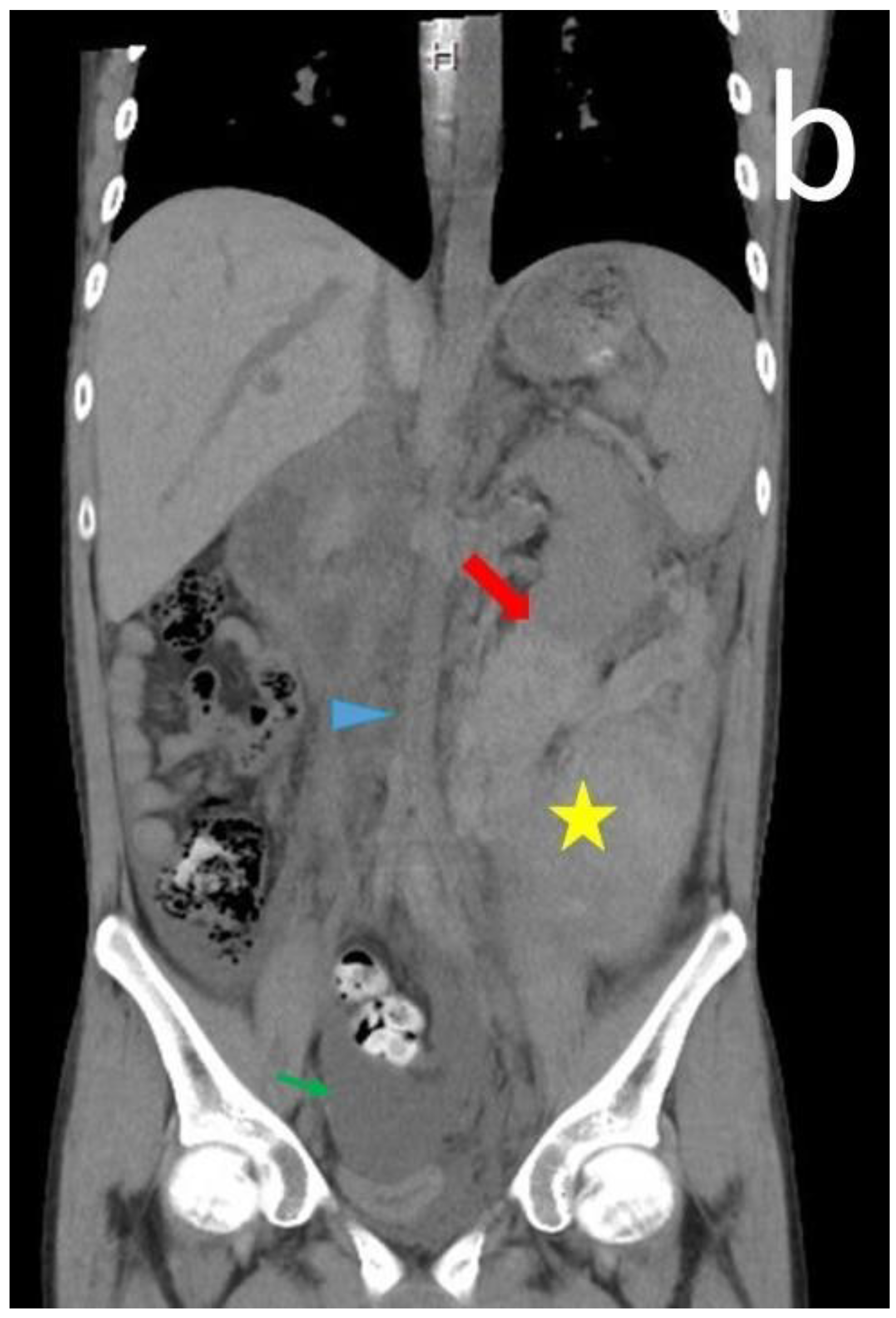
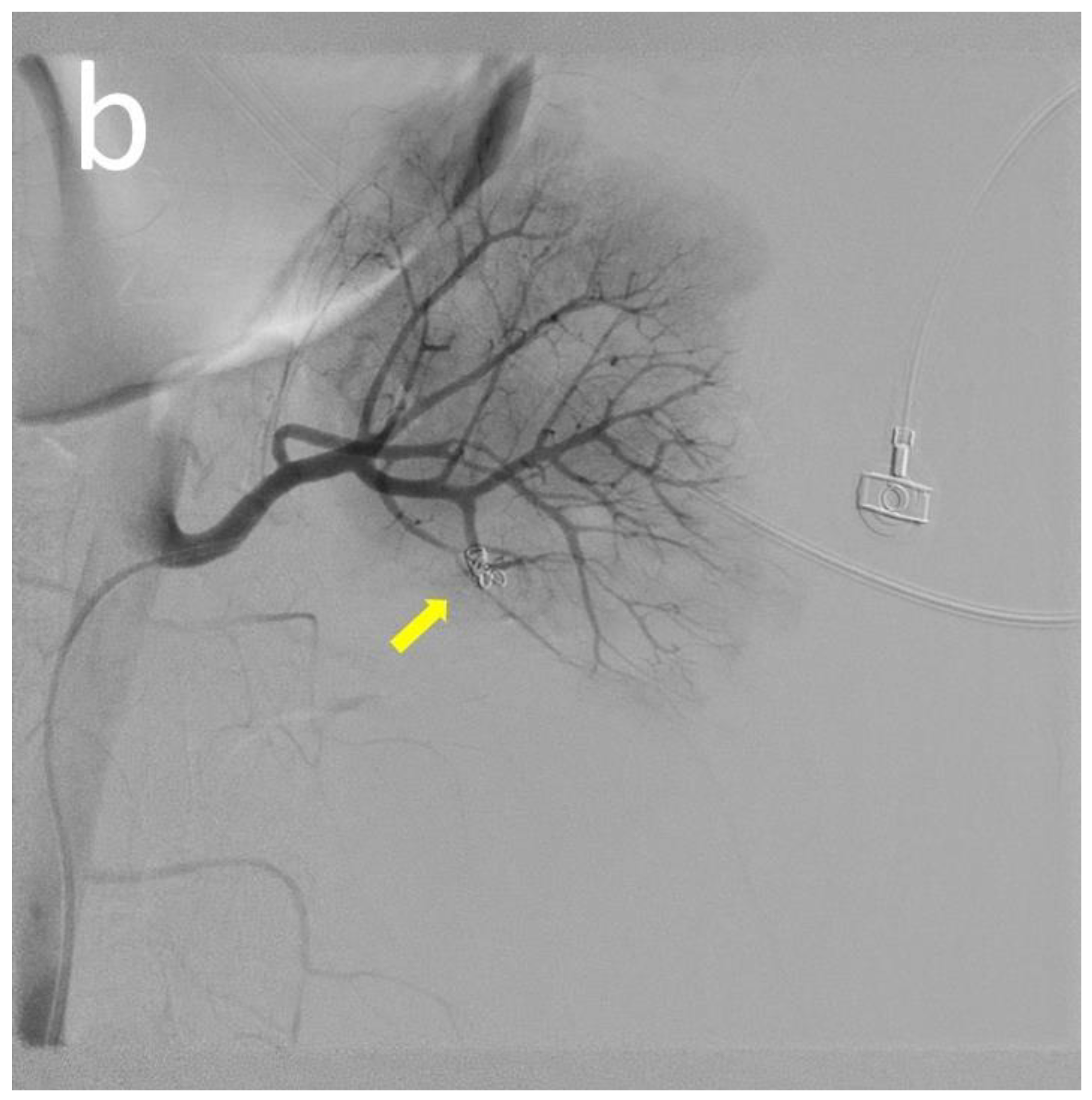
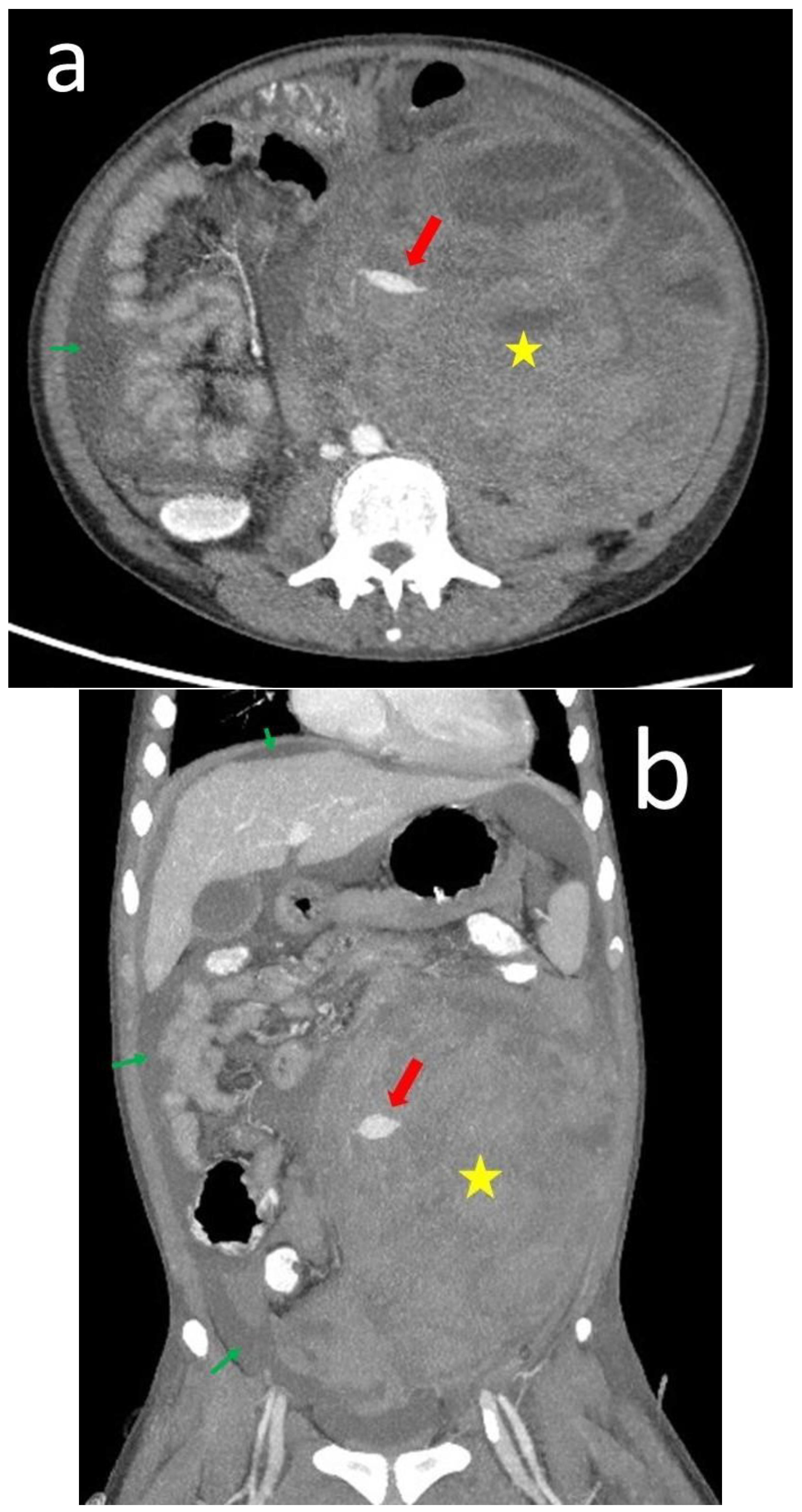
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- D’Andrea, D.M.; Coupaye-Gerard, B.; Kleyman, T.R.; Foster, M.H.; Madaio, M.P. Lupus autoantibodies interact directly with distinct glomerular and vascular cell surface antigens. Kidney Int. 1996, 49, 1214–1221. [Google Scholar] [CrossRef] [PubMed]
- Vlahakos, D.V.; Foster, M.H.; Adams, S.; Katz, M.; Ucci, A.A.; Barrett, K.J.; Datta, S.K.; Madaio, M.P. Anti-DNA antibodies form immune deposits at distinct glomerular and vascular sites. Kidney Int. 1992, 41, 1690–1700. [Google Scholar] [CrossRef] [PubMed]
- Sarabi, Z.S.; Chang, E.; Bobba, R.; Ibanez, D.; Gladman, D.; Urowitz, M.; Fortin, P.R. Incidence rates of arterial and venous thrombosis after diagnosis of systemic lupus erythematosus. Arthritis Care Res. Off. J. Am. Coll. Rheumatol. 2005, 53, 609–612. [Google Scholar] [CrossRef] [PubMed]
- Mcdougal, W.S.; Kursh, E.D.; Persky, L. Spontaneous Rupture of the Kidney with Perirenal Hematoma. J. Urol. 1975, 114, 181–184. [Google Scholar] [CrossRef] [PubMed]
- Hellström, P.A.; Mehik, A.; Talja, M.T.; Siniluoto, T.M.; Perälä, J.M.; Leinonen, S.S. Spontaneous subcapsular or perirenal haemorrhage caused by renal tumours: A urological emergency. Scand. J. Urol. Nephrol. 1999, 33, 17–23. [Google Scholar] [PubMed]
- Tsai, Y.-G.; Lai, J.-H.; Kuo, S.-Y.; Chen, H.-C.; Wan, H.-L.; Chang, D.-M. Ruptured renal microaneurysms complicated with a retroperitoneal abscess for a patient with systemic lupus erythematosus. Lupus 2003, 12, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Melamed, N.; Molad, Y. Spontaneous retroperitoneal bleeding from renal microaneurysms and pancreatic pseudocyst in a patient with systemic lupus erythematosus. Scand. J. Rheumatol. 2006, 35, 481–484. [Google Scholar] [CrossRef]
- Lin, Y.-Y.; Chen, J.-D.; How, C.-K.; Yen, D.H.-T. Spontaneous Perinephric Hemorrhage from a Hemorrhagic Renal Cyst. Intern. Med. 2010, 49, 2189–2190. [Google Scholar] [CrossRef][Green Version]
- Ku, J.H.; Kim, J.-K.; Ha, S.; Lee, J.W. Bilateral spontaneous perirenal haemorrhage in a patient on haemodialysis. Nephrol. Dial. Transplant. Plus 2009, 2, 412–414. [Google Scholar] [CrossRef]
- Libra, F.; Falsaperla, D.; Desiderio, C.M.; Santo Signorelli, S.; Palmucci, S.; Basile, A. Spontaneous bleeding in systemic lupus erythe-matosus: Endovascular treatment of two rare cases. Radiol. Case Rep. 2020, 15, 992–998. [Google Scholar] [CrossRef]
- Seong, S.-S.; Joung, C.-I. A case of spontaneous hemoperitoneum presenting as the initial manifestation of systemic lupus erythematosus. Korean J. Intern. Med. 2010, 25, 458. [Google Scholar] [CrossRef] [PubMed]
- Chao, C.-T.; Wang, W.-J.; Ting, J.-T. Wünderlich Syndrome from Lupus-Associated Vasculitis. Am. J. Kidney Dis. 2013, 61, 167–170. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.-H.; Wu, W.-J.; Hsiao, H.-L.; Yeh, H.-C.; Huang, C.-H.; Lee, Y.-C. Spontaneous Perirenal Hematoma: A Case Report. Kaohsiung J. Med. Sci. 2005, 21, 578–581. [Google Scholar] [CrossRef] [PubMed]
- Ufuk, F.; Herek, D. Life-threatening spontaneous kidney rupture in a rare case with systemic lupus erythematosus: Prompt diagnosis with computed tomography. Hemodial. Int. 2016, 20, E9–E11. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Jia, X.; Tong, X.; Niu, G.; Wang, R.; Liu, L.; Zhou, F. Spontaneous perirenal hemorrhage in systemic lupus erythematosus: A rare case report and literature review. BMC Nephrol. 2021, 22, 217. [Google Scholar] [CrossRef] [PubMed]
- Yacobovich, J.R.; Uziel, Y.; Friedman, Z.; Radnay, J.; Wolach, B. Diffuse muscular haemorrhage as presenting sign of juvenile systemic lupus erythematosus and lupus anticoagulant hypoprothrombinaemia syndrome. Rheumatology 2001, 40, 585–587. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.-C.; Chen, C.-H.; Yeh, S.-F.; Lai, J.-H.; Chang, D.-M. A spontaneous intercostal artery hemorrhage in systemic lupus erythematosus. Rheumatol. Int. 2012, 32, 829–831. [Google Scholar] [CrossRef] [PubMed]
- Abdulla, M. Spontaneous soft tissue haemorrhage in systemic lupus erythematosus. Reumatismo 2016, 68, 199–202. [Google Scholar] [CrossRef]
- Pérez, M.L.; Laso, R.V.; Velasco-Rodríguez, D.; Martín-Herrero, S.; Alfonzo, I.M.; García-Raso, A.; Llamas-Sillero, P. Lupus anticoagulant-hypoprothrombinemia syndrome: A cerebral bleeding case report as systemic lupus erythematosus debut. Reumatol. Clínica 2023, 19, 223–227. [Google Scholar] [CrossRef]
- Sahin, T.K.; Aladag, E.; Setterzade, E.; Guven, G.S.; Haznedaroglu, I.C.; Aksu, S. Spontaneous subepithelial hemorrhage of renal pelvis and ureter (Antopol-Goldman lesion) in hemophilia a patient with inhibitor: Case report and review of the literature. Medicine 2020, 99, e20851. [Google Scholar] [CrossRef]
- Sahin, S.; Adrovic, A.; Barut, K.; Canpolat, N.; Ozluk, Y.; Kilicaslan, I.; Caliskan, S.; Sever, L.; Kasapcopur, O. Juvenile systemic lupus erythematosus in Turkey: Demographic, clinical and laboratory features with disease activity and outcome. Lupus 2018, 27, 514–519. [Google Scholar] [CrossRef] [PubMed]
- Paul, R.; Bandyopadhyay, R.; Santra, S.; Patra, T.K. A Case of Systemic Lupus Erythematosus with Spontaneous Intracranial Epidural Hematoma. J. Med. Cases 2010, 1, 32–34. [Google Scholar] [CrossRef][Green Version]
- Itagaki, M.W.; Gregory, J.S. Spontaneous splenic artery hemorrhage with secondary antiphospholipid syndrome in lupus: A case report. Lupus 2005, 14, 479–482. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Zhang, G.; Zhang, L.; Luo, J.; Gao, L. Adrenal hemorrhage in a patient with systemic lupus erythematosus. J. Peking Univ. Health Sci. 2019, 51, 1178–1181. [Google Scholar]
- Chang, Y.-S.; Liu, C.-J.; Chen, W.-S.; Lai, C.-C.; Wang, S.-H.; Chen, T.-J.; Tzeng, C.-H.; Tsai, C.-Y.; Wang, S.-J. Increased Risk of Subarachnoid Hemorrhage in Patients with Systemic Lupus Erythematosus: A Nationwide Population-Based Study. Arthritis Care Res. 2012, 65, 601–606. [Google Scholar] [CrossRef]
- Dux, S.; Pitlik, S.; Boner, G.; Ben-Bassat, M.; Rosenfeld, J.B. Spontaneous Rupture of the Kidney in a Patient with Acute Autoimmune Disease. Urol. Int. 1982, 37, 130–133. [Google Scholar] [CrossRef]
- Mishriki, S.F.; Hopkinson, N.; Shepherd, D.F.; Parham, D.M.; Rundle, J.S. Bilateral rupture of the renal pelves associated with systemic lupus erythematosus. BJU Int. 1999, 83, 865–866. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions, and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |

| No | Study | Age | Gender | History of SLE (Years) | Symptoms | Renal Function | Coagulopathy | Tools for Diagnosis | Bleeding Site | Anatomical Anomalies | Autoantibody Test | Treatment | Pathological Result | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Tsai et al. [6] | 21 | Male | Recent | Abdominal pain Anemia (Hb: 8.1 g/dL) | Normal | Normal | CT | Multiple small aneurysms | Multiple small aneurysms in the bilateral renal arteries | Anti-dsDNA antibody | Steroid AZA HcQ | N/A | Alive |
| 2 | Melamed et al. [7] | 36 | Male | 10 | Flank pain Anemia (Hb: 7.4 g/dL) | N/A | Normal | CT | Multiple microaneurysms | Bilateral multiple renal artery microaneurysms | Anti-dsDNA antibody | Steroid CTX | N/A | Expired |
| 3 | Lin et al. [8] | 46 | Female | N/A | Anemia (Hct: 27.5%) | N/A | N/A | CT | Cystic lesion | Cystic lesion at upper pole of right kidney | N/A | Nephron sparing enucleation | Hemorrhagic cyst | Alive |
| 4 | Ku et al. [9] | 46 | Male | N/A | Flank pain with tender palpable mass Anemia | HD (8 yeas) | N/A | CT | Multiple cysts | Multiple cysts | N/A | Nephrectomy | Multiple cysts | Alive |
| 5 | Chao et al. [12] | 39 | Female | 20 | Abdominal pain Anemia (Hct: 16%) | HD (10 years) | Normal | CT | Small aneurysmal sacs | Small aneurysmal sacs in the right kidney | Anti-dsDNA antibody | Embolization Steroid | N/A | Alive |
| 6 | Chang et al. [13] | 30 | Male | 6 | Flank pain Anemia (Hb: 7.0 g/dL) | HD (6 years) | Thrombocytopenia | CT | N/A | N/A | N/A | Conservative | N/A | Alive |
| 7 | Furkan et al. [14] | 30 | Female | N/A | Fank pain Anemia (Hb: 7.8 g/dL) | HD (7 years) | Normal | CT | Rupture of the right kidney | no | Anti-dsDNA antibody | Conservative | N/A | Alive |
| 8 | Zhao et al. [15] | 33 | Female | Recent | Abdominal guarding and rigidity Flank tenderness Anemia (Hb: 4.2 g/dL) | Normal | Thrombocytopenia | CT | Distant branch of the left renal artery | No | Anti-dsDNA antibody, Anti-smith antibody | Embolization Steroid HcQ CsA CTX | N/A | Alive |
| 9 | Sahin et al. [20] | 32 | Male | N/A | Fank and abdominal tenderness | N/A | Coagulopathy | CT | Left ureteropelvic junction | N/A | N/A | FEIBA | N/A | Alive |
| 10 | Wang et al. [24] | 58 | Female | 1.5 | Anemia (Hb: 5.3 g/dL) | N/A | N/A | CT | Adrenal gland | N/A | Anti-dsDNA antibody, Anti-U1-snRNP/Sm Anticardiolipin antibody Anti-β2-glycoprotein Lupus anticoagulant | Conservative NOAC | N/A | Alive |
| 11 | Dux et al. [26] | 50 | Female | N/A | Palpated hypochondrium mass Loin pain Anemia (Hb: 8.1 g/dL) | ClCr: 2 mL/min no HD | N/A | IV pyelography | Lower pole of the kidney | N/A | N/A | Nephrectomy | Tear of 16 mm in the lower pole of kidney, no connection between the site of biopsy and rupture | Alive |
| 12 | MISHRIKI et al. [27] | 36 | Female | 12 | Left upper abdominal pain | Normal | N/A | CT | Presumed junction between the renal pelvis and kidney anteriorly | N/A | N/A | Nephrectomy Steroid AZA | Postmortem renal biopsy: within normal limits | Expired |
| 13 | Our case | 18 | Male | 12 | Flank pain Anemia(Hb: 6.7 g/dL) | Normal | Normal | CT | Angiodysplasia of the left renal artery & branch of IMA | N/A | Anti-dsDNA antibody Lupus anti-coagulant Anti-cardiolipin IgM | Embolization Steroid | N/A | Alive |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, W.-H.; Yang, D.-H. Spontaneous Retroperitoneal Bleeding in a Patient with Systemic Lupus Erythematosus. Medicina 2024, 60, 78. https://doi.org/10.3390/medicina60010078
Chen W-H, Yang D-H. Spontaneous Retroperitoneal Bleeding in a Patient with Systemic Lupus Erythematosus. Medicina. 2024; 60(1):78. https://doi.org/10.3390/medicina60010078
Chicago/Turabian StyleChen, Wei-Hung, and Deng-Ho Yang. 2024. "Spontaneous Retroperitoneal Bleeding in a Patient with Systemic Lupus Erythematosus" Medicina 60, no. 1: 78. https://doi.org/10.3390/medicina60010078
APA StyleChen, W.-H., & Yang, D.-H. (2024). Spontaneous Retroperitoneal Bleeding in a Patient with Systemic Lupus Erythematosus. Medicina, 60(1), 78. https://doi.org/10.3390/medicina60010078







