Sodium Thiosulfate for Calciphylaxis Treatment in Patients on Peritoneal Dialysis: A Systematic Review
Abstract
1. Introduction
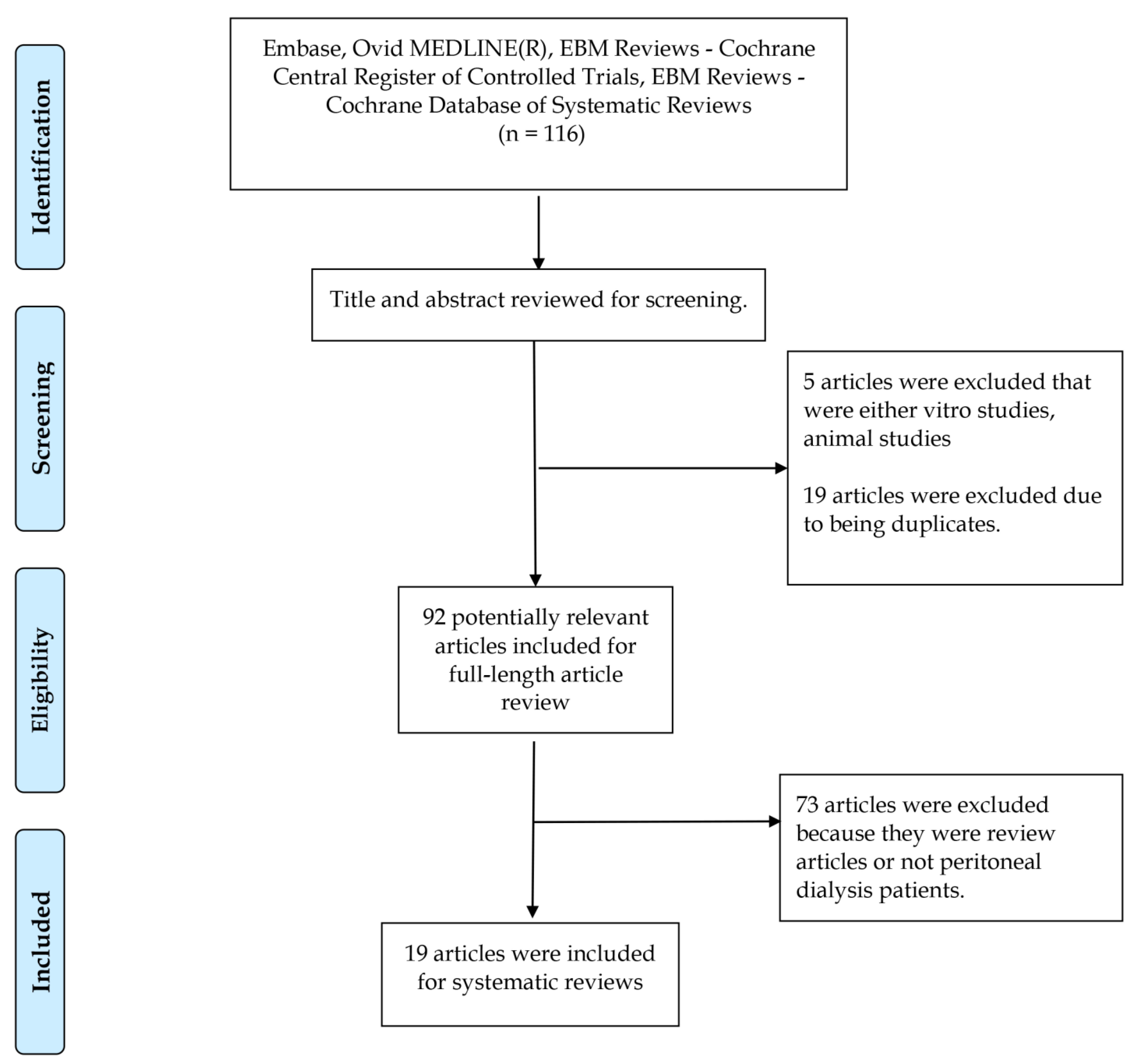
2. Materials and Methods
2.1. Information Sources and Search Strategy
Ovid MEDLINE Search
EMBASE Search
Cochrane CENTRAL and Database of Systematic Reviews Searches
2.2. Selection Criteria
2.3. Data Abstraction
2.4. Evaluation of Bias Risk
2.5. Statistical Analysis
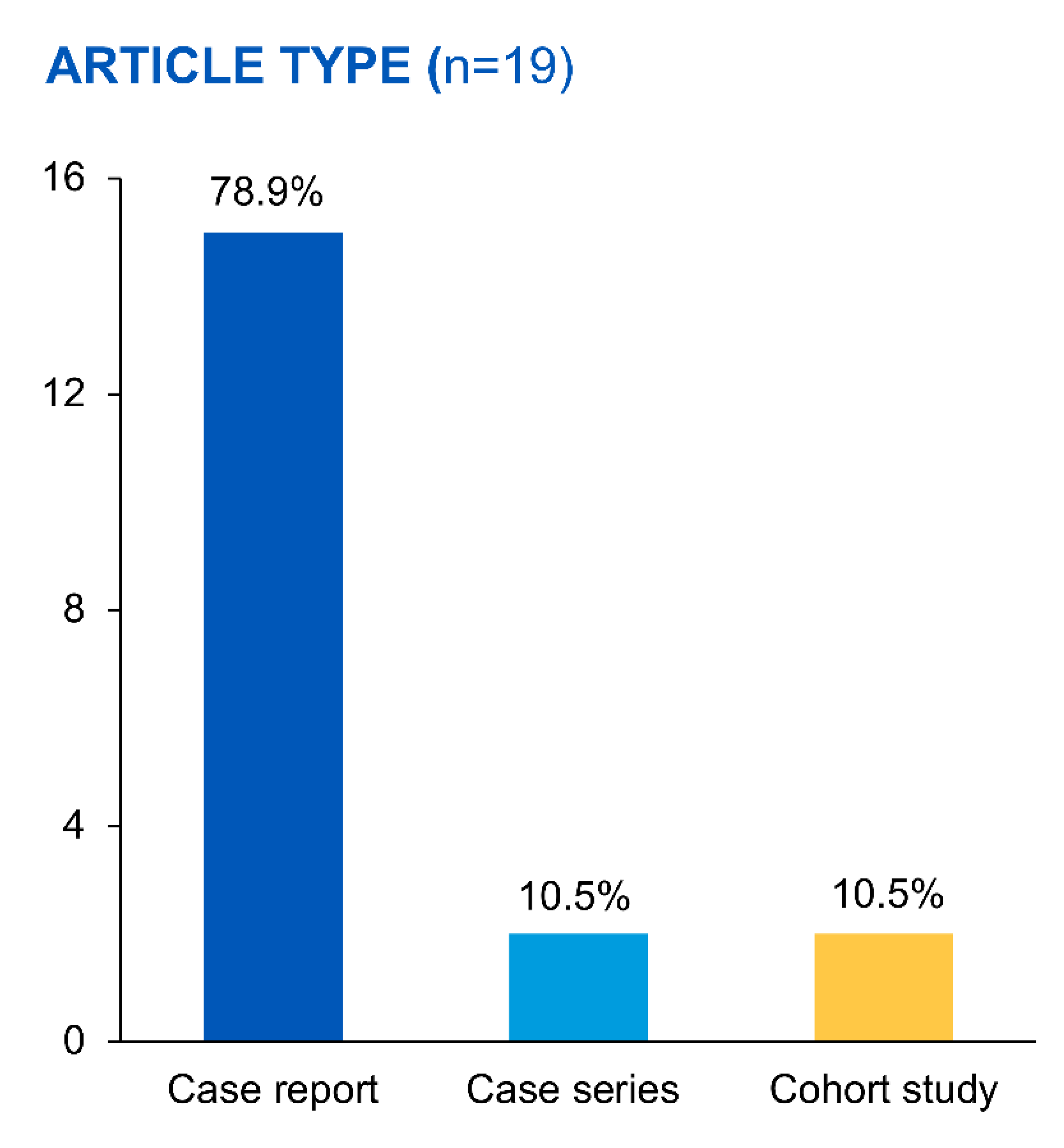
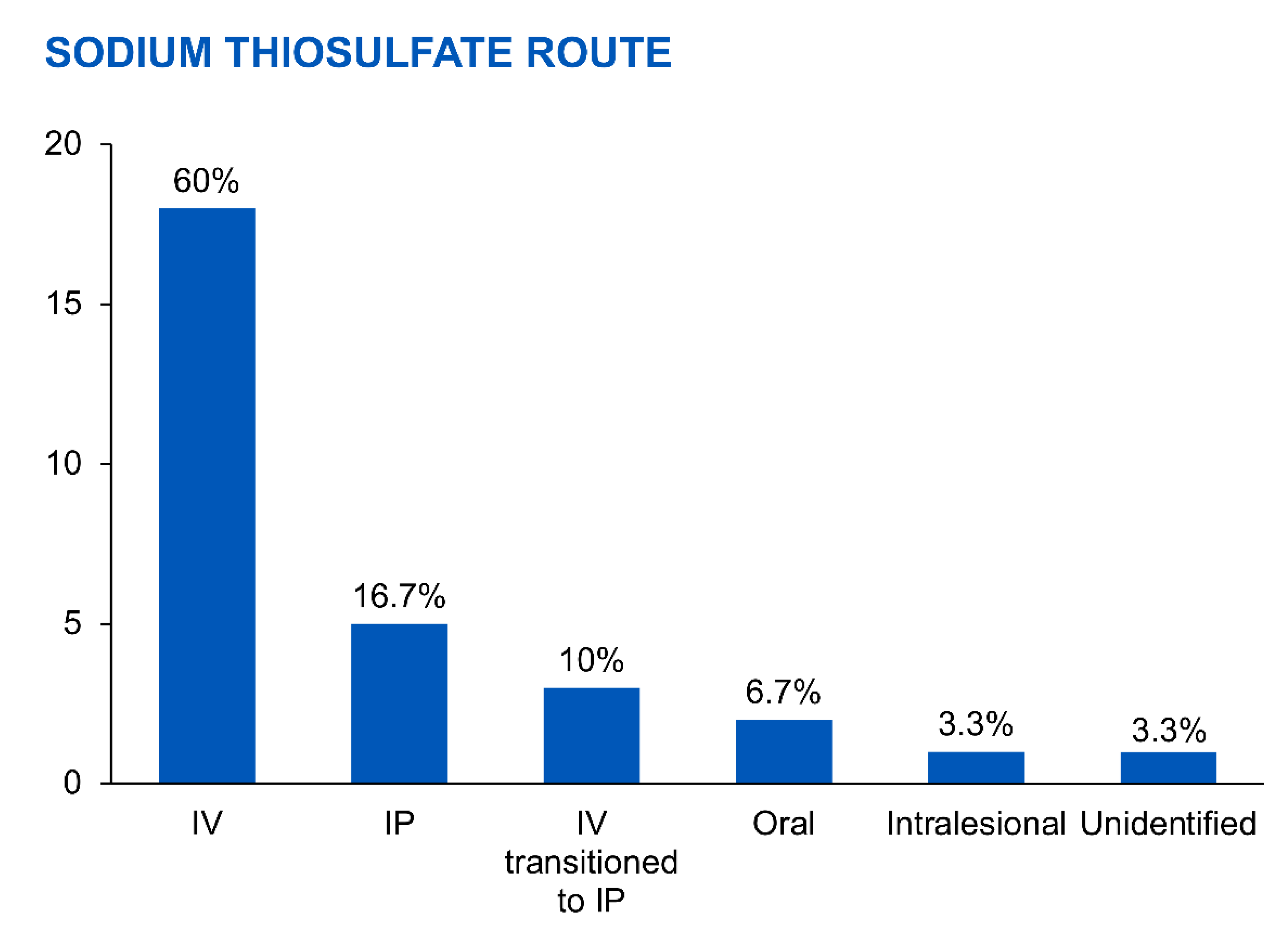
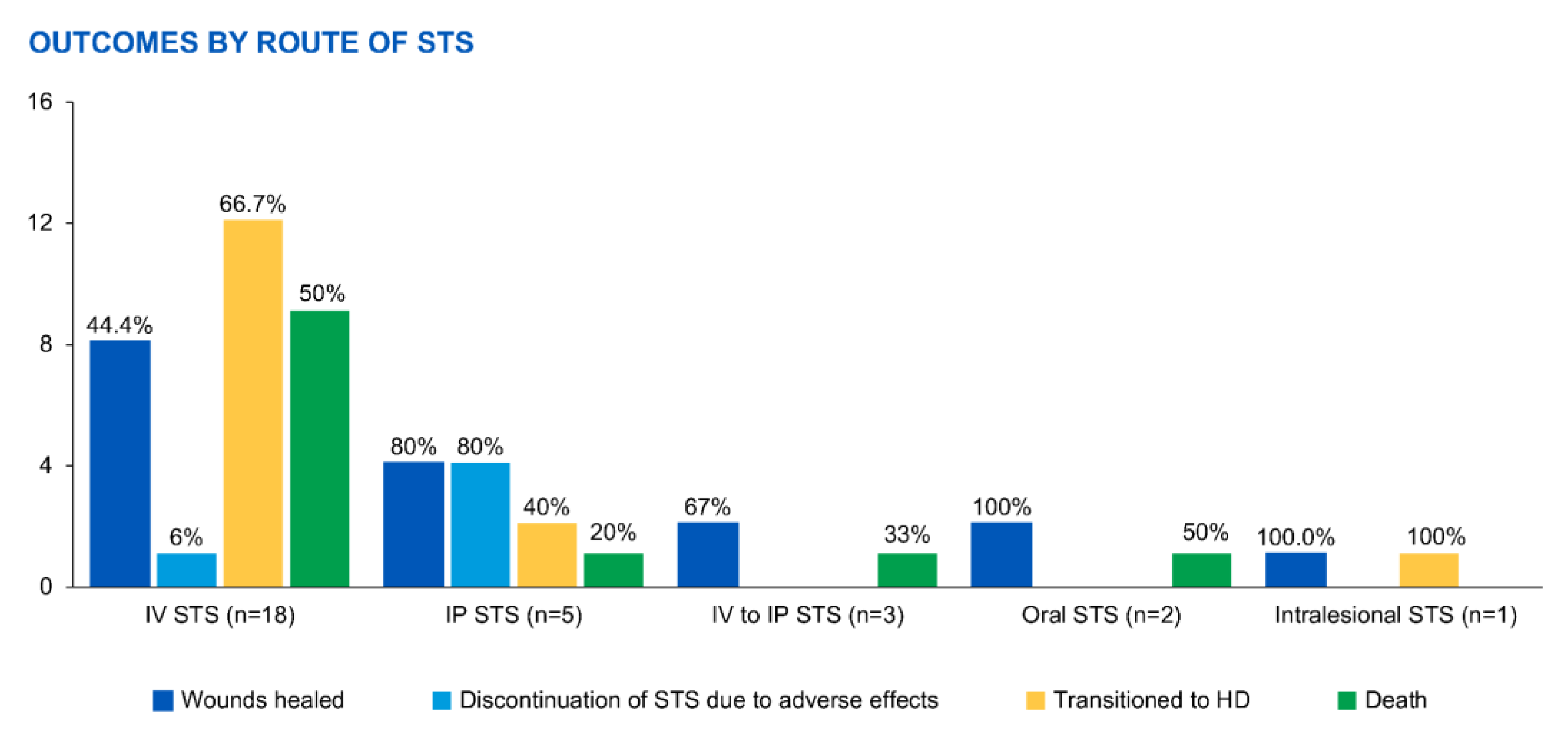
3. Results
| Author Name | Year | Type of Study | N | Location of Calciphylaxis Skin Lesions | Sodium Thiosulfate | Other Adjunctive Treatments | Dialysis Adjustment |
Outcomes (Description) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Dose | Route | Treatment Duration | ||||||||
| Cicone et al. [26] | 2004 | Case study | 1 | Bilateral calves and thighs | 25 g 3×/week | IV | 8 months (attempts at d/c earlier were met with resistance by family and patient) | Calcitriol and calcium acetate stopped, sevelamer binder, prednisone | None | Dramatic pain reduction at 2 weeks and no pain by 8 weeks, reduction in plaque size, improvement in bone scans |
| Danijela Mataic and Bahar Bastani [36] | 2009 | Case study | 1 | Proximal left arm and right lateral and left inner thigh | IV dose 25 g 3×/week; IP 25 g/2 L in long dwell every other day | IV initially; IP after recurrence at 25 g/2 L in long dwell every other day | 2 months IV before d/c due to intolerance; 3 months of IP | low-calcium (2.5 meq/L) dialysate, wound care, parenteral antibiotics | Low calcium dialysate | Wounds improved but then recurrence due to poor compliance; IP Na thiosulfate introduced at this point— lesions progressed, sepsis and death |
| Amin et al. [49] | 2010 | Case study | 1 | Bilateral first metatarsals | 25 g 3×/week | IV | Months | d/c calcium carbonate binder and vitamin d analogs, used noncalcium-based binders, HBO, dietary modification | Added mid-day exchange | Wound progressed and after 2 months, had to switch to HD |
| Finch et al. [48] | 2010 | Case study | 1 | Not listed | 5 g 3/week | IV | 6 months | Opioids for pain control | None | Complete resolution of wounds |
| New et al. [17] | 2011 | Observational retrospective cohort | 5 | Lower extremities | 25 g IV (3 pts); 12.5 g IV (2 pts) | IV (3 pts) IP (3 pts) | IV- 3 mo, 6 mo, 5 weeks; IP- 3 mo | HBO, cinacalcet, parathyroidectomy, pamidronate, d/c calcium and calcitriol, change phosphate binders | 3/5 patients eventually changed to HD after worsening wounds (2 pts) or 2 episodes of peritonitis (1 pt) | Resolution of wounds ×4; 1 died from sepsis Two patients who had resolution of wounds died much later from other causes (one due d/c dialysis due to functional decline; one due ischemic CCF) |
|
Sood et al. [49] | 2011 | Case series | 4 | Lower extremities, buttocks, abdomen | 25 g IV 3×/week | IV | 4–14 weeks | D/c warfarin if able, d/c calcium-based binders/vit d analogs, used sevelamer, cinacalcet, IV pamidronate, antibiotics, wound care, opioids, parathyroidectomy | 2 pts with increased intensity (what was done to increase is not described) | 2/4 with reduced wounds (1 with complete resolution); 3/4 eventually had to switch to HD; 2/4 pts died r/t sepsis by 1 year; ¼ with reduction in pain |
|
Dethloff, Steven B. [45] | 2012 | Case Study | 1 | Distal extremities | Initially 25 g, then decreased to 12.5 g due to nausea before transitioning to IP 25 g | IV initially but transitioned to IP due to intolerance of IV | 10 weeks | Increased protein intake, phosphorus restriction, binders changed to noncalcium, calcitriol discontinued, strict BP control, pain control with hydrocodone | None described | Completely healed by 12 weeks |
|
Gupta et al. [43] | 2012 | Case study | 1 | Medial calf (left) | 25 g/2 L dialysate | IP | 3 exchanges in a 12 h time frame | Calcitriol discontinued, wound care | Switched to CRRT after severe decompensation (not as part of calciphylaxis treatment plan) | Patient developed chemical peritonitis, decompensated rapidly and died days later |
| Mallett et al. [44] | 2012 | Case study | 1 | Distal left leg | 25 g every other day ×3 doses, then 12.5 g every other day (decreased due to nausea) | IP | 6 weeks | Binder changed to sevelamer, hyperbaric oxygen therapy, and wound care; aspirin; SLE was treated with mycophenolate, increase in prednisone, and hydroxychloroquine | No change | Healed lesion, biopsy 6 months later with no calciphylaxis or SLE; had successful pregnancy with post-partum SLE flare but no recurrence of calciphylaxis |
|
Anupkumar Shetty, Jeffrey Klein [50] | 2016 | Case report | 2 | Pt 1- L middle finger, L first toe, abdominal all Pt 2-R fingers | 1500 mg BID | Oral | 11 mo, 6 mo | Amputation, gabapentin, opioids | None | Healed; 1 patient died of SBO 14 months later (not calciphylaxis related) |
|
Zhang et al. [11] | 2016 | Cohort study—retrospective observational | 4 | Lower extremities, penis | 25 g 3×/week | IV | 2.8–5.1 months (3 m median) | Wound care/ debridement, opioids for pain, nutrition consult, surgical debridement, HBO | None | 75% mortality at 1 year due to sepsis (also the same patients who eventually had to transition to HD) |
|
Machavarapu et al. [51] | 2018 | Case Study | 1 | Esophagus | Not specified | IV | 2 months | PPI, supplemental protein shakes | No change initially, transitioned to iHD eventually due to infected PD catheter | Died 2 months after presentation due to suspected spontaneous coronary event |
|
Torres et al. [36] | 2018 | Case study /abstract | 1 | Penis | Not stated | IP | 2 weeks—stopped due to severe nausea | Low calcium dialysate | Low calcium dialysate | Significant reduction in pain and some wound healing |
| Bara Zhaili, Khalid Al-Talib [52] | 2019 | Case Study | 1 | Right calf | 4–5 mL once every 2 weeks | Intralesional | 9 weeks | Wound care, PO sevelamer, IV ceftazidime, collagenase ointment | None | Complete resolution of wounds; eventually transitioned to HD due to peritonitis, not due to calciphylaxis |
| Tangkham et al. [53] | 2019 | Case study | 1 | Bilateral thighs (R first, then left) | 12.5 mg 3×/week | IV | 3 months | IV ciprofloxacin, wound care, discontinuation of calcium-containing phosphate | No changes, continued CAPD 8 h per day | Refused surgical debridement and died 3 months after presentation due to sepsis |
|
Deng et al. [54] | 2020 | Case study | 1 | R shoulder and R fingers | 6 g per day | IV | 55 days | Parathyroidectomy, cinacalcet, sevelamer, antibiotics | 6 days per week CAPD, 1 day per week iHD added | Amputation of 1 finger, improvement in wounds after 2 months |
|
Di et al. [55] | 2020 | Case study | 1 | Neck, shoulders, upper extremities | 6.4 g/day | Not listed | 21 days | None listed | None listed | Diminished skin lesions |
| Janom K et al. [46] | 2021 | Case Study | 1 | Lower extremity | 12.5 g in 1 L of NS as a long day dwell | IP (initially IV but severe nausea necessitated change) | 3 months | Subtotal parathyroidectomy | None | Lesions healed after 6 months; mild decrease in kt/v; PD effluent cell counts monitored with no change noted |
|
Lu et al. [30] | 2022 | Case study | 1 | Fingers and toes | 3.2–6.4 g per day | IV | 6 months | Calcium stopped, wound care, low calcium dialysate, lanthanum for binder, PD adjustment per Kt/V protocol | Per kt/v protocol | Healed after 9 months |
| Author | Age | Sex | PD Duration/ Type of PD | Adequacy (kt/v) | Ethnicity/Race | Cause of Renal Failure | Comorbidities |
|---|---|---|---|---|---|---|---|
| Cicone et al. | 69 years | Female | 3 months (CAPD) | >2.1 | Caucasian | Hypertension and chronic hydronephrosis from renal calculi | Coronary artery disease, obesity, renal calculi, osteoarthritis, Graves’ disease, osteoporosis, hypertension |
| Danijela Mataic and Bahar Bastani | 26 years | Female | 4 years (CCPD) | n/a | Caucasian | Focal segmental glomerulosclerosis | n/a |
| Amin et al. | 17 years | Male | 3 years | n/a | African American | Wegner’s granulomatosis | n/a |
| Finch et al. | 85 years | Female | n/a (CCPD) | n/a | n/a | n/a | n/a |
| New et al. | |||||||
| #1 | 79 years | Female | 9 years (CAPD) | n/a | n/a | Unknown | Hypertension, ischemic heart disease peripheral vascular disease, dyslipidemia, depression |
| #2 | 67 years | Male | 7 months (CAPD) | n/a | n/a | Focal segmental glomerulosclerosis | Hypertension, ischemic heart disease dyslipidemia, obstructive sleep apnea, benign prostatic hyperplasia, gastroesophageal reflux disease |
| #3 | 75 years | Male | 7 months (CAPD) | n/a | n/a | Diabetes, obstructive | Diabetes, ischemic heart disease, dyslipidemia, cerebrovascular accident, gastroesophageal reflux disease, hypertension, gout |
| #4 | 74 years | Male | 3 years (CAPD) | n/a | n/a | Autosomal dominant polycystic kidney disease | Peripheral vascular disease, hypertension, gout, exsmoker |
| #5 | 28 years | Female | 27 months (CAPD) | n/a | n/a | Systemic Lupus Erythematosus | Autoimmune hemolytic anemia, epilepsy, hypertension |
| Sood et al. | |||||||
| #1 | 27 years | Female | 7 years | n/a | Caucasian | Reflux nephropathy | Peripheral vascular disease, congestive heart failure, hypertension |
| #2 | 53 years | Female | 6 months | n/a | Caucasian | Obstruction | Coronary artery disease, peripheral vascular disease, cerebrovascular accident, diabetes mellitus type 2 |
| #3 | 63 years | Female | 8 years | n/a | Caucasian | Myeloma kidney | None |
| #4 | 49 years | Female | 3 years | n/a | Not Caucasian (not defined further) | Diabetes mellitus, type 2 | Diabetes type 2, hypertension |
| Dethloff, Steven B. | 56 years | Female | 18 months (CCPD) | n/a | Asian American | Diabetes mellitus, type 2 | n/a |
| Gupta et al. | 82 years | Female | n/a | n/a | n/a | Lupus nephritis | Coronary artery disease, obstructive airway disease, Sjogren syndrome, obesity |
| Mallett et al. | 30 years | Female | 2 years (CAPD) | “Adequate, stable” | Caucasian | Class 4 lupus nephritis | Autoimmune hemolytic anemia, lupus anticoagulant antibody positivity without thrombosis, and seizure disorder |
| Anupkumar Shetty, Jeffrey Klein | |||||||
| #1 | 55 years | Female | 4 months | n/a | Latina | Diabetes | Diabetes, ovarian cancer with multiple abdominal surgeries |
| #2 | 51 years | Male | n/a | n/a | n/a | Failed kidney transplant (original cause not defined, but presumed diabetes as that is the only comorbidity listed) | Diabetes |
| Zhang et al. | |||||||
| #1 | 41 years | Female | 7 years | 2.12 | Black | Lupus | n/a |
| #2 | 34 years | Male | 3.4 years | 1.61 | White | Lupus | n/a |
| #3 | 59 years | Female | 4.1 years | 1.99 | Black | Unknown | n/a |
| #4 | 65 years | Female | 4.8 years | 2.06 | White | Diabetes | n/a |
| Machavarapu et al. | 57 years | Female | 17 months | n/a | n/a | Not specified | Diabetes, hypertension, STEMI with EF 20%, triple vessel coronary artery disease |
| Torres et al. | 63 years | Male | n/a | n/a | n/a | Not specified | Hypertension, diabetes type 2, peripheral vascular disease, poor medication compliance |
| Bara Zhaili, Khalid Al-Talib | 51 years | Male | 18 months | n/a | n/a | Diabetic nephropathy | Dilated nonischemic cardiomyopathy with diastolic dysfunction, uncontrollable hypertension, diabetic retinopathy |
| Tangkham et al. | 43 years | Male | 10 years (CAPD) | n/a | Asian | Not specified | Osteoporosis, secondary hyperparathyroidism status post subtotal parathyroidectomy, hypertension, dyslipidemia, ex-smoker, prior cannabis use |
| Deng et al. | 33 years | Male | 5 years (CAPD) | “Insufficient” | Chinese | Unknown | n/a |
| Di et al. | 32 years | Male | ~3 years (CAPD) | n/a | n/a | Not specified | Hypertension, hepatitis B |
| Janom K et al. | 80 years | Female | n/a | “Modest, unexplained decrease in kt/v was noted” | n/a | Not specified | n/a |
| Lu et al. | 40 years | Male | 7 years | 1.2 | Chinese | Unknown | Hypertension, secondary hyperparathyroidism status post total parathyroidectomy with partial forearm implant 6 months prior |
Risk of Bias Assessment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nigwekar, S.U.; Thadhani, R.; Brandenburg, V.M. Calciphylaxis. N. Engl. J. Med. 2018, 378, 1704–1714. [Google Scholar] [CrossRef]
- Gallo Marin, B.; Aghagoli, G.; Hu, S.L.; Massoud, C.M.; Robinson-Bostom, L. Calciphylaxis and Kidney Disease: A Review. Am. J. Kidney Dis. 2023, 81, 232–239. [Google Scholar] [CrossRef]
- Krisanapan, P.; Pattharanitima, P.; Thongprayoon, C.; Cheungpasitporn, W. Recent Advances in Understanding of Cardiovascular Diseases in Patients with Chronic Kidney Disease. J. Clin. Med. 2022, 11, 4653. [Google Scholar] [CrossRef]
- Disthabanchong, S.; Srisuwarn, P. Mechanisms of Vascular Calcification in Kidney Disease. Adv. Chronic. Kidney Dis. 2019, 26, 417–426. [Google Scholar] [CrossRef]
- Fine, A.; Fleming, S.; Leslie, W. Calciphylaxis presenting with calf pain and plaques in four continuous ambulatory peritoneal dialysis patients and in one predialysis patient. Am. J. Kidney Dis. 1995, 25, 498–502. [Google Scholar] [CrossRef]
- Thongprayoon, C.; Cheungpasitporn, W.; Bruminhent, J. Aggressive calciphylaxis in end-stage renal disease after a failed kidney allograft. Indian J. Dermatol. Venereol. Leprol. 2015, 81, 50. [Google Scholar] [CrossRef]
- Nigwekar, S.U.; Kroshinsky, D.; Nazarian, R.M.; Goverman, J.; Malhotra, R.; Jackson, V.A.; Kamdar, M.M.; Steele, D.J.; Thadhani, R.I. Calciphylaxis: Risk factors, diagnosis, and treatment. Am. J. Kidney Dis. 2015, 66, 133–146. [Google Scholar] [CrossRef] [PubMed]
- Rogers, N.M.; Teubner, D.; Coates, P. VASCULAR CALCIFICATION IN PATIENTS WITH KIDNEY DISEASE: Calcific uremic arteriolopathy: Advances in pathogenesis and treatment. Semin. Dial. 2007, 20, 150–157. [Google Scholar] [CrossRef] [PubMed]
- Fine, A.; Zacharias, J. Calciphylaxis is usually non-ulcerating: Risk factors, outcome and therapy. Kidney Int. 2002, 61, 2210–2217. [Google Scholar] [CrossRef]
- Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Erickson, S.B. Calcium-phosphate product and its impact on mortality in hospitalized patients. Nephrology 2020, 25, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Corapi, K.M.; Luongo, M.; Thadhani, R.; Nigwekar, S.U. Calciphylaxis in peritoneal dialysis patients: A single center cohort study. Int. J. Nephrol. Renovasc. Dis. 2016, 9, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Sprague, S.M. Painful skin ulcers in a hemodialysis patient. Clin. J. Am. Soc. Nephrol. 2014, 9, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Fine, A.; Fontaine, B. Calciphylaxis: The beginning of the end? Perit. Dial. Int. 2008, 28, 268–270. [Google Scholar] [CrossRef]
- Nigwekar, S.U.; Zhao, S.; Wenger, J.; Hymes, J.L.; Maddux, F.W.; Thadhani, R.I.; Chan, K.E. A nationally representative study of calcific uremic arteriolopathy risk factors. J. Am. Soc. Nephrol. 2016, 27, 3421–3429. [Google Scholar] [CrossRef]
- Angelis, M.; Wong, L.L.; Myers, S.A.; Wong, L.M. Calciphylaxis in patients on hemodialysis: A prevalence study. Surgery 1997, 122, 1083–1089. [Google Scholar] [CrossRef]
- Nigwekar, S.U.; Solid, C.A.; Ankers, E.; Malhotra, R.; Eggert, W.; Turchin, A.; Thadhani, R.I.; Herzog, C.A. Quantifying a rare disease in administrative data: The example of calciphylaxis. J. Gen. Intern. Med. 2014, 29 (Suppl. S3), S724–S731. [Google Scholar] [CrossRef] [PubMed]
- New, N.; Mohandas, J.; John, G.T.; Ratanjee, S.; Healy, H.; Francis, L.; Ranganathan, D. Calcific uremic arteriolopathy in peritoneal dialysis populations. Int. J. Nephrol. 2011, 2011, 982854. [Google Scholar] [CrossRef] [PubMed]
- Brandenburg, V.M.; Kramann, R.; Rothe, H.; Kaesler, N.; Korbiel, J.; Specht, P.; Schmitz, S.; Krüger, T.; Floege, J.; Ketteler, M. Calcific uraemic arteriolopathy (calciphylaxis): Data from a large nationwide registry. Nephrol. Dial. Transplant. 2016, 32, 126–132. [Google Scholar] [CrossRef]
- Brandenburg, V.M.; Cozzolino, M.; Ketteler, M. Calciphylaxis: A still unmet challenge. J. Nephrol. 2011, 24, 142–148. [Google Scholar] [CrossRef]
- Harris, C.; Kiaii, M.; Lau, W.; Farah, M. Multi-intervention management of calcific uremic arteriolopathy in 24 patients. Clin. Kidney J. 2018, 11, 704–709. [Google Scholar] [CrossRef]
- Weenig, R.H.; Sewell, L.D.; Davis, M.D.; McCarthy, J.T.; Pittelkow, M.R. Calciphylaxis: Natural history, risk factor analysis, and outcome. J. Am. Acad. Dermatol. 2007, 56, 569–579. [Google Scholar] [CrossRef] [PubMed]
- Monardo, P.; Lacquaniti, A.; Campo, S.; Bucca, M.; Casuscelli di Tocco, T.; Rovito, S.; Ragusa, A.; Santoro, A. Updates on hemodialysis techniques with a common denominator: The personalization of the dialytic therapy. Semin. Dial. 2021, 34, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Savica, V.; Calò, L.A.; Monardo, P.; Santoro, D.; Mallamace, A.; Muraca, U.; Bellinghieri, G. Salivary phosphorus and phosphate content of beverages: Implications for the treatment of uremic hyperphosphatemia. J. Ren. Nutr. 2009, 19, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Udomkarnjananun, S.; Kongnatthasate, K.; Praditpornsilpa, K.; Eiam-Ong, S.; Jaber, B.L.; Susantitaphong, P. Treatment of Calciphylaxis in CKD: A Systematic Review and Meta-analysis. Kidney Int. Rep. 2019, 4, 231–244. [Google Scholar] [CrossRef]
- McCarthy, J.T.; El-Azhary, R.A.; Patzelt, M.T.; Weaver, A.L.; Albright, R.C.; Bridges, A.D.; Claus, P.L.; Davis, M.D.; Dillon, J.J.; El-Zoghby, Z.M.; et al. Survival, Risk Factors, and Effect of Treatment in 101 Patients with Calciphylaxis. Mayo Clin. Proc. 2016, 91, 1384–1394. [Google Scholar] [CrossRef]
- Cicone, J.S.; Petronis, J.B.; Embert, C.D.; Spector, D.A. Successful treatment of calciphylaxis with intravenous sodium thiosulfate. Am. J. Kidney Dis. 2004, 43, 1104–1108. [Google Scholar] [CrossRef]
- Araya, C.E.; Fennell, R.S.; Neiberger, R.E.; Dharnidharka, V.R. Sodium thiosulfate treatment for calcific uremic arteriolopathy in children and young adults. Clin. J. Am. Soc. Nephrol. 2006, 1, 1161–1166. [Google Scholar] [CrossRef]
- Ackermann, F.; Levy, A.; Daugas, E.; Schartz, N.; Riaux, A.; Derancourt, C.; Urena, P.; Lebbé, C. Sodium thiosulfate as first-line treatment for calciphylaxis. Arch. Dermatol. 2007, 143, 1331–1344. [Google Scholar] [CrossRef]
- Schlieper, G.; Brandenburg, V.; Ketteler, M.; Floege, J. Sodium thiosulfate in the treatment of calcific uremic arteriolopathy. Nat. Rev. Nephrol. 2009, 5, 539–543. [Google Scholar] [CrossRef]
- Lu, Y.; Shen, L.; Zhou, L.; Xu, D. Success of small-dose fractionated sodium thiosulfate in the treatment of calciphylaxis in a peritoneal dialysis patient. BMC Nephrol. 2022, 23, 4. [Google Scholar] [CrossRef]
- An, J.; Devaney, B.; Ooi, K.Y.; Ford, S.; Frawley, G.; Menahem, S. Hyperbaric oxygen in the treatment of calciphylaxis: A case series and literature review. Nephrology 2015, 20, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Wen, W.; Portales-Castillo, I.; Seethapathy, R.; Krinsky, S.; Kroshinsky, D.; Kalim, S.; Goverman, J.; Nazarian, R.M.; Chitalia, V.; Malhotra, R.; et al. Intravenous sodium thiosulphate for vascular calcification of hemodialysis patients-a systematic review and meta-analysis. Nephrol. Dial. Transpl. 2023, 38, 733–745. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.P.; Derendorf, H.; Ross, E.A. Simulation-Based Sodium Thiosulfate Dosing Strategies for the Treatment of Calciphylaxis. Clin. J. Am. Soc. Nephrol. 2011, 6, 1155–1159. [Google Scholar] [CrossRef]
- Generali, J.A.; Cada, D.J. Sodium Thiosulfate: Calciphylaxis. Hosp. Pharm. 2015, 50, 975–977. [Google Scholar] [CrossRef] [PubMed]
- Galassi, A.; Perna, F.; De Nicola, E.; Moneghini, L.; Sganzaroli, A.B.; Cozzolino, M. Calciphylaxis in a dialysis patient treated by intralesional and systemic sodium thiosulphate on top of multifactorial intervention. Clin. Kidney J. 2018, 12, 546–549. [Google Scholar] [CrossRef]
- Mataic, D.; Bastani, B. Intraperitoneal sodium thiosulfate for the treatment of calciphylaxis. Ren. Fail. 2006, 28, 361–363. [Google Scholar] [CrossRef] [PubMed]
- Teh, Y.K.; Renaud, C.J. Clinical experience with intraperitoneal sodium thiosulphate for calciphylaxis in peritoneal dialysis: A case series. Perit. Dial. Int. 2023, 08968608231163669. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Reddy, S.N.; Garcha, A.S.; Vantipalli, P.; Patel, S.S.; Ur Rahman, E.; Adapa, S. Successful Treatment of Calciphylaxis in a Young Female With End-Stage Renal Disease on Peritoneal Dialysis With Parathyroidectomy, Intensification of Dialysis, and Sodium Thiosulphate-A Case Report and Literature Review. J. Investig. Med. High Impact Case Rep. 2021, 9, 23247096211060580. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Munn, Z.; Barker, T.H.; Moola, S.; Tufanaru, C.; Stern, C.; McArthur, A.; Stephenson, M.; Aromataris, E. Methodological quality of case series studies: An introduction to the JBI critical appraisal tool. JBI Evid. Synth. 2020, 18, 2127–2133. [Google Scholar] [CrossRef]
- National Institutes of Health. National Heart, Lung, and Blood Institute. In Study Quality Assessment Tool for Case Series Studies. Bethesda.; 2018. Available online: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools (accessed on 10 June 2023).
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.R.; Sangha, H.; Khanna, R. Chemical peritonitis after intraperitoneal sodium thiosulfate. Perit. Dial. Int. 2012, 32, 220–222. [Google Scholar] [CrossRef]
- Mallett, A.; John, G.; Ranganathan, D.; Kark, A.; Berquier, I.; Casey, J.; Healy, H.; Francis, L. Sustained remission of systemic lupus erythematosus related calciphylaxis. Lupus 2012, 21, 441–444. [Google Scholar] [CrossRef] [PubMed]
- Dethloff, S.B. Calcific uremic arteriolopathy: Treatment with intraperitoneal sodium thiosulfate in a patient on peritoneal dialysis. Nephrol. Nurs. J. 2012, 39, 323–325. [Google Scholar]
- Janom, K.; Shaikhouni, S.; Perlman, R.; Swartz, R.D. Revisiting Route of Therapy for Calciphylaxis in Peritoneal Dialysis. In Proceedings of the Kidney Week Annual Meeting, Virtual, 4–7 November 2021. [Google Scholar]
- Sood, A.R.; Wazny, L.D.; Raymond, C.B.; Leung, K.; Komenda, P.; Reslerova, M.; Verrelli, M.; Rigatto, C.; Sood, M.M. Sodium thiosulfate-based treatment in calcific uremic arteriolopathy: A consecutive case series. Clin. Nephrol. 2011, 75, 8–15. [Google Scholar]
- Finch, S.; Aspden, I.; Johnson, L.; Bashir, K. The Use of Intravenous Sodium Thiosulfate for the Treatment of Calciphylaxis in an Elderly Peritoneal Dialyisis Patient. J. Ren. Nutr. 2010, 20, 137. [Google Scholar] [CrossRef]
- Amin, N.; Gonzalez, E.; Lieber, M.; Salusky, I.B.; Zaritsky, J.J. Successful treatment of calcific uremic arteriolopathy in a pediatric dialysis patient. Pediatr. Nephrol. 2010, 25, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Shetty, A.; Klein, J. Treatment of Calciphylaxis: A Case for Oral Sodium Thiosulfate. Adv. Perit. Dial. 2016, 32, 51–55. [Google Scholar] [PubMed]
- Machavarapu, A.; Brown, T.A.; Nwakoby, I.E. Rare Case of Hematemesis: Calciphylaxis of the Esophagus. Clin. Gastroenterol. Hepatol. 2018, 16, A35. [Google Scholar] [CrossRef]
- Zuhaili, B.; Al-Talib, K. Successful Treatment of Single Infected Calciphylaxis Lesion With Intralesional Injection of Sodium Thiosulfate at High Concentration. Wounds A Compend. Clin. Res. Pract. 2019, 31, E54–E57. [Google Scholar]
- Tangkham, R.; Sangmala, S.; Aiempanakit, K.; Chiratikarnwong, K.; Auepemkiate, S. Calciphylaxis mimicking ecthyma gangrenosum. IDCases 2019, 18, e00594. [Google Scholar] [CrossRef] [PubMed]
- Deng, Y.; Shu, Y.; Gong, R. Calciphylaxis in patient with peritoneal dialysis: A case report. Cogent Med. 2020, 7, 1736250. [Google Scholar] [CrossRef]
- Di, J.; Liu, Y.; Wang, D.; Yang, M. A Case of Early Calciphylaxis Diagnosed by Bone Scan. Case Rep. Med. 2020, 2020, 9526836. [Google Scholar] [CrossRef]
- Vedvyas, C.; Winterfield, L.S.; Vleugels, R.A. Calciphylaxis: A systematic review of existing and emerging therapies. J. Am. Acad. Dermatol. 2012, 67, e253–e260. [Google Scholar] [CrossRef]
- Hayden, M.R.; Goldsmith, D.; Sowers, J.R.; Khanna, R. Calciphylaxis: Calcific uremic arteriolopathy and the emerging role of sodium thiosulfate. Int. Urol. Nephrol. 2008, 40, 443–451. [Google Scholar] [CrossRef] [PubMed]
- Sherman, C. Chemical peritonitis after intraperitoneal sodium thiosulfate. Perit. Dial. Int. 2013, 33, 104. [Google Scholar] [CrossRef]
- Raymond, C.B.; Wazny, L.D. Sodium thiosulfate, bisphosphonates, and cinacalcet for treatment of calciphylaxis. Am. J. Health Syst. Pharm. 2008, 65, 1419–1429. [Google Scholar] [CrossRef]
- Lal, G.; Nowell, A.G.; Liao, J.; Sugg, S.L.; Weigel, R.J.; Howe, J.R. Determinants of survival in patients with calciphylaxis: A multivariate analysis. Surgery 2009, 146, 1028–1034. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD-MBD Update Work Group. KDIGO 2017 Clinical Practice Guideline Update for the Diagnosis, Evaluation, Prevention, and Treatment of Chronic Kidney Disease-Mineral and Bone Disorder (CKD-MBD). Kidney Int. Suppl. 2017, 7, 1–59. [Google Scholar] [CrossRef]
- Fernández-Martín, J.L.; Martínez-Camblor, P.; Dionisi, M.P.; Floege, J.; Ketteler, M.; London, G.; Locatelli, F.; Gorriz, J.L.; Rutkowski, B.; Ferreira, A.; et al. Improvement of mineral and bone metabolism markers is associated with better survival in haemodialysis patients: The COSMOS study. Nephrol. Dial. Transplant. 2015, 30, 1542–1551. [Google Scholar] [CrossRef]
- Farese, S.; Stauffer, E.; Kalicki, R.; Hildebrandt, T.; Frey, B.M.; Frey, F.J.; Uehlinger, D.E.; Pasch, A. Sodium thiosulfate pharmacokinetics in hemodialysis patients and healthy volunteers. Clin. J. Am. Soc. Nephrol. 2011, 6, 1447–1455. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gossett, C.; Suppadungsuk, S.; Krisanapan, P.; Tangpanithandee, S.; Thongprayoon, C.; Mao, M.A.; Cheungpasitporn, W. Sodium Thiosulfate for Calciphylaxis Treatment in Patients on Peritoneal Dialysis: A Systematic Review. Medicina 2023, 59, 1306. https://doi.org/10.3390/medicina59071306
Gossett C, Suppadungsuk S, Krisanapan P, Tangpanithandee S, Thongprayoon C, Mao MA, Cheungpasitporn W. Sodium Thiosulfate for Calciphylaxis Treatment in Patients on Peritoneal Dialysis: A Systematic Review. Medicina. 2023; 59(7):1306. https://doi.org/10.3390/medicina59071306
Chicago/Turabian StyleGossett, Christy, Supawadee Suppadungsuk, Pajaree Krisanapan, Supawit Tangpanithandee, Charat Thongprayoon, Michael A. Mao, and Wisit Cheungpasitporn. 2023. "Sodium Thiosulfate for Calciphylaxis Treatment in Patients on Peritoneal Dialysis: A Systematic Review" Medicina 59, no. 7: 1306. https://doi.org/10.3390/medicina59071306
APA StyleGossett, C., Suppadungsuk, S., Krisanapan, P., Tangpanithandee, S., Thongprayoon, C., Mao, M. A., & Cheungpasitporn, W. (2023). Sodium Thiosulfate for Calciphylaxis Treatment in Patients on Peritoneal Dialysis: A Systematic Review. Medicina, 59(7), 1306. https://doi.org/10.3390/medicina59071306









