Knowledge of Dental Trauma and Orthodontic Management of Traumatized Teeth by a Group of Lithuanian Orthodontists
Abstract
1. Introduction
2. Materials and Methods
- The first demographic part of the questionnaire consisted of 3 questions to examine the academic and professional profile of the respondent (work experience, and workplace).
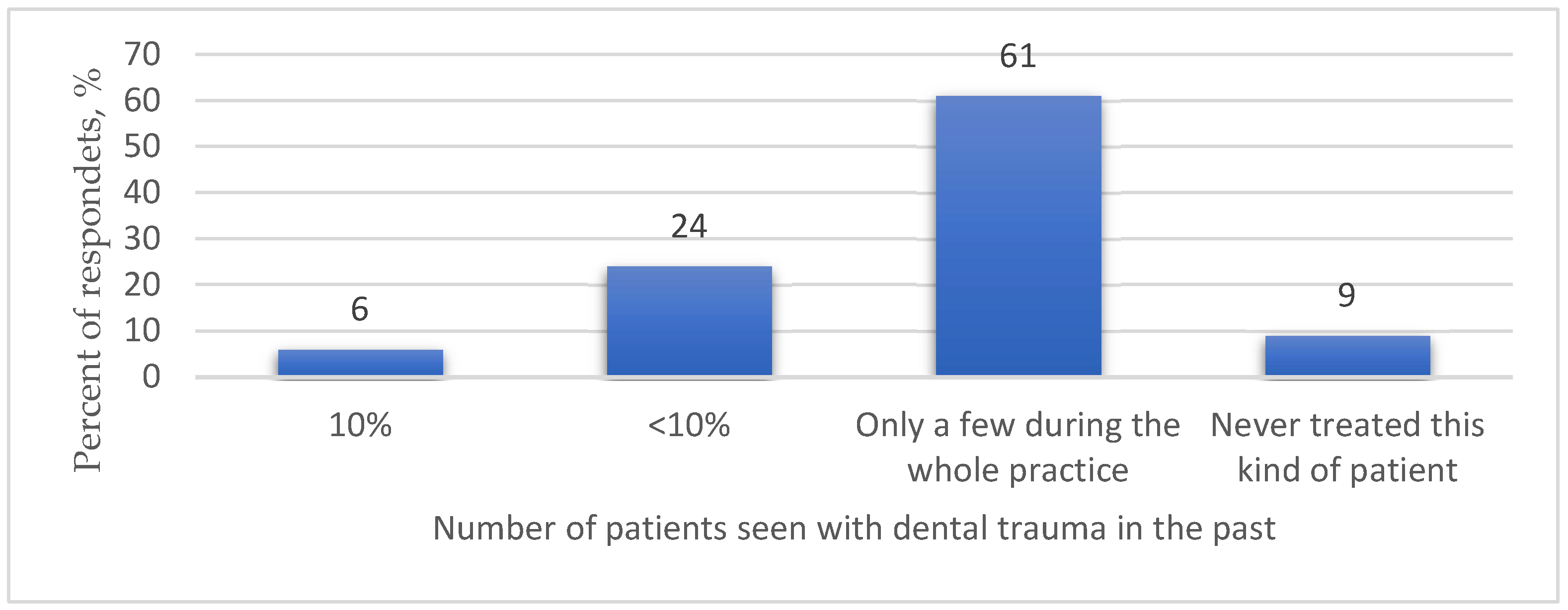
- The second part (3 questions) aimed to find out about the participants’ personal experience with patients who had experienced dental trauma.
- The third part presented 5 specific questions about dental trauma (clinical symptoms, the most common age of patients with dental trauma, and the action required immediately after the injury).
- The fourth part consisted of 15 questions regarding the orthodontic management tactics for patients with a history of dental trauma (when the treatment can be started in the case of a certain trauma; complications to be expected). The last question was asked to address the reasons why respondents were unsure of when to start orthodontic treatment after dental trauma.
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Magno, M.B.; Nadelman, P.; de França Leite, K.L.; Ferreira, D.M.; Pithon, M.M.; Maia, L.C. Associations and risk factors for dental trauma: A systematic review of systematic reviews. Community Dent. Oral Epidemiol. 2020, 48, 447–463. [Google Scholar] [CrossRef]
- Zaleckiene, V.; Peciuliene, V.; Brukiene, V.; Drukteinis, S. Traumatic dental injuries: Etiology, prevalence and possible outcomes. Stomatologija 2014, 16, 8. [Google Scholar]
- Kindelan, S.A.; Day, P.F.; Kindelan, J.D.; Spencer, J.R.; Duggal, M.S. Dental trauma: An overview of its influence on the management of orthodontic treatment. Part 1. J. Orthod. 2008, 35, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Owtad, P.; Shastry, S.; Papademetriou, M.; Park, J. Management Guidelines for Traumatically Injured Teeth during Orthodontic Treatment. J. Clin. Pediatr. Dent. 2015, 39, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Van Gorp, G.; Bormans, N.; Vanham, I.; Willems, G.; Declerck, D. Knowledge of orthodontic treatment approach of traumatized teeth by a group of Belgian general dentists, pediatric dentists, and orthodontists. Dent. Traumatol. 2019, 35, 233–240. [Google Scholar] [CrossRef] [PubMed]
- Sandler, C.; Al-Musfir, T.; Barry, S.; Duggal, M.S.; Kindelan, S.; Kindelan, J.; Littlewood, S.; Nazzal, H. Guidelines for the orthodontic management of the traumatised tooth. J. Orthod. 2021, 48, 74–81. [Google Scholar] [CrossRef]
- Sandler, C.; Barry, S.; Littlewood, S.; Al-Musfir, T.; Nazzal, H. Orthodontic management of traumatized teeth: A national survey of UK orthodontists. Dent. Traumatol. 2019, 35, 241–250. [Google Scholar] [CrossRef]
- Bauss, O.; Rohling, J.; Schwestka-Polly, R. Prevalence of traumatic injuries to the permanent incisors in candidates for orthodontic treatment. Dent. Traumatol. 2004, 20, 61–66. [Google Scholar] [CrossRef]
- Lin, S.; Pilosof, N.; Karawani, M.; Wigler, R.; Kaufman, A.; Teich, S. Occurrence and timing of complications following traumatic dental injuries: A retrospective study in a dental trauma department. J. Clin. Exp. Dent. 2016, 8, e429–e436. [Google Scholar] [CrossRef]
- de Andrade Veras, S.R.; Bem, J.S.P.; de Almeida, E.C.B.; Dos Santos Accioly Lins, C.C. Dental splints: Types and time of immobilization post tooth avulsion. J. Istanb. Univ. Fac. Dent. 2017, 51, S69–S75. [Google Scholar]
- Abbott, P. Prevention and management of external inflammatory resorption following trauma to teeth. Aust. Dent. J. 2016, 61, 82–94. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, R.S.; Gutmann, J.L. Endodontic-orthodontic relationships: A review of integrated treatment planning challenges. Int. Endod. J. 1999, 32, 343–360. [Google Scholar] [CrossRef]
- Chaniotis, A.; Chanioti, A. Long-term Complications of Previously Successful Regenerative Endodontic Procedures after Orthodontic Movement: A Report of 3 Different Complications after 4, 8, and 11 Years. J. Endod. 2022, 48, 951–960. [Google Scholar] [CrossRef]
- Tondelli, P.M.; de Mendonça, M.R.; Cuoghi, O.A.; Pereira, A.L.P.; Busato, M.C.A. Knowledge on dental trauma and orthodontic tooth movement held by a group of orthodontists. Braz. Oral Res. 2010, 24, 76–82. [Google Scholar] [CrossRef]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O’Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef]
- Sönmez, H.; Tunç, E.Ş.; Dalcı, Ö.N.; Şaroglu, I. Orthodontic extrusion of a traumatically intruded permanent incisor: A case report with a 5-year follow up. Dent. Traumatol. 2008, 24, 691–694. [Google Scholar] [CrossRef]
- Elfrink, M.E.C.; Heijdra, J.S.C.; Krikken, J.B.; Kouwenberg-Bruring, W.H.; Kouwenberg, H.; Weerheijm, K.L.; Veerkamp, J.S.J. Regenerative endodontic therapy: A follow-up of 47 anterior traumatised teeth. Eur. Arch. Paediatr. Dent. 2021, 22, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Feller, L.; Khammissa, R.A.G.; Schechter, I.; Thomadakis, G.; Fourie, J.; Lemmer, J. Biological Events in Periodontal Ligament and Alveolar Bone Associated with Application of Orthodontic Forces. Sci. World J. 2015, 2015, 876509. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.; Mack, G.; Djemal, S. Management of acute traumatic dental injuries in the orthodontic patient. Br. Dent. J. 2022, 232, 695–700. [Google Scholar] [CrossRef]
- Kallel, I.; Douki, N.; Amaidi, S.; Ben Amor, F. The Incidence of Complications of Dental Trauma and Associated Factors: A Retrospective Study. Int. J. Dent. 2020, 2020, 2968174. [Google Scholar] [CrossRef] [PubMed]

| Do You Ask Patients about Past Dental Trauma When Collecting a Medical History? * | In Total | |
|---|---|---|
| n | % | |
| I always ask the patient if he had a dental trauma in the past before the orthodontic treatment | 27 | 50 |
| If you notice signs of a previous dental injury, complications | 29 | 53.7 |
| If you notice increased horizontal overjet | 3 | 5.6 |
| The patient completes a special questionnaire before treatment, which also includes questions about dental injuries | 24 | 44.4 |
| Questions about Dental Trauma (Correct Answer) | Total Number of Correct Answers of Respondents | |
|---|---|---|
| n | % | |
| A displacement of the tooth out of its socket in an incisal/axial direction when there’s no alveolar bone, is classified as: (extrusion) | 32 | 59.3 |
| An injury to the tooth supporting structures without increasing tooth mobility or displacement but with significant sensibility to the percurssion, is classified as: (concussion) | 50 | 92.6 |
| Which device would you choose during the period of acute dental trauma (the patient arrived immediately after the injury, changes in the position of the tooth, damage to the periodontal ligament)? (Segmental bracket-system) | 22 | 40.7 |
| At what age do dental injuries occur the most? (7–14 years) | 32 | 59.3 |
| What recovery method would you choose for a tooth that has been submerged in the alveolus during an injury? (Surgical extrusion and immobilization or orthodontic extrusion immediately after injury) | 36 | 66.7 |
| Questions about Orthodontic Management of Traumatized Teeth (Correct Answer) | Total Number of Correct Answers of Respondents | |
|---|---|---|
| n | % | |
| In your opinion, which orthodontic movement is the least harmful to teeth who have suffered an injury? (Extrusion) | 21 | 38.9 |
| How long is it estimated to wait prior to orthodontic treatment after a crown fracture? (3 months) | 20 | 37 |
| How long is it estimated to wait prior to orthodontic treatment after a crown-root fracture? (3 months) | 12 | 22.2 |
| How long is it estimated to wait prior to orthodontic treatment after a minor damage to the periodontum? (3–6 months) | 35 | 64.8 |
| How long is it estimated to wait prior to orthodontic treatment after a severe damage to the periodontum? (6 months) | 19 | 35.2 |
| How long is it estimated to wait prior to orthodontic treatment for a tooth requiring endodontic treatment due to trauma? (12 months) | 4 | 7.4 |
| How long is it estimated to wait prior to orthodontic treatment for a tooth requiring regenerative endodontic treatment due to trauma? (12 months) | 11 | 20.4 |
| Do you take X-rays regularly (every 3 months) during orthodontic treatment of traumatized teeth? (Yes) | 25 | 46.3 |
| In your opinion, can a tooth that has suffered a root fracture in the past be subjected to normal orthodontic forces? (No) | 35 | 64.8 |
| In your opinion, can an injured tooth experience greater (compared to intact teeth) root resorption due to orthodontic forces? (Yes) | 52 | 96.3 |
| Do you think there is a possibility that other teeth have been injured during the trauma, but the consequences of the trauma are not visible until orthodontic treatment is initiated? (Yes) | 48 | 88.9 |
| How would you react if you notice a change in the color of a patient’s tooth during orthodontic treatment? (I would eliminate the action of orthodontic forces directed towards the damaged tooth until the cause of such changes is resolved) | 47 | 87 |
| How long is it estimated to wait prior to orthodontic treatment for a tooth with signs of inflammatory resorption? (When complete healing and integrity of periodontal ligament are observed and regular (every 3 months) X-ray examination is taken for one year) | 51 | 94.4 |
| Do you think that rational orthodontic forces promote bone repair processes? (Yes) | 42 | 77.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stučinskaitė, S.; Laugalė, P.; Grinkevičienė, D.; Vėberienė, R.; Smailienė, D. Knowledge of Dental Trauma and Orthodontic Management of Traumatized Teeth by a Group of Lithuanian Orthodontists. Medicina 2023, 59, 1289. https://doi.org/10.3390/medicina59071289
Stučinskaitė S, Laugalė P, Grinkevičienė D, Vėberienė R, Smailienė D. Knowledge of Dental Trauma and Orthodontic Management of Traumatized Teeth by a Group of Lithuanian Orthodontists. Medicina. 2023; 59(7):1289. https://doi.org/10.3390/medicina59071289
Chicago/Turabian StyleStučinskaitė, Simona, Paulina Laugalė, Dominyka Grinkevičienė, Rita Vėberienė, and Dalia Smailienė. 2023. "Knowledge of Dental Trauma and Orthodontic Management of Traumatized Teeth by a Group of Lithuanian Orthodontists" Medicina 59, no. 7: 1289. https://doi.org/10.3390/medicina59071289
APA StyleStučinskaitė, S., Laugalė, P., Grinkevičienė, D., Vėberienė, R., & Smailienė, D. (2023). Knowledge of Dental Trauma and Orthodontic Management of Traumatized Teeth by a Group of Lithuanian Orthodontists. Medicina, 59(7), 1289. https://doi.org/10.3390/medicina59071289




