The Survival Outcomes of Patients Requiring Prolonged Mechanical Ventilation
Abstract
1. Introduction
2. Methods
2.1. Participants
2.2. Data Collection
2.3. Outcomes Measure
2.4. Statistical Analysis
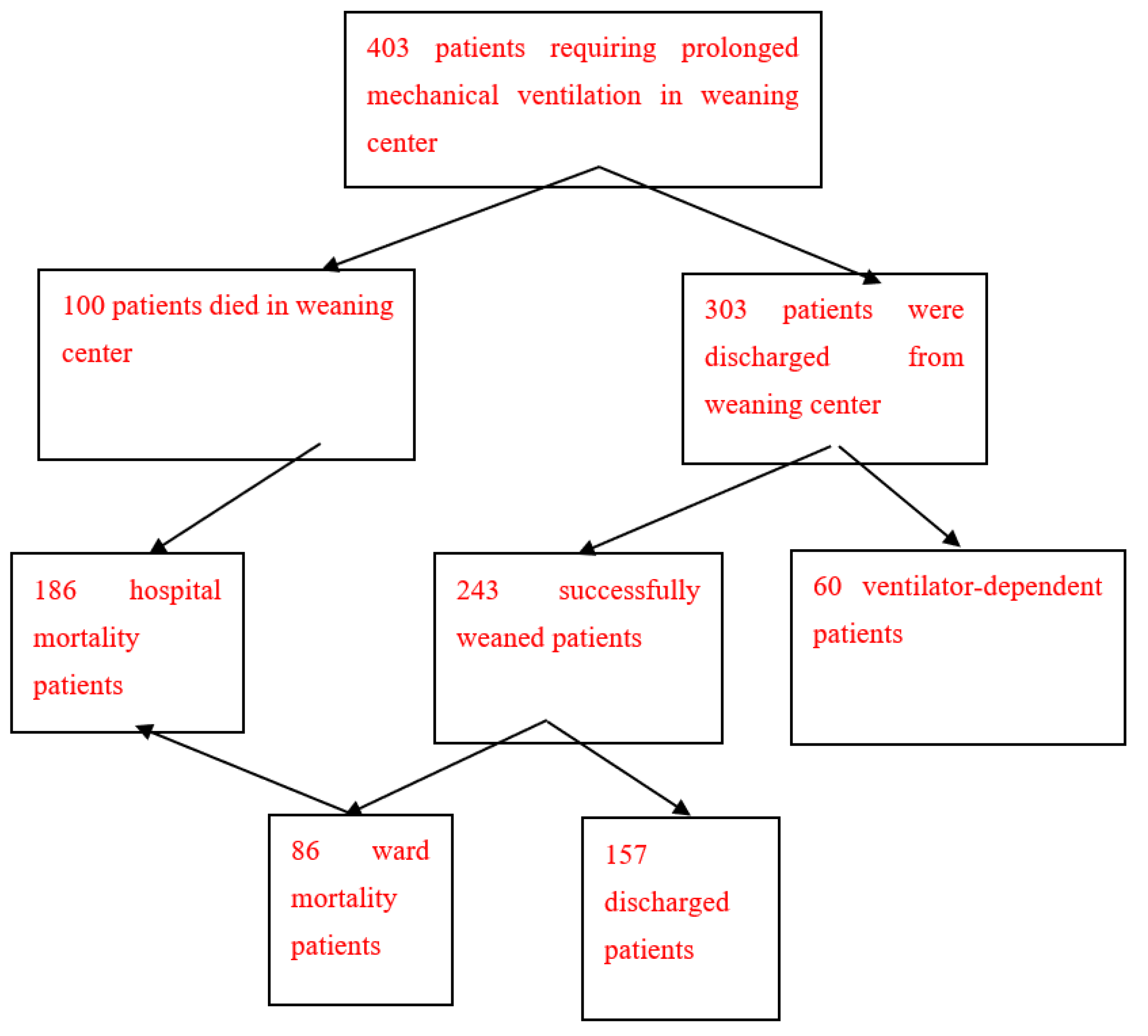
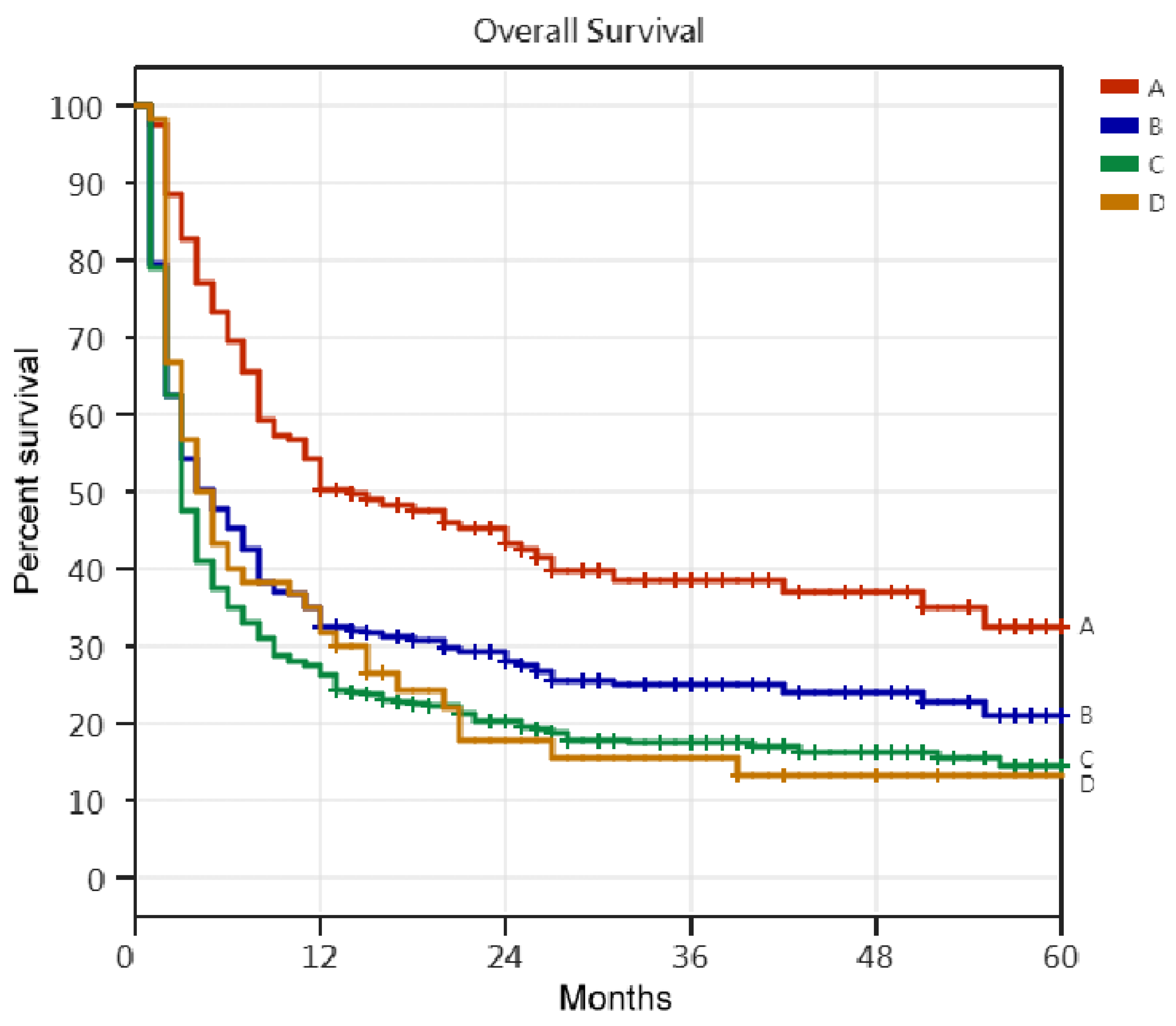
3. Results
4. Discussion
4.1. The One-Year Survival Rate of PMV Patients
4.2. The One-Year Survival Rate of Patients Discharged after Successfully Weaned from PMV (Discharged PMV Patients)
4.3. Five-Year Survival Rate of PMV Patients
4.4. Five-Year Survival Rate of Discharged PMV Patients
4.5. Improving the Long-Term Survival Outcomes of PMV Patients
4.6. Clinical Outcomes in COVID-19 Patients Requiring Mechanical Ventilation
Limitations of This Study
5. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- MacIntyre, N.R.; Epstein, S.K.; Carson, S.; Scheinhorn, D.; Christopher, K.; Muldoon, S. Management of Patients Requiring Prolonged Mechanical Ventilation: Report of a NAMDRC Consensus Conference. Chest 2005, 128, 3937–3954. [Google Scholar] [CrossRef] [PubMed]
- Huang, C. How prolonged mechanical ventilation is a neglected disease in chest medicine: A study of prolonged mechanical ventilation based on 6 years of experience in Taiwan. Ther. Adv. Respir. Dis. 2019, 13, 1753466619878552. [Google Scholar] [CrossRef]
- Carson, S.S. Outcomes of prolonged mechanical ventilation. Curr. Opin. Crit. Care 2006, 12, 405–411. [Google Scholar] [CrossRef]
- Carson, S.S. Definitions and Epidemiology of the Chronically Critically Ill. Respir. Care 2012, 57, 848–858. [Google Scholar] [CrossRef] [PubMed]
- Damuth, E.; Mitchell, J.A.; Bartock, J.L.; Roberts, B.W.; Trzeciak, S. Long-term survival of critically ill patients treated with prolonged mechanical ventilation: A systematic review and meta-analysis. Lancet Respir. Med. 2015, 3, 544–553. [Google Scholar] [CrossRef]
- Bureau of National Health Insurance. Prospective Payment System of Ventilator Dependents Managed Care Demonstration. Available online: https://www.nhi.gov.tw/Resource/webdata/13988_1_1050002331-1.pdf (accessed on 1 April 2016).
- Auld, S.C.; Caridi-Scheible, M.; Blum, J.M.; Robichaux, C.; Kraft, C.; Jacob, J.T.; Jabaley, C.S.; Carpenter, D.; Kaplow, R.; Hernandez-Romieu, A.C.; et al. ICU and Ventilator Mortality Among Critically Ill Adults with Coronavirus Disease 2019. Crit. Care Med. 2020, 48, e799–e804. [Google Scholar] [CrossRef]
- Guan, W.J.; Ni, Z.Y.; Hu, Y.; Liang, W.H.; Qu, C.Q.; He, J.X.; Liu, L.; Shan, H.; Lei, C.L.; Hui, D.S.C.; et al. Clinical Characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Stoller, J.K.; Xu, M.; Mascha, E.; Rice, R. Long-term Outcomes for Patients Discharged from a Long-term Hospital-Based Weaning Unit. Chest 2003, 124, 1892–1899. [Google Scholar] [CrossRef]
- Pilcher, D.V.; Bailey, M.J.; Treacher, D.F.; Hamid, S.; Williams, A.J.; Davidson, A.C. Outcomes, cost and long term survival of patients referred to a regional weaning centre. Thorax 2005, 60, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Scheinhorn, D.J.; Hassenpflug, M.S.; Votto, J.J.; Chao, D.C.; Epstein, S.K.; Doig, G.S.; Knight, E.B.; Petrak, R.A. Post-ICU Mechanical Ventilation at 23 Long-term Care Hospitals: A Multicenter Outcomes Study. Chest 2007, 131, 85–93. [Google Scholar] [CrossRef]
- Bigatello, L.M.; Stelfox, H.T.; Berra, L.; Schmidt, U.; Gettings, E.M. Outcome of patients undergoing prolonged mechanical ventilation after critical illness. Crit. Care Med. 2007, 35, 2491–2497. [Google Scholar] [CrossRef]
- Cox, C.E.; Martinu, T.; Sathy, S.J.; Clay, A.S.; Chia, J.; Gray, A.L.; Olsen, M.K.; Govert, J.A.; Carson, S.S.; Tulsky, J.A. Expectations and outcomes of prolonged mechanical ventilation. Crit. Care Med. 2009, 37, 2888–2894. [Google Scholar] [CrossRef]
- Carson, S.S.; Kahn, J.; Hough, C.L.; Seeley, E.J.; White, D.B.; Douglas, I.; Cox, C.E.; Caldwell, E.; Bangdiwala, S.I.; Garrett, J.M.; et al. A multicenter mortality prediction model for patients receiving prolonged mechanical ventilation. Crit. Care Med. 2012, 40, 1171–1176. [Google Scholar] [CrossRef] [PubMed]
- Rose, L.; Fraser, I.M. Patient Characteristics and Outcomes of a Provincial Prolonged-Ventilation Weaning Centre: A Retrospective Cohort Study. Can. Respir. J. 2012, 19, 216–220. [Google Scholar] [CrossRef]
- Lin, M.-S.; Yan, Y.-H.; Wang, J.-D.; Lu, H.-M.; Chen, L.; Hung, M.-C.; Fan, P.-S.; Chen, C.-R. Improved Survival for an Integrated System of Reduced Intensive Respiratory Care for Patients Requiring Prolonged Mechanical Ventilation. Respir. Care 2013, 58, 517–524. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-T.; Lin, J.-W.; Ruan, S.-Y.; Chen, C.-Y.; Yu, C.-J. Preadmission tracheostomy is associated with better outcomes in patients with prolonged mechanical ventilation in the postintensive care respiratory care setting. J. Formos. Med. Assoc. 2017, 116, 169–176. [Google Scholar] [CrossRef]
- Schönhofer, B.; Euteneuer, S.; Nava, S.; Suchi, S.; Kohler, D. Survival of mechanically ventilated patients admitted to a specialised weaning centre. Intensiv. Care Med. 2002, 28, 908–916. [Google Scholar] [CrossRef] [PubMed]
- Su, J.; Lin, C.-Y.; Chen, P.-J.; Lin, F.J.; Chen, S.-K.; Kuo, H.-T. Experience with a step-down respiratory care center at a tertiary referral medical center in Taiwan. J. Crit. Care 2006, 21, 156–161. [Google Scholar] [CrossRef]
- Davies, M.G.; Quinnell, T.G.; Oscroft, N.S.; Clutterbuck, S.P.; Shneerson, J.M.; Smith, I.E. Hospital outcomes and long-term survival after referral to a specialized weaning unit. Br. J. Anaesth. 2017, 118, 563–569. [Google Scholar] [CrossRef]
- Jubran, A.; Grant, B.J.B.; Duffner, L.A.; Collins, E.G.; Lanuza, D.M.; Hoffman, L.A.; Tobin, M.J. Long-Term Outcome after Prolonged Mechanical Ventilation. A Long-Term Acute-Care Hospital Study. Am. J. Respir. Crit. Care Med. 2019, 199, 1508–1516. [Google Scholar] [CrossRef]
- Warnke, C.; Heine, A.; Müller-Heinrich, A.; Knaak, C.; Friesecke, S.; Obst, A.; Bollmann, T.; Desole, S.; Boesche, M.; Stubbe, B.; et al. Predictors of survival after prolonged weaning from mechanical ventilation. J. Crit. Care 2020, 60, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Huang, C. The Long-Term Survival of Successfully Weaned Prolonged Mechanical Ventilation Patients. Int. J. Gen. Med. 2021, 14, 3981–3988. [Google Scholar] [CrossRef] [PubMed]
- Combes, A.; Luyt, C.-E.; Nieszkowska, A.; Trouillet, J.-L.; Gibert, C.; Chastre, J. Is tracheostomy associated with better outcomes for patients requiring long-term mechanical ventilation? Crit. Care Med. 2007, 35, 802–807. [Google Scholar] [CrossRef]
- Huang, C.H.; Chen, I.-H. The Clinical Application of the Tracheostomy Decision-Making Program in Respiratory Care Center Prolonged Mechanical Ventilation Patients in Taiwan. Int. J. Gen. Med. 2020, 13, 1487–1494. [Google Scholar] [CrossRef]
- Docherty, A.B.; Mulholland, R.H.; Lone, N., I; Cheyne, C.P.; De Angelis, D.; Diaz-Ordaz, K.; Donegan, C.; Drake, T.M.; Dunning, J.; Funk, S.; et al. Changes in in-hospital mortality in the first wave of COVID-19: A multicentre prospective observational cohort study using the WHO Clinical Characterisation Protocol UK. Lancet Respir. Med. 2021, 9, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.-D.; Ding, M.; Dong, X.; Zhang, J.-J.; Azkur, A.K.; Azkur, D.; Gan, H.; Sun, Y.-L.; Fu, W.; Li, W.; et al. Risk factors for severe and critically ill COVID-19 patients: A review. Allergy 2021, 76, 428–455. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and Important Lessons from the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef]
- Grasselli, G.; Pesenti, A.; Cecconi, M. Critical Care Utilization for the COVID-19 Outbreak in Lombardy, Italy: Early experience and forecast during an emergency response. JAMA 2020, 323, 1545–1546. [Google Scholar] [CrossRef]
- Zhou, F.; Yu, T.; Du, R.; Fan, G.; Liu, Y.; Liu, Z.; Xiang, J.; Wang, Y.; Song, B.; Gu, X.; et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet 2020, 395, 1054–1062. [Google Scholar] [CrossRef]
- Rawson, T.M.; Moore, L.S.P.; Zhu, N.; Ranganathan, N.; Skolimowska, K.; Gilchrist, M.; Satta, G.; Cooke, G.; Holmes, A.H. Bacterial and Fungal Coinfection in Individuals with Coronavirus: A Rapid Review to Support COVID-19 Antimicrobial Prescribing. Clin. Infect. Dis. 2020, 71, 2459–2468. [Google Scholar] [CrossRef]
- Musuuza, J.S.; Watson, L.; Parmasad, V.; Putman-Buehler, N.; Christensen, L.; Safdar, N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0251170. [Google Scholar] [CrossRef] [PubMed]
- Melamed, R.; Paz, F.; Jepsen, S.; Smith, C.; Saavedra, R.; Mulder, M.; Masood, A.; Huelster, J.; Kirkland, L.; Guenther, A.; et al. Prognostic factors and outcomes in COVID-19 patients requiring prolonged mechanical ventilation: A retrospective cohort study. Ther. Adv. Respir. Dis. 2022, 16, 17534666221086415. [Google Scholar] [CrossRef] [PubMed]
- Bergman, Z.R.; Tignanelli, C.J.; Gould, R.; Pendleton, K.M.; Chipman, J.G.; Lusczek, E.; Beilman, G. Factors Associated with Mortality in Patients with COVID-19 Receiving Prolonged Ventilatory Support. Surg. Infect. 2022, 23, 893–901. [Google Scholar] [CrossRef] [PubMed]
| Ward Mortality Patients | Discharged PMV Patients | RCC Mortality Patients | RCW Patients | |
|---|---|---|---|---|
| (No = 86) | (No = 157) | (No = 100) | (No = 60) | |
| Tracheostomy, No | 4 (4.65%) | 29 (18.47%) | 12 (12.0%) | 20 (33.3%) |
| Age Groups, No | ||||
| Age < 45 Y/O, No | 3 (3.49%) | 4 (2.55%) | 1 (1.0%) | 1 (1.67%) |
| Age 45–54 Y/O, No | 6 (6.98%) | 14 (8.92%) | 9 (9.0%) | 9 (15.0%) |
| Age 55–64 Y/O, No | 7 (8.14%) | 22 (14.01%) | 14 (14.0%) | 4 (6.67%) |
| Age 65–74 Y/O, No | 22 (25.58%) | 36 (22.93%) | 15 (15.0%) | 15 (25.0%) |
| Age 75–84 Y/O, No | 34 (39.53) | 51 (32.48%) | 42 (42.0%) | 26 (43.3%) |
| Age ≥ 85 Y/O, No | 14 (16.28%) | 30 (19.11%) | 19 (19.0%) | 5 (8.33%) |
| Causes of respiratory failure led to PMV, No | ||||
| pneumonia, No | 31 (36.04%) | 65 (41.4%) | 34 (34.0%) | 19 (31.7%) |
| intracranial hemorrhage, No | 20 (23.26%) | 31 (19.75%) | 13 (13.0%) | 4 (6.67.%) |
| sepsis, No | 10 (11.63%) | 11 (7.01%) | 15 (15.0%) | 9 (15.0%) |
| COPD, No | 2 (2.33%) | 7 (4.46%) | 7 (7.0%) | 7 (11.6%) |
| cardiac disease, No | 6 (6.98%) | 8 (5.1%) | 8 (8.0%) | 3 (5.0%) |
| malignant patients, No | 2 (2.33%) | 3 (1.91%) | 7 (7.0%) | 3 (5.0%) |
| post operation, No | 3 (3.49%) | 12 (7.64%) | 6 (6.0%) | 7 (11.6%) |
| cervical spine diseases, No | 0(0%) | 3 (1.91%) | 2 (2.0%) | 1 (1.67%) |
| post-CPCR, No | 2 (2.33%) | 2 (1.27%) | 1 (1.0%) | 2 (3.33%) |
| cerebral infarction, No | 3 (3.49%) | 3 (1.91%) | 1 (1.0%) | 0 (0%) |
| Comorbidity, No | ||||
| cardiovascular disease, No | 58 (67.44%) | 100 (63.7%) | 65 (65.0%) | 37 (61.7%) |
| chronic lung disease, No | 13 (15.12%) | 36 (22.93%) | 19 (19.0%) | 12 (2.0%) |
| chronic kidney disease, No | 16 (18.6%) | 16 (10.19%) | 12 (12.0%) | 5 (8.33%) |
| end-stage renal disease (requiring dialysis), No | 12 (13.95%) | 9 (5.73%) | 11 (11.0%) | 5 (8.33%) |
| neurologic disease, No | 27 (31.4%) | 52 (33.12%) | 27 (27.0%) | 21 (35.0%) |
| metabolic disease, No | 39 (45.35%) | 56 (35.67%) | 35 (35.0%) | 27 (45.0%) |
| malignant diseases, No | 15 (17.44%) | 16 (10.19%) | 26 (26.0%) | 6 (10.0%) |
| no comorbidity, No | 4 (4.65%) | 19 (12.1%) | 4 (4.0%) | 4 (6.67%) |
| one comorbidity, No | 25 (29.07%) | 33 (21.02%) | 30 (30.0%) | 19 (31.7%) |
| two comorbidities, No | 27 (31.4%) | 53 (33.76%) | 30 (30.0%) | 15 (25.0%) |
| three comorbidities, No | 14 (16.28%) | 40 (25.48%) | 25 (25.0%) | 17 (28.3%) |
| ≥four comorbidities, No | 16 (18.6%) | 12 (7.64%) | 11 (11.0%) | 5 (8.33%) |
| Patients, No /Survival Time | Patients Requiring PMV (No = 403) | Successfully Weaned Patients (No = 243) | Discharged PMV Patients (No = 157) | RCW Patients (No = 60) |
|---|---|---|---|---|
| Dead patients, No | 331 (82.1%) | 181 (74.5%) | 95 (60.5%) | 50 (83.3%) |
| 0–3 months, No | 212 (52.6%) | 111 (45.7%) | 27 (17.2%) | 26 (43.3%) |
| 4–6 months, No | 50 (12.4%) | 22 (9.0%) | 21 (13.4%) | 10 (16.7%)5(8.3%) |
| 7–12 months, No | 35 (8.7%) | 31 (12.8%) | 30 (19.1%) | 7 (11.7%) |
| less than 2 years, No | 22 (5.5%) | 9 (3.7%) | 9 (5.7%) | 1 (1.7%) |
| less than 3 years, No | 8 (2.0%) | 5 (2.0%) | 5 (3.2%) | 1 (1.7%) |
| less than 4 years, No | 2 (0.5%) | 1 (0.4%) | 1 (0.6%) | 0 |
| less than 5 years, No | 2 (0.5%) | 2 (0.8%) | 2 (1.3%) | 0 |
| more than 5 years, No | 0 | 0 | 0 | |
| Alive patients, No | 72 (17.9%) | 62 (25.5%) | 62 (39.5%) | 0 |
| 0–3 months, No | 0 | 0 | 0 | 0 |
| 4–6 months, No | 0 | 0 | 0 | 0 |
| 7–12 months, No | 1 (0.30%) | 1 (0.4%) | 1 (0.6%) | 4 (6.7%) |
| less than 2 years, No | 25 (6.2%) | 21 (8.6%) | 21 (13.4%) | 0 |
| less than 3 years, No | 10 (2.5%) | 10 (4.1%) | 10 (6.7%) | 3 (5.0%) |
| less than 4 years, No | 14 (3.5%) | 11 (4.5%) | 11 (7.0%) | 1 (1.7%) |
| less than 5 years, No | 13 (3.2%) | 12 (4.9%) | 12 (7.6%) | 2 (3.3%) |
| more than 5 years, | 9 (2.2%) | 7 (2.9%) | 7 (4.5%) |
| Authors | Patients No. | One-Year Survival Rate (%) | Factors of Poor One-Year Survival Rate | Factors of Good One-Year Survival Rate |
|---|---|---|---|---|
| Stoller [9] | 162 | 43% | older age | |
| Pilcher [10] | 153 | 58% | older age, high | |
| APACHE score | ||||
| Scheinhorn [11] | 1419 | 40% | failure to wean | |
| Bigatello [12] | 146 | 61% | ||
| Cox [13] | 126 | 56% | ||
| Carson [14] | 260 | 52% | age > 65 Y/O, | |
| thrombocytopenia, | ||||
| use vasopressors, | ||||
| Rose [15] | 115 | 50% | ESRD | |
| Lin [16] | 533 | 37.20% | young age, absence of liver cirrhosis | |
| tracheostomy | ||||
| Huang [17] | 401 | 46% | patients | |
| high APACHE II | ||||
| score, CHF, ESRD, | ||||
| malignancy, liver | no comorbidity | |||
| Huang [2] | 403 | 24.30% | cirrhosis | |
| age > 75Y/O, ESRD, | ||||
| four comorbidities, |
| Authors | Patients No. | One-Year Survival Rate (%) | Factors of Poor One-Year Survival Rate | Factors of Good One-Year Survival Rate |
|---|---|---|---|---|
| Schonhofer [18] | 293 | 49.40% | failure to wean | young age, low |
| APACHE II score | ||||
| Su [19] | 244 | 44.60% | ||
| Davies [20] | 458 | 65.00% | failure to wean, | nocturnal use of |
| older age, | NIV | |||
| Jubran [21] | 315 | 66.90% | high SAPS score, high APACHII, low body mass index, failure to wean | |
| Warnke [22] | 597 | 66.50% | older age, | |
| failure to wean | ||||
| Huang [23] | 157 | 50.30% | ||
| age > 85Y/O, | no comorbidity, undergoing tracheostomy | |||
| four comorbidities, |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, C. The Survival Outcomes of Patients Requiring Prolonged Mechanical Ventilation. Medicina 2023, 59, 614. https://doi.org/10.3390/medicina59030614
Huang C. The Survival Outcomes of Patients Requiring Prolonged Mechanical Ventilation. Medicina. 2023; 59(3):614. https://doi.org/10.3390/medicina59030614
Chicago/Turabian StyleHuang, Chienhsiu. 2023. "The Survival Outcomes of Patients Requiring Prolonged Mechanical Ventilation" Medicina 59, no. 3: 614. https://doi.org/10.3390/medicina59030614
APA StyleHuang, C. (2023). The Survival Outcomes of Patients Requiring Prolonged Mechanical Ventilation. Medicina, 59(3), 614. https://doi.org/10.3390/medicina59030614







