Adherence to the Mediterranean Diet Association with Serum Inflammatory Factors Stress Oxidative and Appetite in COVID-19 Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Biochemical Measurements
2.3. Appetite Assessment
2.4. Mediterranean Dietary Pattern Assessment
2.5. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ciotti, M.; Ciccozzi, M.; Terrinoni, A.; Jiang, W.-C.; Wang, C.-B.; Bernardini, S. The COVID-19 pandemic. Crit. Rev. Clin. Lab. Sci. 2020, 57, 365–388. [Google Scholar] [CrossRef] [PubMed]
- Calder, P.C.; Carr, A.C.; Gombart, A.F.; Eggersdorfer, M. Optimal nutritional status for a well-functioning immune system is an important factor to protect against viral infections. Nutrients 2020, 12, 1181. [Google Scholar] [CrossRef] [PubMed]
- Polverino, E.; Goeminne, P.C.; McDonnell, M.J.; Aliberti, S.; Marshall, S.E.; Loebinger, M.R.; Murris, M.; Cantón, R.; Torres, A.; Dimakou, K.; et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur. Respir. J. 2017, 50, 1700629. [Google Scholar] [CrossRef]
- McElvaney, O.J.; McEvoy, N.L.; McElvaney, O.F.; Carroll, T.P.; Murphy, M.P.; Dunlea, D.M.; Ni Choileain, O.; Clarke, J.; O’Connor, E.; Hogan, G.; et al. Characterization of the inflammatory response to severe COVID-19 illness. Am. J. Respir. Crit. Care Med. 2020, 202, 812–821. [Google Scholar] [CrossRef] [PubMed]
- Merad, M.; Subramanian, A.; Wang, T.T. An aberrant inflammatory response in severe COVID-19. Cell Host Microbe 2021, 29, 1043–1047. [Google Scholar] [CrossRef]
- Jafarzadeh, A.; Chauhan, P.; Saha, B.; Jafarzadeh, S.; Nemati, M. Contribution of monocytes and macrophages to the local tissue inflammation and cytokine storm in COVID-19: Lessons from SARS and MERS, and potential therapeutic interventions. Life Sci. 2020, 257, 118102. [Google Scholar] [CrossRef]
- Bouayad, A. Innate immune evasion by SARS-CoV-2: Comparison with SARS-CoV. Rev. Med. Virol. 2020, 30, 1–9. [Google Scholar] [CrossRef]
- Song, P.; Li, W.; Xie, J.; Hou, Y.; You, C. Cytokine storm induced by SARS-CoV-2. Clin. Chim. Acta. 2020, 509, 280–287. [Google Scholar] [CrossRef]
- Martínez-Colón, G.J.; Ratnasiri, K.; Chen, H.; Jiang, S.; Zanley, E.; Rustagi, A.; Verma, R.; Chen, H.; Andrews, J.R.; Mertz, K.D.; et al. SARS-CoV-2 infection drives an inflammatory response in human adipose tissue through infection of adipocytes and macrophages. Sci. Transl. Med. 2022, 14, eabm9151. [Google Scholar] [CrossRef]
- Akbari, H.; Tabrizi, R.; Lankarani, K.B.; Aria, H.; Vakili, S.; Asadian, F.; Noroozi, S.; Keshavarz, P.; Faramarz, S. The role of cytokine profile and lymphocyte subsets in the severity of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis. Life Sci. 2020, 258, 118167. [Google Scholar] [CrossRef]
- Pieri, M.; Ciotti, M.; Nuccetelli, M.; Perrone, M.A.; Caliò, M.T.; Lia, M.S.; Minieri, M.; Bernardini, S. Serum Amyloid A Protein as a useful biomarker to predict COVID-19 patients severity and prognosis. Int. Immunopharmaco. 2021, 95, 107512. [Google Scholar] [CrossRef]
- Sorić Hosman, I.; Kos, I.; Lamot, L. Serum amyloid A in inflammatory rheumatic diseases: A compendious review of a renowned biomarker. Front. Immunol. 2021, 11, 631299. [Google Scholar] [CrossRef] [PubMed]
- Tanacan, A.; Yazihan, N.; Erol, S.A.; Anuk, A.T.; Yetiskin, F.D.Y.; Biriken, D.; Ozgu-Erdinc, A.; Keskin, H.L.; Tekin, O.M.; Sahin, D. The impact of COVID-19 infection on the cytokine profile of pregnant women: A prospective case-control study. Cytokine 2021, 140, 155431. [Google Scholar] [CrossRef] [PubMed]
- Ullah, R.; Khan, J.; Basharat, N.; Huo, D.; Ud Din, A.; Wang, G. Evaluation of Cardiac Biomarkers and Expression Analysis of IL-1, IL-6, IL-10, IL-17, and IL-25 among COVID-19 Patients from Pakistan. Viruses 2022, 14, 2149. [Google Scholar] [CrossRef]
- Anania, C.; Perla, F.M.; Olivero, F.; Pacifico, L.; Chiesa, C. Mediterranean diet and nonalcoholic fatty liver disease. World J. Gastroenterol. 2018, 24, 2083. [Google Scholar] [CrossRef] [PubMed]
- Saura-Calixto, F.; Goni, I. Definition of the Mediterranean diet based on bioactive compounds. Crit. Rev. Food Sci. Nutr. 2009, 49, 145–152. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Martínez-González, M.A.; Tong, T.Y.; Forouhi, N.G.; Khandelwal, S.; Prabhakaran, D.; Mozaffarian, D.; de Lorgeril, M. Definitions and potential health benefits of the Mediterranean diet: Views from experts around the world. BMC Med. 2014, 12, 112. [Google Scholar] [CrossRef]
- Martín-Peláez, S.; Fito, M.; Castaner, O. Mediterranean diet effects on type 2 diabetes prevention, disease progression, and related mechanisms. A review. Nutrients 2020, 12, 2236. [Google Scholar] [CrossRef]
- Finicelli, M.; Squillaro, T.; Di Cristo, F.; Di Salle, A.; Melone, M.A.B.; Galderisi, U.; Peluso, G. Metabolic syndrome, Mediterranean diet, and polyphenols: Evidence and perspectives. J. Cell. Physiol. 2019, 234, 5807–5826. [Google Scholar] [CrossRef]
- Veček, N.N.; Mucalo, L.; Dragun, R.; Miličević, T.; Pribisalić, A.; Patarčić, I.; Hayward, C.; Polašek, O.; Kolčić, I. The association between salt taste perception, mediterranean diet and metabolic syndrome: A cross-sectional study. Nutrients 2020, 12, 1164. [Google Scholar] [CrossRef]
- Koopen, A.M.; Almeida, E.L.; Attaye, I.; Witjes, J.J.; Rampanelli, E.; Majait, S.; Kemper, M.; Levels, J.H.M.; Schimmel, A.W.M.; Herrema, H.; et al. Effect of fecal microbiota transplantation combined with Mediterranean diet on insulin sensitivity in subjects with metabolic syndrome. Front. Microbiol. 2021, 12, 662159. [Google Scholar] [CrossRef] [PubMed]
- Finicelli, M.; Di Salle, A.; Galderisi, U.; Peluso, G. The Mediterranean Diet: An Update of the Clinical Trials. Nutrients 2022, 14, 2956. [Google Scholar] [CrossRef] [PubMed]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean diet: A review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef] [PubMed]
- Mazzocchi, A.; Leone, L.; Agostoni, C.; Pali-Schöll, I. The secrets of the Mediterranean diet. Does [only] olive oil matter? Nutrients 2019, 11, 2941. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventós, R.; Ros, E.; Salaverría, I.; Fiol, M.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2011, 141, 1140–1145. [Google Scholar] [CrossRef] [PubMed]
- Barrea, L.; Vetrani, C.; Caprio, M.; Cataldi, M.; Ghoch, M.E.; Elce, A.; Camajani, E.; Verde, L.; Savastano, S.; Colao, A.; et al. From the Ketogenic Diet to the Mediterranean Diet: The Potential Dietary Therapy in Patients with Obesity after CoVID-19 Infection (Post CoVID Syndrome). Curr. Obes. Rep. 2022, 11, 144–165. [Google Scholar] [CrossRef]
- Greene, M.W.; Roberts, A.P.; Frugé, A.D. Negative association between Mediterranean diet adherence and COVID-19 cases and related deaths in Spain and 23 OECD countries: An ecological study. Front. Nutr. 2021, 8, 591964. [Google Scholar] [CrossRef]
- Perez-Araluce, R.; Martinez-Gonzalez, M.A.; Fernández-Lázaro, C.I.; Bes-Rastrollo, M.; Gea, A.; Carlos, S. Mediterranean diet and the risk of COVID-19 in the ‘Seguimiento Universidad de Navarra’ cohort. Clin. Nutr. 2021, 41, 3061–3068. [Google Scholar] [CrossRef]
- Fedullo, A.L.; Schiattarella, A.; Morlando, M.; Raguzzini, A.; Toti, E.; De Franciscis, P.; Peluso, I. Mediterranean Diet for the Prevention of Gestational Diabetes in the Covid-19 Era: Implications of Il-6 In Diabesity. Int. J. Mol. Sci. 2021, 22, 1213. [Google Scholar] [CrossRef]
- Guilleminault, L.; Williams, E.J.; Scott, H.A.; Berthon, B.S.; Jensen, M.; Wood, L.G. Diet and asthma: Is it time to adapt our message? Nutrients 2017, 9, 1227. [Google Scholar] [CrossRef]
- Koloverou, E.; Panagiotakos, D.B.; Pitsavos, C.; Chrysohoou, C.; Georgousopoulou, E.N.; Grekas, A.; Christou, A.; Chatzigeorgiou, M.; Skoumas, I.; Tousoulis, D.; et al. Adherence to Mediterranean diet and 10-year incidence (2002–2012) of diabetes: Correlations with inflammatory and oxidative stress biomarkers in the ATTICA cohort study. Diabetes Metab. Res. Rev. 2016, 32, 73–81. [Google Scholar] [CrossRef]
- Maiorino, M.I.; Bellastella, G.; Longo, M.; Caruso, P.; Esposito, K. Mediterranean diet and COVID-19: Hypothesizing potential benefits in people with diabetes. Front. Endocrinol. 2020, 11, 574315. [Google Scholar] [CrossRef] [PubMed]
- Lampropoulos, C.E.; Konsta, M.; Dradaki, V.; Roumpou, A.; Dri, I.; Papaioannou, I. Effects of Mediterranean diet on hospital length of stay, medical expenses, and mortality in elderly, hospitalized patients: A 2-year observational study. Nutrition 2020, 79, 110868. [Google Scholar] [CrossRef] [PubMed]
- Del Valle, D.M.; Kim-Schulze, S.; Huang, H.H.; Beckmann, N.D.; Nirenberg, S.; Wang, B.; Lavin, Y.; Swartz, T.H.; Madduri, D.; Stock, A.; et al. An inflammatory cytokine signature predicts COVID-19 severity and survival. Nat. Med. 2020, 26, 1636–1643. [Google Scholar] [CrossRef] [PubMed]
- Yaghoubi, N.; Youssefi, M.; Jabbari Azad, F.; Farzad, F.; Yavari, Z.; Zahedi Avval, F. Total antioxidant capacity as a marker of severity of COVID-19 infection: Possible prognostic and therapeutic clinical application. J. Med. Virol. 2022, 94, 1558–1565. [Google Scholar] [CrossRef]
- Sureda, A.; Bibiloni, M.D.; Julibert, A.; Bouzas, C.; Argelich, E.; Llompart, I.; Pons, A.; Tur, J.A. Adherence to the Mediterranean Diet and Inflammatory Markers. Nutrients 2018, 10, 62. [Google Scholar] [CrossRef]
- Chrysohoou, C.; Panagiotakos, D.B.; Pitsavos, C.; Das, U.N.; Stefanadis, C. Adherence to the Mediterranean diet attenuates inflammation and coagulation process in healthy adults: The ATTICA Study. J. Am. Coll. Cardiol. 2004, 44, 152–158. [Google Scholar] [CrossRef]
- Martínez-González, M.A.; Salas-Salvadó, J.; Estruch, R.; Corella, D.; Fitó, M.; Ros, E.; Predimed Investigators. Benefits of the Mediterranean diet: Insights from the PREDIMED study. Prog. Cardiovasc. Dis. 2015, 58, 50–60. [Google Scholar] [CrossRef]
- Davis, C.; Bryan, J.; Hodgson, J.; Murphy, K. Definition of the Mediterranean diet: A literature review. Nutrients 2015, 7, 9139–9153. [Google Scholar] [CrossRef]
- Naureen, Z.; Dhuli, K.; Donato, K.; Aquilanti, B.; Velluti, V.; Matera, G.; Iaconelli, A.; Bertelli, M. Foods of the Mediterranean diet: Tomato, olives, chili pepper, wheat flour and wheat germ. J. Prev. Med. Hyg. 2022, 63 (Suppl. 3), E4. [Google Scholar]
- Gantenbein, K.V.; Kanaka-Gantenbein, C. Mediterranean diet as an antioxidant: The impact on metabolic health and overall wellbeing. Nutrients 2021, 13, 1951. [Google Scholar] [CrossRef] [PubMed]
- Koebnick, C.; Black, M.H.; Wu, J.; Shu, Y.-H.; MacKay, A.W.; Watanabe, R.M.; Buchanan, T.A.; Xiang, A.H. A diet high in sugar-sweetened beverage and low in fruits and vegetables is associated with adiposity and a pro-inflammatory adipokine profile. Br. J. Nutr. 2018, 120, 1230–1239. [Google Scholar] [CrossRef] [PubMed]
- Morvaridi, M.; Jafarirad, S.; Seyedian, S.S.; Alavinejad, P.; Cheraghian, B. The effects of extra virgin olive oil and canola oil on inflammatory markers and gastrointestinal symptoms in patients with ulcerative colitis. Eur. J. Clin. Nutr. 2020, 74, 891–899. [Google Scholar] [CrossRef] [PubMed]
- Noce, A.; Marrone, G.; Urciuoli, S.; Di Daniele, F.; Di Lauro, M.; Zaitseva, A.P.; Di Daniele, N.; Romani, A. Usefulness of extra virgin olive oil minor polar compounds in the management of chronic kidney disease patients. Nutrients 2021, 13, 581. [Google Scholar] [CrossRef] [PubMed]
- Angelidi, A.M.; Kokkinos, A.; Katechaki, E.; Ros, E.; Mantzoros, C.S. Mediterranean diet as a nutritional approach for COVID-19. Metab. Clin. Exp. 2021, 114, 154407. [Google Scholar]
- Angelis, A.; Chrysohoou, C.; Tzorovili, E.; Laina, A.; Xydis, P.; Terzis, I.; Ioakeimidis, N.; Aznaouridis, K.; Vlachopoulos, C.; Tsioufis, K. The Mediterranean diet benefit on cardiovascular hemodynamics and erectile function in chronic heart failure male patients by decoding central and peripheral vessel rheology. Nutrients 2020, 13, 108. [Google Scholar] [CrossRef]
- Serra-Majem, L.; Roman-Vinas, B.; Sanchez-Villegas, A.; Guasch-Ferre, M.; Corella, D.; La Vecchia, C. Benefits of the Mediterranean diet: Epidemiological and molecular aspects. Mol. Asp. Med. 2019, 67, 1–55. [Google Scholar] [CrossRef]
- Strasser, B.; Wolters, M.; Weyh, C.; Krüger, K.; Ticinesi, A. The effects of lifestyle and diet on gut microbiota composition, inflammation and muscle performance in our aging society. Nutrients 2021, 13, 2045. [Google Scholar] [CrossRef]
- Baratta, F.; Cammisotto, V.; Tozzi, G.; Coronati, M.; Bartimoccia, S.; Castellani, V.; Nocella, C.; D’Amico, A.; Angelico, F.; Carnevale, R.; et al. High Compliance to Mediterranean Diet Associates with Lower Platelet Activation and Liver Collagen Deposition in Patients with Nonalcoholic Fatty Liver Disease. Nutrients 2022, 14, 1209. [Google Scholar] [CrossRef]
- Nomikos, T.; Fragopoulou, E.; Antonopoulou, S.; Panagiotakos, D.B. Mediterranean diet and platelet-activating factor; a systematic review. Clin. Biochem. 2018, 60, 1–10. [Google Scholar] [CrossRef]
- García-Montero, C.; Fraile-Martínez, O.; Gómez-Lahoz, A.; Pekarek, L.; Castellanos, A.; Noguerales-Fraguas, F.; Coca, S.; Guijarro, L.; García-Honduvilla, N.; Asúnsolo, A.; et al. Nutritional components in Western diet versus Mediterranean diet at the gut microbiota–immune system interplay. Implications for health and disease. Nutrients 2021, 13, 699. [Google Scholar] [CrossRef] [PubMed]

| Variables | Mean ± SD | Men N = 305 | Women N = 295 | p * |
|---|---|---|---|---|
| Age (y) | 52.9 ± 6.8 | 51.8 ± 3.4 | 51.6 ± 6.4 | 0.08 |
| Body mass index (Kg/m2) | 29.5 ± 2.3 | 30.2 ± 2.8 | 28.4 ± 3.9 | 0.02 |
| Smoking (%) | 15 (35.83%) | 215 (72.88%) | 0 | 0.01 & |
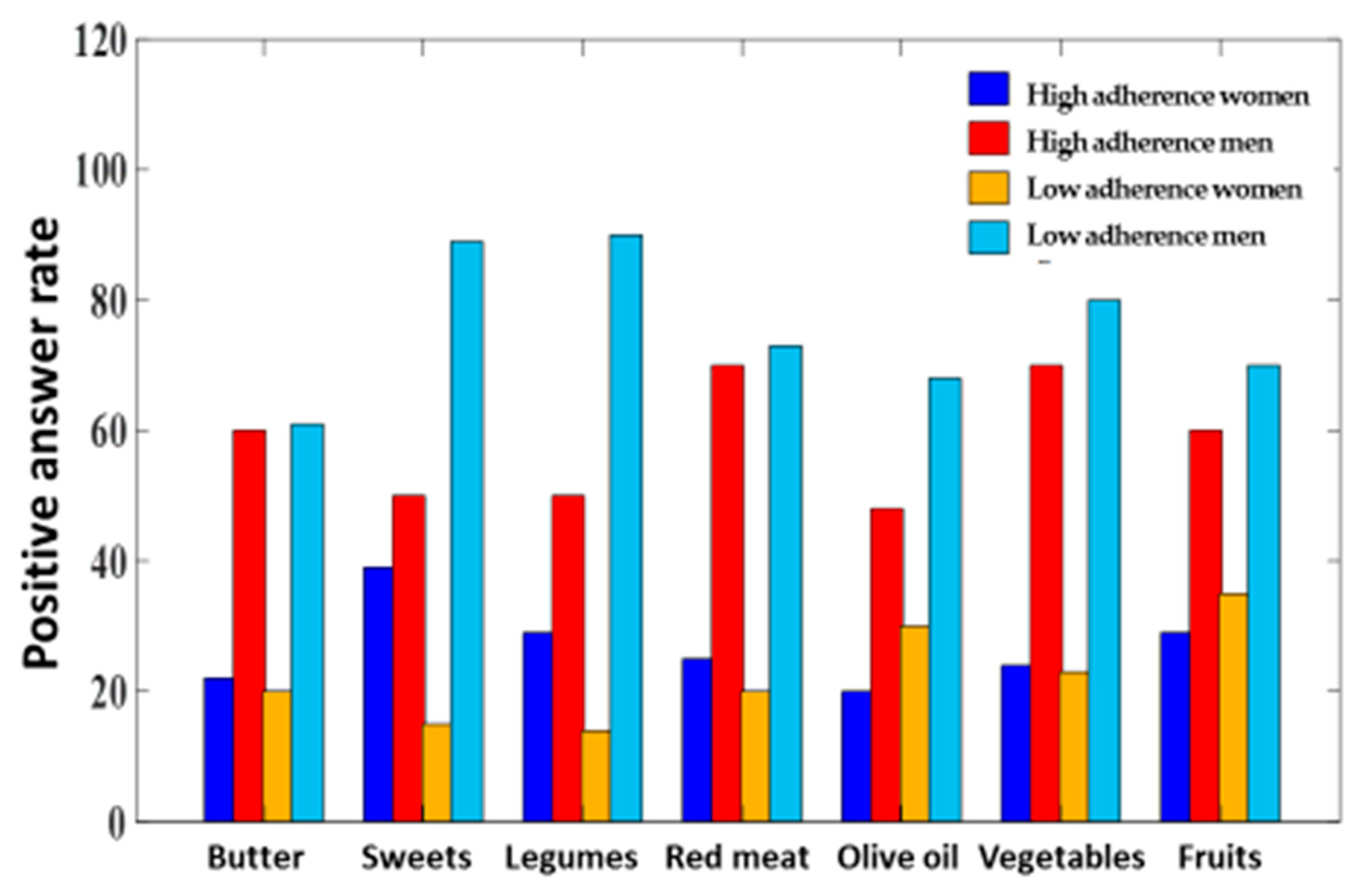
| Low Adherence to MD (N = 495) | High Adherence to MD (N = 105) | p | |||
|---|---|---|---|---|---|
| Olive oil, the main dressing | 68 | (13.73%) | 98 | (93.33%) | 0.01 |
| Olive oil, 4 ts/day | 67 | (13.53%) | 97 | (92.38%) | 0.04 |
| Vegetables, 2 s/day | 94 | (18.98%) | 103 | (98.09%) | 0.02 * |
| Fruits, 3 s/day | 89 | (17.97%) | 105 | (88.57%) | 0.04 * |
| Red meat, <1 s/day | 95 | (19.19%) | 93 | (88.57%) | 0.07 |
| Butter, <1 s/day | 82 | (16.56%) | 81 | (77.14%) | 0.07 |
| Sweet beverage, <1 s/day | 89 | (17.97%) | 104 | (99.04%) | 0.05 * |
| Legumes, 3 s/week | 79 | (15.59%) | 104 | (99.04%) | 0.01 * |
| Fish and seafood, 3 s/week | 61 | (12.32%) | 101 | (96.19%) | 0.02 |
| Sweets, <3 s/week | 101 | (20.40%) | 102 | (97.14%) | 0.06 |
| Nuts, 3/week | 88 | (17.77%) | 104 | (99.04%) | 0.01 * |
| White meat over red | 102 | (20.60%) | 104 | (99.04%) | 0.06 |
| Symptoms | High Adherence N = 105 (%) | Low Adherence N = 495 (%) | p * |
|---|---|---|---|
| Fever | 50 (47.6%) | 482 (92.5%) | 0.02 |
| Cough | 38 (36.1%) | 380 (76.7%) | 0.01 |
| Dyspnea | 62 (59.04%) | 392 (79.1%) | 0.02 |
| Fatigue | 98 (93.3%) | 421 (85.05%) | 0.03 |
| Taste/smell abnormalities | 23 (21.9%) | 365 (73.7%) | 0.05 |
| Diarrhea | 44 (41.9%) | 280 (56.5%) | 0.02 |
| Systolic BP (mmHg) Mean ± SD | 102.2 ± 12.1 | 120.3 ± 10.5 | 0.04 # |
| Diastolic BP (mmHg) Mean ± SD | 77.3 ± 12.1 | 81.2 ± 9.8 | 0.01 # |
| Heart rate (/min) Mean ± SD | 88.6 ± 4.2 | 87.9 ± 2.3 | 0.09 # |
| Respiratory rate (/min) Mean ± SD | 18.6 ± 2.9 | 18.5 ± 2.9 | 0.8 # |
| Pneumonia Severity Index Mean ± SD | 70.4 ± 6.3 | 73.4 ± 2.4 | 0.04 # |
| Variables | High Adherence N = 105 N (%) | Low Adherence N = 495 N (%) | p * |
|---|---|---|---|
| Desire to eat | 63 (60%) | 114 (23%) | 0.02 |
| Satiety time after eating | |||
| After eating a few tablespoons to a third of a plate | 35 (33%) | 248 (50.10%) | |
| After eating half of all the food served | 30 (25.57%) | 206 (41.61%) | |
| Rarely satiated | 40 (30.09%) | 41 (8.28%) | 0.01 |
| Time of feeling hungry | 0.03 | ||
| Never | 18 (3.63%) | 283 (51.17%) | |
| Low and sometimes | 49 (65.71%) | 104 (21.01%) | |
| The whole day | 38 (36.19%) | 108 (21.81%) | |
| Patients’ opinions about the taste of food | 0.01 | ||
| Bad and very bad | 14 (13.33%) | 264 (53.33%) | |
| Moderate | 28 (26.66%) | 181 (36.59%) | |
| Good and very good | 42 (63%) | 50 (10.10%) |
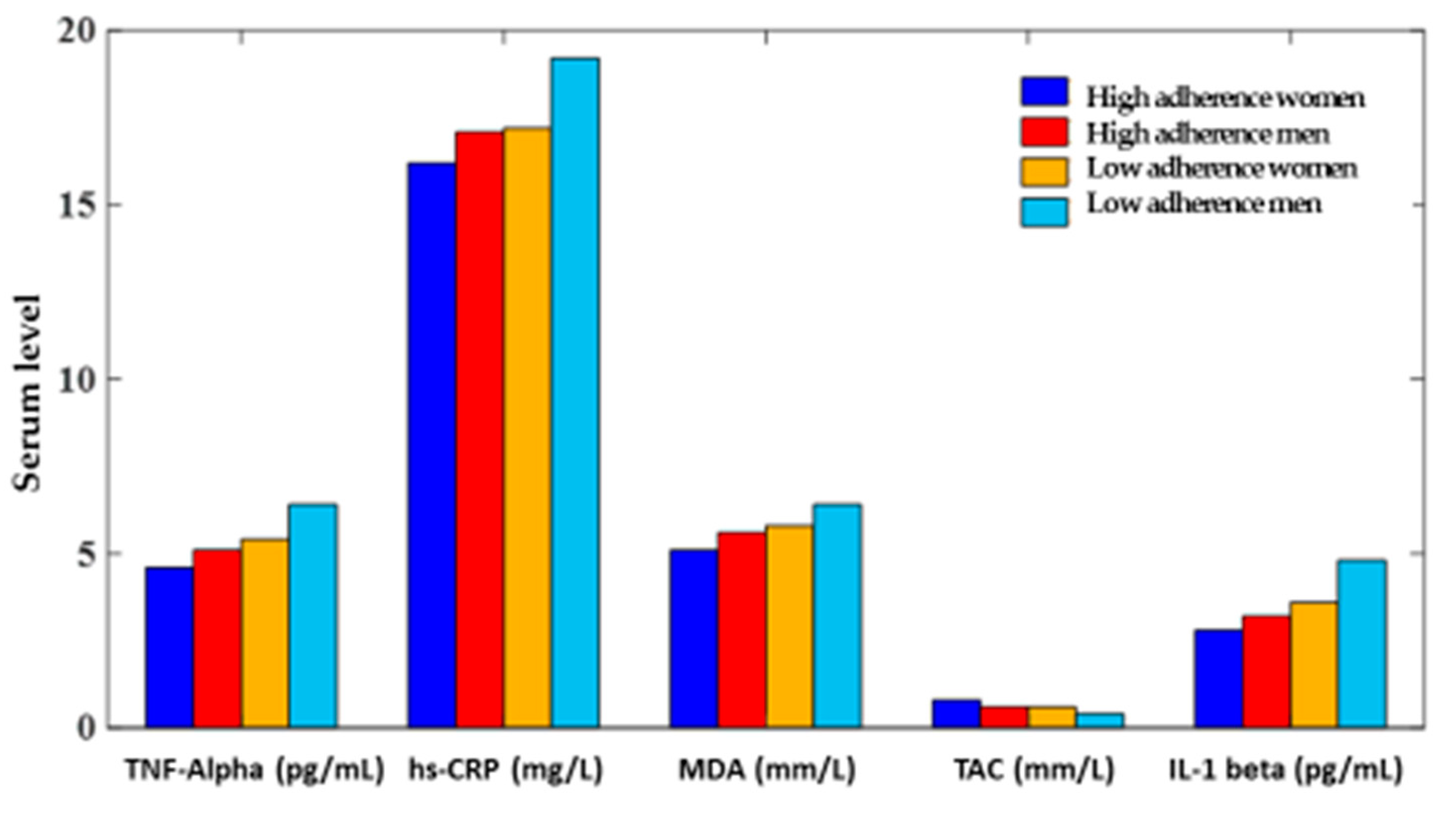
| Adherence to MD (%) | TNF-α pg/mL | Hs-CRP Mg/L | MDA µM/L | TAC Mm/L | Interleukin 1 Beta (pg/mL) |
|---|---|---|---|---|---|
| High adherence N = 105 (%) | 5.7 ± 2.1 | 17.08 ± 4.2 | 5.7 ± 0.2 | 0.8 ± 0.02 | 3.2 ± 0.02 |
| Low adherence N = 495 (%) | 6.9 ± 2.8 | 19.8 ± 2.5 | 6.2 ± 0.3 | 0.6 ± 0.04 | 4.9 ± 0.01 |
| p * | 0.02 | 0.03 | 0.02 | 0.04 | 0.02 |
| Dependent Variables | Coeff. | 95% CI | p * |
|---|---|---|---|
| TNF-α | −1.32 | −1.28, −1.38 | 0.02 |
| Hs-CRP | −1.89 | −1.76, −1.92 | 0.01 |
| MDA | −1.34 | −1.22, −1.48 | 0.04 |
| TAC | 2.04 | 1.98, 2.14 | 0.03 |
| Interleukin 1 beta | −1.08 | −1.02, −1.15 | 0.04 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mohajeri, M.; Mohajery, R.; Cicero, A.F.G. Adherence to the Mediterranean Diet Association with Serum Inflammatory Factors Stress Oxidative and Appetite in COVID-19 Patients. Medicina 2023, 59, 227. https://doi.org/10.3390/medicina59020227
Mohajeri M, Mohajery R, Cicero AFG. Adherence to the Mediterranean Diet Association with Serum Inflammatory Factors Stress Oxidative and Appetite in COVID-19 Patients. Medicina. 2023; 59(2):227. https://doi.org/10.3390/medicina59020227
Chicago/Turabian StyleMohajeri, Mahsa, Reza Mohajery, and Arrigo F. G. Cicero. 2023. "Adherence to the Mediterranean Diet Association with Serum Inflammatory Factors Stress Oxidative and Appetite in COVID-19 Patients" Medicina 59, no. 2: 227. https://doi.org/10.3390/medicina59020227
APA StyleMohajeri, M., Mohajery, R., & Cicero, A. F. G. (2023). Adherence to the Mediterranean Diet Association with Serum Inflammatory Factors Stress Oxidative and Appetite in COVID-19 Patients. Medicina, 59(2), 227. https://doi.org/10.3390/medicina59020227










