Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding
Abstract
:1. Introduction
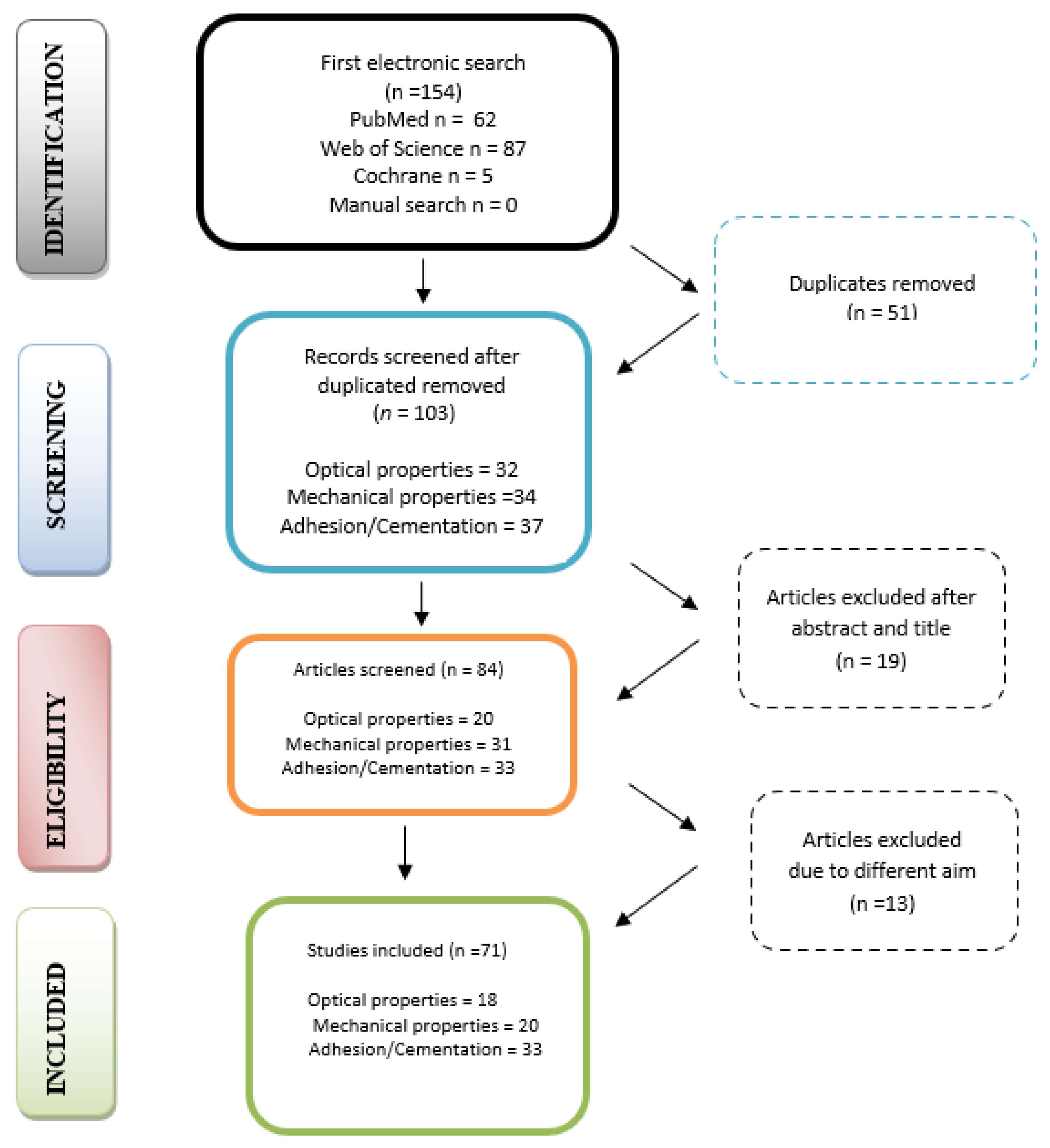
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Study Selection and Data Extraction
2.4. Risk of Bias Assessment
3. Results
4. Discussion
4.1. Optical Properties of ZLS Ceramic Systems
4.2. Mechanical Properties of ZLS Ceramic Systems
4.3. Cementation and Adhesion Features of ZLS Ceramic Systems
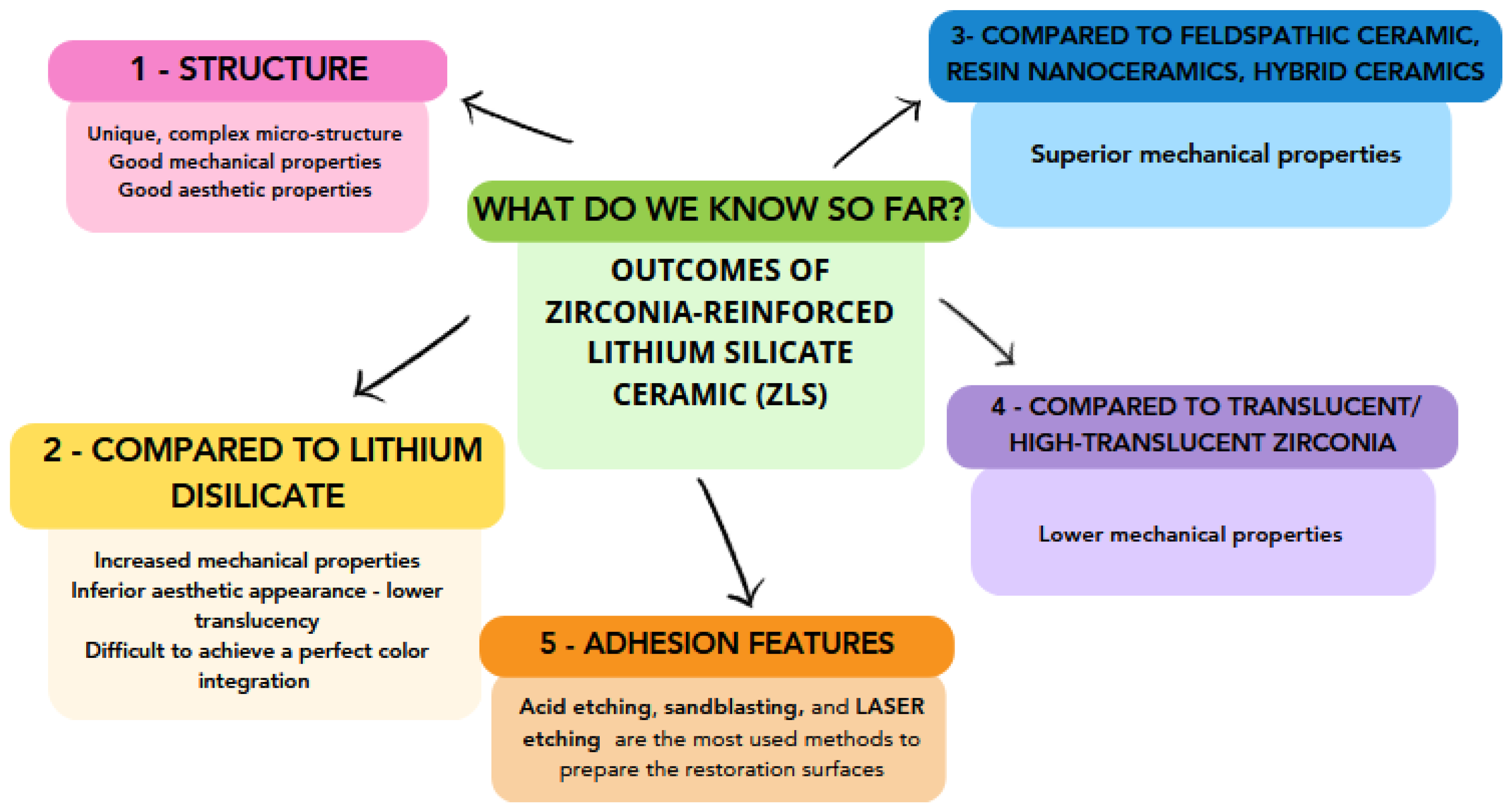
5. Conclusions
- 1.
- Unlike lithium disilicate glass ceramic, zirconia-reinforced lithium-silicate-based ceramic presents a unique, complex microstructure, which increases its mechanical resistance, but decreases its aesthetic appearance, especially its translucency, due to tetragonal zirconia content.
- 2.
- Over the years, the mechanical behavior of ZLS restorations has been widely studied and the results revealed that ZLS restorations exhibit better mechanical properties compared to feldspathic, lithium disilicate, and hybrid ceramics or resin nanoceramic but worse properties compared to translucent or high-translucency zirconia.
- 3.
- For accurate adhesion between the ZLS ceramics and the resin cement, chemical or micromechanical retentions must be created in the inner surface of the restorations.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guess, P.C.; Schultheis, C.; Bonfante, E.A.; Coelho, P.G.; Ferencz, J.L.; Silva, N.R. All-Ceramic Systems: Laboratory and Clinical Performance. Dent. Clin. N. Am. 2011, 55, 333–352. [Google Scholar] [CrossRef] [PubMed]
- Awad, D.; Stawarczyk, B.; Liebermann, A.; Ilie, N. Translucency of esthetic dental restorative CAD/CAM materials and composite resins with respect to thickness and surface roughness. J. Prosthet. Dent. 2015, 113, 534–540. [Google Scholar] [CrossRef] [PubMed]
- Pieger, S.; Salman, A.; Bidra, A.S. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2014, 112, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Gunal, B.; Ulusoy, M.M. Optical properties of contemporary monolithic CAD-CAM restorative materials at different thick-nesses. J. Esthet. Restor. Dent. 2018, 30, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Sen, N.; Us, Y.O. Mechanical and optical properties of monolithic CAD-CAM restorative materials. J. Prosthet. Dent. 2018, 119, 593–599. [Google Scholar] [CrossRef] [PubMed]
- Al-Thobity, A.M.; Alsalman, A. Flexural properties of three lithium disilicate materials: An in vitro evaluation. Saudi Dent. J. 2021, 33, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, C.; Eckert, H.; Apel, E.; Rheinberger, V.M.; Höland, W. Phase evolution in lithium disilicate glass–ceramics based on non-stoichiometric compositions of a multi-component system: Structural studies by 29Si single and double resonance solid state NMR. Phys. Chem. Chem. Phys. 2011, 13, 4540–4551. [Google Scholar] [CrossRef]
- Vita Suprinity CAD/CAM Restorative. Vita Suprinity Brochure. Available online: https://www.vita-zahnfabrik.com/en/VITA-SUPRINITY-14036.html (accessed on 15 July 2023).
- Celtra® Duo, Dentsply Sirona. Guidelines for Processing Celtra Duo. Hanau-Wolfgang, Germany: Dentsply Sirona. 2018. Available online: https://www.dentsplysiro-na.com/content/dam/dentsply/pim/manufacturer/Prosthetics/Fixed/High_strength_glass_ceramic/Celtra_Duo/GA%20Celtra%20Duo%20Processing%20Guidelines%20eN.pdf) (accessed on 15 July 2023).
- Sorrentino, R.; Ruggiero, G.; Di Mauro, M.I.; Breschi, L.; Leuci, S.; Zarone, F. Optical behaviors, surface treatment, adhesion, and clinical indications of zirconia-reinforced lithium silicate (ZLS): A narrative review. J. Dent. 2021, 112, 103722. [Google Scholar] [CrossRef]
- AlHelal, A.A. Biomechanical behavior of all-ceramic endocrowns fabricated using CAD/CAM: A systematic review. J. Prosthodont. Res. 2023, 1–13. [Google Scholar] [CrossRef]
- De Melo Alencar, C.; Zaniboni, J.F.; Silva, A.M.; Ortiz, M.I.G.; Lima, D.A.N.L.; Alves de Campos, E. Impact of finishing pro-tocols on color stability of CAD/CAM ceramics: A Systematic Review. Int. J. Prosthodont. 2022, 35, 109–118. [Google Scholar] [CrossRef]
- de Carvalho Ramos, N.; Campos, T.M.; de La Paz, I.S.; Machado, J.P.; Bottino, M.A.; Cesar, P.F. Microstructure characterization and SCG of newly engineered dental ceramics. Dent. Mater. 2016, 32, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Baldissara, P.; Llukacej, A.; Ciocca, L.; Valandro, F.L.; Scotti, R. Translucency of zirconia copings made with different CAD/CAM systems. J. Prosthet. Dent. 2010, 104, 6–12. [Google Scholar] [CrossRef] [PubMed]
- Bahannan, S.A.; Awad, M.A. Effect of Porcelain Shade and Application Time on Shade Reproduction. J. Prosthodont. 2018, 27, 227–231. [Google Scholar] [CrossRef] [PubMed]
- Skyllouriotis, A.L.; Yamamoto, H.L.; Nathanson, D. Masking properties of ceramics for veneer restorations. J. Prosthet. Dent. 2017, 118, 517–523. [Google Scholar] [CrossRef] [PubMed]
- Harada, R.; Takemoto, S.; Hattori, M.; Yoshinari, M.; Oda, Y.; Kawada, E. The influence of colored zirconia on the optical properties of all-ceramic restorations. Dent. Mater. J. 2015, 34, 918–924. [Google Scholar] [CrossRef]
- Della Bona, A.; Nogueira, A.D.; Pecho, O. Optical properties of CAD–CAM ceramic systems. J. Dent. 2014, 42, 1202–1209. [Google Scholar] [CrossRef]
- Barão, V.A.R.; Gennari-Filho, H.; Goiato, M.C.; dos Santos, D.M.; Pesqueira, A.A. Factors to Achieve Aesthetics in All-Ceramic Restorations. J. Craniofacial Surg. 2010, 21, 2007–2012. [Google Scholar] [CrossRef]
- Jurisic, S.; Jurisic, G.; Zlataric, D.K. In vitro evaluation and comparison of the translucency of two different all-ceramic systems. Acta Stomatol. Croat. 2015, 49, 195–203. [Google Scholar] [CrossRef]
- Gonuldas, F.; Yılmaz, K.; Ozturk, C. The effect of repeated firings on the color change and surface roughness of dental ceramics. J. Adv. Prosthodont. 2014, 6, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Ragain, J.C. A Review of Color Science in Dentistry: The Process of Color Vision. J. Dent. Oral Disord. Ther. 2015, 3, 1–4. [Google Scholar] [CrossRef]
- Zum Gahr, K.H.; Bundschuh, W.; Zimmerlin, B. Effect of grain size of friction and sliding wear of oxide ceramics. Wear 1993, 162, 269–279. [Google Scholar] [CrossRef]
- He, Y.; Winnubst, L.; Burggraaf, A.J.; Verweij, H.; van der Varst, P.G.T.; de With, B. Grain-Size Dependence of Sliding Wear on Tetragonal Zirconia Polycrystals. J. Am. Ceram. Soc. 1996, 79, 3090–3096. [Google Scholar] [CrossRef]
- Gracis, S.; Thompson, V.P.; Ferencz, J.L.; Silva, N.R.F.A.; Bonfante, E.A. A New Classification System for All-Ceramic and Ceramic-like Restorative Materials. Int. J. Prosthodont. 2015, 28, 227–235. [Google Scholar] [CrossRef]
- Bajraktarova-Valjakova, E.; Korunoska-Stevkovska, V.; Kapusevska, B.; Gigovski, N.; Bajraktarova-Misevska, C.; Grozdanov, A. Contemporary Dental Ceramic Materials, A Review: Chemical Composition, Physical and Mechanical Properties, Indications for Use. J. Med Sci. 2018, 6, 1742–1755. [Google Scholar] [CrossRef]
- Belli, R.; Wendler, M.; de Ligny, D.; Cicconi, M.R.; Petschelt, A.; Peterlik, H.; Lohbauer, U. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent. Mater. 2017, 33, 84–98. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Correlation between ceramics translucency and polymerization efficiency through ceramics. Dent. Mater. 2008, 24, 908–914. [Google Scholar] [CrossRef]
- Yan, Z.; Xian, S.; Tan, T.; Lia, Y.; Yang, X. Influence of zirconia content on translucency of zirconia-toughened alumina glass-infiltrated ceramic. West China J. Stomatol. 2011, 29, 191–194. [Google Scholar]
- Subaşı, M.; Alp, G.; Johnston, W.; Yilmaz, B. Effect of thickness on optical properties of monolithic CAD-CAM ceramics. J. Dent. 2018, 71, 38–42. [Google Scholar] [CrossRef]
- Vichi, A.; Zhao, Z.; Paolone, G.; Scotti, N.; Mutahar, M.; Goracci, C.; Louca, C. Factory Crystallized Silicates for Monolithic Metal-Free Restorations: A Flexural Strength and Translucency Comparison Test. Materials 2022, 15, 7834. [Google Scholar] [CrossRef] [PubMed]
- Passos, L.; Linke, B.; Street, A.; Torrealba, Y. Effect of thickness, translucency, and firing protocol on the masking ability of a CAD/CAM zirconia-reinforced lithium silicate for different backgrounds. Int. J. Comp. Dent. 2019, 22, 29–38. [Google Scholar]
- Stawarczyk, B.; Sener, B.; Trottmann, A.; Roos, M.; Özcan, M.; Hämmerle, C.H.F. Discoloration of manually fabricated resins and industrially fabricated CAD/CAM blocks versus glass-ceramic: Effect of storage media, duration, and subsequent polishing. Dent. Mater. J. 2012, 31, 377–383. [Google Scholar] [CrossRef] [PubMed]
- Sarıkaya, I.; Hayran, Y. Effects of Polishing on Color Stability and Surface Roughness of CAD-CAM Ceramics. Meandros Med. Dent. J. 2018, 19, 153–159. [Google Scholar] [CrossRef]
- Aydın, N.; Karaoğlanoğlu, S.; Kılıçarslan, M. Investigating the color changes on resin-based CAD/CAM Blocks. J. Esthet. Restor. Dent. 2019, 32, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Arif, R.; Yilmaz, B.; Johnston, W. In vitro color stainability and relative translucency of CAD-CAM restorative materials used for laminate veneers and complete crowns. J. Prosthet. Dent. 2018, 122, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Kanat-Ertürk, B. Color Stability of CAD/CAM Ceramics Prepared with Different Surface Finishing Procedures. J. Prosthodont. 2019, 29, 166–172. [Google Scholar] [CrossRef]
- Al Moaleem, M.M.; Adawi, H.A.; Alsharif, K.F.; Alhazmi, H.A.; Alshahrani, F.A.; Abu Hadi, R.M.; Kara, R.; Muyidi, H.M.; Khalid, A.; Asiri, A.M.; et al. Impact of Smokeless Tobacco on the Color Stability of Zirconia, Zirco-nia-Reinforced Lithium Silicate and Feldspathic CAD/CAM Restorative Materials: An In Vitro Study. Coatings 2022, 12, 207. [Google Scholar] [CrossRef]
- Alp, G.; Subasi, M.G.; Johnston, W.; Yilmaz, B. Effect of surface treatments and coffee thermocycling on the color and trans-lucency of CAD-CAM monolithic glass-ceramic. J. Prosthet. Dent. 2017, 120, 263–268. [Google Scholar] [CrossRef]
- Demirel, M.; Diken Türksayar, A.A.; Donmez, M.B. Translucency, color stability, and biaxial flexural strength of advanced lithium disilicate ceramic after coffee thermocycling. J. Esthet. Restor. Dent. 2022, 35, 390–396. [Google Scholar] [CrossRef]
- Vasiliu, R.-D.; Porojan, S.D.; Bîrdeanu, M.I.; Porojan, L. Effect of Thermocycling, Surface Treatments and Microstructure on the Optical Properties and Roughness of CAD-CAM and Heat-Pressed Glass Ceramics. Materials 2020, 13, 381. [Google Scholar] [CrossRef] [PubMed]
- Donmez, M.B.; Olcay, E.O.; Demirel, M. Load-to-Failure Resistance and Optical Characteristics of Nano-Lithium Disilicate Ceramic after Different Aging Processes. Materials 2022, 15, 4011. [Google Scholar] [CrossRef] [PubMed]
- Akmak, G.; Donmez, M.; Kashkari, A.; Johnston, W.; Yilmaz, B. Effect of thickness, cement shade, and coffee thermocycling on the optical properties of zirconia-reinforced lithium silicate ceramic. J. Esthet. Restor. Dent. 2021, 33, 1132–1138. [Google Scholar]
- Choi, Y.S.; Kang, K.H.; Att, W. Evaluation of the response of esthetic restorative materials to ultraviolet aging. J. Prosthet. Dent. 2020, 126, 679–685. [Google Scholar] [CrossRef] [PubMed]
- Comba, A.; Paolone, G.; Baldi, A.; Vichi, A.; Goracci, C.; Bertozzi, G.; Scotti, N. Effects of Substrate and Cement Shade on the Translucency and Color of CAD/CAM Lithium-Disilicate and Zirconia Ceramic Materials. Polymers 2022, 14, 1778. [Google Scholar] [CrossRef] [PubMed]
- Spink, L.S.; Rungruanganut, P.; Megremis, S.; Kelly, J.R. Comparison of an absolute and surrogate measure of relative translu-cency in dental ceramics. Dent. Mater. 2013, 29, 702–707. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Pang, L.; Yao, J. The effects of firing numbers on the opening total pore volume, translucency parameter and color of dental all-ceramic systems. West China J. Stomatol. 2012, 30, 417–419. [Google Scholar]
- Yılmaz, K.; Gonuldas, F.; Ozturk, C. The effect of repeated firings on the color change of dental ceramics using different glazing methods. J. Adv. Prosthodont. 2014, 6, 427–433. [Google Scholar] [CrossRef]
- Dong-Dong, Q.; Lei, Z.; Xiaoping, L.; Wenli, C. Effect of repeated sintering on the color and translucency of dental lithium disilicate-based glass ceramic. West China J. Stomatol. 2015, 33, 50–53. [Google Scholar]
- Campanelli de Morais, D.; de Oliveira Abu-Izze, F.; Rivoli Rossi, N.; Gallo Oliani, M.; de Assunção E Souza, R.O.; de Siqueira Anzolini Saavedra, G.; Bottino, M.A.; Marques de Melo Marinho, R. Effect of Consecutive Firings on the Optical and Mechanical Properties of Silicate and Lithium Disilicate Based Glass-Ceramics. J. Prosthodont. 2021, 30, 776–782. [Google Scholar] [CrossRef]
- Nejatidanesh, F.; Azadbakht, K.; Savabi, O.; Sharifi, M.; Shirani, M. Effect of repeated firing on the translucency of CAD-CAM monolithic glass-ceramics. J. Prosthet. Dent. 2019, 123, 530.e1–530.e6. [Google Scholar] [CrossRef] [PubMed]
- Schweitzer, F.; Spintzyk, S.; Geis-Gerstorfer, J.; Huettig, F. Influence of minimal extended firing on dimensional, optical, and mechanical properties of crystalized zirconia-reinforced lithium silicate glass ceramic. J. Mech. Behav. Biomed. Mater. 2020, 104, 103644. [Google Scholar] [CrossRef] [PubMed]
- Aurélio, I.L.; Dorneles, L.S.; May, L.G. Extended glaze firing on ceramics for hard machining: Crack healing, residual stresses, optical and microstructural aspects. Dent. Mater. 2016, 33, 226–240. [Google Scholar] [CrossRef] [PubMed]
- Motro, P.F.; Kursoglu, P.; Kazazoglu, E. Effects of different surface treatments on stainability of ceramics. J. Prosthet. Dent. 2012, 108, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Yılmaz, C.; Korkmaz, T.; Demirköprülü, H.; Ergün, G.; Özkan, Y. Color Stability of Glazed and Polished Dental Porcelains. J. Prosthodont. 2008, 17, 20–24. [Google Scholar] [CrossRef] [PubMed]
- Ozen, F.; Demirkol, N.; Oz, O.P. Effect of surface finishing treatments on the color stability of CAD/CAM materials. J. Adv. Prosthodont. 2020, 12, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Elsaka, S.E.; Elnaghy, A.M. Mechanical properties of zirconia reinforced lithium silicate glass-ceramic. Dent. Mater. 2016, 32, 908–914. [Google Scholar] [CrossRef]
- Vasiliu, R.D.; Uțu, I.-D.; Rusu, L.; Boloș, A.; Porojan, L. Fractographic and Microhardness Evaluation of All-Ceramic Hot-Pressed and CAD/CAM Restorations after Hydrothermal Aging. Materials 2022, 15, 3987. [Google Scholar] [CrossRef]
- Guilardi, L.F.; Soares, P.; Werner, A.; de Jager, N.; Pereira, G.K.R.; Kleverlaan, C.J.; Rippe, M.P.; Valandro, L.F. Fatigue performance of distinct CAD/CAM dental ceramics. J. Mech. Behav. Biomed. Mater 2020, 103, 103540. [Google Scholar]
- Attar, E.A.; Aldharrab, A.; Ajaj, R. Flexural Strength Properties of Five Different Monolithic Computer-Aided De-sign/Computer-Aided Manufacturing Ceramic Materials: An In Vitro Study. Cureus 2023, 15, e36958. [Google Scholar]
- Abu-Izze, F.O.; Ramos, G.F.; Borges, A.L.S.; Anami, L.C.; Bottino, M.A. Fatigue behavior of ultrafine tabletop ceramic resto-rations. Dent. Mater. 2018, 34, 1401–1409. [Google Scholar] [CrossRef] [PubMed]
- Mendonca, A.F.; Shahmoradi, M.; Depes de Gouve, C.V.; De Souza, G.M.; Ellakwa, A. Microstructural and Mechanical Characterization of CAD/CAM Materials for Monolithic Dental Restorations. J. Prosthodont. 2018, 28, E587–E594. [Google Scholar]
- Bergamo, T.P.E.; Bordin, D.; Ramalho, I.S.; Lopes, A.C.O.; Gomesa, R.S.; Kaizer, M.; Witek, L.; Bonfante, E.A.; Coelho, P.G.; Cury, A.A.D.B. Zirconia-reinforced lithium silicate crowns: Effect of thickness on survival and failure mode. Dent. Mater. 2019, 35, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, J.B.; Riquieri, H.; Prochnow, C.; Guilardi, L.F.; Pereira, G.K.R.; Borges, A.L.S.; Marques de Melo Marinho, R.; Valandro, L.F. Fatigue failure load of two res-in-bonded zirconia-reinforced lithium silicate glass-ceramics: Effect of ceramic thickness. Dent. Mater. 2018, 34, 891–900. [Google Scholar] [CrossRef]
- Picolo, M.Z.; Kury, M.; Romario-Silva, D.; Rosalen, P.L.; Pecorari, V.G.A.; Gianinni, M.; Cavalli, V. Effects of gastric acid and me-chanical toothbrushing in CAD-CAM restorative materials: Mechanical properties, surface topography, and biofilm adhesion. J. Mech. Behav. Biomed. Mater. 2023, 138, 105606. [Google Scholar] [CrossRef] [PubMed]
- Cinar, S.; Altan, B.; Akgungor, G. Comparison of Bond Strength of Monolithic CAD-CAM Materials to Resin Cement Using Different Surface Treatment Methods. J. Adv. Oral Res. 2019, 10, 120–127. [Google Scholar] [CrossRef]
- Yavuz, T.; Dilber, E.; Kara, H.B.; Tuncdemir, A.R.; Ozturk, A.N. Effects of different surface treatments on shear bond strength in two different ceramic systems. Lasers Med. Sci. 2013, 28, 1233–1239. [Google Scholar] [CrossRef]
- Rinke, S.; RoÃdiger, M.; Ziebolz, D.; Schmidt, A.-K. Fabrication of Zirconia-Reinforced Lithium Silicate Ceramic Restorations Using a Complete Digital Workflow. Case Rep. Dent. 2015, 2015, 162178. [Google Scholar] [CrossRef]
- Altan, B.; Cınar, S.; Tuncelli, B. Evaluation of shear bond strength of zirconia-based monolithic CAD-CAM materials to resin cement after different surface treatments. Niger. J. Clin. Pract. 2019, 22, 1475–1482. [Google Scholar] [CrossRef]
- Blatz, M.B.; Sadan, A.; Kern, M. Resin-ceramic bonding: A review of the literature. J. Prosthet. Dent. 2003, 89, 268–274. [Google Scholar] [CrossRef]
- Maawadh, A.; Alayad, A.; Almohareb, T.; Alsulami, R.; Alosaimi, R.; Alromi, F.; Alhalees, S. The Effect of Different Hydrofluoric Acid Etching Times on The Bond Strength of Zirconia Reinforced Lithium Silicate Glass Ceramics. Biomaterials. Med. Devices 2021, 25, 42–48. [Google Scholar]
- Ataol, A.S.; Ergun, G. Effects of surface treatments on repair bond strength of a new CAD/CAM ZLS glass ceramic and two different types of CAD/CAM ceramics. J. Oral Sci. 2018, 60, 201–211. [Google Scholar] [CrossRef] [PubMed]
- Fonseca, R.G.; Haneda, I.G.; Almeida-Júnior, A.A.; de Oliveira Abi-Rached, F.; Adabo, G.L. Efficacy of Air-abrasion Technique and Additional Surface Treatment at Titanium/Resin Cement Interface. J. Adhes. Dent. 2012, 14, 453–459. [Google Scholar] [PubMed]
- Kim, B.K.; Bae, H.E.K.; Shim, J.-S.; Lee, K.W. The influence of ceramic surface treatments on the tensile bond strength of composite resin to all-ceramic coping materials. J. Prosthet. Dent. 2005, 94, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Aladağ, S.U.; Ayaz, E.A. Repair bond strength of different CAD-CAM ceramics after various surface treatments combined with laser irradiation. Lasers Med. Sci. 2023, 38, 51. [Google Scholar] [CrossRef] [PubMed]
- Azevedo, V.L.B.; de Castro, E.F.; Bonvent, J.J.; Scopin de Andrade, O.; Nascimento, F.D.; Gianni, M.; Cavalli, V. Surface treatments on CAD/CAM glass– ceramics: Influence on roughness, topography, and bond strength. J. Esthet. Restor. Dent. 2021, 33, 739–749. [Google Scholar] [CrossRef]
- Tribst, J.; Anami, L.C.; Özcan, M.; Bottino, M.; Melo, R.; Saavedra, G. Self-etching Primers vs Acid Conditioning: Impact on Bond Strength Between Ceramics and Resin Cement. Oper. Dent. 2018, 43, 372–379. [Google Scholar] [CrossRef]
- Honda, M.I.; Florio, F.M.; Basting, R.T. Effectiveness of indirect composite resin silanization evaluated by microtensile bond strength test. Am. J. Dent. 2008, 21, 153–158. [Google Scholar]
- Weyhrauch, M.; Igiel, C.; Scheller, H.; Weibrich, G.; Lehmann, K.M. Fracture Strength of Monolithic All-Ceramic Crowns on Titanium Implant Abutments. Quintessence Publ. 2016, 31, 304–309. [Google Scholar] [CrossRef]
- Sevmez, H.; Yilmaz, H. Comparison of The Effect of Surface Conditioning Methods on The Bond Strength of Different Zirconia Reinforced Lithium Silicate and Hybrid Ceramics to Resin Cement. Clin. Exp. Health Sci. 2021, 11, 554–563. [Google Scholar] [CrossRef]
- Secilmis, A.; Ustun, O.; Buyukhatipoglu, I.K. Evaluation of the shear bond strength of two resin cements on different CAD/CAM materials. J. Adhes. Sci. Technol. 2016, 30, 983–993. [Google Scholar] [CrossRef]
- Traini, T.; Sinjari, B.; Pascetta, R.; Serafini, N.; Perfetti, G.; Trisi, P.; Caputi, S. The zirconia-reinforced lithium silicate ceramic: Lights and shadows of a new material. Dent. Mater. J. 2016, 35, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Donmez, M.B.; Okutan, Y.; Yucel, M.T. Effect of prolonged application of single-step self-etching primer and hydrofluoric acid on the surface roughness and shear bond strength of CAD/CAM materials. Eur. J. Oral Sci. 2020, 128, 542–549. [Google Scholar] [CrossRef] [PubMed]
- Al-Thagafi, R.; Al-Zordk, W.; Saker, S. Influence of Surface Conditioning Protocols on Reparability of CAD/CAM Zirco-nia-reinforced Lithium Silicate Ceramic. J. Adhes. Dent. 2016, 18, 135–141. [Google Scholar] [PubMed]
- Pucci, J.; Dal Picolo, M.Z.; Brasil, I.; Giannini, M.; Cavalli, V. Influence of surface treatment and ageing on the bond strength of resin cement to hybrid and glass-ceramic CAD/CAM materials. Prim. Dent. J. 2022, 11, 78–85. [Google Scholar] [CrossRef]
- Elsaka, S.E. Bond strength of novel CAD/CAM restorative materials to self-adhesive resin cement: The effect of surface treat-ments. J. Adhes. Dent. 2014, 16, 531–540. [Google Scholar] [PubMed]
- Okutan, Y.; Kandemir, B.; Donmez, M.B.; Yucel, M.T. Effect of the thickness of CAD-CAM materials on the shear bond strength of light-polymerized resin cement. Eur. J. Oral Sci. 2022, 130, e12892. [Google Scholar] [CrossRef]
- Preis, V.; Behr, M.; Hahnel, S.; Rosentritt, M. Influence of cementation on in vitro performance, marginal adaptation and fracture resistance of CAD/CAM-fabricated ZLS molar crowns. Dent. Mater. 2015, 31, 1363–1369. [Google Scholar] [CrossRef]
- Falahchai, M.; Babaee Hemmati, Y.; Neshandar Asli, H.; Asli, M.N. Marginal adaptation of zirconia-reinforced lithium silicate overlays with different preparation designs. J. Esthet. Restor. Dent. 2020, 32, 823–830. [Google Scholar] [CrossRef]
- McLean, J.W.; von Fraunhofer, J.A. The estimation of cement film thickness by an in vivo technique. Br. Dent. J. 1971, 131, 107–111. [Google Scholar] [CrossRef]
- Kim, D.-Y.; Kim, J.-H.; Kim, H.-Y.; Kim, W.-C. Comparison and evaluation of marginal and internal gaps in cobalt–chromium alloy copings fabricated using subtractive and additive manufacturing. J. Prosthodont. Res. 2018, 62, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Amini, A.; Zeighami, S.; Ghodsi, S. Comparison of Marginal and Internal Adaptation in Endocrowns Milled from Translucent Zirconia and Zirconium Lithium Silicate. Int. J. Dent. 2021, 2021, 1544067. [Google Scholar] [CrossRef] [PubMed]
- Vasiliu, R.-D.; Porojan, S.D.; Porojan, L. In Vitro Study of Comparative Evaluation of Marginal and Internal Fit between Heat-Pressed and CAD-CAM Monolithic Glass-Ceramic Restorations after Thermal Aging. Materials 2020, 13, 4239. [Google Scholar] [CrossRef] [PubMed]
- Taha, D.; Spintzyk, S.; Sabet, A.; Wahsh, M.; Salah, T. Assessment of marginal adaptation and fracture resistance of endocrown restorations utilizing different machinable blocks subjected to thermomechanical aging. J. Esthet. Restor. Dent. 2018, 30, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Alves, M.D.; Cadore-Rodrigues, A.C.; Prochnow, C.; de Lima Burgo, A.; Spazzin, A.O.; Bacchi, A.; Valandro, L.F.; Rocha Pereira, G.K. Fatigue performance of adhesively luted glass or polycrystalline CAD-CAM monolithic crowns. J. Prosthet. Dent. 2020, 126, 119–127. [Google Scholar] [CrossRef] [PubMed]
- Sahebi, M.; Ghodsi, S.; Berahman, P.; Amini, A.; Zeighami, S. Comparison of retention and fracture load of endocrowns made from zirconia and zirconium lithium silicate after aging: An in vitro study. BMC Oral Health 2022, 22, 41. [Google Scholar] [CrossRef] [PubMed]
- Rinke, S.; Brandt, A.; Hausdoerfer, T.; Leha, A.; Ziebolz, D. Clinical Evaluation of Chairside-Fabricated Partial Crowns Made of Zirconia-Reinforced Lithium Silicate Ceramic—2-Year-Results. Eur. J. Prosthodont. Restor. Dent. 2020, 28, 36–42. [Google Scholar] [CrossRef]
- Rinke, S.; Pfitzenreuter, T.; Leha, A.; Roediger, M.; Ziebolz, D. Clinical evaluation of chairside-fabricated partial crowns composed of zirconia-reinforced lithium silicate ceramics: 3-year results of a prospective practice-based study. J. Esthet. Restor. Dent. 2019, 32, 226–235. [Google Scholar] [CrossRef]
- Rinke, S.; Zuck, T.; Hausdörfer, T.; Leha, A.; Wassmann, T.; Ziebolz, D. Prospective clinical evaluation of chairside-fabricated zirconia-reinforced lithium silicate ceramic partial crowns—5-year results. Clin. Oral Investig. 2022, 26, 1593–1603. [Google Scholar] [CrossRef]
- Kui, A.; Popescu, C.; Labuneț, A.; Almășan, O.; Petruțiu, A.; Păcurar, M.; Buduru, S. Is Teledentistry a Method for Optimizing Dental Practice, Even in the Post-Pandemic Period? An Integrative Review. Int. J. Environ. Res. Public Health 2022, 19, 7609. [Google Scholar] [CrossRef]
| Search Terms and Combinations | |
|---|---|
| PubMed | “zirconia reinforced lithium silicate ceramic*”[tw] OR “zirconia reinforced lithium silicate glass-ceramic*”[tw] OR “ZLS”[tw] AND “Computer-Aided Design”[Mesh] OR “CAD-CAM*”[tw] AND “Optical Phenomena”[Mesh] OR “color*”[tw] OR “optical property*”[tw] OR “light scattering”[tw] OR “light transmission”[tw] |
| “zirconia reinforced lithium silicate ceramic*”[tw] OR “zirconia reinforced lithium silicate glass-ceramic*”[tw] OR “ZLS”[tw] AND “Computer-Aided Design”[Mesh] OR “CAD-CAM*”[tw] AND “Mechanical Phenomena”[Mesh] AND “Flexural Strength”[Mesh] AND “Mechanical Tests”[Mesh] OR “mechanical performance”[tw] OR “flexural strength”[tw] OR “fatigue failure load”[tw] OR “surface hardness”[tw] OR “Young’s modulus”[tw] | |
| “zirconia reinforced lithium silicate ceramic*”[tw] OR “zirconia reinforced lithium silicate glass-ceramic*”[tw] OR “ZLS”[tw] AND “Computer-Aided Design”[Mesh] OR “CAD-CAM*”[tw] AND “Dental Bonding”[Mesh] AND “Acid Etching, Dental”[Mesh] OR “adhesion*”[tw] OR “surface treatment”[tw] OR “cementation*”[tw] | |
| “zirconia reinforced lithium silicate ceramic*”[tw] OR “zirconia reinforced lithium silicate glass-ceramic*”[tw] OR “ZLS”[tw] AND “Computer-Aided Design”[Mesh] OR “CAD-CAM*”[tw] AND “Clinical indication*”[tw] OR “Performances”[tw] | |
| Web of Science | “zirconia reinforced lithium silicate ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “Optical Phenomena” OR “color” OR “optical property” OR “light scattering” OR “light transmission” |
| “zirconia reinforced lithium silicate ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “Mechanical Phenomena” AND “Flexural Strength” AND “Mechanical Tests” OR “mechanical performance” OR “flexural strength” OR “fatigue failure load” OR “surface hardness” OR “Young’s modulus” | |
| “zirconia reinforced lithium silicate ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “Dental Bonding” AND “Acid Etching, Dental” OR “adhesion” OR “surface treatment” OR “cementation” | |
| “zirconia reinforced lithium silicate ceramic” OR “zirconia reinforced lithium silicate glass-ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “Clinical indication” OR “Performances” | |
| Cochrane Library | “zirconia reinforced lithium silicate ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND OR “color” OR “optical property” OR “light transmission” |
| “zirconia reinforced lithium silicate ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “flexural strength” OR “fatigue failure load” OR “surface hardness” OR “Young’s modulus” | |
| “zirconia reinforced lithium silicate ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “Acid Etching” OR “adhesion” OR “surface treatment” OR “cementation” | |
| “zirconia reinforced lithium silicate ceramic” OR “zirconia reinforced lithium silicate glass-ceramic” OR “ZLS” AND “Computer-Aided Design” OR “CAD-CAM” AND “Clinical indication” OR “Performances” | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manziuc, M.; Kui, A.; Chisnoiu, A.; Labuneț, A.; Negucioiu, M.; Ispas, A.; Buduru, S. Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding. Medicina 2023, 59, 2135. https://doi.org/10.3390/medicina59122135
Manziuc M, Kui A, Chisnoiu A, Labuneț A, Negucioiu M, Ispas A, Buduru S. Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding. Medicina. 2023; 59(12):2135. https://doi.org/10.3390/medicina59122135
Chicago/Turabian StyleManziuc, Manuela, Andreea Kui, Andrea Chisnoiu, Anca Labuneț, Marius Negucioiu, Ana Ispas, and Smaranda Buduru. 2023. "Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding" Medicina 59, no. 12: 2135. https://doi.org/10.3390/medicina59122135
APA StyleManziuc, M., Kui, A., Chisnoiu, A., Labuneț, A., Negucioiu, M., Ispas, A., & Buduru, S. (2023). Zirconia-Reinforced Lithium Silicate Ceramic in Digital Dentistry: A Comprehensive Literature Review of Our Current Understanding. Medicina, 59(12), 2135. https://doi.org/10.3390/medicina59122135









