Occupational Exposure of Employees in a Multispecialty Hospital to Factors Causing Contact Dermatitis—A Questionnaire Study
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- EU-OSHA—European Agency for Safety and Health at Work. Skin Diseases and Dermal Exposure: Policy and Practice Overview. 2008. Available online: https://osha.europa.eu/en/publications/report-skin-diseases-and-dermal-exposure-policy-and-practice-overview (accessed on 3 February 2021).
- Doryńska, A.; Śpiewak, R. Epidemiology of skin diseases from the spectrum of dermatitis and eczema. Malays. J. Dermatol. 2012, 29, 1–11. [Google Scholar]
- Schäfer, T.; Nienhaus, A.; Vieluf, D.; Berger, J.; Ring, J. Epidemiology of acne in the general population: The risk of smoking. Br. J. Dermatol. 2001, 145, 100–104. [Google Scholar] [CrossRef] [PubMed]
- Śpiewak, R. Częstość występowania chorób skóry w losowej grupie dorosłych Polaków. Estetologia Med. Kosmetol. 2012, 2, 50–53. [Google Scholar] [CrossRef]
- Ibler, K.S.; Jemec, G.B.; Garvey, L.H.; Agner, T. Prevalence of delayed-type and immediate-type hypersensitivity in healthcare workers with hand eczema. Contact Dermat. 2016, 75, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Prodi, A.; Rui, F.; Fortina, A.B.; Corradin, M.T.; Filon, F.L. Healthcare workers and skin sensitization: North-eastern Italian database. Occup. Med. 2016, 66, 72–74. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schwensen, J.F.; Menné, T.; Sommerlund, M.; Andersen, K.E.; Mortz, C.G.; Zachariae, C.; Johansen, J.D. Contact Allergy in Danish Healthcare Workers: A Retrospective Matched Case-control Study. Acta Derm. Venereol. 2016, 96, 237–240. [Google Scholar] [CrossRef] [PubMed]
- Turjanmaa, K. Incidence of immediate allergy to latex gloves in hospital personnel. Contact Dermat. 1987, 17, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Spiewak, R.; Moed, H.; Von Blomberg, B.M.E.; Bruynzeel, D.P.; Scheper, R.J.; Gibbs, S.; Rustemeyer, T. Allergic contact dermatitis to nickel: Modified in vitro test protocols for better detection of allergen-specific response. Contact Dermat. 2007, 56, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Drozdowska, A.; Drozdowski, P.; Jaworski, A.; Bula, D.; Adamczyk, D.; Reich, A. The novel questionnaire assessing occupational exposure to the risk factors of contact allergy among health professionals. Adv. Dermatol. Allergol. 2023, 40, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Machovcová, A.; Fenclová, Z.; Pelclová, D. Occupational skin diseases in Czech healthcare workers from 1997 to 2009. Int. Arch. Occup. Environ. Health 2013, 86, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Opstrup, M.S.; Johansen, J.D.; Zachariae, C.; Garvey, L.H. Contact allergy to chlorhexidine in a tertiary dermatology clinic in Denmark. Contact Dermat. 2016, 74, 29–36. [Google Scholar] [CrossRef] [PubMed]
- Tramontana, M.; Bianchi, L.; Hansel, K.; Agostinelli, D.; Stingeni, L. Nickel Allergy: Epidemiology, Pathomechanism, Clinical Patterns, Treatment and Prevention Programs. Endocr. Metab. Immune Disord. Drug Targets 2020, 20, 992–1002. [Google Scholar] [CrossRef] [PubMed]
- Elves, M.W.; Wilson, J.N.; Scales, J.T.; Kemp, H.B. Incidence of metal sensitivity in patients with total joint replacements. Br. Med. J. 1975, 4, 376–378. [Google Scholar] [CrossRef] [PubMed]
- Wakkers-Garritsen, B.G.; Nater, J.P. Patch tests in hip prosthesis rejection. Contact Dermat. 1975, 1, 254–255. [Google Scholar] [CrossRef] [PubMed]
- Munro-Ashman, D.; Miller, A.J. Rejection of metal to metal prosthesis and skin sensitivity to cobalt. Contact Dermat. 1976, 2, 65–67. [Google Scholar] [CrossRef] [PubMed]
| Item | Questions | Scoring |
|---|---|---|
| Do these phenomena occur in the workplace? | If “Yes”, circle the point | |
| 1. | Soaking hands | 1 |
| 2. | Exposure to detergents | 1 |
| 3. | Exposure to chemical disinfectants | 1 |
| 4. | Exposure to chemotherapeutics | 1 |
| 5. | Exposure to chemical reagents | 1 |
| 6. | Exposure to other chemicals | 1 |
| If yes please specify: | ||
| 7. | Wearing gloves (any type)? | 1 |
| 8. | Wearing latex gloves? | 1 |
| 9. | Wearing vinyl gloves? | 1 |
| 10. | Wearing powdered gloves? | 1 |
| 11. | Was personal protective equipment used? | 1 |
| 12. | Was there a rotation of employees at work positions? | 1 |
| 13. | Does the location of lesions correspond to occupational exposure? | 1 |
| 14. | Do the symptoms subside after days off work? | 1 |
| 15. | Do similar lesions occur in other employees in the same position in company? | 1 |
| If the skin symptoms occur, are they accompanied by: | ||
| 16. | Nasal discharge? | 1 |
| 17. | Tearing, burning, redness of the eyes? | 1 |
| 18. | Dyspnoea? | 1 |
| 19. | Eczema? | 1 |
| 20. | If yes, please specify the frequency of eczema occurrence | |
| Occasionally | 0.25 | |
| Regularly, but less than once a month | 0.5 | |
| Regularly, at least once a week | 0.75 | |
| Regularly, at last once a week, but the lesions cease after a weekend or a break from work | 1 | |
| Are there tendencies for the following skin lesions? | 1 | |
| 21. | Erythema? | 1 |
| 22. | Exfoliation? | 1 |
| 23. | Fissures? | 1 |
| 24. | Erosions? | 1 |
| 25. | Hyperkeratosis? | 1 |
| 26. | Dryness of the skin/lichenification? | 1 |
| 27. | Blisters? | 1 |
| 28. | Ulcers? | 1 |
| 29. | Burning and/or sore skin? | 1 |
| 30. | Pruritus? | 1 |
| 31. | Have you been diagnosed with atopic dermatitis? | 1 |
| 32. | Have you been diagnosed with psoriasis? | 1 |
| 33. | Have you been diagnosed with vitiligo? | 1 |
| 34. | Are there any other skin diseases? | 1 |
| If yes, please specify: | ||
| 35. | Are the lesions spreading outside the place of exposure? | 1 |
| 36. | Is the onset of the lesions sudden? | 1 |
| 37. | Do symptoms occur 24–72 h after exposure? | 1 |
| 38. | Have you been diagnosed with bronchial asthma? | 1 |
| 39. | Were patch tests performed? | 1 |
| 40. | Have any other diseases been diagnosed? | 1 |
| If yes, please specify: | 1 | |
| 41. | Have the following treatments been used?—systemic steroids, local steroids, calcineurin inhibitors, phototherapy | 1 |
| 42. | Were any measures that help to restore the epidermal barrier used? | 1 |
| 43. | Do symptoms occur after additional exposure to another irritant such as solar radiation? | 1 |
| If yes, please specify after what period of time: | ||
| 44. | The most frequently affected area of the body | 1, if hands |
| Are there tendencies for the following symptoms occurrence? | ||
| 45. | Dryness of skin | 1 |
| 46. | Excessive activity of the sebaceous glands (Seborrhea) | 1 |
| 47. | Excessive sweating | 1 |
| 48. | Excessive pigmentation | 1 |
| 49. | Frequency of burning and painfulness: | |
| Occasionally | 0.25 | |
| Regularly, but less than once a month | 0.5 | |
| Regularly, at least once a week | 0.75 | |
| Regularly, at least once a week, but the lesions cease after a weekend or a break from work | 1 | |
| Total score | ||
| Item | Questions | Scoring (Points Awarded for an Affirmative Answer) |
|---|---|---|
| 1. | Do the symptoms subside after days off work? | 1 |
| 2. | Do similar lesions occur in other employees in the same position in the company? | 1 |
| If the skin symptoms occur are they accompanied by: | ||
| 3. | Nasal discharge | 1 |
| 4. | Tearing, burning, redness of the eyes | 1 |
| 5. | Eczema | 1 |
| 6. | If yes, please specify the frequency of eczema occurrence | |
| Occasionally | 0.25 | |
| Regularly, but less than once a month | 0.5 | |
| Regularly, at least once a week | 0.75 | |
| Regularly, at least once a week, but the lesions cease after a weekend or a break from work | 1 | |
| 7. | Erythema | 1 |
| 8. | Dryness and/or lichenification | 1 |
| 9. | Burning and/or sore skin | 1 |
| 10. | Frequency of skin burning and/or painfulness | |
| Occasionally | 0.25 | |
| Regularly, but less than once a month | 0.5 | |
| Regularly, at least once a week | 0.75 | |
| Regularly, at least once a week, but the lesions cease after a weekend or a break from work | 1 | |
| 11. | Pruritus | 1 |
| 12. | Is the onset of the lesions sudden? | 1 |
| 13. | Do symptoms occur 24–72 h after exposure? | 1 |
| 14. | Have any measures that help to restore the epidermal barrier been used? | 1 |
| 15. | Any area of the body affected | 1 |
| 16. | Dryness of the skin | 1 |
| Total score: | ||
| Item | Questions | “Yes” n (%) |
|---|---|---|
| 1. | Do the symptoms subside after days off work? | 94 (40.9) |
| 2. | Do similar lesions occur in other employees in the same position in company? | 75 (32.6) |
| If the skin symptoms occur are they accompanied by: | ||
| 3. | Nasal discharge | 65 (28.3) |
| 4. | Tearing, burning, redness of the eyes | 98 (42.6) |
| 5. | Eczema | 138 (60.0) |
| 6. | If yes, please specify the frequency of eczema occurrence | |
| Occasionally | 62 (27.0) | |
| Regularly, but less than once a month | 19 (8.3) | |
| Regularly at least once a week | 17 (7.4) | |
| Regularly at least once a week, but the lesions cease after a weekend or a break from work | 40 (17.4) | |
| 7. | Erythema | 62 (27.0) |
| 8. | Dryness and/or lichenification | 112 (48.7) |
| 9. | Burning and/or sore skin | 50 (21.7) |
| 10. | Frequency of skin burning and/or painfulness | |
| Occasionally | 45 (19.6) | |
| Regularly, but less than once a month | 18 (7.8) | |
| Regularly, at least once a week | 15 (6.5) | |
| Regularly, at least once a week, but the lesions cease after a weekend or a break from work | 31 (31.5) | |
| 11. | Pruritus | 92 (40.0) |
| 12. | Is the onset of the lesions sudden? | 71 (30.9) |
| 13. | Do symptoms occur 24–72 h after exposure? | 57 (24.8) |
| 14. | Have any measures that help to restore the epidermal barrier been used? | 46 (20.0) |
| 15. | Any area of the body affected | 103 (44.8) |
| 16. | Dryness of the skin | 126 (54.8) |
| Total score: | ||
| Item | Position | p Test Score | |||
|---|---|---|---|---|---|
| Physicians N = 21 (%) | Nurses N = 162 (%) | Analytics N = 17 (%) | Others N = 30 (%) | ||
| 1. Do the symptoms subside after days off work? | 4 (19.0) | 76 (46.9) | 7 (41.2) | 7 (23.3) | 0.015 |
| 2. Do similar lesions occur in other employees in the same position in company? | 3 (14.3) | 66 (40.7) | 3 (17.6) | 3 (10.0) | <0.001 |
| 3. Nasal discharge | 3 (14.3) | 46 (28.4) | 6 (35.3) | 10 (33.3%) | 0.42 |
| 4. Tearing, Burning, Redness of the eyes | 4 (19.0) | 72 (44.4) | 9 (52.9) | 13 (43.3) | 0.125 |
| 5. Eczema occurs | 11 (52.4) | 100 (61.7) | 12 (70.6) | 15 (50.0) | - |
| 6. Frequency of eczema’s occurrence | 0.523 | ||||
| Does not occur | 10 (47.6) | 62 (38.3) | 5 (29.4) | 15 (50.0) | |
| Occasionally | 5 (23.8) | 41 (25.3) | 7 (41.2) | 9 (30.0) | |
| Regularly, but less than once a month | 2 (9.5) | 13 (8.0) | 3 (17.6) | 1 (3.3) | |
| Regularly, at least once a week | 1 (4.8) | 13 (8.0) | 0 (0.0) | 3 (10.0) | |
| Regularly, at least once a week, but the lesions cease after a weekend or break from work | 3 (14.3) | 33 (20.4) | 2 (11.8) | 2 (6.7) | |
| 7. Erythema | 8 (38.1) | 41 (25.3) | 5 (29.4) | 8 (26.7) | 0.659 |
| 8. Dryness, lichenification | 9 (42.9) | 83 (51.2) | 8 (47.1) | 12 (40.0) | 0.652 |
| 9. Burning and/or sore skin | 4 (19.0) | 35 (21.6) | 5 (29.4) | 6 (20.0) | 0.865 |
| 10. If any of the above occurs please specify, with what frequency? | 0.875 | ||||
| Does not occur | 10 (47.6) | 85 (52.5) | 8 (47.1) | 18 (60.0) | |
| Occasionally | 5 (23.8) | 29 (17.9) | 5 (29.4) | 6 (20.0) | |
| Regularly, but less than once a month | 2 (9.5) | 13 (8.0) | 2 (11.8) | 1 (3.3) | |
| Regularly, at least once a week | 2 (9.5) | 10 (6.2) | 0 (0.0) | 3 (10.0) | |
| Regularly, at least once a week, but the lesions cease after a break from work | 2 (9.5) | 25 (15.4) | 2 (11.8) | 2 (6.7) | |
| 11. Pruritus | 10 (47.6) | 62 (38.3) | 8 (47.1) | 12 (40.0) | 0.786 |
| 12. Is the onset of the lesions sudden | 6 (28.6) | 54 (33.3) | 4 (23.5) | 7 (23.3) | 0.628 |
| 13. Do symptoms occur 24–72 h after exposure? | 5 (23.8) | 44 (27.2) | 4 (23.5) | 4 (13.3) | 0.453 |
| 14. Were any measures that help to restore the epidermal barrier used? | 5 (23.8) | 32 (19.8) | 6 (35.3) | 3 (10.0) | 0.207 |
| 15. Any area of the body affected | 10 (47.6) | 75 (46.3) | 8 (47.1) | 10 (33.3) | 0.605 |
| 16. Dryness of skin | 11 (52.4) | 91 (56.2) | 10 (58.8) | 14 (46.7) | 0.781 |
| Variable | Female N = 203 | Male N = 27 | p Test Score |
|---|---|---|---|
| OSDES (score) | |||
| M ± SD | 6.2 ± 4.7 | 2.7 ± 4.2 | <0.001 |
| Me [Q1;Q3] | 7 [1; 10] | 0 [0; 6] | |
| Min–Max | 0–16 | 0–13 | |
| OSDES-16 | |||
| Low level | 71 (35.0) | 20 (74.1) | <0.001 |
| Average level | 41 (20.2) | 2 (7.4) | |
| High level | 91 (44.8) | 5 (18.5) | |
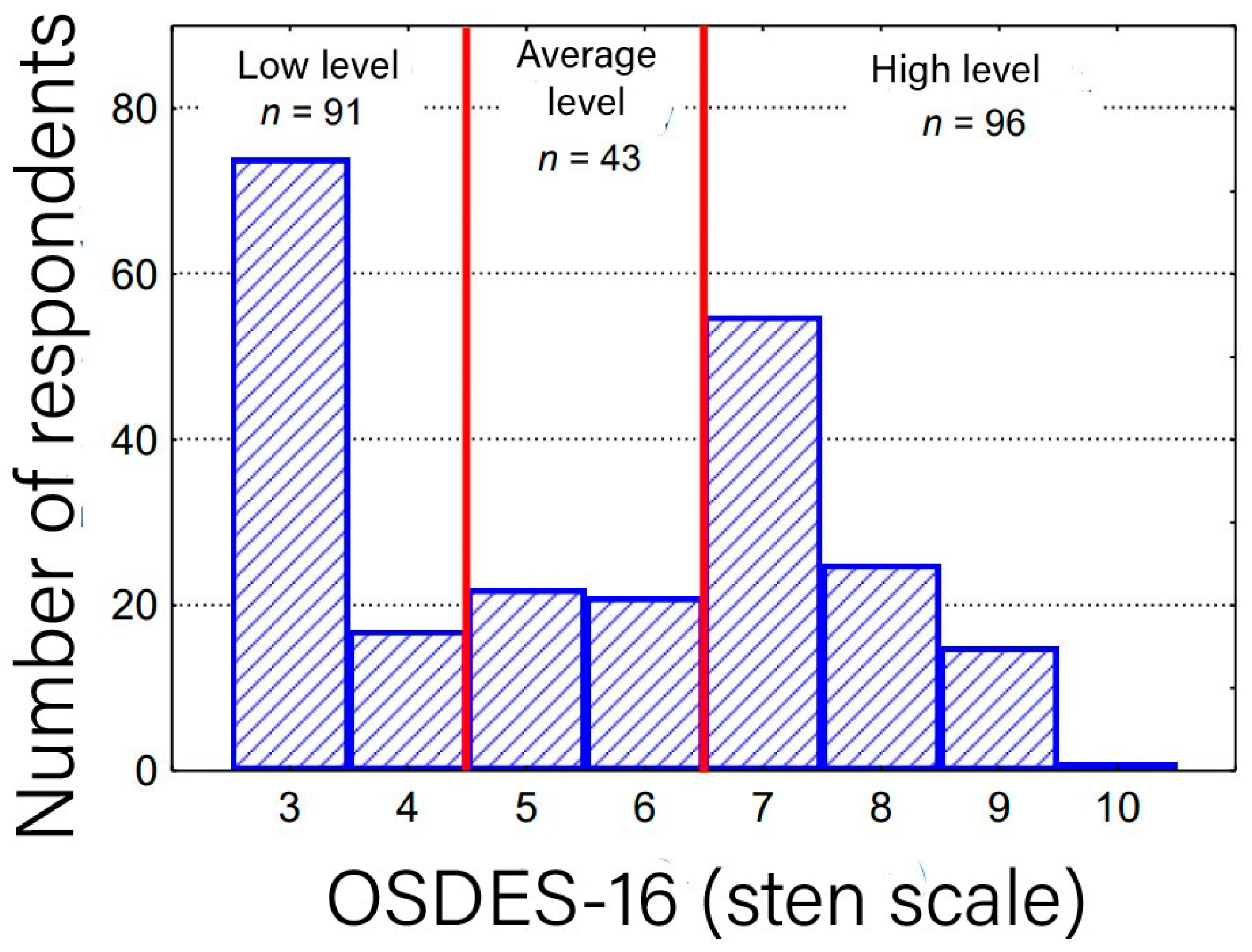
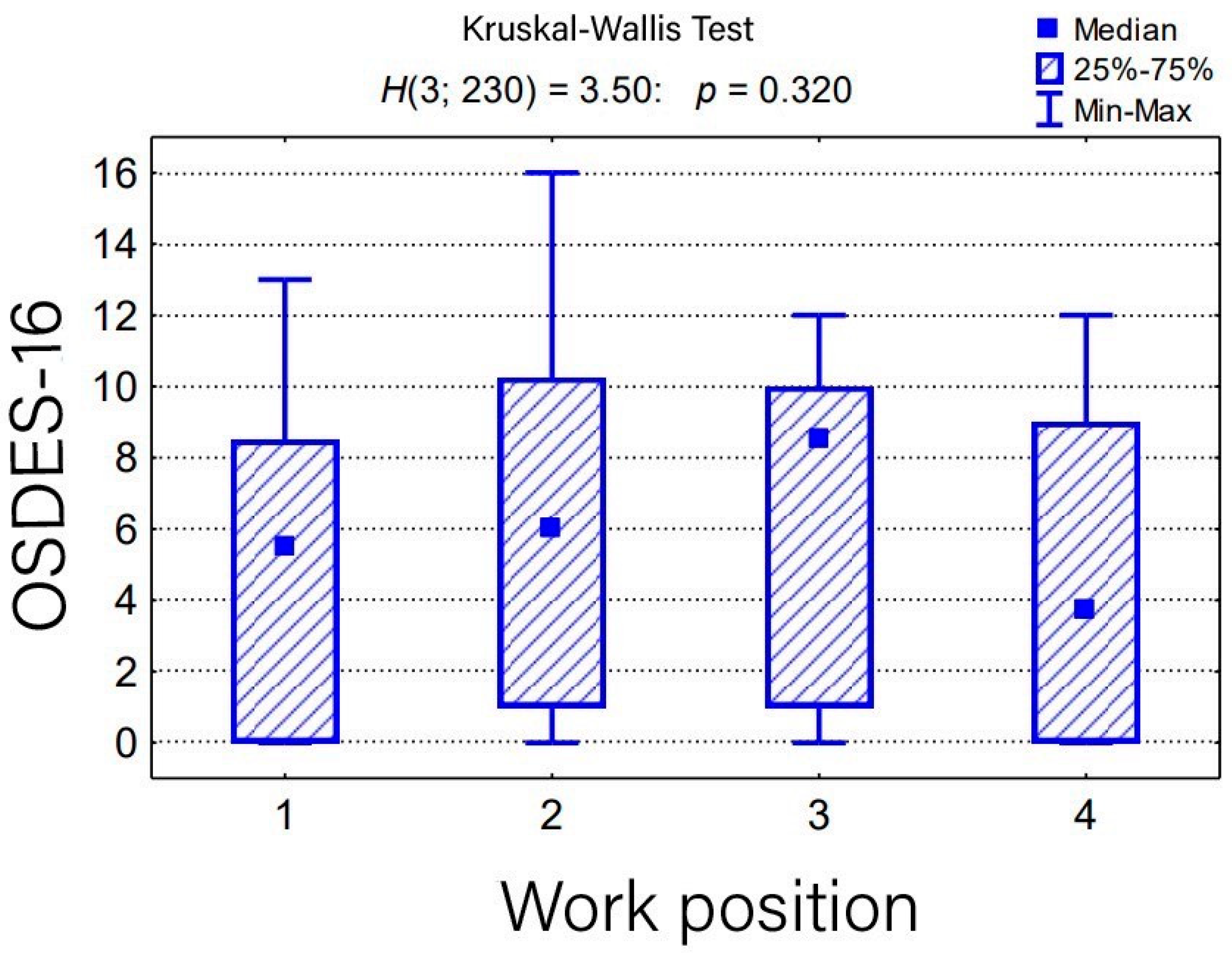
| The Level of Exposure | Position | p Test Score | |||
|---|---|---|---|---|---|
| Physicians N = 21 (%) | Nurses N = 162 (%) | Analytics N = 17 (%) | Others N = 30 (%) | ||
| OSDES-16 score | 0.32 | ||||
| M ± SD | 5.0 ± 4.3 | 6.1 ± 4.9 | 6.1 ± 4.6 | 4.6 ± 4.4 | |
| Me [Q1; Q3] | 6 [0; 9] | 6 [1; 10] | 9 [1; 10] | 4 [0; 9] | |
| Min–Max | 0–13 | 0–16 | 0–12 | 0–12 | |
| OSDES-16 scale rating | 0.78 | ||||
| Low level | 9 (42.9) | 62 (38.3) | 5 (29.4) | 15 (50.0) | |
| Average level | 5 (23.8) | 30 (18.5) | 3 (17.6) | 5 (16.7) | |
| High level | 7 (33.3) | 70 (43.2) | 9 (52.9) | 10 (33.3) | |
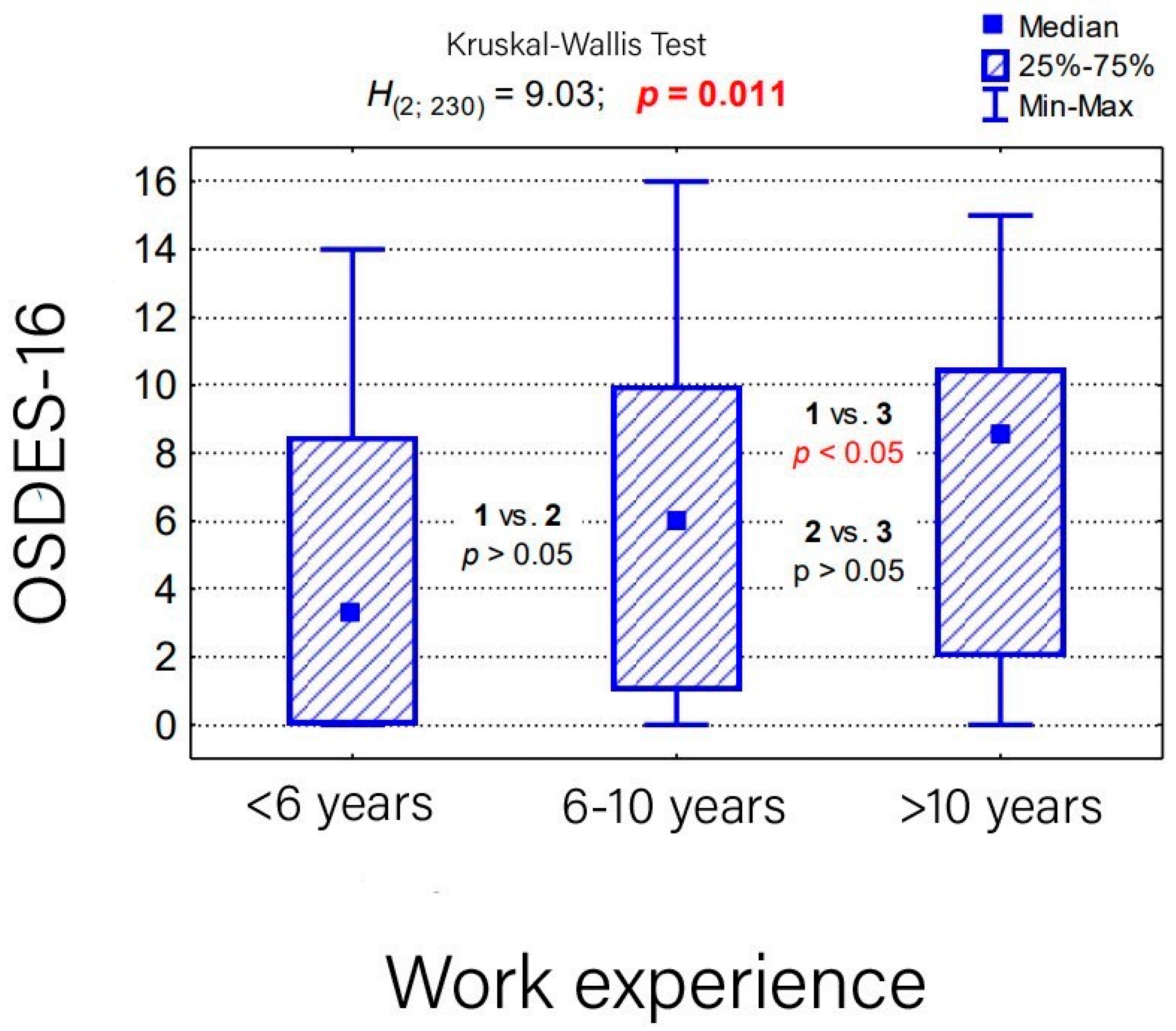
| The Level of Exposure | Seniority | p Test Score | ||
|---|---|---|---|---|
| <6 Lat N = 74 | 6–10 Lat N = 87 | >10 Lat N = 69 | ||
| OSDES-16 score | 0.011 | |||
| M ± SD | 4.5 ± 4.5 | 6.1 ± 4.7 | 6.8 ± 4.8 | |
| Me [Q1; Q3] | 3 [0; 9] | 6 [1; 10] | 9 [2; 11] | |
| Min–Max | 0–14 | 0–16 | 0–15 | |
| OSDES-16 scale rating | 0.037 | |||
| Low level | 38 (51.4) | 32 (36.8) | 21 (30.4) | |
| Average level | 15 (20.3) | 17 (19.5) | 11 (15.9) | |
| High level | 21 (28.4) | 38 (43.7) | 37 (53.6) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drozdowska, A.; Drozdowski, P.; Jaworski, A.; Ryczek, A.; Bula, D.; Adamczyk, D.; Adamczyk, J.; Łątkowska, A.; Sławińska, B.; Reich, A. Occupational Exposure of Employees in a Multispecialty Hospital to Factors Causing Contact Dermatitis—A Questionnaire Study. Medicina 2023, 59, 2084. https://doi.org/10.3390/medicina59122084
Drozdowska A, Drozdowski P, Jaworski A, Ryczek A, Bula D, Adamczyk D, Adamczyk J, Łątkowska A, Sławińska B, Reich A. Occupational Exposure of Employees in a Multispecialty Hospital to Factors Causing Contact Dermatitis—A Questionnaire Study. Medicina. 2023; 59(12):2084. https://doi.org/10.3390/medicina59122084
Chicago/Turabian StyleDrozdowska, Aneta, Piotr Drozdowski, Aleksander Jaworski, Anna Ryczek, Daniel Bula, Dawid Adamczyk, Jowita Adamczyk, Ada Łątkowska, Barbara Sławińska, and Adam Reich. 2023. "Occupational Exposure of Employees in a Multispecialty Hospital to Factors Causing Contact Dermatitis—A Questionnaire Study" Medicina 59, no. 12: 2084. https://doi.org/10.3390/medicina59122084
APA StyleDrozdowska, A., Drozdowski, P., Jaworski, A., Ryczek, A., Bula, D., Adamczyk, D., Adamczyk, J., Łątkowska, A., Sławińska, B., & Reich, A. (2023). Occupational Exposure of Employees in a Multispecialty Hospital to Factors Causing Contact Dermatitis—A Questionnaire Study. Medicina, 59(12), 2084. https://doi.org/10.3390/medicina59122084







