An Outbreak of Vancomycin-Resistant Enterococci in a City Hospital Intensive Care Unit: Molecular Characterization of Resistance
Abstract
1. Introduction
2. Materials and Methods
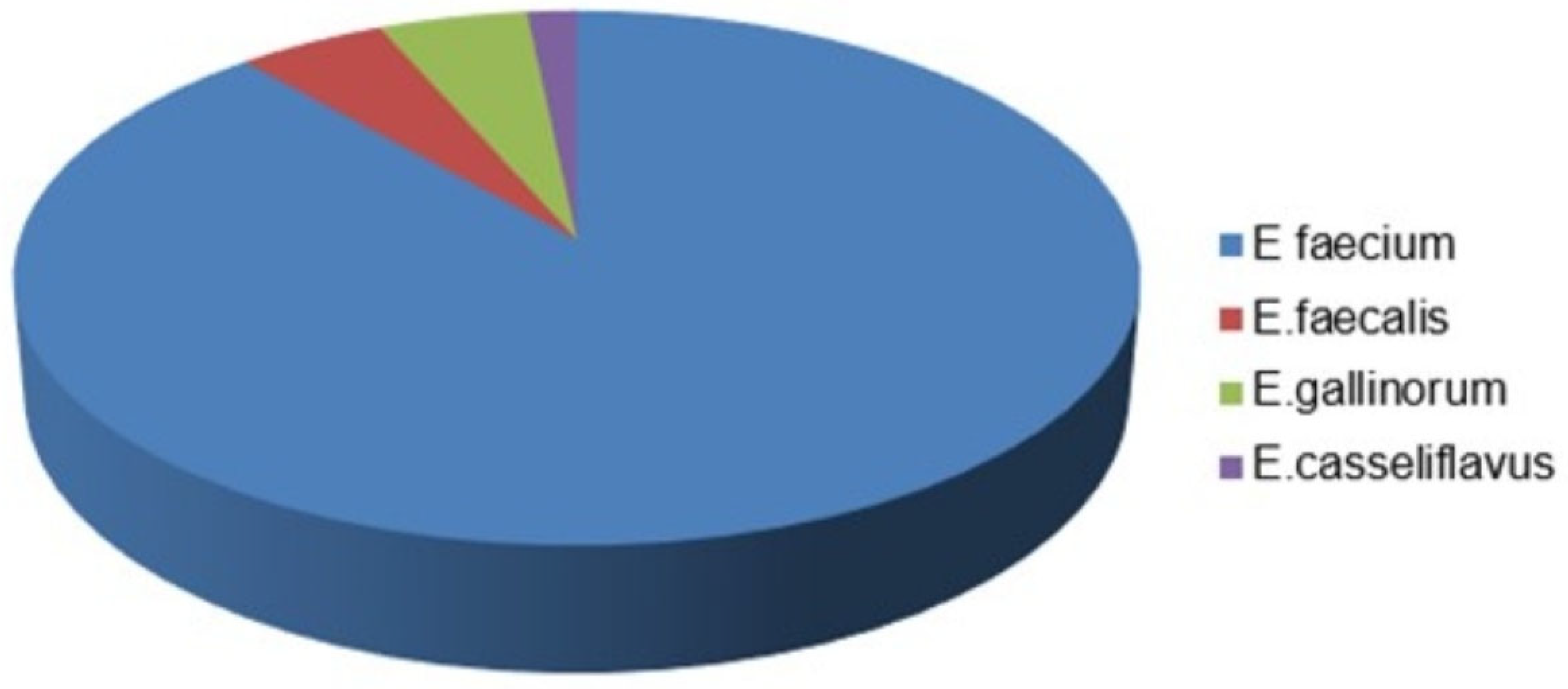
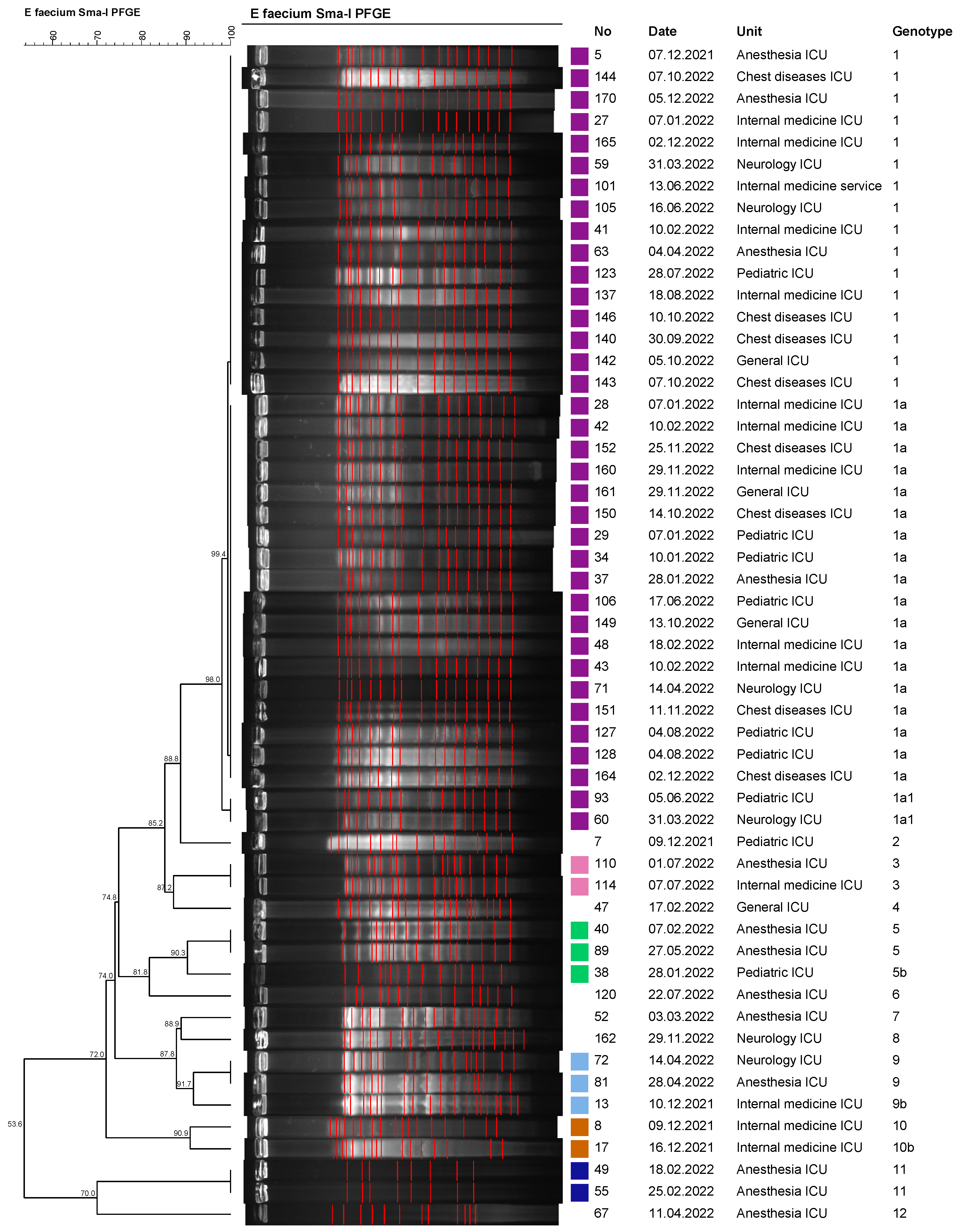
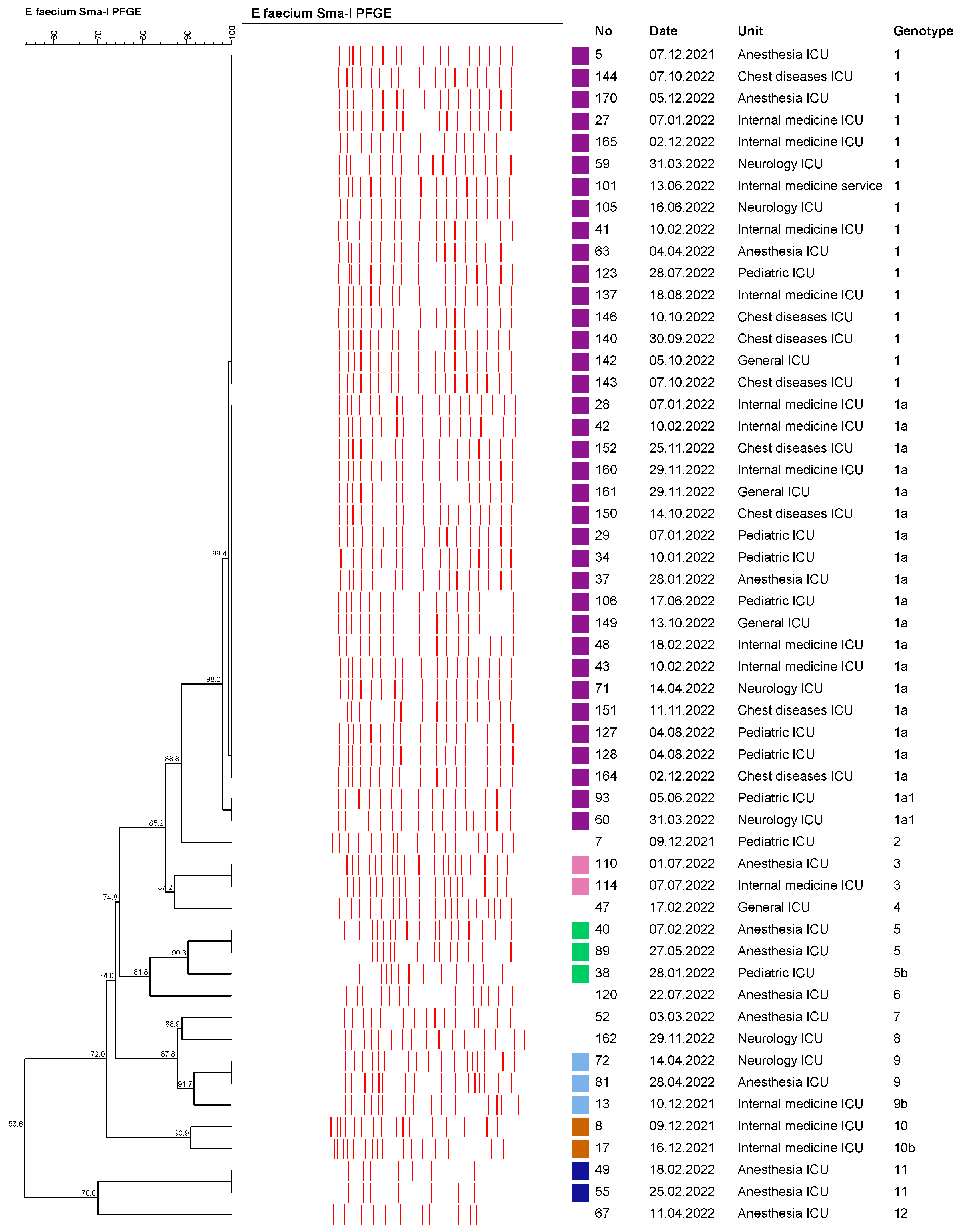
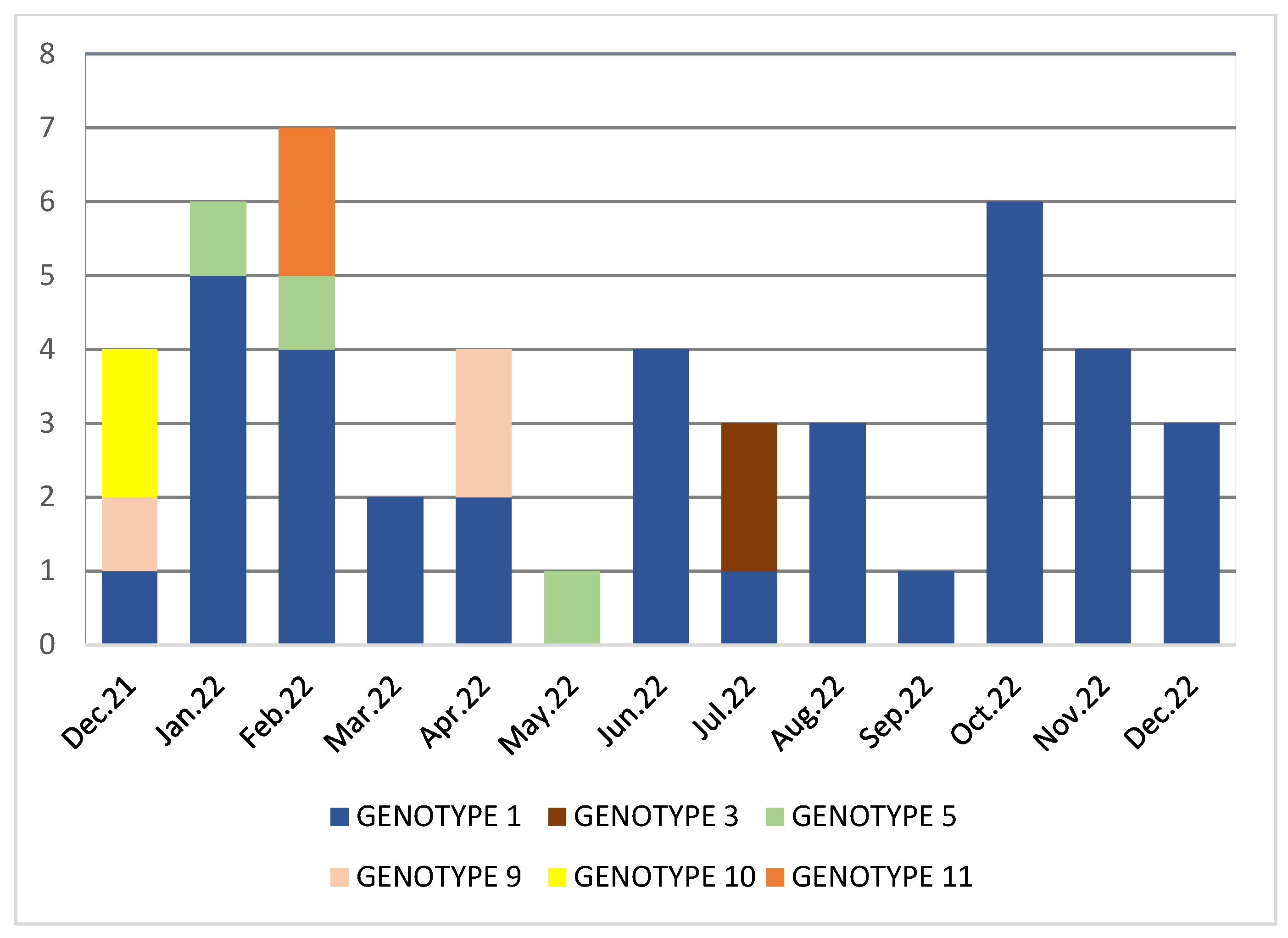
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Comerlato, C.B.; Ritter, A.C.; Miyamoto, K.N.; Brandelli, A. Proteomic study of Enterococcus durans LAB18S growing on prebiotic oligosaccharides. Food Microbiol. 2020, 89, 103430. [Google Scholar] [CrossRef] [PubMed]
- Zaheer, R.; Cook, S.R.; Barbieri, R.; Goji, N.; Cameron, A.; Petkau, A.; Polo, R.O.; Tymensen, L.; Stamm, C.; Song, J.; et al. Surveillance of Enterococcus spp. reveals distinct species and antimicrobial resistance diversity across a One-Health continuum. Sci. Rep. 2020, 10, 3937. [Google Scholar] [CrossRef] [PubMed]
- El-Kersh, T.A.; Marie, M.A.; Al-Sheikh, Y.A.; Al-Agamy, M.H.; Al Bloushy, A.A. Prevalence and risk factors of early fecal carriage of Enterococcus faecalis and Staphylococcus spp. and their antimicrobial resistant patterns among healthy neonates born in a hospital setting in central Saudi Arabia. Saudi Med. J. 2016, 37, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Ramos, S.; Silva, V.; Dapkevicius, M.d.L.E.; Igrejas, G.; Poeta, P. Enterococci, from Harmless Bacteria to a Pathogen. Microorganisms 2020, 8, 1118. [Google Scholar] [CrossRef] [PubMed]
- Orsi, G.B.; Ciorba, V. Vancomycin resistant enterococci healthcare associated infections. Ann. Ig. 2013, 25, 485–492. [Google Scholar] [CrossRef]
- Rios, R.; Reyes, J.; Carvajal, L.P.; Rincon, S.; Panesso, D.; Echeverri, A.M.; Dinh, A.; Kolokotronis, S.-O.; Narechania, A.; Tran, T.T.; et al. Genomic epidemiology of vancomycin-resistant Enterococcus faecium (VREfm) in Latin America: Revisiting the global VRE population structure. Sci. Rep. 2020, 10, 5636. [Google Scholar] [CrossRef]
- Miller, W.R.; Murray, B.E.; Rice, L.B.; Arias, C.A. Resistance in Vancomycin-Resistant Enterococci. Infect. Dis. Clin. 2020, 34, 751–771. [Google Scholar] [CrossRef]
- Polidori, M.; Nuccorini, A.; Tascini, C.; Gemignani, G.; Iapoce, R.; Leonildi, A.; Tagliaferri, E.; Menichetti, F. Vancomycin-resistant Enterococcus faecium (VRE) bacteremia in infective endocarditis successfully treated with combination daptomycin and tigecycline. J. Chemother. 2011, 23, 240–241. [Google Scholar] [CrossRef]
- Tacconelli, E.; Carrara, E.; Savoldi, A.; Harbarth, S.; Mendelson, M.; Monnet, D.L.; Pulcini, C.; Kahlmeter, G.; Kluytmans, J.; Carmeli, Y.; et al. WHO Pathogens Priority List Working Group. Discovery, research, and development of new antibiotics: The WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect. Dis. 2018, 18, 318–327. [Google Scholar] [CrossRef]
- European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint Tables for Interpretation of MICs and Zone Diameters. Version 12.0.2022. Available online: https://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_12.0_Breakpoint_Tables.pdf (accessed on 29 June 2023).
- Menekşe, Ş.; Tanrıverdi, E.S.; Oğuş, H.; Altınay, E.; Kaya, Ç.; Çağlayan, E.; Aydoğan, A.A.; Otlu, B.; Kırali, M.K. Stenotrophomonas maltophilia outbreak with a commercial blood gas injector as the culprit and interventions for source and prevention: A possible passage between patient and ECMO water heater device. Am. J. Infect. Control 2023, 51, 533–538. [Google Scholar] [CrossRef]
- Turabelidze, D.; Kotetishvili, M.; Kreger, A.; Morris, J.G., Jr.; Sulakvelidze, A. Improved pulsed-field gel electrophoresis for typing vancomycin-resistant enterococci. J. Clin. Microbiol. 2000, 38, 4242–4245. [Google Scholar] [CrossRef]
- Marcone, G.L.; Binda, E.; Berini, F.; Marinelli, F. Old and new glycopeptide antibiotics: From product to gene and back in the post-genomic era. Biotechnol. Adv. 2018, 36, 534–554. [Google Scholar] [CrossRef] [PubMed]
- Alçi, G.; Güneşer, D.; Güner, A.; Karahasan, A. Hastanede yatan hastalardan alınan rektal sürüntü örneklerinde vankomisine dirençli enterokok taranması: Stratejik değerlendirme. ANKEM Derg. 2021, 35, 70–76. [Google Scholar] [CrossRef]
- World Health Organization Regional Office for Europe. Antimicrobial Resistance Map. Available online: https://worldhealthorg.shinyapps.io/WHO-AMRDashboard/?_ga=2.172166563.1827800992.16686544401324205868.1668654440 (accessed on 13 January 2023).
- World Health Organization Regional Office for Europe/European Centre for Disease Prevention and Control. Antimicrobial resistance surveillance in Europe 2022–2020 Data; WHO Regional Office for Europe: Copenhagen, Danmark, 2022; Available online: https://www.ecdc.europa.eu/en/publications-data/antimicrobialresistance-surveillance-europe-2022-2020-data (accessed on 13 January 2023).
- Bulut, A.; Şengül, H.; Kaşıkcı, Ö.M. Vankomisine dirençli enterokok sürveyans çalışması: Bir devlet hastanesi örneği. J. Acad. Res. Nurs. 2018, 4, 21–27. [Google Scholar] [CrossRef]
- Kınıklı, S.; Cesur, S.; Hatipoğlu, Ç.A.; Arslan, K.; Karakök, T.; Demircan, Ş.A. Vankomisine dirençli enterokokların saptanmasında iki farklı kromojenik besiyerinin karşılaştırılması. Turk. J. Clin. Lab. 2019, 10, 319–323. [Google Scholar] [CrossRef][Green Version]
- Kirişçi, Ö.; Çalışkan, A. Rektal tarama örnekleri ile klinik örneklerde üreyen vankomisine dirençli enterokokların irdelenmesi:yedi yıllık sürveyans, retrospektif kesitsel bir çalışma. ANKEM Derg. 2020, 34, 105–111. [Google Scholar] [CrossRef]
- Kacar, F.; Eroğlu, E.; Tarakçı, A.; Çölkesen, F.D.; Özdemir Armağan, Ş.; Can, S. Vankomisine Dirençli Enterekok Enfeksiyonlarının İrdelenmesi. J. Turk. Soc. Intens. Care 2022, 20, 44–50. [Google Scholar] [CrossRef]
- Türk Mikrobiyoloji Cemiyeti, EUCAST Dirençli Olması Beklenen Fenotipler. Available online: https://www.tmconline.org/userfiles/file/Diren%C3%A7li-Olmas%C4%B1-Beklenen-Fenotipler-2022.pdf (accessed on 11 January 2023).
- Arslan, U.; Demir, E.; Oryaşin, E.; Türk Dağı, H.; Tuncer, I.; Fındık, D.; Bozdoğan, B. Kan kültürlerinden izole edilen vankomisine dirençli Enterococcus faecium suşlarının MLST tipleri [MLST types of vancomycinresistant Enterococcus faecium strains isolated from blood cultures]. Mikrobiyol. Bul. 2013, 47, 432–441. [Google Scholar] [CrossRef] [PubMed]
- Gozalan, A.; Coskun-Ari, F.F.; Ozdem, B.; Unaldi, O.; Celikbilek, N.; Kirca, F.; Aydogan, S.; Muderris, T.; Guven, T.; Acikgoz, Z.C.; et al. Molecular characterization of vancomycin-resistant Enterococcus faecium strains isolated from carriage and clinical samples in a tertiary hospital, Turkey. J. Med. Microbiol. 2015, 64, 759–766. [Google Scholar] [CrossRef]
- Güldemir, D.; Karagöz, A.; Dal, T.; Tekin, A.; Özekinci, T.; Durmaz, R. Hastane kaynaklı enterokok izolatlarının pulsed-field jel elektroforezis yöntemiyle moleküler tiplendirilmesi. Turk. Hij. Den. Biyol. Derg. 2015, 72, 1–10. [Google Scholar] [CrossRef]
- Sakin, F.; Aslantaş, Ö.; Bağcı, F. Molecular characterization of vancomycin resistant Enterococcus faecium isolates from patients admitted to intensive care unit in Hatay state hospital. Turk. J. Intensive Care 2019, 17, 204–208. [Google Scholar] [CrossRef]
- Asgin, N.; Otlu, B. Antibiotic Resistance and Molecular Epidemiology of Vancomycin-Resistant Enterococci in a Tertiary Care Hospital in Turkey. Infect. Drug Resist. 2020, 13, 191–198. [Google Scholar] [CrossRef] [PubMed]
- Bourdon, N.; Fines-Guyon, M.; Thiolet, J.M.; Maugat, S.; Coignard, B.; Leclercq, R.; Cattoir, V. Changing trends in vancomycin-resistant enterococci in French hospitals, 2001–2008. J. Antimicrob. Chemother. 2011, 66, 713–721. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, Y.; He, Z.; Wang, Y.; Wang, J.; Jin, D. A molecular study regarding the spread of vanA vancomycin-resistant Enterococcus faecium in a tertiary hospital in China. J. Glob. Antimicrob. Resist. 2022, 31, 270–278. [Google Scholar] [CrossRef]
- Purohit, G.; Gaind, R.; Dawar, R.; Verma, P.K.; Aggarwal, K.C.; Sardana, R.; Deb, M. Characterization of Vancomycin Resistant Enterococci in Hospitalized Patients and Role of Gut Colonization. J. Clin. Diagn. Res. 2017, 11, DC01–DC05. [Google Scholar] [CrossRef]
- Hammerum, A.M.; Baig, S.; Kamel, Y.; Roer, L.; Pinholt, M.; Gumpert, H.; Holzknecht, B.; Røder, B.; Justesen, U.S.; Samulioniené, J.; et al. Emergence of vanA Enterococcus faecium in Denmark, 2005–2015. J. Antimicrob. Chemother. 2017, 72, 2184–2190. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Şenol, F.F.; Tanrıverdi, E.S.; Aytaç, Ö.; Aşçı Toraman, Z.; Otlu, B. An Outbreak of Vancomycin-Resistant Enterococci in a City Hospital Intensive Care Unit: Molecular Characterization of Resistance. Medicina 2023, 59, 2081. https://doi.org/10.3390/medicina59122081
Şenol FF, Tanrıverdi ES, Aytaç Ö, Aşçı Toraman Z, Otlu B. An Outbreak of Vancomycin-Resistant Enterococci in a City Hospital Intensive Care Unit: Molecular Characterization of Resistance. Medicina. 2023; 59(12):2081. https://doi.org/10.3390/medicina59122081
Chicago/Turabian StyleŞenol, Feray Ferda, Elif Seren Tanrıverdi, Özlem Aytaç, Zulal Aşçı Toraman, and Barış Otlu. 2023. "An Outbreak of Vancomycin-Resistant Enterococci in a City Hospital Intensive Care Unit: Molecular Characterization of Resistance" Medicina 59, no. 12: 2081. https://doi.org/10.3390/medicina59122081
APA StyleŞenol, F. F., Tanrıverdi, E. S., Aytaç, Ö., Aşçı Toraman, Z., & Otlu, B. (2023). An Outbreak of Vancomycin-Resistant Enterococci in a City Hospital Intensive Care Unit: Molecular Characterization of Resistance. Medicina, 59(12), 2081. https://doi.org/10.3390/medicina59122081






