The Taiwanese Map of Axial Spondyloarthritis: Living with the Condition
Abstract
:1. Introduction
2. Materials and Methods
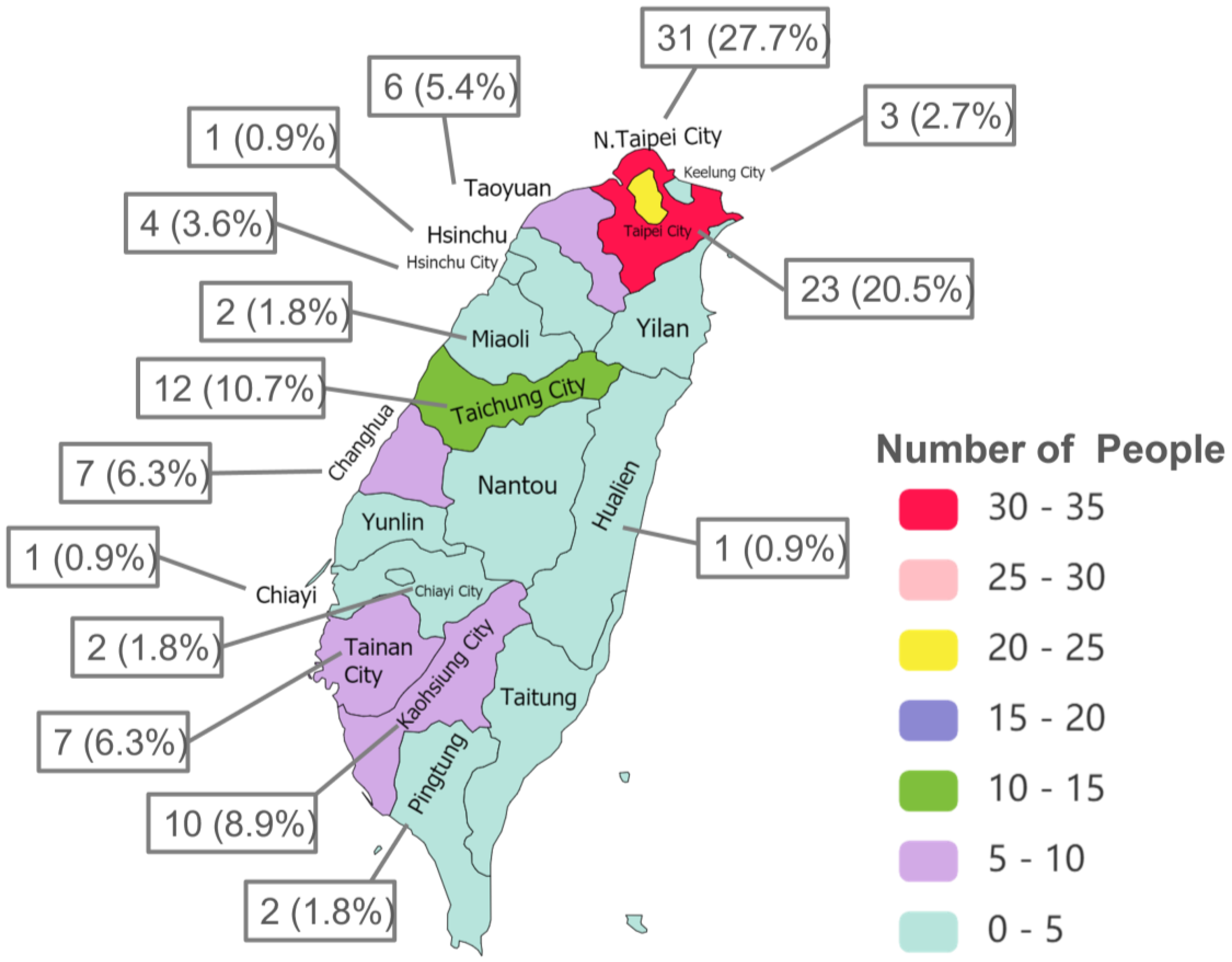
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, C.-T.; Hsieh, M.-Y.; Kuo, C.-F. Trend of Epidemiology of Ankylosing Spondylitis between 2006 and 2015 in Taiwan: A 10 Years Nationwide Population Study. Formos. J. Rheumatol. 2017, 31, 1–9. [Google Scholar] [CrossRef]
- Wei, J.C.-C. Ankylosing Spondylitis Databank Project in Taiwan: Epidemiology, Validation of Clinical indices, Inflammatory Markers and Human Leukocyte Antigen Analysis. Ph.D. Thesis, Chung Shan Medical University, Taichung, Taiwan, 2007. [Google Scholar]
- Garrido-Cumbrera, M.; Poddubnyy, D.; Gossec, L.; Gálvez-Ruiz, D.; Bundy, C.; Mahapatra, R.; Makri, S.; Christen, L.; Delgado-Domínguez, C.J.; Sanz-Gómez, S.; et al. The European Map of Axial Spondyloarthritis: Capturing the Patient Perspective-an Analysis of 2846 Patients Across 13 Countries. Curr. Rheumatol. Rep. 2019, 21, 19. [Google Scholar] [CrossRef] [PubMed]
- Garrett, S.; Jenkinson, T.; Kennedy, L.G.; Whitelock, H.; Gaisford, P.; Calin, A. A New Approach to Defining Disease Status in Ankylosing Spondylitis: The Bath Ankylosing Spondylitis Disease Activity Index. J. Rheumatol. 1994, 21, 2286–2291. [Google Scholar]
- Goldberg, D.P.; Williams, P. A User’s Guide to the General Health Questionnaire; nferNELSON: Windsor, UK, 1988. [Google Scholar]
- Chang, H.-C.; Yang, H.-C.; Chang, H.-Y.; Yeh, C.-J.; Chen, H.-H.; Huang, K.-C.; Pan, W.-H. Morbid Obesity in Taiwan: Prevalence, Trends, Associated Social Demographics, and Lifestyle Factors. PLoS ONE 2017, 12, e0169577. [Google Scholar] [CrossRef]
- Lu, M.-C.; Huang, K.-Y.; Tung, C.-H.; Hsu, B.-B.; Wu, C.-H.; Koo, M.; Lai, N.-S. Factors Associated with Disease-specific Quality of Life in Taiwanese Patients with Ankylosing Spondylitis: A Cross-sectional Study. BMJ Open 2019, 9, e028966. [Google Scholar] [CrossRef] [PubMed]
- Stokes, A.; Preston, S.H. Smoking and Reverse Causation Create an Obesity Paradox in Cardiovascular Disease. Obesity 2015, 23, 2485–2490. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Cumbrera, M.; Navarro-Compán, V.; Bundy, C.; Mahapatra, R.; Makri, S.; Correa-Fernández, J.; Christen, L.; Delgado-Domínguez, C.J.; Poddubnyy, D.; EMAS Working Group. Identifying Parameters Associated with Delayed Diagnosis in Axial Spondyloarthritis: Data from the European Map of Axial Spondyloarthritis. Rheumatology 2022, 61, 705–712. [Google Scholar] [CrossRef] [PubMed]
- Kreng, V.B.; Yang, C.T. The equality of resource allocation in health care under the National Health Insurance System in Taiwan. Health Policy 2011, 100, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Garrido-Cumbrera, M.; Poddubnyy, D.; Gossec, L.; Mahapatra, R.; Bundy, C.; Makri, S.; Sanz-Gómez, S.; Christen, L.; Delgado-Domínguez, C.J.; Navarro-Compán, V.; et al. Gender Differences in Patient Journey to Diagnosis and Disease Outcomes: Results from the European Map of Axial Spondyloarthritis (EMAS). Clin. Rheumatol. 2021, 40, 2753–2761. [Google Scholar] [CrossRef] [PubMed]
- Jovaní, V.; Blasco, M.; Ruiz-Cantero, M.T.; Pascual, E. Understanding How the Diagnostic Delay of Spondyloarthritis Differs Between Women and Men: A Systematic Review and Metaanalysis. J. Rheumatol. 2017, 44, 174–183. [Google Scholar] [CrossRef] [PubMed]
- Danve, A.; Deodhar, A. Axial spondyloarthritis in the USA: Diagnostic Challenges and Missed Opportunities. Clin. Rheumatol. 2019, 38, 625–634. [Google Scholar] [CrossRef] [PubMed]
- Taiwan Medical Association. 2019 Statistics Yearbook of Practicing Physicians and Health Care Organizations in Taiwan; Taiwan Medical Association: Taipei, Taiwan, 2019. [Google Scholar]
- Walsh, J.; Hunter, T.; Schroeder, K.; Sandoval, D.; Bolce, R. Trends in diagnostic prevalence and treatment patterns of male and female ankylosing spondylitis patients in the United States, 2006–2016. BMC Rheumatol. 2019, 3, 39. [Google Scholar] [CrossRef] [PubMed]
- Castillo-Ortiz, J.D.; Ramiro, S.; Landewé, R.; van der Heijde, D.; Dougados, M.; van den Bosch, F.; Boonen, A. Work Outcome in Patients with Ankylosing Spondylitis: Results from a 12-Year Followup of an International Study. Arthritis Care Res. 2016, 68, 544–552. [Google Scholar] [CrossRef] [PubMed]
- Boonen, A.; Brinkhuizen, T.; Landewé, R.; van der Heijde, D.; Severens, J.L. Impact of Ankylosing Spondylitis on Sick Leave, Presenteeism and Unpaid Productivity, and Estimation of the Societal Cost. Ann. Rheum. Dis. 2010, 69, 1123–1128. [Google Scholar] [CrossRef] [PubMed]
- Boonen, A.; Sieper, J.; van der Heijde, D.; Dougados, M.; Bukowski, J.F.; Valluri, S.; Vlahos, B.; Kotak, S. The Burden of Non-radiographic Axial Spondyloarthritis. Semin. Arthritis Rheum. 2015, 44, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Boonen, A.; Chorus, A.; Miedema, H.; van der Heijde, D.; Landewé, R.; Schouten, H.; van der Tempel, H.; van der Linden, S. Withdrawal from Labour Force Due to Work Disability in Patients with Ankylosing Spondylitis. Ann. Rheum. Dis. 2001, 60, 1033–1039. [Google Scholar] [CrossRef] [PubMed]
- Leverment, S.; Clarke, E.; Wadeley, A.; Sengupta, R. Prevalence and Factors Associated with Disturbed Sleep in Patients with Ankylosing Spondylitis and Non-radiographic Axial Spondyloarthritis: A Systematic Review. Rheumatol. Int. 2017, 37, 257–271. [Google Scholar] [CrossRef] [PubMed]
- Shen, C.-C.; Hu, L.-Y.; Yang, A.C.; Kuo, B.I.-T.; Chiang, Y.-Y.; Tsai, S.-J. Risk of Psychiatric Disorders following Ankylosing Spondylitis: A Nationwide Population-based Retrospective Cohort Study. J. Rheumatol. 2016, 43, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Thong, D.; Miller, N.; Duffield, S.J.; Hughes, D.M.; Chadwick, L.; Goodson, N.J. The Prevalence of Depression in Axial Spondyloarthritis and Its Association with Disease Activity: A Systematic Review and Meta-analysis. Arthritis Res. Ther. 2018, 20, 140. [Google Scholar] [CrossRef] [PubMed]
| Variable, n | Mean ± SD/n (%) |
|---|---|
| Age (years), n = 112 | 38.6 ± 10.3 |
| 18–34 | 39 (34.8%) |
| 35–51 | 60 (53.6%) |
| 52–68 | 13 (11.6%) |
| Gender (female), n = 112 | 28 (25%) |
| Marital status, n = 112 | |
| Single | 40 (35.7%) |
| Married | 67 (59.8%) |
| Divorced/separated | 4 (3.6%) |
| Widowed | 1 (0.9%) |
| Educational level, n = 112 | |
| Primary school | 1 (0.9%) |
| High school | 17 (15.2%) |
| College and university | 94 (83.9%) |
| Monthly income (New Taiwan Dollars) †, n = 107 | 22,971 ± 16,030 |
| Body mass index (BMI), n = 112 | |
| Underweight (BMI < 18.5) | 11 (9.8%) |
| Normal weight (BMI 18.5–24.9) | 59 (52.7%) |
| Overweight (BMI 25.0–29.9) | 28 (25%) |
| Obesity (BMI ≥ 30.0) | 14 (12.5%) |
| Smoking, n = 112 | |
| Non-smoker | 78 (69.6%) |
| Smoker | 34 (30.4%) |
| Alcohol consumption, n = 112 | |
| Never | 34 (30.4%) |
| Occasionally | 60 (53.6%) |
| 1 time per week | 8 (7.1%) |
| 2–3 days per week | 8 (7.1%) |
| 4–5 days per week | 1 (0.9%) |
| Every day | 1 (0.9%) |
| Member of a patient support group, n = 112 | |
| Yes | 44 (39.3%) |
| Variable, n | Mean ± SD/n (%) |
|---|---|
| Age at onset of the 1st symptoms, years, n = 112 | 28.1 ± 10.3 |
| Age at diagnosis, years, n = 112 | 31 ± 10.4 |
| Male (n = 84) | 30.5 ± 10.6 |
| Female (n = 28) | 32.5 ± 9.9 |
| Diagnostic delay, years, n = 112 | 3 ± 5.6 |
| Male (n = 84) | 3.6 ± 6.2 |
| Female (n = 28) | 1.3 ± 2.5 |
| Disease duration, years, n = 112 | |
| Male (n = 84) | 12.3 ± 10.6 |
| Female (n = 28) | 4.8 ± 4.2 |
| Extra-articular manifestations, n = 112 | |
| Uveitis | 9 (8.0%) |
| Crohn’s disease | 6 (5.4%) |
| Ulcerative colitis | 7 (6.3%) |
| HLA-B27 (positive), n = 49 | 35 (71.4%) |
| † BASDAI (0–10), n = 112 | 4.9 ± 1.9 |
| BASDAI < 4 | 32 (28.6%) |
| BASDAI ≥ 4 | 80 (71.4%) |
| Spinal stiffness, n = 112 | |
| No stiffness | 9 (8.0%) |
| Mild | 52 (46.4%) |
| Moderate | 33 (29.5%) |
| Severe | 18 (16.1%) |
| Variable, n | Mean ± SD/n (%) |
|---|---|
| Employment status of labor force, n = 90 | |
| Employed | 87 (96.7%) |
| Unemployed | 3 (3.3%) |
| Left/lost job because of axSpA, n = 3 | 2 (66.7%) |
| Employment status of the economically inactive, n = 22 | |
| Retired | 6 (27.3%) |
| Temporary sick leave | 6 (27.3%) |
| Permanent sick leave | 3 (13.6%) |
| Homemaker | 3 (13.6%) |
| Early retirement | 2 (9.1%) |
| Student | 1 (4.5%) |
| Other | 1 (4.5%) |
| Work-related issues due to axSpA, n = 112 | 99 (88.4%) |
| Missed work for doctor’s appointment, n = 96 | 47 (49.0%) |
| Took sick leave because of axSpA, n = 96 | 34 (35.4%) |
| Difficulties finding a job due to axSpA, n = 103 | 51 (49.5%) |
| AxSpA influenced job choice, n = 106 | 59 (55.7%) |
| Psychological comorbidities, n = 112 | |
| Anxiety | 29 (25.9%) |
| Sleep disorder | 26 (23.2%) |
| Depression | 23 (20.5%) |
| GHQ-12 † score (0–12), n = 112 | 3.3 ± 3.4 |
| GHQ-12 ≥ 3 | 50 (44.6%) |
| GHQ-12 < 3 | 62 (55.4%) |
| Most common fears, n = 111 | |
| Suffering pain | 78 (70.3%) |
| Suffering stiffness | 75 (67.6%) |
| Disease progression | 64 (57.7%) |
| Suffering fatigue | 63 (56.8%) |
| Most common hopes, n = 112 | |
| Eliminate pain | 78 (69.6%) |
| Eliminate stiffness | 74 (66.1%) |
| Reduce flares | 68 (60.7%) |
| Reduce fatigue | 67 (59.8%) |
| Most common treatment goals, n = 112 | |
| To eliminate/reduce pain | 79 (70.5%) |
| To eliminate/reduce stiffness | 75 (67.0%) |
| To reduce flares | 66 (58.9%) |
| Halt disease progression | 61 (54.5%) |
| Talked with treating physician about treatment goals, n = 108 | 40 (37.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yen, Y.-N.; Garrido-Cumbrera, M.; Sun, Y.-S.; Chen, C.-H.; Lai, C.-C.; Tsai, H.-C.; Chen, W.-S.; Liao, H.-T.; Tsao, Y.-P.; The Ankylosing Spondylitis Caring Society of R.O.C. (ASCARES); et al. The Taiwanese Map of Axial Spondyloarthritis: Living with the Condition. Medicina 2023, 59, 1962. https://doi.org/10.3390/medicina59111962
Yen Y-N, Garrido-Cumbrera M, Sun Y-S, Chen C-H, Lai C-C, Tsai H-C, Chen W-S, Liao H-T, Tsao Y-P, The Ankylosing Spondylitis Caring Society of R.O.C. (ASCARES), et al. The Taiwanese Map of Axial Spondyloarthritis: Living with the Condition. Medicina. 2023; 59(11):1962. https://doi.org/10.3390/medicina59111962
Chicago/Turabian StyleYen, Yi-Ning, Marco Garrido-Cumbrera, Yi-Syuan Sun, Chen-Hung Chen, Chien-Chih Lai, Hung-Cheng Tsai, Wei-Sheng Chen, Hsien-Tzung Liao, Yen-Po Tsao, The Ankylosing Spondylitis Caring Society of R.O.C. (ASCARES), and et al. 2023. "The Taiwanese Map of Axial Spondyloarthritis: Living with the Condition" Medicina 59, no. 11: 1962. https://doi.org/10.3390/medicina59111962
APA StyleYen, Y.-N., Garrido-Cumbrera, M., Sun, Y.-S., Chen, C.-H., Lai, C.-C., Tsai, H.-C., Chen, W.-S., Liao, H.-T., Tsao, Y.-P., The Ankylosing Spondylitis Caring Society of R.O.C. (ASCARES), Tsai, C.-Y., & Chou, C.-T. (2023). The Taiwanese Map of Axial Spondyloarthritis: Living with the Condition. Medicina, 59(11), 1962. https://doi.org/10.3390/medicina59111962







